Abstract
While the benefits of physical activity (PA) during and after pregnancy have been established, many women do not reach the recommended PA levels during this time. A major barrier found in the literature is a lack of counselling by healthcare providers (HCPs), which is partly caused by the limited knowledge on the topic. The aim of this study was to develop an intervention to improve the promotion of PA by HCPs. We used Intervention Mapping (IM), a theory-based framework to develop an intervention, called “Baby steps”, in a high-income (Austria) and a low-to-middle-income country (South Africa). We applied the following IM steps: (1) A needs assessment to determine the barriers and enablers of PA promotion by HCPs, including a scoping literature review and community needs assessments (qualitative interviews, questionnaires, and focus groups with midwives, obstetricians, and community health workers) to determine the desired outcomes of the intervention. (2) Performance and change objectives were formulated, describing the behaviors that need to change for the intervention to succeed. (3) Based on these objectives, theory-based behavior change techniques were selected, and practical applications were developed. (4) The applications were combined into two evidence-based interventions tailored to each country’s needs. Step (5) and (6) consist of an implementation and evaluation plan, respectively. The intervention is aimed at HCPs, such as midwives and community health workers, consisting of a two-day training course, including practical resources. Combining didactic and interactive education, it addresses both PA knowledge and the skills needed to transfer knowledge and facilitate behavior change. In the future, the intervention’s effect on women’s activity levels during and after pregnancy needs to be studied.
1. Introduction
There is a wealth of evidence for the beneficial effects of physical activity (PA) during the prenatal period for both mothers and offspring. Research has shown that being active during pregnancy is safe [1,2,3] and reduces the risk of gestational diabetes mellitus [4], as well as gestational hypertension and preeclampsia [5]. PA can also play an important role in reducing weight gain during pregnancy and in the postpartum period [6]. On the back of this evidence, women with uncomplicated pregnancies are recommended to participate in 150 min of moderate physical activity per week during pregnancy [7,8] and as soon as medically safe postpartum [9].
However, despite the numerous benefits and reputable recommendations, as much as 20–56% of pregnant women are not sufficiently active [10,11,12,13,14]. Regardless of the population and healthcare diversity in high- and low-to-middle income countries, it appears that both struggle with the same issues of prenatal physical inactivity. For example, formative work in South Africa (SA) has shown a decline in PA levels during pregnancy [15], as well as a lot of time spent in sedentary behavior [16]. This is similar to findings in Austria as part of the European DALI study [17]. Additionally, most women do not reach their pre-pregnancy levels of PA after giving birth [18,19].
While barriers such as an unsafe environment and cultural beliefs and norms might differ between low-to-middle and high-income countries, many personal barriers to achieving sufficient PA levels, such as a lack of time and motivation and physical discomforts, appear to be a common challenge [16,20,21,22,23]. In addition, a major barrier found both in our own formative work in SA [24] and in many other studies, is the lack of clear, specific information provided regarding PA during pregnancy by healthcare providers (HCPs) [20,21,25,26]. Indeed, studies have shown that while HCPs were identified as an important source of information [20,27], only a few discuss the topic of PA in pregnancy. At the HCP level, several barriers have been identified to explain this lack of promotion of PA, such as a lack of time and resources and insufficient skills [28].
Therefore, the development of an intervention focusing on improving PA promotion in HCPs is warranted. To develop the intervention, the Intervention Mapping (IM) process was applied. This provides a systematic protocol, which facilitates the development of interventions through an iterative, theory-based process, starting with the identification of health problems and leading to the development, implementation, and evaluation of an intervention. Due to the universal lack of PA promotion by HCPs and the global problem of inactivity during and after pregnancy, the intervention is developed in both a high-income (Austria) and a low-to-middle income country (SA) in order to expand the reach of the intervention and provide possible solutions that could be adapted and implemented across a variety of such settings.
In summary, the aim of this study is to develop a sustainable, evidence-based HCP intervention, focusing on reducing the barriers to PA promotion, and to ultimately improve women’s PA levels during pregnancy and the postpartum period.
2. Materials and Methods
2.1. Study Setting
The work in this paper was carried out at two sites: (1) Soweto, Johannesburg, SA, which is a previously disadvantaged area and is home to approximately 1.2 million people; and (2) Graz, Austria, which is the capital city of the Southern Austrian province of Styria and Austria’s second largest city, with approximately 330,000 inhabitants.
2.2. Intervention Development Group
The main group developing the intervention consisted of a physical activity researcher (E.W.), an epidemiologist with expertise in physical activity interventions and public health (M.V.P.), and a research midwife (A.D.).
2.3. Feedback Panel
External stakeholders and researchers with expertise in intervention development, behavior change, motivational interviewing, and PA promotion were consulted for input and feedback: the head of a midwifery school, two professors of midwifery, a professor in exercise science, a human movement scientist, and a research psychologist. Additionally, intervention target group participants, such as midwives and community health workers, have been consulted.
2.4. Intervention Mapping
This paper follows the systematic Intervention Mapping (IM) approach, a framework for the development of behavior change programs that incorporate both evidence and theory into the planning [29,30]. Interventions based on theory are more effective than those with little or no use of theory [31]. IM follows six steps: (1) needs assessment, (2) formulation of change objectives, (3) selection of methods and strategies, (4) intervention development, (5) implementation plan, and (6) evaluation plan [32], which are summarized in Figure 1. While the IM steps were performed for both countries simultaneously, the final developed intervention differs for both countries, reflecting differences in needs and healthcare systems. All intervention details are reported according to the TIDieR [33] checklist and guide (Supplementary File S1).
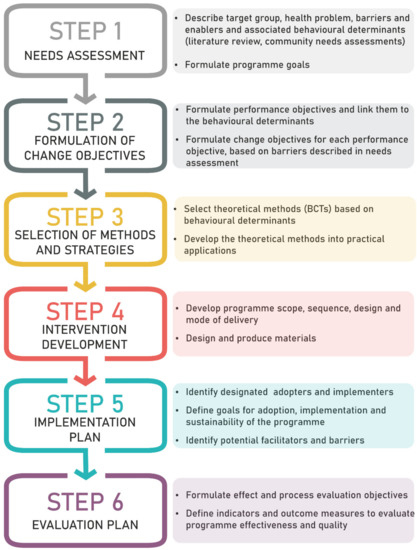
Figure 1.
Summary of the six Intervention Mapping steps. BCTs: behavior change techniques.
2.4.1. Step 1: Needs Assessment
The needs assessment uses a combination of published literature and our own formative work to describe the target group, the health problem, and its associated behavioral determinants. A literature review was performed to describe modifiable barriers and enablers of HCPs for the promotion of PA. Additionally, community needs assessments were performed both in Austria and in SA.
In Austria, no previous research on the barriers or enablers of PA promotion around pregnancy in the context of the Austrian healthcare system is available. Therefore, semi-structured interviews were undertaken (n = 10) with midwives and obstetricians, as well as the head of a midwifery school, to elicit information on how they currently promote PA to identify barriers and enablers and establish the participants’ attitudes towards a possible intervention.
In SA, previous research among healthcare professionals has already identified potential barriers and enablers of PA promotion during pregnancy [34]. Therefore, in order to provide an effective and sustainable solution, this work focused on the role of community health workers (CHWs) to deliver the intervention. A similar, self-administered questionnaire (Supplementary File S2) was administered to CHWs (n = 159) in order to assess their knowledge and attitudes towards general and prenatal PA. Additionally, ten focus groups were conducted on their role in the community, as well as issues of current knowledge and training in PA, to discover potential barriers that might not have been covered by the questionnaire. All methods were employed in accordance with the relevant guidelines and regulations. Informed consent was obtained from all participants. Ethical approval was obtained from the Human Research Ethics Committee of the University of the Witwatersrand (Clearance number M170273).
The updated version of the Theoretical Domains Framework (TDF) [35] was used to sort the findings from the needs assessment according to 14 TDF domains. The TDF domains were used to facilitate the combination of behavioral determinants with behavior change techniques in later steps. In the results section, only TDF domains, for which relevant associated behaviors were found in the needs assessment, are presented.
Step 1 concludes with the formulation of the program goals, defining the overall desired outcomes of the intervention, based on the findings of the needs assessment.
2.4.2. Step 2: Formulation of Change Objectives
In step 2, we determined performance objectives, meaning the behavior changes that are necessary to achieve the program goals. The performance objectives were then linked to the behavioral determinants described during the needs assessment. For each performance objective, change objectives were generated based on the barriers described in step 1. Thus, change objectives determine the very specific behaviors that will lead to changes in the behavioral determinants, which need to be changed successfully in order to achieve each respective performance objective. The performance and change objectives were refined and finalized after being reviewed by the feedback panel.
2.4.3. Step 3: Selection of Methods and Strategies
For step 3, appropriate theoretical methods to induce the desired behavior changes were chosen, and strategies were formulated on how these methods could be translated into practical applications. As theoretical methods, we selected specific behavior change techniques (BCT) from version 1 of the Behavior Change Technique Taxonomy (BCTTv1) [36]. A BCT is the “active ingredient” of an intervention—an observable and replicable component designed to change the behavior in question.
To help select appropriate BCTs, a recent publication by Johnston et al. was consulted, which aims to identify links between BCTs and their impact on determinants of behavior, based on literature and expert consensus [37]. Therefore, the BCTs for this intervention were selected based on these links, the input from the feedback panel, and taking into consideration their feasibility, relevance, and acceptability for each site.
2.4.4. Step 4: Intervention Development
In this step, the chosen practical applications of the BCTs, which were developed in step 3, were structured into two separate programs, tailored to the specific situations in Austria and SA. In addition to the program scope and sequence, the design and mode of delivery of the program were decided. Prototypes of all needed program materials were designed and pre-tested. To make sure that the program format is acceptable, and the produced materials are culturally appropriate and relevant, the two programs were matched visually, in language and experience, to the intended participant groups in SA and Austria, and future potential participants and stakeholders were asked for input and feedback.
2.4.5. Step 5: Implementation Plan
In step 5, an adoption and implementation plan was developed for the program. First, designated adopters and implementers of the program were identified. Next, program goals were specified for the adoption, implementation (encompassing fidelity, completeness, and dose), and sustainability of the intervention. To achieve these goals, potential facilitators and barriers were determined through brainstorming and a literature search, and methods and practical applications were chosen to address these for each country.
2.4.6. Step 6: Evaluation Plan
Finally, effect and process evaluation objectives were produced, and indicators and outcome measures to evaluate the effectiveness and quality of the intervention, were determined. This was based on the results of the needs assessment in step 1 and summarized into an evaluation plan.
3. Results
3.1. Step 1: Needs Assessment
3.1.1. Description of the Intervention Target Group
In Austria, the majority of prenatal care is supplied by obstetricians, including five compulsory prenatal check-ups, which are part of the “Mother-Child-Program” [38]. Additionally, a one-hour consult with a midwife at around 18–22 weeks of gestation is offered, which is also part of the standard prenatal care and covered by health insurance. Next to topics like birth preparation and breastfeeding, the subject of health-promoting behaviors, such as nutrition and PA, should be addressed during this consult [38]. As part of standard care after birth, all women are also entitled to home visits by a midwife up to 8 weeks postpartum. This puts midwives in an excellent position to promote physical activity, both in pregnancy and the postpartum period.
In SA, with its healthcare restraints and limited resources, community health workers (CHWs) are a sustainable alternative to healthcare professionals for delivering health promotion. CHWs are essentially members of a community that are supported by the health care system to provide culturally relevant health care services. They typically have no professional training but may have varying degrees of in-service training [39]. In recent years, there has been a drive within SA to re-design the healthcare delivery system to focus on the prevention, health promotion, and advocacy of healthy lifestyles [40]. CHWs play an integral role in this new healthcare model and have already been shown to be effective in improving maternal and child health outcomes [41]. CHWs will see pregnant or postpartum mothers not only in the clinic, but also for follow-up home visits as well, creating opportunities to support families, provide health information, and solve health problems and social challenges [40]. This would be a suitable platform for providing prenatal and postpartum lifestyle advice on PA levels and recommendations. In addition, women appear to prefer receiving health promoting messages from CHWs, as opposed to nurses or midwives at the clinic, which they find unfriendly, intimidating, and unapproachable for questions [24,42].
3.1.2. Description of the Health Problem
Despite the undisputed benefits of PA, many women do not meet the recommended levels during pregnancy and after birth. A lack of advice and information, or conflicting information, is a common barrier to being active in pregnancy and postpartum [20,21,24,26,43,44,45,46,47,48].
In line with this, there have been several successful interventions aimed at increasing physical activity levels, including counselling and education on the topic [49]. Providing information is an effective technique to change PA behavior during pregnancy [50]. Healthcare providers are an important source of information and advice [20,27] and are recommended to discuss physical activity, with practical, tailored advice at the earliest opportunity [51,52].
However, not all HCPs provide advice or specific counselling on PA [53], and less than a quarter do this on a regular basis [54]. In addition, women sometimes feel that HCPs lack the knowledge to answer their questions, and if information is given, it is often unclear or conflicting [27] and does not contain specific advice on the intensity, frequency, and duration of PA [55]. In our own community needs assessments, few of the interviewed Austrian midwives and gynecologists actively talked to pregnant women about PA in pregnancy, and even fewer saw it as their role to try to change the women’s behavior. In SA, while 96.6% of the participating CHWs believed that PA promotion is part of their job, they felt this role was hindered by their own lack of knowledge, training, and confidence to perform the role.
3.1.3. Determinants of Behavior Change
The results from the literature and community needs assessments on HCPs barriers and enablers of PA promotion are presented and sorted by the respective determinants of behavior change. A summary of the findings is provided in Table 1.

Table 1.
Summary of HCP barriers and enablers of PA promotion, sorted by TDF domain.
Knowledge
Pregnant women often receive no PA advice or advice that is limited, conservative, incorrect, or lacking in specificity [45,48,55,56,57], leading them to perceive their midwife’s knowledge on the topic as limited [58]. Indeed, some midwives themselves perceive their knowledge as too limited to give advice and have difficulties with providing recommendations on specific activities [28,59]. This lack of knowledge can be explained by a lack of familiarity with current guidelines and recommendations [53,60,61,62]. In a UK study, as little as 2% correctly identified the current PA in pregnancy guidelines, while nearly 60% reported a high confidence in answering questions relating to it [55]. Indeed, in SA, we encountered similar problems, with only 17% of HCPs aware of the current guidelines [34]. For the CHWs, 69% stated that they were familiar with the PA public health guidelines, and yet 19.7% believed that only vigorous PA is beneficial for health, while 45.9% did not know how to measure intensity. Almost ¼ described this lack of knowledge as a major barrier to giving advice to members of their community.
This lack of knowledge of PA advice and guidelines likely stems from HCPs’ lack of effective training in this area. Leiferman et al. [53] found that 17% of HCPs had never received any training on PA, and out of those who had, 69% rated its quality as fair or poor. Midwives in other studies similarly report that they received little to no formal training on PA during pregnancy [28,59], and very few (4%) reported having access to continued education in this area [55].
Consequently, many HCPs cite common sense, their own experiences, colleagues, or the internet as their sources of information, as opposed to evidence-based resources [55,59,62]. Many midwives are unaware of the professional resources available to them [59], which emphasizes the importance of increasing undergraduate teaching, as well as continued professional development in this area [34,59,61].
Austrian participants of the community needs assessment reported that they had received little to no training on the topic of PA in pregnancy and postpartum during their education and had limited access to post-graduate training on the subject, although most showed interest in future trainings when offered. In SA, only 15.9% of CHWs reported having any formal training in the area of PA, causing a discord between their perceived role and the training received. Current training focused mainly on communicable diseases (HIV/AIDS, tuberculosis) or changes in health policy (immunizations), rather than on PA.
Skills
Many HCPs see the task of counselling their patients on PA as a complex challenge [63]. They report both a lack of ability, as well as a lack confidence and self-belief, to adequately advise women [28,53,59], resulting in the feeling that they are unable to induce behavior change in their clients [53]. While they are often aware of the common barriers to becoming active that pregnant women face, addressing those barriers has also been named as a challenge [63].
Similar barriers were observed in the community needs assessment, where only few of the Austrian participants reported that they had received training on facilitating behavior change in pregnant women, while others appeared to have neither the necessary skills nor the confidence for the task. In SA, hardly any CHWs reported having any formal training on behavior change.
Social/Professional Role and Identity
Many midwives see giving advice on PA as part of their professional role [28] and acknowledge that they are ideally placed for this role. However, some think that too many aspects of health promotion are placed on them [63,64], and some feel unqualified or question their own suitability as a source of advice and guidance [59]. Some midwives also think it is the women’s general practitioner and obstetric team’s responsibility to counsel women on PA [28], and others reported they have colleagues who think health promotion is unnecessary [64]. Referral to exercise professionals can also be a challenge, where pregnant women are often referred back to their midwife for further advice [59].
In our community needs assessment, it was unclear to the interviewed Austrian midwives who should be responsible for counselling women on the subject, and most identified the mid-pregnancy one-hour consult as an opportunity to discuss PA. In SA, while the majority (96.6%) of CHWs believed that PA promotion is part of their job, a lack of knowledge and training was seen as a major barrier in fulfilling this role.
Beliefs about Capabilities
HCPs need confidence to transfer knowledge to patients and to encourage and motivate them in an effective way. However, even though HCPs can have a positive effect on PA levels in pregnant women by means of counselling or education [49], many HCPs feel that they are unable to induce behavior change in their patients [53]. They report feeling frustrated when seeing that their PA promotion efforts were ineffective [63] and report a lack of confidence to advise women [28]. HCPs describe meeting expecting parents’ increasingly high expectations in their professional performance as demanding [63].
Similarly, in the Austrian community needs assessment, HCPs identified overweight and obese women as a risk group, which would especially benefit from improved PA levels. However, they felt that this group was unlikely to change their behavior and that counselling these women would therefore be futile. In SA, many CHWs expressed concern about being ridiculed if they provided the wrong information, especially since pregnant women can readily look up information on the internet or other media sources. They felt that training would equip them to feel confident to provide the right information and answer questions.
Beliefs about Consequences
Nearly all midwives and other HCPs acknowledge the importance of PA [28,60]. However, several HCPs report feeling uncomfortable discussing PA with pregnant women and worry about how to communicate effectively without offending and damaging their relationship with them [28,59,63]. Especially when talking to overweight or obese women, PA is seen as a sensitive topic by many caregivers [53]. HCPs think only women who are already active will be interested in specific PA advice in pregnancy [59]. Pregnant women reported that they felt that advice given by their midwife or sports trainer was overly cautious and risk adverse out of a fear that the mother might harm herself or her offspring [27]. A fear of potential litigation was also named a barrier to discussing PA in practice [59].
Intentions
While many HCPs are reportedly motivated to promote healthy behavior in pregnant women, they regard it as secondary to their clinical tasks [64] and consequently do not prioritize the promotion of PA or plan to discuss it in daily practice [28,59]. During the interviews in Austria, a large majority of participating midwives and gynecologists also reported that they did not think PA was a topic of priority and consequently did not actively talk to pregnant women about it.
Environmental Context and Resources
HCPs report a lack of supportive materials as a barrier to PA counselling, such as educational and motivational leaflets or online tools [59]. Previous formative work in SA has also highlighted the need to provide an information booklet to hand out [65]. Another potential barrier to promoting PA is the lack of awareness of local exercise offerings to which HCPs could refer to [53,59]. In Austria, some HCPs actively referred to local pregnancy-specific activity programs. However, most had very limited knowledge on the programs offered in the area. Several felt a pamphlet to hand out to their patients would be useful, which should also include information about existing local programs. In SA, when discussing what PA training CHWs required, one of the main priorities reported was the provision of specific exercises for pregnant women. They reported the need for specific, standardized information provided on a regular basis. They felt that having a pamphlet to give to pregnant women would also be helpful, as well as a training manual for future reference.
One of the resources most often reported lacking, which therefore hinders the inclusion of PA advice in daily practice, is time [28,53,59,63,64]. A possible explanation for this lack of time is increased pressure at work due to an increase in tasks to perform [63,64], which results in other tasks gaining priority over health promotion [59,64]. A shortage of time was also a widely reported barrier in our community needs assessment, with clinical or other tasks generally being prioritized.
In summary, due to the profound barriers to PA promotion found in HCPs, it is imperative to first address these barriers on the HCP level to create a supportive environment, before focusing on perinatal interventions at the level of the women themselves. The goal of this intervention is therefore to increase the frequency and quality of perinatal PA promotion by HCPs.
3.2. Step 2: Formulation of Change Objectives
The desired intervention outcome is specified in more detail by the performance objectives and change objectives. Due to limited resources, the objectives focus on individual level changes, with organizational and community level changes lying outside the scope of this project.
After formulating the performance objectives, the barriers and enablers and their associated behaviors, which were mapped onto TDF domains during the needs assessment, were matched to the performance objectives and reformulated as change objectives in Table 2. Some change objectives were associated with more than one TDF domain. For example, “HCPs see themselves as the right person to promote PA in pregnancy and postpartum” was mapped against the determinants “Social/professional role and identity” and “Beliefs about capabilities”. Barriers were found to represent seven of the 14 domains (Knowledge, Skills, Social/professional role and identity, Beliefs about capabilities, Beliefs about consequences, Intentions, Environmental context, and resources).

Table 2.
Performance objectives with mapped change objectives and respective TDF domains.
3.3. Step 3: Selection of Theory-Based Methods and Practical Strategies
In step 3, methods to induce behavior change were selected and translated into practical applications. We selected 14 suitable BCTs linked to the seven TDF domains relevant to our project (Supplementary File S3). Several BCTs apply to more than one TDF domain, for example, the BCT “Problem solving” is linked to the domains “Skills”, “Beliefs about capabilities”, and “Environmental context and resources”.
In Table 3, for each chosen BCT, practical applications are presented. For example, the BCT “Graded tasks” refers to role plays with participants practicing the desired behavior of PA promotion, starting with simple scenarios and progressing towards increasingly complex cases. The practical intervention applications were developed considering their affordability, relevance, and practicality, as well as their acceptability for the intended participants.

Table 3.
Performance objectives with mapped change objectives and respective TDF domains.
3.4. Step 4: Intervention Development
The intervention, named “Baby steps”, is designed as an in-person training, combining didactic and interactive education, which has been shown to be effective in changing professional practice [66]. The two-day training will focus on two key points, firstly to equip the participants with all relevant knowledge about PA during and after pregnancy, and secondly to give them tools to transfer this knowledge and to induce behavior change in pregnant women.
The first part of the training will cover the theory of physiological changes during pregnancy and the implications these changes have on PA prescription and the benefits and risks of participating in PA during pregnancy. The PA guidelines and recommendations will be discussed. Participants will receive information on exercise safety and learn to use a standardized, systematic approach to prescribe tailored PA during pregnancy and the postpartum period and when and how to refer to a specialist if needed. Common barriers that women face in becoming active and solutions to overcome them will be addressed.
The second part focuses on knowledge transfer, as well as how to motivate and empower women to change their behavior, while respecting the women’s autonomy. Participants will learn the theory and application of motivational interviewing, a client-centered counselling style aimed at facilitating behavior change [67], which has already been successfully applied to induce behavior change during pregnancy [17]. To apply the learned theory in practice, interactive demonstrations, discussions of case studies, and role plays will be performed. The training in each country will be tailored to fit the different cultures and languages, barriers, and medical background knowledge of South African CHWs and Austrian midwives.
Multiple materials were designed for the intervention. A detailed handbook accompanying the training in each country, containing all contents of the intervention, will be given out to all participants and will include the core elements of the intervention, as well as a list of evidence-based resources, regional specialists, and local programs. As it has been shown that printed educational materials can improve HCPs’ performance [68], an information pamphlet was produced and will be provided to all HCPs to be handed out during the PA promotion. Additionally, a poster to put up in waiting areas will be given out during the training, as it can prompt discussion of the subject. Different versions were produced of all materials, including German and Zulu translations, as well as different culturally relevant pictures and examples. The handbook, pamphlet, and poster can be downloaded from https://baby-steps.international/ (accessed on 27 May 2021).
3.5. Step 5: Implementation Plan
Step 5 is concerned with the successful adoption and implementation of the intervention. The program will be adopted and implemented in both countries by the program developers. The goal is to implement the complete intervention in both countries and achieve sustainability through the maintenance of the training at regular intervals. As the program developers are directly involved in the process, we expect a high fidelity and completeness in the implementation of the training.
The training will be offered in a group setting in both countries and will be repeated yearly. In Austria, the training on motivational interviewing will be provided by a psychologist experienced in giving motivational interviewing training. A sports scientist specialized in pregnancy and the postpartum period will provide real-life experiences and examples. Additional support will be given by a midwifery school, including the provision of premises for the training. The training will be credited by the Austrian Midwives Association (Österreichisches Hebammengremium) to increase participation and form part of their continued professional development. It will be embedded in the midwives association’s online system, which offers all credited trainings on the official website and will therefore automatically be accessible to all Austrian midwives. To increase the visibility and thus the recruitment of participants for the training, it will, in addition, be advertised in the Austrian midwifery journal and newsletters. While the current intervention is aimed at qualified midwives, a future goal is to embed the training in their vocational education and to extend the intervention to all healthcare professions associated with pregnancy.
In SA, the training will be facilitated by PA researchers and supported by clinic managers and nurses. It will be run through the public health sector of the organization that employs the CHWs and will therefore be part of their initial recruitment training, as well as a compulsory yearly training. The aim is to demonstrate to the South African government the effectiveness of the training to embed PA promotion into the new national CHWs training curriculum.
3.6. Step 6: Evaluation Plan
To assess the intervention effect, the first instalment of the training will serve as a pilot in both countries. The aim of our intervention was to increase the promotion of PA in pregnancy and postpartum by HCPs. To measure the effect of the training on the behavior of HCPs, we developed a survey to be administered immediately before and four weeks after the intervention, assessing how and how often participants promote PA in daily practice (Supplementary File S4). Additional questions will assess whether the intervention had an effect on the various TDF domains and ultimately on the performance and change objectives. The survey is based on a questionnaire by Huijg et al. developed to assess TDF domains [69] and existing questionnaires on PA in pregnancy, aimed at HCPs [28,60]. Additional questions assessing knowledge were based on current PA guidelines.
As part of the process evaluation, we evaluate the reach, recruitment, fidelity, and satisfaction of our training intervention [70]. The reach will measure whether the intervention reached the intended group, which comprises mainly midwives in Austria and CHWs in South Africa, although other HCPs in a position to promote PA around pregnancy will not be excluded. The reach will be assessed by determining how many of the participants of the intervention were part of the intended group. An adequate reach would mean that 100% of participants are HCPs from the target group. As the training in SA will be compulsory for all CHWs, an acceptable recruitment in SA will be reached if at least 70% of all CHWs within the designated region receive the training. In Austria, acceptable recruitment will be reached if, for each training instalment, at least 70% of the total capacity of 20 participants is reached. In addition, we will review whether all strategies on the recruitment and advertising of the training were applied as planned. The fidelity will be assessed by means of the handbook, which contains all core elements of the intervention. Each training session will be compared against the handbook sequence and content. The fidelity will be acceptable if each section was covered during the training. Additional questions were added to the post-intervention effect evaluation survey to assess the HCPs’ satisfaction with the training, including the overall satisfaction with regard to the delivery of the training, training content, and usefulness of the training and materials. Additionally, a focus group is scheduled in both countries at the end of each training session to allow for more in-depth feedback, including barriers and enablers of the effectiveness and implementation of the intervention.
4. Discussion and Next Steps
In this paper, we have presented how we used the IM protocol to develop an intervention aimed at healthcare workers in order to equip them with the necessary tools to be able to deliver evidence-based, tailored, high-quality PA promotion to all women during and after pregnancy. The intervention addresses the barriers to PA promotion using theory-based behavior change techniques to achieve the desired behavior in healthcare workers. In the future, a randomized controlled trial will be performed to assess the effectiveness of the intervention.
Our intervention is based on a detailed description of the barriers and enablers found both in the literature and community needs assessments and aims to influence different behavioral determinants of HCPs. It has been shown that the identification and addressing of barriers improves the effectiveness of interventions [71]. The key barriers that we found were a lack of knowledge, skills, and resources, a lack of time and prioritization, and uncertainty about the professional role of HCPs. Similarly, Keyworth et al. [72] found that the barriers of a lack of time, professional role perception, and prioritization were common across different healthcare professions. The authors call for support in identifying opportunities for diverse professional groups to deliver interventions, which is what our research proposes to do. Addressing these barriers is important, as a review investigating the factors influencing primary healthcare professionals’ PA promotion behaviors found that healthcare professionals’ attitudes, intentions, and education on the topic were positively associated with PA promotion [73].
The importance of educating HCPs on the topic of PA was underlined by the findings from our needs assessment, showing that HCPs had limited knowledge about PA in general and specifically during pregnancy. This lack of knowledge is likely caused by the limited availability of undergraduate and continued professional training on the topic, which is also an issue found in other healthcare professions [74]. Our intervention combines education about physical activity with a training session on facilitating behavior change. Training sessions aimed at the acquisition of knowledge and skills are an important enabler for HCPs to deliver individualized and tailored behavior change interventions [51,72], and the ‘making every contact count’ program showed that equipping HCPs with skills to support behavior change, including the promotion of PA, is associated with a significant increase in utilizing these skills in clinical practice [75]. In addition, our intervention is largely based on theoretical approaches and frameworks, which have been shown to improve the effectiveness of the intervention [76], and the use of BCTs ensures that the program is standardized and the results could be replicated in future [36].
Finally, another strength of our study is its development in two economically different countries, expanding the reach of our interventions and making the associated materials more generalizable and relevant to a broader public. The intervention can be adapted and adopted by a variety of professionals in a variety of settings.
Our intervention study has a few limitations. The proposed links between the BCTs and TDF domains used [37] remain hypothetical and are yet to be empirically proven. However, through the systematic and transparent reporting of our intervention development, a replicable intervention is presented, making it possible to identify and investigate individual components, thereby adding to the evidence and providing information for the development of future interventions.
Next Steps
An RCT is planned to objectively assess the intervention’s effect on HCPs’ behavior, and its effect on women’s PA levels during and after pregnancy. Furthermore, the long-term aim is to integrate the training into HCPs’ vocational education and extend the training to other, relevant professions. Additionally, PA promotion should be addressed on an organizational and community level to increase the reach of the intervention.
5. Conclusions
This paper describes how we systematically applied Intervention Mapping to develop an evidence-informed, theory-based intervention, called “Baby steps”, to improve PA promotion by healthcare providers during and after pregnancy and how we plan to implement and evaluate it. The effectiveness of the program will be investigated in the future in a randomized controlled trial. It is clear, from the literature, that intervening to improve PA levels during and after pregnancy is essential for women’s health. This evidence- and theory-based intervention aims at tackling this international problem in various settings.
Supplementary Materials
The following are available online at https://www.mdpi.com/article/10.3390/ijerph18115869/s1, File S1: TiDieR Checklist, File S2: Needs assessment survey for community health workers, File S3: Table describing the chosen BCTs linked to TDF domains, File S4: Survey on Physical Activity in Pregnancy and Postpartum for Healthcare Providers.
Author Contributions
Conceptualization, M.N.M.v.P. and E.D.W.; methodology, M.N.M.v.P. and E.D.W.; formal analysis, A.M.D. and E.D.W.; writing—original draft preparation, A.M.D. and E.D.W.; writing—review and editing, A.M.D., M.N.M.v.P., and E.D.W.; supervision, M.N.M.v.P.; funding acquisition, M.N.M.v.P. and E.D.W. All authors have read and agreed to the published version of the manuscript.
Funding
Funded in Austria by the Centre for International Cooperation and Mobility (ICM) of the Austrian Agency for International Cooperation in Education and Research (OeAD-GmbH): Project nr ZA 17/2019 and in South Africa by the NRF program for Scientific and Technological Cooperation: Grant nr 116071. A.M.D. was funded by the Austrian Science Fund (FWF; DOC 31-B26) and the Medical University of Graz through the PhD Program, Inflammatory Disorders in Pregnancy (DP-iDP). Open access funding provided by the Austrian Science Fund (FWF). The funders had no role in any aspect of the study, besides the funding.
Institutional Review Board Statement
The study was conducted according to the guidelines of the Declaration of Helsinki and approved by the Human Research Ethics Committee of the University of Witwatersrand (Clearance number M170273). All methods were carried out in accordance with the relevant guidelines and regulations.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The data presented in this study are available on reasonable request from the corresponding author.
Acknowledgments
We would like to thank all participants of the needs assessments, as well as the midwives, community health workers, experts, and stakeholders who gave feedback during the intervention development, including Annick Bogaerts; Sarah van Haeken; Judith Jelsma; Moenie van der Kleyn; Vicki Lambert; Marianne Nieuwenhuijze; Mark Stoutenberg; and Tebogo Mabubula. We thank Anna Prattes for her help with conducting the interviews in Austria and Gudani Mukoma and Sandra Pretorius for their assistance with the data collection in South Africa. Thank you to all the community health workers, midwives, and obstetricians who so willingly gave up their time to discuss physical activity with us.
Conflicts of Interest
The authors declare no conflict of interest. The funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript, or in the decision to publish the results.
References
- Brown, W. The benefits of physical activity during pregnancy. J. Sci. Med. Sport 2002, 5, 37–45. [Google Scholar] [CrossRef]
- Mudd, L.M.; Owe, K.M.; Mottola, M.F.; Pivarnik, J.M. Health benefits of physical activity during pregnancy: An international perspective. Med. Sci. Sports Exerc. 2013, 45, 267–288. [Google Scholar] [CrossRef] [PubMed]
- Schlüssel, M.M.; De Souza, E.B.; Reichenheim, M.E.; Kac, G. Physical activity during pregnancy and maternal-child health outcomes: A systematic literature review. Cadernos Saúde Pública 2008, 24, s531–s544. [Google Scholar] [CrossRef]
- Aune, D.; Sen, A.; Henriksen, T.; Saugstad, O.D.; Tonstad, S. Physical activity and the risk of gestational diabetes mellitus: A systematic review and dose–response meta-analysis of epidemiological studies. Eur. J. Epidemiol. 2016, 31, 967–997. [Google Scholar] [CrossRef]
- Davenport, M.H.; Ruchat, S.-M.; Poitras, V.J.; Garcia, A.J.; Gray, C.; Barrowman, N.; Skow, R.J.; Meah, V.L.; Riske, L.; Sobierajski, F.; et al. Prenatal exercise for the prevention of gestational diabetes mellitus and hypertensive disorders of pregnancy: A systematic review and meta-analysis. Br. J. Sports Med. 2018, 52, 1367–1375. [Google Scholar] [CrossRef] [PubMed]
- Ruchat, S.-M.; Mottola, M.F.; Skow, R.J.; Nagpal, T.S.; Meah, V.L.; James, M.; Riske, L.; Sobierajski, F.; Kathol, A.J.; Marchand, A.-A.; et al. Effectiveness of exercise interventions in the prevention of excessive gestational weight gain and postpartum weight retention: A systematic review and meta-analysis. Br. J. Sports Med. 2018, 52, 1347–1356. [Google Scholar] [CrossRef] [PubMed]
- Artal, R. Exercise in Pregnancy: Guidelines. Clin. Obstet. Gynecol. 2016, 59, 639–644. [Google Scholar] [CrossRef] [PubMed]
- Mottola, M.F.; Davenport, M.H.; Ruchat, S.M.; Davies, G.A.; Poitras, V.J.; Gray, C.E.; Garcia, A.J.; Barrowman, N.; Adamo, K.B.; Duggan, M.; et al. 2019 Canadian guideline for physical activity throughout pregnancy. Br. J. Sports Med. 2018, 52, 1349–1366. [Google Scholar] [CrossRef]
- American College of Obstetricians and Gynecologists. Physical Activity and Exercise during Pregnancy and the Postpartum Period: ACOG Committee Opinion, Number 804. Obstet. Gynecol. 2020, 126, e135–142. [Google Scholar]
- Borodulin, K.; Evenson, K.R.; Herring, A.H. Physical activity patterns during pregnancy through postpartum. BMC Women’s Health 2009, 9, 32. [Google Scholar] [CrossRef] [PubMed]
- Borodulin, K.M.; Evenson, K.R.; Wen, F.; Herring, A.H.; Benson, A.M. Physical activity patterns during pregnancy. Med. Sci. Sports Exerc. 2008, 40, 1901. [Google Scholar] [CrossRef] [PubMed]
- Evenson, K.R.; Wen, F. National trends in self-reported physical activity and sedentary behaviors among pregnant women: NHANES 1999–2006. Prev. Med. 2010, 50, 123–128. [Google Scholar] [CrossRef]
- Hesketh, K.R.; Evenson, K.R. Prevalence of U.S. Pregnant Women Meeting 2015 ACOG Physical Activity Guidelines. Am. J. Prev. Med. 2016, 51, e87–e89. [Google Scholar] [CrossRef]
- Poudevigne, M.S.; O’Connor, P.J. A Review of Physical Activity Patterns in Pregnant Women and Their Relationship to Psychological Health. Sports Med. 2006, 36, 19–38. [Google Scholar] [CrossRef] [PubMed]
- Watson, E.D.; Brage, S.; White, T.; Westgate, K.; Norris, S.A.; Van Poppel, M.N.M.; Micklesfield, L.K. The Influence of Objectively Measured Physical Activity During Pregnancy on Maternal and Birth Outcomes in Urban Black South African Women. Matern. Child Health J. 2018, 22, 1190–1199. [Google Scholar] [CrossRef]
- Watson, E.D.; Van Poppel, M.N.M.; Jones, R.A.; Norris, A.S.; Micklesfield, L.K. Are South African Mothers Moving? Patterns and Correlates of Physical Activity and Sedentary Behavior in Pregnant Black South African Women. J. Phys. Act. Health 2017, 14, 329–335. [Google Scholar] [CrossRef]
- Simmons, D.; Devlieger, R.; Van Assche, A.; Jans, G.; Galjaard, S.; Corcoy, R.; Adelantado, J.M.; Dunne, F.; Desoye, G.; Harreiter, J.; et al. Effect of Physical Activity and/or Healthy Eating on GDM Risk: The DALI Lifestyle Study. J. Clin. Endocrinol. Metab. 2016, 102, 903–913. [Google Scholar] [CrossRef]
- Hesketh, K.R.; Evenson, K.R.; Stroo, M.; Clancy, S.M.; Østbye, T.; Benjamin-Neelon, S.E. Physical activity and sedentary behavior during pregnancy and postpartum, measured using hip and wrist-worn accelerometers. Prev. Med. Rep. 2018, 10, 337–345. [Google Scholar] [CrossRef] [PubMed]
- Pereira, M.A.; Rifas-Shiman, S.L.; Kleinman, K.P.; Rich-Edwards, J.W.; Peterson, K.E.; Gillman, M.W. Predictors of Change in Physical Activity During and After Pregnancy: Project Viva. Am. J. Prev. Med. 2007, 32, 312–319. [Google Scholar] [CrossRef]
- Thompson, E.L.; Vamos, C.A.; Daley, E.M. Physical activity during pregnancy and the role of theory in promoting positive behavior change: A systematic review. J. Sport Health Sci. 2017, 6, 198–206. [Google Scholar] [CrossRef]
- Harrison, A.L.; Taylor, N.F.; Shields, N.; Frawley, H.C. Attitudes, barriers and enablers to physical activity in pregnant women: A systematic review. J. Physiother. 2018, 64, 24–32. [Google Scholar] [CrossRef] [PubMed]
- Jelsma, J.G.M.; van Leeuwen, K.; Oostdam, N.; Bunn, C.; Simmons, D.; Desoye, G.; Corcoy, R.; Adelantado, J.M.; Kautzky-Willer, A.; Harreiter, J.; et al. Beliefs, Barriers, and Preferences of European Overweight Women to Adopt a Healthier Lifestyle in Pregnancy to Minimize Risk of Developing Gestational Diabetes Mellitus: An Explorative Study. J. Pregnancy 2016, 2016, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Evenson, K.R.; Aytur, S.A.; Borodulin, K. Physical activity beliefs, barriers, and enablers among postpartum women. J. Womens Health 2009, 18, 1925–1934. [Google Scholar] [CrossRef] [PubMed]
- Watson, E.D.; Norris, S.A.; Draper, C.E.; Jones, R.A.; van Poppel, M.N.M.; Micklesfield, L.K. “Just because you’re pregnant, doesn’t mean you’re sick!” A qualitative study of beliefs regarding physical activity in black South African women. BMC Pregnancy Childbirth 2016, 16, 174. [Google Scholar] [CrossRef] [PubMed]
- Coll, C.; Domingues, M.; Santos, I.; Matijasevich, A.; Horta, B.L.; Hallal, P.C. Changes in Leisure-Time Physical Activity from the Prepregnancy to the Postpartum Period: 2004 Pelotas (Brazil) Birth Cohort Study. J. Phys. Act. Health 2016, 13, 361–365. [Google Scholar] [CrossRef]
- Clarke, P.E.; Gross, H. Women’s behaviour, beliefs and information sources about physical exercise in pregnancy. Midwifery 2004, 20, 133–141. [Google Scholar] [CrossRef]
- Findley, A.; Smith, D.M.; Hesketh, K.; Keyworth, C. Exploring womens’ experiences and decision making about physical activity during pregnancy and following birth: A qualitative study. BMC Pregnancy Childbirth 2020, 20, 1–10. [Google Scholar] [CrossRef] [PubMed]
- McParlin, C.; Bell, R.; Robson, S.C.; Muirhead, C.; Araújo-Soares, V. What helps or hinders midwives to implement physical activity guidelines for obese pregnant women? A questionnaire survey using the Theoretical Domains Framework. Midwifery 2017, 49, 110–116. [Google Scholar] [CrossRef]
- Bartholomew, L.K.; Parcel, G.S.; Kok, G.; Gottlieb, N.H.; Schaalma, H.C.; Markham, C.C.; Tyrrell, S.C.; Shegog, R.C.; Fernández, M.C.; Mullen, P.D.C.; et al. Planning Health Promotion Programs: An Intervention Mapping Approach, 2nd ed.; Jossey Bass: San Francisco, CA, USA, 2006. [Google Scholar]
- Craig, P.; Dieppe, P.; Macintyre, S.; Michie, S.; Nazareth, I.; Petticrew, M. Medical Research Council: Developing and evaluating complex interventions: New guidance. Br. Med. J. 2008, 337, a1655. [Google Scholar] [CrossRef]
- Taylor, N.; Conner, M.; Lawton, R. The impact of theory on the effectiveness of worksite physical activity interventions: A meta-analysis and meta-regression. Health Psychol. Rev. 2012, 6, 33–73. [Google Scholar] [CrossRef]
- Bartholomew, L.K.; Parcel, G.S.; Kok, G.; Gottlieb, N.H.; Fernández, M.E. Planning Health Promotion Programs: An Intervention Mapping Approach, 3rd ed.; Jossey-Bass: San Francisco, CA, USA, 2011. [Google Scholar]
- Hoffmann, T.C.; Glasziou, P.P.; Boutron, I.; Milne, R.; Perera, R.; Moher, D.; Altman, D.G.; Barbour, V.; Macdonald, H.; Johnston, M.; et al. Better reporting of interventions: Template for intervention description and replication (TIDieR) checklist and guide. BMJ 2014, 348, g1687. [Google Scholar] [CrossRef]
- Watson, E.D.; Oddie, B.; Constantinou, D. Exercise during pregnancy: Knowledge and beliefs of medical practitioners in South Africa: A survey study. BMC Pregnancy Childbirth 2015, 15, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Cane, J.; O’Connor, D.; Michie, S. Validation of the theoretical domains framework for use in behaviour change and implementation research. Implement. Sci. 2012, 7, 37. [Google Scholar] [CrossRef] [PubMed]
- Michie, S.; Richardson, M.; Johnston, M.; Abraham, C.; Francis, J.; Hardeman, W.; Eccles, M.P.; Cane, J.; Wood, C.E. The Behavior Change Technique Taxonomy (v1) of 93 Hierarchically Clustered Techniques: Building an International Consensus for the Reporting of Behavior Change Interventions. Ann. Behav. Med. 2013, 46, 81–95. [Google Scholar] [CrossRef] [PubMed]
- Johnston, M.; Carey, R.N.; Bohlen, L.E.C.; Johnston, D.W.; Rothman, A.J.; De Bruin, M.; Kelly, M.P.; Groarke, H.; Michie, S. Development of an online tool for linking behavior change techniques and mechanisms of action based on triangulation of findings from literature synthesis and expert consensus). Transl. Behav. Med. 2020. [Google Scholar] [CrossRef] [PubMed]
- Bundesminister für soziale Sicherheit und Generationen. Verordnung des Bundesministers für soziale Sicherheit und Generationen über die Festlegung eines Mutter-Kind-Pass-Untersuchungsprogrammes, die Voraussetzungen zur Weitergewährung des Kinderbetreuungsgeldes in voller Höhe sowie über den Mutter-Kind-Pass Austria. 2002. Available online: https://www.ris.bka.gv.at/GeltendeFassung/Bundesnormen/20001694/MuKiPassV%2CFassungvom.pdf (accessed on 23 November 2020).
- Wilford, A.; Phakathi, S.; Haskins, L.; Jama, N.A.; Mntambo, N.; Horwood, C. Exploring the care provided to mothers and children by community health workers in South Africa: Missed opportunities to provide comprehensive care. BMC Public Health 2018, 18, 171. [Google Scholar] [CrossRef]
- Le Roux, K.; Le Roux, I.M.; Mbewu, N.; Davis, E. The role of community health workers in the re-engineering of primary health care in rural eastern cape. South Afr. Fam. Pract. 2015, 57, 116–120. [Google Scholar] [CrossRef]
- Daviaud, E.; Nkonki, L.; Ijumba, P.; Doherty, T.; Lawn, E.J.; Owen, H.; Jackson, D.; Tomlinson, M. South-Africa (Goodstart III) trial: Community-based maternal and newborn care economic analysis. Health Policy Plan. 2017, 32, i53–i63. [Google Scholar] [CrossRef] [PubMed]
- Bosire, E.N.; Ware, L.J.; Draper, C.E.; Amato, B.; Kapueja, L.; Lye, S.; Norris, S.A. Young women’s perceptions of life in urban South Africa: Contextualising the preconception knowledge gap. Afr. J. Reprod. Health 2021, 25, 39–49. [Google Scholar]
- Coll, C.V.; Domingues, M.R.; Gonçalves, H.; Bertoldi, A.D. Perceived barriers to leisure-time physical activity during pregnancy: A literature review of quantitative and qualitative evidence. J. Sci. Med. Sport 2017, 20, 17–25. [Google Scholar] [CrossRef]
- Alvis, M.L.; Morris, C.E.; Garrard, T.L.; Hughes, A.G.; Hunt, L.; Koester, M.M.; Yocum, I.C.; Tinius, R.A. Educational Brochures Influence Beliefs and Knowledge Regarding Exercise during Pregnancy: A Pilot Study. Int. J. Exerc. Sci. 2019, 12, 581–589. [Google Scholar] [PubMed]
- Stengel, M.R.; Kraschnewski, J.L.; Hwang, S.W.; Kjerulff, K.H.; Chuang, C.H. “What My Doctor Didn’t Tell Me”: Examining Health Care Provider Advice to Overweight and Obese Pregnant Women on Gestational Weight Gain and Physical Activity. Women’s Health Issues 2012, 22, e535–e540. [Google Scholar] [CrossRef] [PubMed]
- Santo, E.C.; Forbes, P.W.; Oken, E.; Belfort, M.B. Determinants of physical activity frequency and provider advice during pregnancy. BMC Pregnancy Childbirth 2017, 17, 286. [Google Scholar] [CrossRef] [PubMed]
- Van der Pligt, P.; Olander, E.K.; Ball, K.; Crawford, D.; Hesketh, K.D.; Teychenne, M.; Campbell, K. Maternal dietary intake and physical activity habits during the postpartum period: Associations with clinician advice in a sample of Australian first time mothers. BMC Pregnancy Childbirth 2016, 16, 27. [Google Scholar] [CrossRef] [PubMed]
- Ferrari, R.M.; Siega-Riz, A.M.; Evenson, K.R.; Moos, M.-K.; Carrier, K.S. A qualitative study of women’s perceptions of provider advice about diet and physical activity during pregnancy. Patient Educ. Couns. 2013, 91, 372–377. [Google Scholar] [CrossRef]
- Currie, S.; Sinclair, M.; Murphy, M.H.; Madden, E.; Dunwoody, L.; Liddle, D. Reducing the Decline in Physical Activity during Pregnancy: A Systematic Review of Behaviour Change Interventions. PLoS ONE 2013, 8, e66385. [Google Scholar] [CrossRef]
- Pearce, E.E.; Evenson, K.R.; Downs, D.S.; Steckler, A. Strategies to Promote Physical Activity during Pregnancy. Am. J. Lifestyle Med. 2013, 7, 38–50. [Google Scholar] [CrossRef] [PubMed]
- National Institute for Health and Care Excellence (NICE). Weight Management before, during and after Pregnancy (PH27); Public Health Guideline: London, UK, 2010. [Google Scholar]
- World Health Organisation. WHO Recommendation on Antenatal Care for Positive Pregnancy Experience; World Health Organisation: Geneva, Switzerland, 2016. [Google Scholar]
- Leiferman, J.; Gutilla, M.; Paulson, J.; Pivarnik, J. Antenatal physical activity counseling among healthcare providers. Open J. Obstet. Gynecol. 2012, 02, 346–355. [Google Scholar] [CrossRef]
- McGee, L.D.; Cignetti, A.C.; Sutton, A.; Harper, L.; Dubose, C.; Gould, S. Exercise During Pregnancy: Obstetricians’ Beliefs and Recommendations Compared to American Congress of Obstetricians and Gynecologists’ 2015 Guidelines. Cureus 2018, 10, e3204. [Google Scholar] [CrossRef]
- Hopkinson, Y.; Hill, D.M.; Fellows, L.; Fryer, S. Midwives understanding of physical activity guidelines during pregnancy. Midwifery 2018, 59, 23–26. [Google Scholar] [CrossRef]
- Hayman, M.; Reaburn, P.; Alley, S.; Cannon, S.; Short, C. What exercise advice are women receiving from their healthcare practitioners during pregnancy? Women Birth 2020, 33, e357–e362. [Google Scholar] [CrossRef] [PubMed]
- Entin, P.L.; Munhall, K.M. Recommendations regarding exercise during pregnancy made by private/small group practice obstetricians in the USA. J. Sports Sci. Med. 2006, 5, 449–458. [Google Scholar] [PubMed]
- Flannery, C.; McHugh, S.; Anaba, A.E.; Clifford, E.; O’Riordan, M.; Kenny, L.C.; McAuliffe, F.M.; Kearney, P.M.; Byrne, M. Enablers and barriers to physical activity in overweight and obese pregnant women: An analysis informed by the theoretical domains framework and COM-B model. BMC Pregnancy Childbirth 2018, 18, 1–13. [Google Scholar] [CrossRef]
- De Vivo, M.; Mills, H. “They turn to you first for everything”: Insights into midwives’ perspectives of providing physical activity advice and guidance to pregnant women. BMC Pregnancy Childbirth 2019, 19, 462. [Google Scholar] [CrossRef]
- Bauer, P.W.; Broman, C.L.; Pivarnik, J.M. Exercise and Pregnancy Knowledge among Healthcare Providers. J. Women’s Health 2010, 19, 335–341. [Google Scholar] [CrossRef]
- Evenson, K.R.; Pompeii, L.A. Obstetrician Practice Patterns and Recommendations for Physical Activity during Pregnancy. J. Women’s Health 2010, 19, 1733–1740. [Google Scholar] [CrossRef]
- Crampton, J.S.; O’Brien, S.; Heathcote, K. Recreational exercise during pregnancy: Attitudes and beliefs of midwives and physiotherapists. Br. J. Midwifery 2018, 26, 455–461. [Google Scholar] [CrossRef]
- Lindqvist, M.; Mogren, I.; Eurenius, E.; Edvardsson, K.; Persson, M. “An on-going individual adjustment”: A qualitative study of midwives’ experiences counselling pregnant women on physical activity in Sweden. BMC Pregnancy Childbirth 2014, 14, 343. [Google Scholar] [CrossRef] [PubMed]
- McLellan, J.M.; O’Carroll, R.E.; Cheyne, H.; Dombrowski, S.U. Investigating midwives’ barriers and facilitators to multiple health promotion practice behaviours: A qualitative study using the theoretical domains framework. Implement. Sci. 2019, 14, 1–10. [Google Scholar] [CrossRef]
- Muzigaba, M.; Kolbe-Alexander, T.L.; Wong, F. The Perceived Role and Influencers of Physical Activity among Pregnant Women From Low Socioeconomic Status Communities in South Africa. J. Phys. Act. Health 2014, 11, 1276–1283. [Google Scholar] [CrossRef]
- Forsetlund, L.; Bjørndal, A.; Rashidian, A.; Jamtvedt, G.; O’Brien, M.A.; Wolf, F.M.; Davis, D.; Odgaard-Jensen, J.; Oxman, A.D. Continuing education meetings and workshops: Effects on professional practice and health care outcomes. Cochrane Database Syst. Rev. 2009, 2009, CD003030. [Google Scholar] [CrossRef]
- Miller, W.R.; Rollnick, S. Motivational Interviewing: Preparing People to Change Addictive Behaviours; Guilford Press: New York, NY, USA, 1991. [Google Scholar]
- Giguère, A.; Zomahoun, H.T.V.; Carmichael, P.-H.; Uwizeye, C.B.; Légaré, F.; Grimshaw, J.; Gagnon, M.-P.; Auguste, D.U.; Massougbodji, J. Printed educational materials: Effects on professional practice and healthcare outcomes. Cochrane Database Syst. Rev. 2020. [Google Scholar] [CrossRef]
- Huijg, J.M.; A Gebhardt, W.; Crone, M.R.; Dusseldorp, E.; Presseau, J. Discriminant content validity of a theoretical domains framework questionnaire for use in implementation research. Implement. Sci. 2014, 9, 11. [Google Scholar] [CrossRef]
- Linnan, L.; Steckler, A. Process evaluation for public health interventions and research: An overview. In Process Evaluation for Public Health Interventions and Research; Jossey-Bass: San Francisco, CA, USA, 2002. [Google Scholar]
- Johnson, M.J.; May, C.R. Promoting professional behaviour change in healthcare: What interventions work, and why? A theory-led overview of systematic reviews. BMJ Open 2015, 5, e008592. [Google Scholar] [CrossRef]
- Keyworth, C.; Epton, T.; Goldthorpe, J.; Calam, R.; Armitage, C.J. Delivering Opportunistic Behavior Change Interventions: A Systematic Review of Systematic Reviews. Prev. Sci. 2020, 21, 319–331. [Google Scholar] [CrossRef]
- Huijg, J.M.; Gebhardt, W.A.; Verheijden, M.W.; Van Der Zouwe, N.; De Vries, J.D.; Middelkoop, B.J.C.; Crone, M.R. Factors Influencing Primary Health Care Professionals’ Physical Activity Promotion Behaviors: A Systematic Review. Int. J. Behav. Med. 2014, 22, 32–50. [Google Scholar] [CrossRef]
- Weiler, R.; Chew, S.; Coombs, N.; Hamer, M.; Stamatakis, E. Physical activity education in the undergraduate curricula of all UK medical schools. Are tomorrow’s doctors equipped to follow clinical guidelines? Br. J. Sports Med. 2012, 46, 1024–1026. [Google Scholar] [CrossRef]
- Lawrence, W.; Black, C.; Tinati, T.; Cradock, S.; Begum, R.; Jarman, M.; Pease, A.; Margetts, B.; Davies, J.; Inskip, H.; et al. ‘Making every contact count’: Evaluation of the impact of an intervention to traiAn health and social care practitioners in skills to support health behaviour change. J. Health Psychol. 2016, 21, 138–151. [Google Scholar] [CrossRef]
- Brug, J.; Oenema, A.; Ferreira, I. Theory, evidence and Intervention Mapping to improve behavior nutrition and physical activity interventions. Int. J. Behav. Nutr. Phys. Act. 2005, 2, 2. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).