Smart City and High-Tech Urban Interventions Targeting Human Health: An Equity-Focused Systematic Review
Abstract
1. Introduction
2. History of Smart Cities
2.1. Smart Cities and Public Health
2.2. Equity and Smart Cities
3. Materials and Methods
3.1. Current State of Reviews and Justification
3.2. Review Question and Objectives
3.3. Search Strategy
3.4. Eligibility Criteria
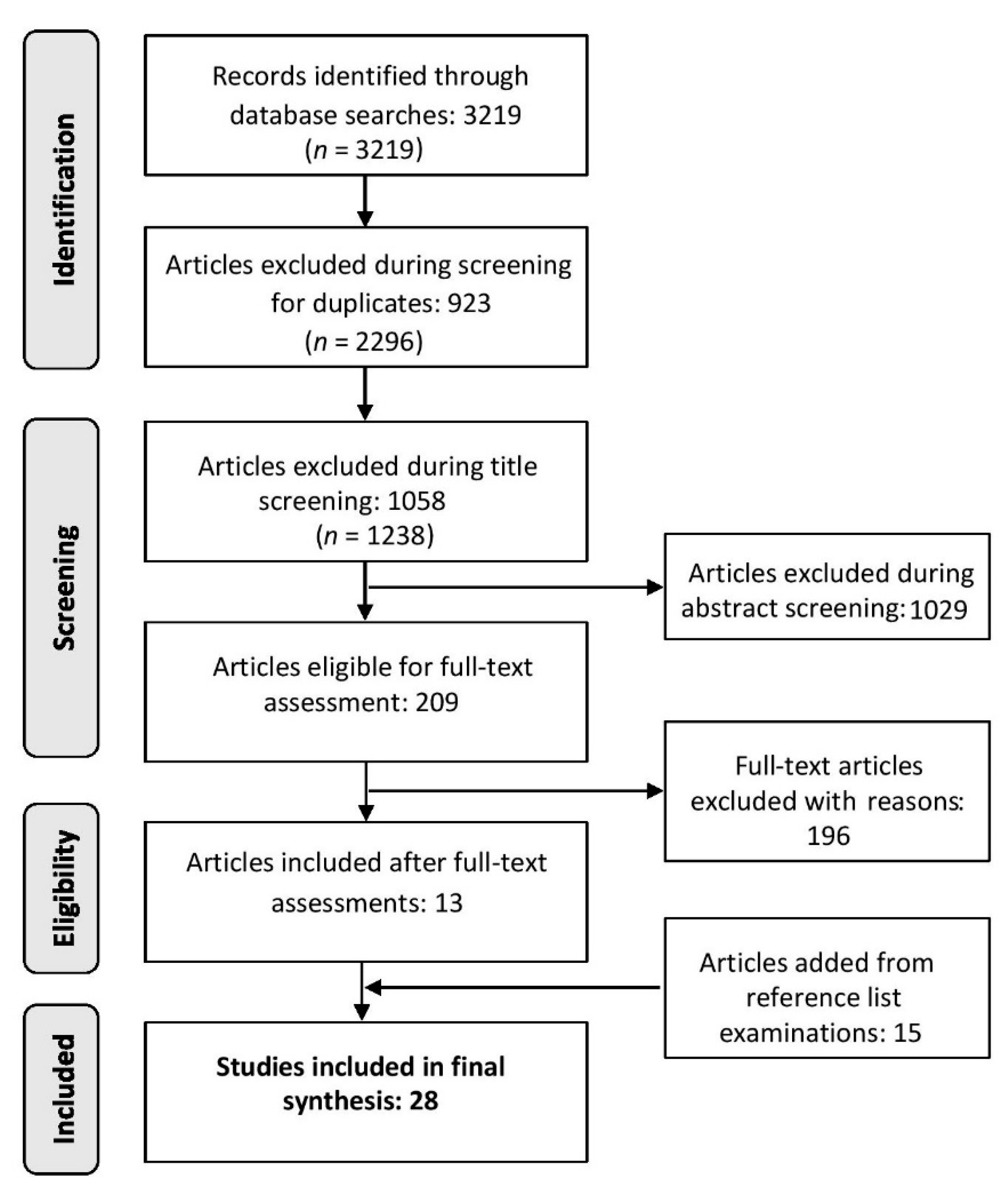
3.5. Study Selection and Review Process
3.6. Data Extraction
3.7. Quality Assessment and Risk of Bias in Individual Studies
4. Results
4.1. General Characteristics of Included Articles
4.2. Place of Residence
4.3. Race, Ethnicity, Culture, Language
4.4. Occupation
4.5. Sex and Gender
4.6. Religion
4.7. Education
4.8. Socioeconomic Status
4.9. Social Capital
4.10. Personal Characteristics
5. Discussion
5.1. Implications for Practice and Policy
5.2. Limitations
5.3. Recommendations for Future Research
6. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Giles-Corti, B.; Vernez-Moudon, A.; Reis, R.; Turrell, G.; Dannenberg, A.L.; Badland, H.; Foster, S.; Lowe, M.; Sallis, J.F.; Stevenson, M.; et al. City Planning and Population Health: A Global Challenge. Lancet 2016, 388, 2912–2924. [Google Scholar] [CrossRef]
- World Health Organization; United Nations. Hidden Cities: Unmasking and Overcoming Health Inequities in Urban Settings; World Health Organization: Geneva, Switzerland, 2010. [Google Scholar]
- United Nations, Department of Economic and Social Affairs. World Urbanization Prospects: The 2014 Revision; United Nations, Department of Economic and Social Affairs: New York, NY, USA, 2014. [Google Scholar]
- United Nations, Department of Economic and Social Affairs, Population Division. World Urbanization Prospects—Population Division—United Nations. Available online: https://population.un:wup/ (accessed on 8 October 2019).
- Davidson, M. Sustainability as Ideological Praxis: The Acting out of Planning’s Master-signifier. City 2010, 14, 390–405. [Google Scholar] [CrossRef]
- Stratigea, A.; Leka, A.; Panagiotopoulou, M. In Search of Indicators for Assessing Smart and Sustainable Cities and Communities’ Performance. Int. J. E Plan. Res. 2017, 6, 43–73. [Google Scholar] [CrossRef]
- Trencher, G.; Karvonen, A. Stretching “Smart”: Advancing Health and Well-Being through the Smart City Agenda. Local Environ. 2017, 1–18. [Google Scholar] [CrossRef]
- Kummitha, R.K.R.; Crutzen, N. How Do We Understand Smart Cities? An Evolutionary Perspective. Cities 2017, 67, 43–52. [Google Scholar] [CrossRef]
- Trencher, G. Towards the Smart City 2.0: Empirical Evidence of Using Smartness as a Tool for Tackling Social Challenges. Technol. Forecast. Soc. Chang. 2018, 142, 117–128. [Google Scholar] [CrossRef]
- Schumacher, J.; Feurstein, K. Living Labs—The User as Co-Creator. In Proceedings of the 2007 IEEE International Technology Management Conference (ICE), Sophia Antipolis, France, 4–6 June 2007; pp. 1–6. [Google Scholar]
- Hodson, M.; Marvin, S. Intensifying or Transforming Sustainable Cities? Fragmented Logics of Urban Environmentalism. Local Environ. 2017, 22 (Suppl. 1), 8–22. [Google Scholar] [CrossRef]
- Martin, C.; Evans, J.; Karvonen, A. Smart and Sustainable? Five Tensions in the Visions and Practices of the Smart-Sustainable City in Europe and North America. Technol. Forecast. Soc. Chang. 2018, 133, 269–278. [Google Scholar] [CrossRef]
- Crowley, M.; Nutter, M.; Wheeler, C.; Schuetz, N.; Lamberg, R.; Bent, E. Smart Cities for Sustainability—A Sector by Sector Review—U.S. Local Solutions; U.S. Urban Solutions: Washington, DC, USA, 2016; pp. 1–85. [Google Scholar]
- Calzada, I.; Cobo, C. Unplugging: Deconstructing the Smart City. J. Urban Technol. 2015, 22, 23–43. [Google Scholar] [CrossRef]
- Nomura, A.T.G.; Pruinelli, L.; da Silva, M.B.; de Fátima Lucena, A.; de Abreu Almeida, M. Quality of Electronic Nursing Records: The Impact of Educational Interventions During a Hospital Accreditation Process. Comput. Inf. Nurs. 2018, 36, 127–132. [Google Scholar] [CrossRef]
- Baccarne, B.; Mechant, P.; Schuurman, D.; Colpaert, P.; De Marez, L. Urban Socio-Technical Innovations with and by Citizens. Interdiscip. Stud. J. 2014, 3, 143–156. [Google Scholar]
- De Lange, M.; De Waal, M. Owning the City: New Media and Citizen Engagement in Urban Design. First Monday 2013, 18. [Google Scholar] [CrossRef]
- Kitchin, R. The Real-Time City? Big Data and Smart Urbanism. GeoJournal 2014, 79, 1–14. [Google Scholar] [CrossRef]
- Saunders, T.; Baeck, P. Rethinking Smart Cities from the Ground Up; Nesta: London, UK, 2015; pp. 1–72. [Google Scholar]
- Almirall, E.; Wareham, J.; Ratti, C.; Conesa, P.; Bria, F.; Gaviria, A.; Edmondson, A. Smart Cities at the Crossroads: New Tensions in City Transformation. Calif. Manag. Rev. 2016, 59, 141–152. [Google Scholar] [CrossRef]
- Capdevila, I.; Zarlenga, M.I. Smart City or Smart Citizens? The Barcelona Case. J. Strateg. Manag. Bingley 2015, 8, 266–282. [Google Scholar] [CrossRef]
- Goodspeed, R. Smart Cities: Moving beyond Urban Cybernetics to Tackle Wicked Problems. Camb. J. Reg. Econ. Soc. 2015, 8, 79–92. [Google Scholar] [CrossRef]
- McFarlane, C.; Söderström, O. On Alternative Smart Cities. City 2017, 21, 312–328. [Google Scholar] [CrossRef]
- Badland, H.; Whitzman, C.; Lowe, M.; Davern, M.; Aye, L.; Butterworth, I.; Hes, D.; Giles-Corti, B. Urban Liveability: Emerging Lessons from Australia for Exploring the Potential for Indicators to Measure the Social Determinants of Health. Soc. Sci. Med. 2014, 111, 64–73. [Google Scholar] [CrossRef]
- Murray, C.J.L.; Vos, T.; Lozano, R.; Naghavi, M.; Flaxman, A.D.; Michaud, C.; Ezzati, M.; Shibuya, K.; Salomon, J.A.; Abdalla, S.; et al. Disability-Adjusted Life Years (DALYs) for 291 Diseases and Injuries in 21 Regions, 1990–2010: A Systematic Analysis for the Global Burden of Disease Study 2010. Lancet 2012, 380, 2197–2223. [Google Scholar] [CrossRef]
- Watts, N.; Adger, W.N.; Agnolucci, P.; Blackstock, J.; Byass, P.; Cai, W.; Chaytor, S.; Colbourn, T.; Collins, M.; Cooper, A.; et al. Health and Climate Change: Policy Responses to Protect Public Health. Lancet 2015, 386, 1861–1914. [Google Scholar] [CrossRef]
- Kamel Boulos, M.N.; Tsouros, A.D.; Holopainen, A. “Social, Innovative and Smart Cities Are Happy and Resilient”: Insights from the WHO EURO 2014 International Healthy Cities Conference. Int. J. Health Geogr. 2015, 14, 3. [Google Scholar] [CrossRef] [PubMed]
- Flores Mateo, G.; Granado-Font, E.; Ferré-Grau, C.; Montaña-Carreras, X. Mobile Phone Apps to Promote Weight Loss and Increase Physical Activity: A Systematic Review and Meta-Analysis. J. Med. Internet Res. 2015, 17, e253. [Google Scholar] [CrossRef] [PubMed]
- WHO Global Observatory for eHealth; World Health Organization. MHealth: New Horizons for Health through Mobile Technologies; World Health Organization: Geneva, Switzerland, 2011. [Google Scholar]
- Koch, S. Healthy Ageing Supported by Technology—A Cross-Disciplinary Research Challenge. Inf. Health Soc. Care 2010, 35, 81–91. [Google Scholar] [CrossRef] [PubMed]
- Obi, T.; Ishmatova, D.; Iwasaki, N. Promoting ICT Innovations for the Ageing Population in Japan. Int. J. Med. Inf. 2013, 82, e47–e62. [Google Scholar] [CrossRef] [PubMed]
- Pfaeffli Dale, L.; Dobson, R.; Whittaker, R.; Maddison, R. The Effectiveness of Mobile-Health Behaviour Change Interventions for Cardiovascular Disease Self-Management: A Systematic Review. Eur. J. Prev. Cardiol. 2016, 23, 801–817. [Google Scholar] [CrossRef] [PubMed]
- Schippers, M.; Adam, P.C.G.; Smolenski, D.J.; Wong, H.T.H.; de Wit, J.B.F. A Meta-Analysis of Overall Effects of Weight Loss Interventions Delivered via Mobile Phones and Effect Size Differences According to Delivery Mode, Personal Contact, and Intervention Intensity and Duration. Obes. Rev. 2017, 18, 450–459. [Google Scholar] [CrossRef]
- Solanas, A.; Patsakis, C.; Conti, M.; Vlachos, I.S.; Ramos, V.; Falcone, F.; Postolache, O.; Perez-martinez, P.A.; Pietro, R.D.; Perrea, D.N.; et al. Smart Health: A Context-Aware Health Paradigm within Smart Cities. IEEE Commun. Mag. 2014, 52, 74–81. [Google Scholar] [CrossRef]
- Trencher, G.; Karvonen, A. Innovating for an Ageing Society: Insights from Two Japanese Smart Cities. In Inside Smart Cities: Place, Politics, and Urban Innovation; Routledge: New York, NY, USA, 2018; pp. 258–274. [Google Scholar]
- Maye, D. ‘Smart Food City’: Conceptual Relations between Smart City Planning, Urban Food Systems and Innovation Theory. City Cult. Soc. 2017. [Google Scholar] [CrossRef]
- Behrendt, F. Why Cycling Matters for Smart Cities. Internet of Bicycles for Intelligent Transport. J. Transp. Geogr. 2016, 56, 157–164. [Google Scholar] [CrossRef]
- World Health Organization. Commission on Social Determinants of Health—Final Report. Closing the Gap in a Generation: Health Equity through Action on the Social Determinants of Health. Available online: http://www.who.int/social_determinants/thecommission/finalreport/en/ (accessed on 16 May 2019).
- National Institutes of Health. Health Disparities. Available online: https://www.nhlbi.nih.gov/health/educational/healthdisp/index.htm (accessed on 16 May 2019).
- United States Department of Health and Human Services. Healthy People 2010: Final Review; DHHS Publication; U.S. Dept. of Health and Human Services, Centers for Disease Control and Prevention, National Center for Health Statistics: Hyattsville, MD, USA, 2012.
- Woodward, A.; Kawachi, I. Why Reduce Health Inequalities? J. Epidemiol. Community Health 2000, 54, 923–929. [Google Scholar] [CrossRef]
- Wallace, R.; Wallace, D. Socioeconomic Determinants of Health: Community Marginalisation and the Diffusion of Disease and Disorder in the United States. BMJ 1997, 314, 1341–1345. [Google Scholar] [CrossRef] [PubMed]
- Wilson, M.; Daly, M. Life Expectancy, Economic Inequality, Homicide, and Reproductive Timing in Chicago Neighbourhoods. BMJ 1997, 314, 1271–1274. [Google Scholar] [CrossRef] [PubMed]
- Whitehead, M.; Dahlgren, G. Concepts and Principles for Tackling Social Inequities in Health: Levelling up Part 1; World Health Organization: Geneva, Switzerland, 2006; p. 45. [Google Scholar]
- Colding, J.; Barthel, S. An Urban Ecology Critique on the “Smart City” Model. J. Clean. Prod. 2017, 164, 95–101. [Google Scholar] [CrossRef]
- Glasmeier, A.; Christopherson, S. Thinking about Smart Cities. Camb. J. Reg. Econ. Soc. 2015, 8, 3–12. [Google Scholar] [CrossRef]
- Viitanen, J.; Kingston, R. Smart Cities and Green Growth: Outsourcing Democratic and Environmental Resilience to the Global Technology Sector. Environ. Plan. A 2014, 46, 803–819. [Google Scholar] [CrossRef]
- Cardullo, P.; Kitchin, R. Being a ‘Citizen’ in the Smart City: Up and down the Scaffold of Smart Citizen Participation in Dublin, Ireland. GeoJournal 2018, 84, 1–13. [Google Scholar] [CrossRef]
- Hollands, R.G. Critical Interventions into the Corporate Smart City. Camb. J. Reg. Econ. Soc. 2015, 8, 61–77. [Google Scholar] [CrossRef]
- Kitchin, R. Making Sense of Smart Cities: Addressing Present Shortcomings. Camb. J. Reg. Econ. Soc. 2015, 8, 131–136. [Google Scholar] [CrossRef]
- Glasmeier, A.; Nebiolo, M. Thinking about Smart Cities: The Travels of a Policy Idea That Promises a Great Deal, but So Far Has Delivered Modest Results. Sustainability 2016, 8, 1122. [Google Scholar] [CrossRef]
- Hollands, R.G. Will the Real Smart City Please Stand Up? City 2008, 12, 303–320. [Google Scholar] [CrossRef]
- Mouton, M.; Ducey, A.; Green, J.; Hardcastle, L.; Hoffman, S.; Leslie, M.; Rock, M. Towards “smart Cities” as “Healthy Cities”: Health Equity in a Digital Age. Can. J. Public Health 2019. [Google Scholar] [CrossRef] [PubMed]
- Haarstad, H. Constructing the Sustainable City: Examining the Role of Sustainability in the ‘Smart City’ Discourse. J. Environ. Policy Plan. 2017, 19, 423–437. [Google Scholar] [CrossRef]
- Ramaswami, A.; Russell, A.G.; Culligan, P.J.; Sharma, K.R.; Kumar, E. Meta-Principles for Developing Smart, Sustainable, and Healthy Cities. Science 2016, 352, 940–943. [Google Scholar] [CrossRef] [PubMed]
- Ruhlandt, R.W.S. The Governance of Smart Cities: A Systematic Literature Review. Cities 2018, 81, 1–23. [Google Scholar] [CrossRef]
- Trindade, E.P.; Hinnig, M.P.F.; Moreira da Costa, E.; Marques, J.S.; Bastos, R.C.; Yigitcanlar, T. Sustainable Development of Smart Cities: A Systematic Review of the Literature. J. Open Innov. Technol. Market Complex. 2017, 3, 11. [Google Scholar] [CrossRef]
- Safarov, I.; Meijer, A.; Grimmelikhuijsen, S. Utilization of Open Government Data: A Systematic Literature Review of Types, Conditions, Effects and Users. Inf. Polity 2017, 22, 1–24. [Google Scholar] [CrossRef]
- Graham, S.; Marvin, S. Splintering Urbanism: Networked Infrastructures, Technological Mobilities and the Urban Condition; Routledge: London, UK, 2001. [Google Scholar]
- Coutard, O. Placing Splintering Urbanism: Introduction. Geoforum 2008, 39, 1815–1820. [Google Scholar] [CrossRef]
- O’Neill, J.; Tabish, H.; Welch, V.; Petticrew, M.; Pottie, K.; Clarke, M.; Evans, T.; Pardo Pardo, J.; Waters, E.; White, H.; et al. Applying an Equity Lens to Interventions: Using PROGRESS Ensures Consideration of Socially Stratifying Factors to Illuminate Inequities in Health. J. Clin. Epidemiol. 2014, 67, 56–64. [Google Scholar] [CrossRef]
- Petticrew, M.; Roberts, H. Systematic Reviews in the Social Sciences: A Practical Guide; Blackwell Pub: Oxford, UK; Malden, MA, USA, 2006. [Google Scholar]
- Cocchia, A. Smart and Digital City: A Systematic Literature Review. In Smart City: How to Create Public and Economic Value with High Technology in Urban Space; Dameri, R.P., Rosenthal-Sabroux, C., Eds.; Progress in IS; Springer International Publishing: Cham, Switzerland, 2014; pp. 13–43. [Google Scholar] [CrossRef]
- Couclelis, H. The Construction of the Digital City. Environ. Plan. B Plan. Des. 2004, 31, 5–19. [Google Scholar] [CrossRef]
- Bătăgan, L. Smart Cities and Sustainability Models. Rev. Inf. Econ. 2011, 15, 80–87. [Google Scholar]
- Komninos, N. The Architecture of Intelligent Cities: Integrating Human, Collective and Artificial Intelligence to Enhance Knowledge and Innovation. In Proceedings of the 2nd IET International Conference on Intelligent Environments (IE 06), Athens, Greece, 5–6 July 2006; IEE: Athens, Greece, 2006; Volume 6, pp. 53–61. [Google Scholar] [CrossRef]
- Industry Canada. Report of the Panel on Smart Communities; Information Distribution Centre, Communications Branch, Industry Canada: Ottawa, ON, Canada, 1998. [Google Scholar]
- Braveman, P.; Gruskin, S. Defining Equity in Health. J. Epidemiol. Commun. Health 2003, 57, 254–258. [Google Scholar] [CrossRef] [PubMed]
- Cochrane Methods. PROGRESS-Plus. Available online: https://methods.cochrane:equity/projects/evidence-equity/progress-plus (accessed on 16 May 2019).
- Effective Public Health Practice Project. Quality Assessment Tool for Quantitative Studies. Available online: https://merst.ca/wp-content/uploads/2018/02/quality-assessment-tool_2010.pdf (accessed on 29 November 2018).
- Lee, S.H.; Nurmatov, U.B.; Ulugbek, B.; Mome, M.; Grant, L.; Pagliari, C. Effectiveness of MHealth Interventions for Maternal, Newborn and Child Health in Low- and Middle–Income Countries: Systematic Review and Meta–Analysis. J. Glob. Health 2016, 6, 010401. [Google Scholar] [CrossRef]
- National Institute for Health and Care Excellence. Methods for the Development of NICE Public Health Guidance, 3rd ed.; Department of Health: London, UK, 2012. [Google Scholar]
- Oluka, O.C.; Nie, S.; Sun, Y. Quality Assessment of TPB-Based Questionnaires: A Systematic Review. PLoS ONE 2014, 9, e94419. [Google Scholar] [CrossRef] [PubMed]
- Paredes, P.; Ko, R.; Calle-Ortiz, E.; Canny, J.; Hartmann, B.; Niemeyer, G. Fiat-Lux: Interactive Urban Lights for Combining Positive Emotion and Efficiency. In Proceedings of the 2016 ACM Conference on Designing Interactive Systems—DIS ’16, Brisbane, QLD, Australia, 4–8 June 2016; ACM Press: Brisbane, QLD, Australia, 2016; pp. 785–795. [Google Scholar] [CrossRef]
- Howe, K.B.; Suharlim, C.; Ueda, P.; Howe, D.; Kawachi, I.; Rimm, E.B. Gotta Catch’em All! Pokémon GO and Physical Activity among Young Adults: Difference in Differences Study. BMJ 2016, 355. [Google Scholar] [CrossRef] [PubMed]
- Bakolis, I.; Hammoud, R.; Smythe, M.; Gibbons, J.; Davidson, N.; Tognin, S.; Mechelli, A. Urban Mind: Using Smartphone Technologies to Investigate the Impact of Nature on Mental Well-Being in Real Time. BioScience 2018, 68, 134–145. [Google Scholar] [CrossRef] [PubMed]
- Ferrara, E.; Liotta, A.; Erhan, L.; Ndubuaku, M.; Giusto, D.; Richardson, M.; Sheffield, D.; McEwan, K. A Pilot Study Mapping Citizens’ Interaction with Urban Nature. In Proceedings of the 2018 IEEE 16th International Conference on Dependable, Autonomic and Secure Computing, 16th International Conference on Pervasive Intelligence and Computing, 4th International Conference on Big Data Intelligence and Computing and Cyber Science and Technology Congress(DASC/PiCom/DataCom/CyberSciTech), Athens, Greece, 12–15 August 2018; pp. 836–841. [Google Scholar] [CrossRef]
- Hamann, G.A.; Ivtzan, I. 30 Minutes in Nature a Day Can Increase Mood, Well-Being, Meaning in Life and Mindfulness: Effects of a Pilot Programme. Soc. Inq. Well-Being 2016, 2, 34–46. [Google Scholar] [CrossRef]
- MacKerron, G.; Mourato, S. Happiness Is Greater in Natural Environments. Glob. Environ. Chang. 2013, 23, 992–1000. [Google Scholar] [CrossRef]
- McEwan, K.; Richardson, M.; Brindley, P.; Sheffield, D.; Tait, C.; Johnson, S.; Sutch, H.; Ferguson, F.J. Shmapped: Development of an App to Record and Promote the Well-Being Benefits of Noticing Urban Nature. Transl. Behav. Med. 2019. [Google Scholar] [CrossRef]
- Isaac, N.; Sampath, N.; Gay, V. Modernising Asthma Management: Personalised Asthma Action Plans Using a Smartphone Application. In Proceedings of the 2018 12th International Symposium on Medical Information and Communication Technology (ISMICT), Sydney, Australia, 26–28 March 2018; pp. 1–5. [Google Scholar] [CrossRef]
- Krome, S.; Holopainen, J.; Greuter, S. AutoGym: An Exertion Game for Autonomous Driving. In Proceedings of the Annual Symposium on Computer-Human Interaction in Play; ACM: New York, NY, USA, 2017; pp. 33–42. [Google Scholar] [CrossRef]
- Martin, M.; Geiger, F.; Götz, M.; Beeh, T.; Sosnowski, M.; Keppner, M.; Aslan, I.; Bittner, B.; André, E. Traeddy: A Stress Sensitive Traffic Jam Companion for Car Commuters. In Proceedings of the Workshop on Human-Habitat for Health (H3), Boulder, CO, USA, 16 October 2018. [Google Scholar] [CrossRef]
- Paredes, P.; Zhou, Y.; Hamdan, N.A.; Balters, S.; Murnane, E.L.; Ju, W.; Landay, J.A. Just Breathe: In-Car Interventions for Guided Slow Breathing. IMWUT 2018, 2, 28. [Google Scholar] [CrossRef]
- Pichlmair, M.; Brandt, C.; Henrich, M.; Biederer, A.; Aslan, I.; Bittner, B.; André, E. Pen-Pen: A Wellbeing Design to Help Commuters Rest and Relax. In Proceedings of the Workshop on Human-Habitat for Health (H3) Human-Habitat Multimodal Interaction for Promoting Health and Well-Being in the Internet of Things Era—H3’18, Boulder, CO, USA, 16 October 2018; ACM Press: Boulder, CO, USA, 2018; pp. 1–9. [Google Scholar] [CrossRef]
- Terken, Z.; Haex, R.; Beursgens, L.; Arslanova, E.; Vrachni, M.; Terken, J.; Szostak, D. Unwinding after Work: An in-Car Mood Induction System for Semi-Autonomous Driving. In Proceedings of the 5th International Conference on Automotive User Interfaces and Interactive Vehicular Applications—AutomotiveUI’13, Eindhoven, The Netherlands, 27–30 October 2013; ACM Press: Eindhoven, The Netherlands, 2013; pp. 246–249. [Google Scholar] [CrossRef]
- Nigg, C.R.; Mateo, D.J.; An, J. Pokémon GO May Increase Physical Activity and Decrease Sedentary Behaviors. Am. J. Public Health 2017, 107, 37–38. [Google Scholar] [CrossRef]
- Klakegg, S.; van Berkel, N.; Visuri, A.; Luo, C.; Goncalves, J.; Hosio, S.; Huttunen, H.-L.; Ferreira, D. Informing Caregivers Through an Assistive Tool: An Investigation of Elderly Care Metrics. In Proceedings of the 31st British Computer Society Human Computer Interaction Conference, Sunderland, UK, 3–6 July 2017. [Google Scholar] [CrossRef]
- Tewell, J.; O’Sullivan, D.; Maiden, N.; Lockerbie, J.; Stumpf, S. Monitoring Meaningful Activities Using Small Low-Cost Devices in a Smart Home. Pers. Ubiquit. Comput. 2019, 23, 339–357. [Google Scholar] [CrossRef]
- Althoff, T.; White, R.W.; Horvitz, E. Influence of Pokémon Go on Physical Activity: Study and Implications. J. Med. Internet Res. 2016, 18, e315. [Google Scholar] [CrossRef] [PubMed]
- Ruiz-Ariza, A.; Casuso, R.A.; Suarez-Manzano, S.; Martínez-López, E.J. Effect of Augmented Reality Game Pokémon GO on Cognitive Performance and Emotional Intelligence in Adolescent Young. Comput. Educ. 2018, 116, 49–63. [Google Scholar] [CrossRef]
- Davis, K.; Owusu, E.B.; Marcenaro, L.; Feijs, L.; Regazzoni, C.; Hu, J. Effects of Ambient Lighting Displays on Peripheral Activity Awareness. IEEE Access 2017, 5, 9318–9335. [Google Scholar] [CrossRef]
- Lane, N.D.; Lin, M.; Mohammod, M.; Yang, X.; Lu, H.; Cardone, G.; Ali, S.; Doryab, A.; Berke, E.; Campbell, A.T.; et al. BeWell: Sensing Sleep, Physical Activities and Social Interactions to Promote Wellbeing. Mob. Netw. Appl. 2014, 19, 345–359. [Google Scholar] [CrossRef]
- Frey, J.; Grabli, M.; Slyper, R.; Cauchard, J. Breeze: Sharing Biofeedback through Wearable Technologies. In Proceedings of the 2018 CHI Conference on Human Factors in Computing Systems—CHI’18, Montreal, QC, Canada, 21–26 April 2018; pp. 1–12. [Google Scholar] [CrossRef]
- Martindale, S.; Bedwell, B.; Phillips, R.; Pedros, M. “Proof in the Pudding”: Designing IoT Plants to Promote Wellbeing. In Proceedings of the 2017 Conference on Designing Interactive Systems (DIS ’17), Edinburgh, UK, 10–14 June 2017; ACM: New York, NY, USA, 2017; pp. 529–540. [Google Scholar] [CrossRef]
- Nef, T.; Urwyler, P.; Büchler, M.; Tarnanas, I.; Stucki, R.; Cazzoli, D.; Müri, R.; Mosimann, U. Evaluation of Three State-of-the-Art Classifiers for Recognition of Activities of Daily Living from Smart Home Ambient Data. Sensors 2015, 15, 11725–11740. [Google Scholar] [CrossRef]
- Amiri, A.M.; Peltier, N.; Goldberg, C.; Sun, Y.; Nathan, A.; Hiremath, S.V.; Mankodiya, K. WearSense: Detecting Autism Stereotypic Behaviors through Smartwatches. Healthcare 2017, 5, 11. [Google Scholar] [CrossRef]
- Gutiérrez García, M.A.; Martín Ruiz, M.L.; Rivera, D.; Vadillo, L.; Valero Duboy, M.A. A Smart Toy to Enhance the Decision-Making Process at Children’s Psychomotor Delay Screenings: A Pilot Study. J. Med. Internet Res. 2017, 19. [Google Scholar] [CrossRef]
- Yang, S.; Gao, B.; Jiang, L.; Jin, J.; Gao, Z.; Ma, X.; Woo, W.L. IoT Structured Long-Term Wearable Social Sensing for Mental Wellbeing. IEEE Internet Things J. 2019, 6, 3652–3662. [Google Scholar] [CrossRef]
- Park, S.; Kim, J.Y.; Lee, J.C.; Kim, H.R.; Song, S.; Kwon, H.; Ji, W.; Choi, C.M. Mobile Phone App–Based Pulmonary Rehabilitation for Chemotherapy-Treated Patients with Advanced Lung Cancer: Pilot Study. JMIR Mhealth Uhealth 2019, 7. [Google Scholar] [CrossRef]
- Gilchrist, A. The Well-Connected Community: A Networking Approach to Community Development, 3rd ed.; Policy Press: Bristol, UK, 2019. [Google Scholar]
- Government of Canada, Statistics Canada. Geographic Distribution of Immigrants and Recent Immigrants and Their Proportion within the Population of Census Metropolitan Areas, Canada. 2016. Available online: https://www150.statcan.gc.ca/n1/daily-quotidien/171025/t001b-eng.htm (accessed on 3 October 2019).
- Kirmayer, L.J.; Narasiah, L.; Munoz, M.; Rashid, M.; Ryder, A.G.; Guzder, J.; Hassan, G.; Rousseau, C.; Pottie, K.; Canadian Collaboration for Immigrant and Refugee Health (CCIRH). Common Mental Health Problems in Immigrants and Refugees: General Approach in Primary Care. CMAJ 2011, 183, E959–E967. [Google Scholar] [CrossRef] [PubMed]
- Setia, M.S.; Quesnel-Vallee, A.; Abrahamowicz, M.; Tousignant, P.; Lynch, J. Different Outcomes for Different Health Measures in Immigrants: Evidence from a Longitudinal Analysis of the National Population Health Survey (1994–2006). J. Immigr. Minor. Health 2012, 14, 156–165. [Google Scholar] [CrossRef] [PubMed]
- Deloitte Touche Tohmatsu Limited. Global Mobile Consumer Trends; Deloitte: London, UK, 2017; p. 19. [Google Scholar]
- Cutler, D.M.; Lleras-Muney, A. Education and Health: Evaluating Theories and Evidence; Working Paper 12352; National Bureau of Economic Research: Cambridge, MA, USA, 2006. [Google Scholar] [CrossRef]
- Cendales-Ayala, B.; Useche, S.A.; Gómez-Ortiz, V.; Bocarejo, J.P. Bus Operators’ Responses to Job Strain: An Experimental Test of the Job Demand—Control Model. J. Occup. Health Psychol. 2016, 22, 518. [Google Scholar] [CrossRef] [PubMed]
- Imran, M.R.; Devi, B.S. Study of Changes in Cardiovascular and Cerebrovascular Risk Factors Due to Stress Using Physiological and Biochemical Profiles in Professional Urban Bus Drivers. Int. J. Recent Trends Sci. Technol. 2013, 6, 98–103. [Google Scholar]
- Kouvonen, A.; Vahtera, J.; Oksanen, T.; Pentti, J.; Väänänen, A.K.P.; Heponiemi, T.; Salo, P.; Virtanen, M.; Kivimäki, M. Chronic Workplace Stress and Insufficient Physical Activity: A Cohort Study. Occup. Environ. Med. 2013, 70, 3–8. [Google Scholar] [CrossRef] [PubMed]
- Bureau of Labor Statistics. American Time Use Survey-2018 Results; U.S. Department of Labor: Washington, DC, USA, 2019; p. 26.
- Glanz, K.; Rimer, B.K.; Viswanath, K. Health Behavior and Health Education: Theory, Research, and Practice; John Wiley & Sons: San Francisco, CA, USA, 2008. [Google Scholar]
- Corburn, J. Confronting the Challenges in Reconnecting Urban Planning and Public Health. Am. J. Public Health 2004, 94, 541–546. [Google Scholar] [CrossRef]
- BinDhim, N.F.; McGeechan, K.; Trevena, L. Smartphone Smoking Cessation Application (SSC App) Trial: A Multicountry Double-Blind Automated Randomised Controlled Trial of a Smoking Cessation Decision-Aid ‘App’. BMJ Open 2018, 8, e017105. [Google Scholar] [CrossRef]
- Oviedo Hernandez, D.; Dávila, J.D. Transport, Urban Development and the Peripheral Poor in Colombia—Placing Splintering Urbanism in the Context of Transport Networks. J. Transp. Geogr. 2016, 51, 180–192. [Google Scholar] [CrossRef]
- Zérah, M.-H. Splintering Urbanism in Mumbai: Contrasting Trends in a Multilayered Society. Geoforum 2008, 39, 1922–1932. [Google Scholar] [CrossRef]
- Jaglin, S. Differentiating Networked Services in Cape Town: Echoes of Splintering Urbanism? Geoforum 2008, 39, 1897–1906. [Google Scholar] [CrossRef]
- Roe, J.J.; Thompson, C.W.; Aspinall, P.A.; Brewer, M.J.; Duff, E.I.; Miller, D.; Mitchell, R.; Clow, A. Green Space and Stress: Evidence from Cortisol Measures in Deprived Urban Communities. Int. J. Environ. Res. Public Health 2013, 10, 4086–4103. [Google Scholar] [CrossRef] [PubMed]
- Kaźmierczak, A. The Contribution of Local Parks to Neighbourhood Social Ties. Landsc. Urban Plan. 2013, 109, 31–44. [Google Scholar] [CrossRef]
- Rudolph, L.; Caplan, J.; Ben-Moshe, K.; Dillion, L. Health in All Policies: A Guide for State and Local Governments; American Public Health Association: Washington, DC, USA, 2013. [Google Scholar]
| Author (Year) | Selection Bias | Study Design | Confounders | Blinding | Data Collection | Withdrawals and Dropouts | Global Rating |
|---|---|---|---|---|---|---|---|
| Althoff et al. (2016) | ** | ** | ** | ** | * | N/A | * |
| Amiri et al. (2017) | ** | ** | N/A | *** | * | ** | ** |
| Bakolis et al. (2018) | ** | ** | N/A | *** | * | ** | ** |
| Ferrara et al. (2018) | *** | ** | N/A | *** | * | N/A | *** |
| Frey et al. (2017)* | *** | ** | N/A | *** | * | ** | *** |
| Gutiérriez Garcia et al. (2017) | ** | ** | N/A | *** | * | ** | ** |
| Hamann et al. (2016) | ** | ** | *** | ** | * | ** | ** |
| Howe et al. (2016) | * | ** | ** | *** | * | ** | ** |
| Isaac et al. (2018) | *** | *** | N/A | *** | ** | N/A | *** |
| Lane et al. (2014) | ** | * | ** | *** | ** | ** | ** |
| MacKerron et al. (2013) | ** | ** | N/A | *** | * | N/A | ** |
| Martin et al. (2018)** | *** | ** | N/A | *** | * | ** | *** |
| McEwan et al. (2019)*** | * | * | * | ** | * | ** | * |
| Nef et al. (2015) | *** | ** | N/A | *** | ** | ** | *** |
| Nigg et al. (2017) | * | ** | N/A | *** | * | N/A | ** |
| Paredes et al. (2016)**** | ** | ** | N/A | *** | ** | ** | ** |
| Paredes et al. (2018)**** | ** | ** | * | *** | * | ** | ** |
| Park et al. (2019) | ** | ** | N/A | *** | * | * | ** |
| #Pichlmair et al. (2018) | ** | ** | N/A | *** | * | ** | ** |
| Ruiz-Ariza et al. (2018) | ** | * | * | ** | * | * | * |
| Yang et al. (2019) | *** | ** | ** | *** | * | ** | *** |
| Author (Year) | Aims of the Research | Study Design | Recruitment and Data Collection | Data Analysis | Findings and Interpretation | Implications of Research | Overall Assessment of the Study |
|---|---|---|---|---|---|---|---|
| Davis et al. (2017) * | ++ | + | – | – | – | ++ | – |
| Klakegg et al. (2017) | ++ | ++ | – | – | – | + | – |
| Krome et al. (2017) ** | ++ | + | + | – | – | + | + |
| Martindale et al. (2017) | ++ | ++ | – | + | – | + | + |
| Terken et al. (2013) | ++ | ++ | + | – | – | – | – |
| Tewell et al. (2019) *** | + | + | – | – | – | + | – |
| Trencher et al. (2017) | ++ | ++ | + | – | – | + | + |
| Author (Year) | Location * | Guiding Theory | Study Design | Health Outcome ** | Equity Characteristic(s) | Intervention Description |
|---|---|---|---|---|---|---|
| Althoff et al. (2016) | United States | No | Retrospective Cohort Analytic | Physical activity | Gender/Sex Plus (P/C) | Pokemon Go app, augmented reality, and map tracking used to promote physical activity in real world searches. |
| Amiri et al. (2017) | United States | No | Cohort | Behavior detection | Plus (P/C) | WearSense, IoT framework with sensing capabilities in the form of stopwatches used to detect stereotypic behaviors in children with autism based on environmental surroundings. |
| Bakolis et al. (2018) | United Kingdom | No | Cohort | Mental well-being | Place of Residence Occupation Gender/Sex | Urban Mind app, smartphone-based tool that tracked exposure to natural features within the built environment and their impacts on mental well-being. |
| Davis et al. (2017) | Italy | No | MM Cohort | Social connectedness | Socio-economic Status Social Capital Plus (P/C) | IoT and ambient-assisted living environments, effects of ambient lighting configurations on cognitive performance, mood, and social connectedness. |
| Ferrara et al. (2018) | United Kingdom | No | Retrospective ITS | Well-being and nature interactions | Social Capital | Smartphone app featuring sensing capabilities, tracked citizen interactions with urban green areas and their impacts on well-being. |
| Frey et al. (2018) | France | No | MM Cohort | Breathing | Social Capital | Breeze wearable pendant, breath-sensing multi-modal biofeedback reported in real-time to assess breathing patterns. |
| Gutiérrez García et al. (2017) | Spain | No | Cohort | Psychomotor development | Plus (P/C) | Ubiquitous Detection Ecosystem to Care and Early Stimulation for Children with Developmental Disorders smart toy, stackable cubes equipped with sensors used to detect delays in psychomotor development in children in real environments (e.g., home, school). |
| Hamann et al. (2016) | United Kingdom | No | Cohort Analytic | Well-being | Place of Residence SES | Rewild Your Life online intervention, online program that promoted spending time in local nature to improve mood, well-being, meaning in life, and mindfulness. |
| Howe et al. (2016) | United States | No | Cohort Analytic | Physical activity | Place of Residence Race, Gender/Sex, SES, Plus (P/C) | Pokemon Go app, augmented reality and map tracking used to promote physical activity in real-world searches. |
| Isaac et al. (2018) *** | Australia | No | Cross-sectional ** | Asthma | Place of Residence Plus (P/C) | Smartphone app that incorporated IoT features and real-time data on local environmental triggers (e.g., temperature, humidity) to inform asthma management. |
| Klakegg et al. (2017) | Australia | No | Cohort | Well-being | Occupation Social Capital Plus (P/C) | Mobile app which utilized sensors (“pervasive sensing approach”) to enhance care service for older adults by raising staff awareness of daily needs and routines. |
| Krome et al. (2017) | Australia | No | MM Cohort | Motivation for contextual exercise | Place of Residence | AutoGym, an in-car fitness program (mini-exercise bike linked to car speed utilizing sensors) run in a simulated rush hour driving scenario to promote physical exertion. |
| Lane et al. (2014) **** | United States | No | Cohort Analytic | Well-being | Social Capital | BeWell + app, runs on off-the-shelf sensor-enabled smartphones and was used to promote the adoption of healthy behavior (e.g., sleep patterns) via user feedback. |
| Mackerron et al. (2013) | United Kingdom | No | Retrospective ITS | Well-being | Place of Residence | Mappiness app, satellite positioning (GPS) was used to track participants and investigate momentary well-being when participants were in different environments. |
| Martin et al. (2018) | United Kingdom | No | MM Cohort | Stress | Place of Residence | Traeddy, an embedded technology augmented teddy bear (paired with an app) positioned as a well-being companion was used to inform car commuters about traffic situations and reduce stress. |
| Martindale et al. (2017) | United Kingdom | No | Cohort | Well-being | Social Capital | Connected Plants, examination of the potential of small-scale plants that incorporated IoT systems and collected personal data to promote health and wellbeing. |
| McEwan et al. (2019) | United Kingdom | No | Controlled Clinical Trial | Well-being | Place of Residence Gender/Sex SES | Shmapped app, smartphone app that used GPS to track participants and promote engaging in “geonarratives” to evaluate the impact of urban green space design on personal well-being. |
| Nef et al. (2015) | Switzerland | No | Cohort | Activities of daily living | Social Capital Plus (P/C) | Passive infrared sensors were installed in a smart apartment to detect and recognize eight different activities of daily living (e.g., cooking, sleeping, eating). |
| Nigg et al. (2017) | United States | No | Retrospective Cohort | Physical activity | Race/Ethnicity/Culture/Language Gender/Sex Plus (P/C) | Pokemon Go app, augmented reality and map tracking used to promote physical activity in real-world searches. |
| Paredes et al. (2016) | United States | Theory of implicit interaction | Cohort | Stress | Place of Residence | IoT interactive urban lights system, sensors used to respond to pedestrian traffic and designed to increase positive affect. |
| Paredes et al. (2018) | United States | No | MM Cohort Analytic | Breathing rate (i.e., stress) | Place of Residence | Physiological sensors (electrocardiogram, breathing rate harness, electrodermal activity bracelet) were used to assess reductions in drivers’ stress in simulated commuting environments. |
| Park et al. (2019) | South Korea | No | Cohort | Quality of Life | Plus (P/C) | Smart Aftercare app, an IoT wearable device connected with the app and other tools were used to assess the quality of life in patients with advanced lung cancer. |
| Pichlmair et al. (2018) | Germany | No | Cohort | Mindfulness | Place of Residence SES | Pen-Pen, a multi-component design which included the combination of a neck-cushion, a mobile app (which included GPS tracking), and a multi-modal feedback loop to improve mindfulness while commuting. |
| Ruiz-Ariza et al. (2018) | Spain | No | Randomized Controlled Trial | Emotional intelligence | Gender/Sex Education SES Plus (P/C) | Pokemon Go app, augmented reality and map tracking used to promote physical activity in real-world searches. |
| Terken et al. (2013) | Netherlands | No | Cohort | Stress | Place of Residence Plus (P/C) | In-car system that utilized a mood-sensing steering wheel and interactive in-car environment (i.e., images and sounds of a simulated environment) to assess mood and stress while commuting. |
| Tewell et al. (2019) | United Kingdom | No | MM Cohort | Meaningful activities | Occupation Plus (P/C) | Toolkit containing passive sensors used to assist individuals affected by dementia and Parkinson’s disease by monitoring meaningful activities in different home environments. |
| Trencher et al. (2017) | Japan | No | Cohort | Lifestyle activities | Social Capital Plus (P/C) | Multiple interventions carried out with wearable information communication technology devices, programs focused on assessing and monitoring daily activities (e.g., sleeping, walking). |
| Yang et al. (2019) | China | No | Cohort Analytic | Depression | Plus (P/C) | IoT structured wearable social sensing platform (wireless sensing technology used to connect with wearable devices, mobile phones, and server databases) used to assess mental state. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Buttazzoni, A.; Veenhof, M.; Minaker, L. Smart City and High-Tech Urban Interventions Targeting Human Health: An Equity-Focused Systematic Review. Int. J. Environ. Res. Public Health 2020, 17, 2325. https://doi.org/10.3390/ijerph17072325
Buttazzoni A, Veenhof M, Minaker L. Smart City and High-Tech Urban Interventions Targeting Human Health: An Equity-Focused Systematic Review. International Journal of Environmental Research and Public Health. 2020; 17(7):2325. https://doi.org/10.3390/ijerph17072325
Chicago/Turabian StyleButtazzoni, Adrian, Marta Veenhof, and Leia Minaker. 2020. "Smart City and High-Tech Urban Interventions Targeting Human Health: An Equity-Focused Systematic Review" International Journal of Environmental Research and Public Health 17, no. 7: 2325. https://doi.org/10.3390/ijerph17072325
APA StyleButtazzoni, A., Veenhof, M., & Minaker, L. (2020). Smart City and High-Tech Urban Interventions Targeting Human Health: An Equity-Focused Systematic Review. International Journal of Environmental Research and Public Health, 17(7), 2325. https://doi.org/10.3390/ijerph17072325





