Abstract
Screen media usage has become increasingly prevalent in daily life with children being exposed to screens at an early age. This is a growing public health concern with evidence linking screen exposure to detrimental health outcomes, whereas relationship between screen exposure and the presence of astigmatism among preschoolers remains unknown, thus we aimed to resolve this issue. During the 2017 survey of the Longhua Child Cohort Study, data of 29,595 preschoolers were collected via a caregiver-reported questionnaire regarding socio-demographics, screen exposure and refraction. Cox regression models were adopted to generate adjusted prevalence ratios (APR) and 95% confidence intervals (CI) to estimate the association between early screen exposure and astigmatism. 28,029 preschoolers were included in the final analysis. After adjustment for potential confounders, screen exposure during early life was significantly associated with the increased risk of astigmatism (APR and 95% CI: 2.25, 1.76–2.88), and the greatest risk was observed in the period from birth to 1-year (APR and 95% CI: 3.10, 2.41–3.98). The risk of astigmatism increased with both the total years of exposure and the average daily duration of screen exposure. Our findings suggested that preschoolers who were exposed to screens during early life might have an increased risk of astigmatism.
1. Introduction
Astigmatism is a refractive condition where light rays are not imaged at a single retinal point. It is due to either the cornea or crystalline lens having surface curvatures that are not spherical but rather differ in orthogonal meridians; it can be optically corrected using a cylindrical lens. Astigmatism is relatively common and can have detrimental visual effects if of high levels (>4.00 diopter cylinder) from a young age [1]. It is associated with high myopia [2], and if it occurs early in life can lead to the development of amblyopia; the visual impacts are greater in a developing visual system [3,4]. It is well-known that visual function rapidly develops and improves after birth to 6 years of age, and that the growth of the eye is greatest during the first year of life and slows with age [5,6]. Thus, determination of modifiable risk factors that are present during this period and might be linked to the development of astigmatism, is important.
With the rapid development of information technology, electronic media devices (e.g., televisions (TVs), computers, smartphones and tablets) are embedded in people’s daily lives for work, education and entertainment [7,8]. Even more dramatic has been the great increase in the use of such devices by young and very young children. A nationally representative survey of the United States found that 68% of children under the age of 2 used screen-based devices during a typical day [7], and another recent survey from Italy showed that 80% of children aged 3 to 5 years used their parent’s smartphone [9]. Excessive screen time is associated with poor sleep, obesity and psychological problems among school-aged children and thus generally considered to be detrimental to children’s health [8]. There are also adverse ocular impacts with several studies reporting that prolonged screen time is linked to asthenopia [10], myopia [11], and low vision [12]. Whether there is any relationship between screen exposure in early life and astigmatism amongst preschoolers is unknown, as is whether any effect is dose and/or age dependent. Due to the increased use of small hand held mobile devices [13], understanding the implications of exposure to both fixed and hand held devices is needed.
The routine vision screening of kindergarten children in Longhua District of Shenzhen and the survey of Longhua Children Cohort Study (LCCS) provided us an opportunity to evaluate the relationship between screen exposure during early life with astigmatism based on a life-course approach [14]. Given that parental history of refractive errors was associated with astigmatism [15,16], we also assessed the combined influence of parental eyesight and screen exposure on astigmatism among preschool children aged 2–7 years in Longhua District, Shenzhen, China.
2. Materials and Methods
2.1. Study Participants
All participants were recruited from the LCCS which examined the influence of environmental factors surrounding children’s early life on child psycho-behavioral development; it commenced in September 2014 with once per year follow up [17,18,19,20]. Children were enrolled in the LCCS at the commencement of kindergarten and their primary caregivers completed a self-administered structured questionnaire. In 2017 a total of 29,595 caregivers of children aged 2 to 7 years were approached to complete the screen exposure and vision survey. The study was conducted in accordance with the Declaration of Helsinki, and the protocol was approved by the Ethics Committee of the School of Public Health at Sun Yat-sen University (ethics clearance No. 2015–016). Signed written informed consent was obtained from the primary caregivers. In the present study, children who had missing information on either the socio-demographic characteristics or refractive condition and children who had been diagnosed with another type of refractive error (i.e., did not have normal vision or astigmatism) were excluded. Figure S1 presents the flow diagram of participant selection. Data of 28,029 (95 %) preschoolers were included in the final analysis.
2.2. Data Collection
Primary caregivers completed a self-administered structured questionnaire regarding the parental socio-demographic characteristics including family income, parental age at childbirth, education level and eyesight status (i.e., poor uncorrected vision due to refractive errors versus good uncorrected vision), as well as children’s general information including gender, date of birth, single child or not, birth history (i.e., full-term versus preterm), birth weight, passive smoking, screen exposure during different stages of early life and refractive status (based on the kindergarten vision screening).
2.3. Measurements of Screen Exposure
A set of questions was asked about the screen exposure. Table 1 presents the questions and options regarding screen exposure from birth to 1 year of age. The questions and options shown in Table 1 were repeated for yearly age bands up to 6 years of age (i.e., 1–2 y, 2–3 y, 3–4 y, 4–5 y and 5–6 y). For children aged less than 6 years, screen exposure across the child’s entire life was investigated, while for children aged over 6 years, only exposure from birth to 6 years was assessed. The following variables were used to describe the screen exposure: (1) the child’s age at first exposure, (2) the total years of exposure, and (3) average daily exposure duration.

Table 1.
Questions and options regarding screen exposure from birth to 1 year of age.
2.4. Determination of the Presence of Astigmatism
Since 2017, the vision screening for preschool children is performed by the ophthalmologists from the Longhua District Maternal and Child Health Hospital twice per school year (i.e., spring term and autumn term) in kindergartens. The results of the vision screening are provided to children’s caregivers by teachers, and if the results of screening implied an abnormal refraction (i.e., myopia, astigmatism, hyperopia and other visual abnormalities), parents will be advised to take the child for a more comprehensive eye examination at the ophthalmic clinic of the hospital. At the clinic, the ophthalmologists would suggest the child to receive a comprehensive eye examination and take appropriate measures (e.g., having the child wear glasses to correct vision, etc.) according to the cycloplegic refraction. The ophthalmologists from Longhua District Maternal and Child Health Hospital defined the children’s refractive problem being astigmatism if the measured astigmatism was 1.75 diopter cylinder or more, myopia if the refraction was 0.50 diopter or lower, and hyperopia if the refraction was 2.00 diopter or more for preschool children.
In the present study, therefore, the following questions [21] were asked about the child’s eye conditions: (1) Has your child ever been diagnosed as having poor sight by the oculist? (0 = ‘no’, 1 = ‘yes’, 2 = ‘uncertain’); and if yes, the subsequent questions were asked separately, i.e., questions (2)–(7): Has your child ever been diagnosed as having astigmatism/myopia/hyperopia/strabismus/amblyopia/other common visual problems? (0 = ‘no’, 1 = ‘yes’, 2 = ‘uncertain’). (8) When was your child diagnosed as having the aforementioned poor eyesight? In this study, only children with astigmatism and children without poor sight were included in the analysis.
2.5. Potential Confounders
According to the previous literature [22,23,24], factors such as a child’s age, gender, premature birth (<37 weeks), birth weight (low birth weight (<2500 g), normal birth weight (2500–4000 g), macrosomia (>4000 g)), parental age at childbirth, parental education level (junior high school and below, high school or technical secondary school, junior college, and graduate and above), monthly household income (<5000, 5000~10000, 10000~15000, 15000~20000, and ≥20000 RMB per month) and passive smoking can impact a child’s refraction and were thus included as potential confounders in this study. Moreover, parental eyesight status (i.e., poor uncorrected vision due to refractive errors versus good uncorrected vision) was the stratification variable in the stratified analysis.
2.6. Statistical Analysis
Means and standard deviations (SD) were used to describe continuous variables, and absolute frequencies and proportions were used for categorical variables. Chi-square tests or t-tests were applied to compare the socio-demographic characteristics and screen exposure between preschoolers with astigmatism and preschoolers with normal eyesight.
Cox regression modelling [25] was adopted to examine the associations between screen exposure and age of first screen exposure and astigmatism, and to evaluate dose-response relationships of total years of exposure and daily duration of exposure with astigmatism. A crossover analysis, based on different permutations of exposure (Yes) versus no exposure (No) in each year from birth to 3 years old, was performed to explore the sensitive period [14]. To determine the impact of screen exposure on astigmatism in children without a hereditary predisposition towards astigmatism and the combined impact of parental eyesight and screen exposure on astigmatism, the participants were stratified based on the status of parental eyesight (i.e., poor uncorrected vision due to refractive errors versus good uncorrected vision), and the aforementioned analyses were repeated. Also, interactive analyses were performed to examine the interaction of screen exposure (Yes/No) and status of parental eyesight (i.e., poor uncorrected vision due to refractive errors versus good uncorrected vision) on children’s astigmatism. All the multiple regression models above were performed with adjustment for the aforementioned potential confounders, and adjusted prevalence ratio (APR) and 95% confidence intervals (95% CI) were determined [25].
Additionally, given that preterm birth has a higher risk of astigmatism than full-term birth [26], stratification analysis was applied to assess the association between screen exposure and astigmatism in two subgroups of preschoolers (i.e., preterm birth and full-term birth). The adjustment for potential confounders including children’s age, gender, maternal age at childbirth, paternal age at childbirth, maternal education level, paternal education level, monthly household income and smoking was also made.
Statistical analyses were performed with R statistical software (version 3.4.0, http://www.r-project.org) and SPSS software (version 23.0; SPSS Inc., Chicago, IL, USA). Two-sided p < 0.05 was considered as the significant difference.
3. Results
3.1. Characteristics of Preschoolers with Astigmatism and Those with Normal Eyesight
Children who had astigmatism were older (4.7 ± 0.9 vs. 4.6 ± 0.9 years old) and had a larger proportion of preterm birth (10.0% vs. 7.3%) and low birth weight (5.0% vs. 3.2%) compared to children with normal eyesight (Table 2). Other characteristics including child’s gender, parental education, age at childbirth, family income and passive smoking were similar between the two groups.

Table 2.
Characteristics and comparison of preschoolers with astigmatism and those with normal eyesight.
3.2. Associations between the Initial Age of Screen Exposure and Preschool Astigmatism
Compared with those who had no screen exposure, preschoolers exposed to screens had a higher risk of astigmatism (APR: 2.25, 95% CI: 1.76–2.88), and preschoolers whose parents had poor uncorrected vision had an even greater risk of astigmatism than those whose parents had good uncorrected vision (APR: 7.15, 95% CI: 4.84–10.56) (Table S1). What is more, preschoolers who were initially exposed to screens during the first three years of life had statistically significant higher risk of astigmatism, and those who were initially exposed to screens in the first year of life had the highest risk (Figure 1A). Furthermore, stratified analyses based on parental eyesight status showed similar trends (Figure 1B). Additionally, the interaction of screen exposure and status of parental eyesight on preschool astigmatism was statistically significant (p < 0.05).
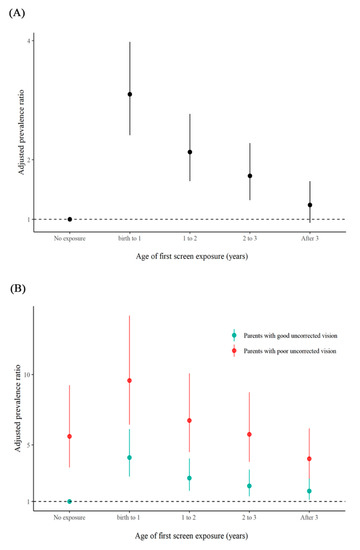
Figure 1.
Associations between the initial age of screen exposure and preschool astigmatism. (A): Associations between the age of first screen exposure and preschool astigmatism. (B): Associations between the age of first screen exposure and preschool astigmatism stratified by the status of parental eyesight.
3.3. Relationships of Average Daily Exposure Duration and the Total Years of Exposure with Preschool Astigmatism
Compared with no screen exposure, average daily screen time over 120 min had the strongest relationship to astigmatism risk, and the strength of the association increased as the number of total years of exposure (i.e., 1, 2, 3, 4, ≥5 years) increased (APR and 95% CI for 1: 2.10, 1.04–4.22; for 2: 1.70, 1.05–2.77; for 3: 2.34, 1.68–3.26, for 4: 2.54, 1.87–3.45; and for ≥5: 3.65, 2.75–4.84) (Table 3). What is more, the association between the total years of screen exposure and preschool astigmatism became weaker as average daily screen time (i.e., >120 min, 60–120 min and <60 min) decreased (Table 3). A similar trend was observed in the results of the stratified analyses based on the status of parental eyesight (Table 3).

Table 3.
Associations between the total years of exposure and preschool astigmatism grouped by average daily screen time.
3.4. Associations between Exposure to Screens during Postnatal Three Years and Astigmatism
Compared with preschoolers never exposed to screens during their first three years of life, all subgroups except the one only exposed in the second year of life had statistically significant higher risk of astigmatism, and the subgroup exposed to screens during the entire three years had the highest risk of astigmatism (APR: 2.78, 95% CI: 2.42–3.19) (Table 4). What’s more, children who were exposed to screens only in the first year of life had a higher risk of astigmatism than children exposed to screens only in the postnatal second or third year of life (APR and 95% CI: for subgroup exposed to screens only in the postnatal first year: 1.91, 1.44–2.54; for subgroup exposed to screens only in the postnatal second year: 1.08, 0.70–1.69; for subgroup exposed to screens only in the postnatal third year: 1.48, 1.25–1.75) (Table 4). A similar trend was observed in the results of the stratified analyses based on the status of parental eyesight (Table 4).

Table 4.
Associations between exposure to screens during early life (postnatal three years) and astigmatism.
3.5. Sensitivity Analysis
The associations between screen exposure (Yes/No), the initial age of screen exposure and astigmatism were still significant in both subgroups (i.e., preterm birth and full-term birth), and preterm preschoolers had a greater risk of astigmatism than those born at term (Table S2).
4. Discussion
It was observed that preschoolers exposed to screens in early life had a high risk of astigmatism and the risk increased as the daily duration and total years of exposure increased. As the age of first screen exposure delayed, the strength of association reduced. Association between screen exposure and astigmatism was still significant in preschoolers whose parents had good uncorrected vision, and strength of the associations was enhanced in preschoolers whose parents had poor uncorrected vision, indicative of the combined impact of parental history of poor vision and screen exposure on astigmatism. This study supports the need to promote public health awareness of the visual harm of screen exposure during early life, especially for those parents who have poor uncorrected vision.
Screen exposure may have adverse health effects, particularly on eyes. Studies regarding the impact of excessive screen time on ocular-related health problems, have been largely confined to the ocular symptoms related to eye fatigue, myopia and low vision [10,11,27]. Here we found that screen exposure was associated with a higher risk of astigmatism amongst preschoolers and the risk increased as the daily duration and total years of exposure increased. Since limited research has been undertaken about screen exposure and astigmatism, no other studies are available for direct comparison. However, a number of related studies support our findings. Several cross-sectional studies in older children aged 6 to 18 years show a positive association between poor vision and excessive time on TV viewing and Internet use (more than 3 hours/day), and another study in a similar age group, 7–15 years, suggested that regular use of computers is a potential risk factor for refractive error [12,28,29,30]. Inspired by life-course epidemiology [14], we found that exposure to screens during the first year of life had the greater impact on preschool astigmatism than that during the second year and the third year, which indicated that the period from birth to 1-year-old was the sensitive period of their association. Intriguingly, such finding supports the idea that environmental impacts during the critical period of visual system development have the most effect [5,6], which possibly revealed the important timing of interventions to prevent astigmatism among preschoolers. However, as cross-sectional studies can only determine associations, longitudinal studies are required to prove if exposure to screens causes high prevalence of astigmatism.
Previous studies have showed that children whose parents have myopia and/or astigmatism are at higher risk of astigmatism than those whose parents have good vision [15,16]. Analogous to this, astigmatism was more prevalent in children whose parents had poor uncorrected vision than in those whose parents had good uncorrected vision, regardless of the screen exposure status. Furthermore, compared with preschoolers whose parents had good uncorrected vision, the strength of the associations between screen exposure and astigmatism was stronger in preschoolers whose parents had poor uncorrected vision, suggesting a combined impact of genetic predisposition and screen exposure on astigmatism. However, that children and their parents share similar environments, nutrition, culture and education may also further strengthen this relationship [31]. Further studies with susceptibility gene measurement are needed to clarify the effect of heredity on astigmatism.
The physiological mechanism via which screen exposure and astigmatism are linked is unknown. There are several untested hypotheses. Excessive screen time at close distances might cause excessive accommodation, thus leading to overworking of the ciliary muscles of the eyes of children and impacting the natural development of the crystalline lens, impacting its curvature [32]. Alternately, looking at the screens up close may lead to changes in the shape of the children’s corneas, due to variations in the palpebral aperture and eye movements performed during the tasks [33], or the mechanical interactions between the cornea and the eyelids [1]. Also, it may be that staring down at the screen increases pressure from eyelids on the cornea, which can result in increased corneal astigmatism [34]. Future ocular biometry studies in very young children and information about posture adopted while they look at handheld screens could provide insight into the underlying mechanism.
This study is one of the very few studies investigating the association between screen exposure during the early life and preschool astigmatism. However, it has several limitations. The astigmatism cases were identified as positive in a large sample screening and further diagnosed as astigmatism at the ophthalmic clinic, and reported by parents or other caregivers, which might lead to information bias. The findings from our published study [21], which used the same measurement of astigmatism, were consistent with the findings from the multi-ethnic pediatric eye disease and Baltimore pediatric eye disease studies [23] which used cycloplegic refraction to define astigmatism, thus illustrating that to some extent, our measurements were reliable. Additionally, the measurement of outcome was monotonous and not graded. Since a previous study from Singapore suggested that playing video games and computers may be associated with astigmatism severity [15], it would be more interesting and insightful if further studies could include the distribution of different levels of astigmatism and its association with screen exposure. Information on screen exposure from birth to 6 years of age was recalled and relied on parental or other caregivers’ reporting, which might lead to information bias. What’s more, information regarding screen exposure in kindergarten might not be fully reported, which could lead to an underestimation of screen exposure. In the present electronic information age, measurements of screen exposure are warranted to be developed. Some characteristics of screen exposure that may have a unique effect on or a different mechanism in affecting astigmatism, such as posture when children are exposed to screens, the screen size and resolution of screen devices, pattern of screen use (i.e., intermittent use, continuous use), were not investigated in the present study. Future studies should take these details regarding screen devices into consideration. Although the data was corrected for age, gender, premature birth, birth weight, parental education, age at childbirth, family income and passive smoking, there may be other unmeasured confounders like other types of near work (e.g., writing, reading) which might impact the findings. Finally, the nature of cross-sectional study design could only provide suggestive but not confirmative causality regarding the association between screen exposure and preschool astigmatism. Further longitudinal studies with objective measurements should be conducted to investigate the cause-effect relationship.
5. Conclusions
Screen exposure in early life could be associated with a higher risk of astigmatism and the postnatal first year might be the sensitive period for their associations. However, considering the poor assessment of astigmatism in our study, it’s premature to conclude that early screen time leads to astigmatism with current data. Further longitudinal studies including objective measurements performed with cycloplegia are needed to verify our finding.
Supplementary Materials
The following are available online at https://www.mdpi.com/1660-4601/17/7/2216/s1, Figure S1: The flow diagram of participant selection, Table S1: Associations between screen exposure and astigmatism among preschoolers, Table S2: Sensitivity analysis.
Author Contributions
Conceptualization, L.H. and W.-Q.C.; Data curation: W.-Q.C.; Methodology: L.H., G.-Y.Y., K.L.S., C.-G.L., J.-Y.C., G.-H.H., Z.-L.R. and W.-Q.C.; Formal analysis: L.H., G.-Y.Y., K.L.S., C.-G.L., J.-Y.C., G.-H.H., Z.-L.R. and W.-Q.C.; Investigation, L.H., G.-Y.Y., C.-G.L., J.-Y.C., G.-H.H., Z.-L.R. and W.-Q.C.; Writing—original draft preparation, L.H., G.-Y.Y. and J.-Y.C.; Writing—review and editing, L.H., G.-Y.Y., K.L.S. and W.-Q.C.; Project administration, W.-Q.C. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by the Government of Longhua District, Shenzhen, China (Longhua STE Fund with grant number 2013142).
Acknowledgments
This study was conducted as part of the Longhua Child Cohort Study with the support of the Government of Longhua District, Shenzhen, China. The School of Public Health, Sun Yat-sen University undertook this study. The authors would like to thank the staff in Longhua District Maternal and Child Health Hospital, especially Chuan-An Wu, Xiao-Na Yin, Jing-Yu Zhang, Yan-Ling Zhang, and Xiao-Qin Jiang, who offered much help during the field investigation. We are also grateful to all the families who participated in this study.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Read, S.A.; Collins, M.J.; Carney, L.G. A review of astigmatism and its possible genesis. Clin. Exp. Optom. 2007, 90, 5–19. [Google Scholar] [CrossRef]
- Fulton, A.B.; Hansen, R.M.; Petersen, R.A. The relation of myopia and astigmatism in developing eyes. Ophthalmology 1982, 89, 298–302. [Google Scholar] [CrossRef]
- Dobson, V.; Miller, J.M.; Harvey, E.M.; Mohan, K.M. Amblyopia in astigmatic preschool children. Vision Res. 2003, 43, 1081–1090. [Google Scholar] [CrossRef]
- Gwiazda, J.; Grice, K.; Held, R.; McLellan, J.; Thorn, F. Astigmatism and the development of myopia in children. Vision Res. 2000, 40, 1019–1026. [Google Scholar] [CrossRef]
- Bremond-Gignac, D.; Cussenot, O.; Deplus, S.; Peuchmar, M.; Ferkadji, L.; Emaleh, M.; Lassau, J.P. Computation of eyeball growth by magnetic resonance imaging (26.11.93). Surg. Radiol. Anat. 1994, 16, 113–115. [Google Scholar] [CrossRef]
- Bremond-Gignac, D.; Copin, H.; Lapillonne, A.; Milazzo, S. Visual development in infants: Physiological and pathological mechanisms. Curr. Opin. Ophthalmol. 2011, 22, S1–S8. [Google Scholar] [CrossRef] [PubMed]
- Duch, H.; Fisher, E.M.; Ensari, I.; Harrington, A. Screen time use in children under 3 years old: A systematic review of correlates. Int. J. Behav. Nutr. Phys. Act 2013, 10, 102. [Google Scholar] [CrossRef] [PubMed]
- Paudel, S.; Jancey, J.; Subedi, N.; Leavy, J. Correlates of mobile screen media use among children aged 0–8: A systematic review. BMJ Open 2017, 7, e014585. [Google Scholar] [CrossRef] [PubMed]
- Bozzola, E.; Spina, G.; Ruggiero, M.; Memo, L.; Agostiniani, R.; Bozzola, M.; Corsello, G.; Villani, A. Media devices in pre-school children: The recommendations of the Italian pediatric society. Ital. J. Pediatr. 2018, 44, 69. [Google Scholar] [CrossRef] [PubMed]
- Rechichi, C.; De Moja, G.; Aragona, P. Video Game Vision Syndrome: A new clinical picture in children? J. Pediatr. Ophthalmol. Strabismus 2017, 54, 346–355. [Google Scholar] [CrossRef] [PubMed]
- Saxena, R.; Vashist, P.; Tandon, R.; Pandey, R.M.; Bhardawaj, A.; Gupta, V.; Menon, V. Incidence and progression of myopia and associated factors in urban school children in Delhi: The North India Myopia Study (NIM Study). PLoS ONE 2017, 12, e0189774. [Google Scholar] [CrossRef] [PubMed]
- Bener, A.; Al-Mahdi, H.S.; Vachhani, P.J.; Al-Nufal, M.; Ali, A.I. Do excessive internet use, television viewing and poor lifestyle habits affect low vision in school children? J. Child Health Care 2010, 14, 375–385. [Google Scholar] [CrossRef] [PubMed]
- Kilic, A.O.; Sari, E.; Yucel, H.; Oguz, M.M.; Polat, E.; Acoglu, E.A.; Senel, S. Exposure to and use of mobile devices in children aged 1–60 months. Eur. J. Pediatr. 2019, 178, 221–227. [Google Scholar] [CrossRef] [PubMed]
- Ben-Shlomo, Y.; Mishra, G.D.; Kuh, D. Life Course Epidemiology. In Handbook of Epidemiology, 2nd ed.; Ahrens, W., Pigeot, I., Eds.; Springer Science + Business Media: New York, NY, USA, 2014; pp. 1521–1550. [Google Scholar]
- Tong, L.; Saw, S.M.; Carkeet, A.; Chan, W.Y.; Wu, H.M.; Tan, D. Prevalence rates and epidemiological risk factors for astigmatism in Singapore school children. Optom. Vis. Sci. 2002, 79, 606–613. [Google Scholar] [CrossRef] [PubMed]
- Rakhshani, M.H.; Mohammad, K.; Zeraati, H.; Nourijelyani, K.; Hashemi, H.; Fotouhi, A. Analysis of familial aggregation in total, against-the-rule, with-the-rule, and oblique astigmatism by conditional and marginal models in the Tehran eye study. Middle East Afr. J. Ophthalmol. 2012, 19, 397–401. [Google Scholar] [CrossRef] [PubMed]
- Lin, Q.; Hou, X.Y.; Yin, X.N.; Wen, G.M.; Sun, D.; Xian, D.X.; Fan, L.; Jiang, H.; Jing, J.; Jin, Y.; et al. Prenatal Exposure to environmental tobacco smoke and hyperactivity behavior in Chinese young children. Int. J. Environ. Res. Public Health 2017, 14, 1132. [Google Scholar] [CrossRef]
- Ruan, Z.L.; Liu, L.; Strodl, E.; Fan, L.J.; Yin, X.N.; Wen, G.M.; Sun, D.L.; Xian, D.X.; Jiang, H.; Jing, J.; et al. Antenatal training with music and maternal talk concurrently may reduce autistic-like behaviors at around 3 years of age. Front. Psychiatry 2017, 8, 305. [Google Scholar] [CrossRef]
- Liu, L.; Fan, L.; Hou, X.Y.; Wu, C.A.; Yin, X.N.; Wen, G.M.; Sun, D.; Xian, D.X.; Jiang, H.; Jing, J.; et al. Family childcare types and conduct problem behaviors in young children: The mediation role of caregiver-child interaction. Front. Pediatr. 2018, 6, 217. [Google Scholar] [CrossRef]
- He, G.H.; Liu, L.; Strodl, E.; Ruan, Z.L.; Jiang, H.; Jing, J.; Jin, Y.; Chen, W.Q. Parental Type D personality and children’s hyperactive behaviors: The mediating role of parent-child interactive activities. Int. J. Environ. Res. Public Health 2019, 16, 1116. [Google Scholar] [CrossRef] [PubMed]
- Li, C.G.; Yang, G.-Y.Y.; Schmid, K.L.; Huang, L.H.; He, G.H.; Liu, L.; Ruan, Z.L.; Chen, W.Q. Associations between environmental tobacco smoke exposure in early life and astigmatism among Chinese preschool children. Int. J. Environ. Res. Public Health 2019, 16, 3725. [Google Scholar] [CrossRef]
- Deng, Y.; Liao, Y.; Yang, Y.; Yu, C.; Peng, X.; Yin, X. Refractive error’s distribution and clinical characteristics of preterm and full-term children. Yan Ke Xue Bao 2010, 25, 93–95. [Google Scholar] [CrossRef] [PubMed]
- McKean-Cowdin, R.; Varma, R.; Cotter, S.A.; Tarczy-Hornoch, K.; Borchert, M.S.; Lin, J.H.; Wen, G.; Azen, S.P.; Torres, M.; Tielsch, J.M.; et al. Risk factors for astigmatism in preschool children: The multi-ethnic pediatric eye disease and Baltimore pediatric eye disease studies. Ophthalmology 2011, 118, 1974–1981. [Google Scholar] [CrossRef] [PubMed]
- Pertile, R.; Trettel, C.; Bombarda, L.; Racano, E.; Piffer, S. Early childhood eye diseases and perinatal risk factors. Potential of record linkage between current information flows. Minerva. Pediatr. 2018. [Google Scholar] [CrossRef]
- Lee, J. Odds ratio or relative risk for cross-sectional data? Int. J. Epidemiol. 1994, 23, 201–203. [Google Scholar] [CrossRef] [PubMed]
- Larsson, E.K.; Holmstrom, G.E. Development of astigmatism and anisometropia in preterm children during the first 10 years of life: A population-based study. Arch. Ophthalmol. 2006, 124, 1608–1614. [Google Scholar] [CrossRef]
- Moon, J.H.; Lee, M.Y.; Moon, N.J. Association between video display terminal use and dry eye disease in school children. J. Pediatr. Ophthalmol. Strabismus 2014, 51, 87–92. [Google Scholar] [CrossRef]
- Bener, A.; Al-Mahdi, H.S.; Ali, A.I.; Al-Nufal, M.; Vachhani, P.J.; Tewfik, I. Obesity and low vision as a result of excessive Internet use and television viewing. Int. J. Food Sci. Nutr. 2011, 62, 60–62. [Google Scholar] [CrossRef]
- Bener, A.; Al-Mahdi, H.S. Internet use and television viewing in children and its association with vision loss: A major public health problem. J. Public Health Afr. 2012, 3, e16. [Google Scholar] [CrossRef]
- Sewunet, S.A.; Aredo, K.K.; Gedefew, M. Uncorrected refractive error and associated factors among primary school children in Debre Markos District, Northwest Ethiopia. BMC Ophthalmol 2014, 14, 95. [Google Scholar] [CrossRef]
- Lim, D.H.; Han, J.; Chung, T.Y.; Kang, S.; Yim, H.W.; Epidemiologic Survey Committee of the Korean Ophthalmologic Society. The high prevalence of myopia in Korean children with influence of parental refractive errors: The 2008–2012 Korean National Health and Nutrition Examination Survey. PLoS ONE 2018, 13, e0207690. [Google Scholar] [CrossRef]
- Agarwal, S.; Goel, D.; Sharma, A. Evaluation of the factors which contribute to the ocular complaints in computer users. J. Clin. Diagn Res. 2013, 7, 331–335. [Google Scholar] [CrossRef]
- Collins, M.J.; Buehren, T.; Bece, A.; Voetz, S.C. Corneal optics after reading, microscopy and computer work. Acta Ophthalmol. Scand. 2006, 84, 216–224. [Google Scholar] [CrossRef] [PubMed]
- Read, S.A.; Collins, M.J.; Carney, L.G. The diurnal variation of corneal topography and aberrations. Cornea 2005, 24, 678–687. [Google Scholar] [CrossRef] [PubMed]
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).