Multi-Year Examination of School-Based Programs in Preventing Childhood Obesity: A Case of a State Policy in the U.S.
Abstract
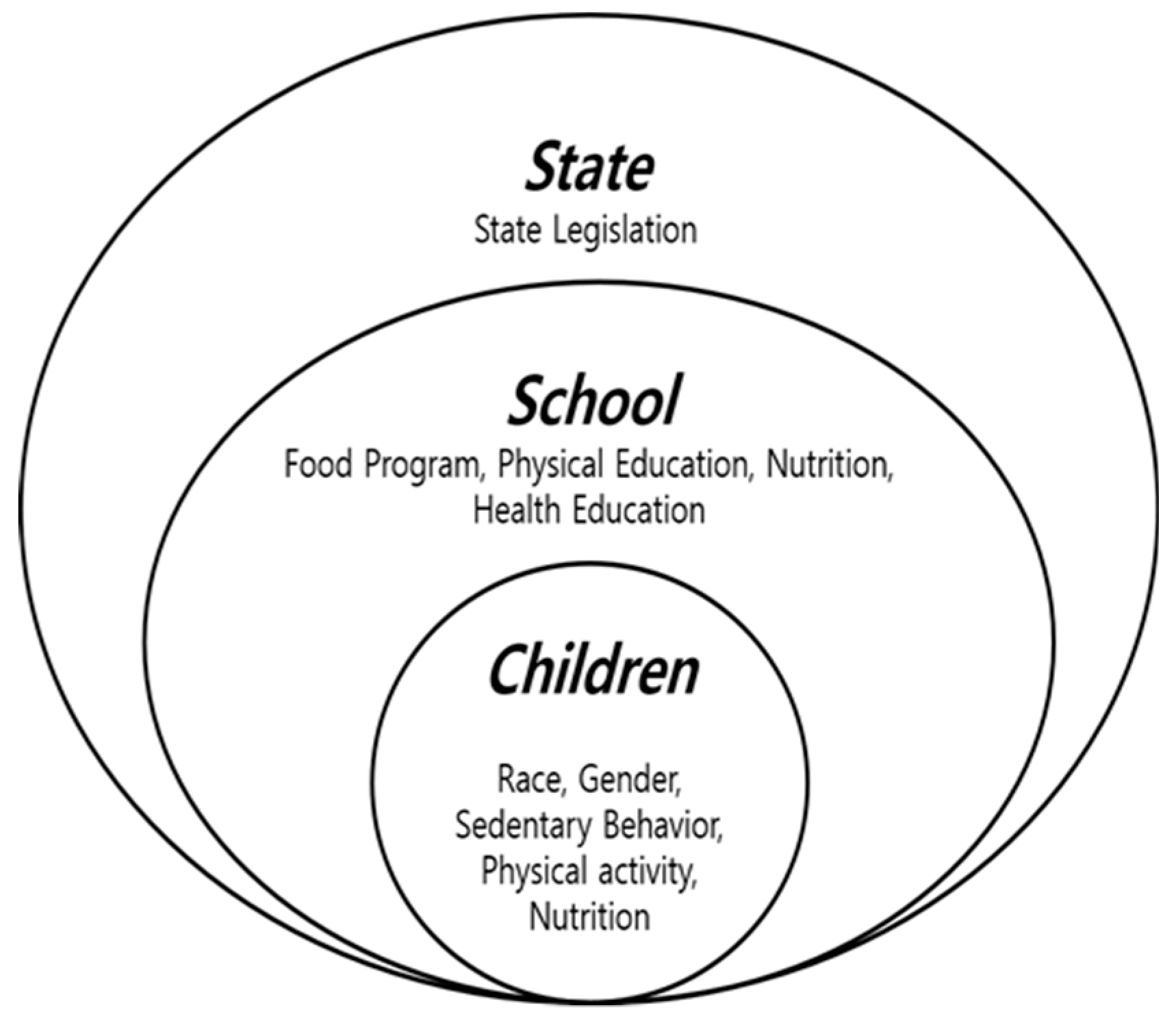
1. Introduction
2. Materials and Methods
2.1. Study Population and Sampling
2.2. Measurement
2.3. Data Analyses
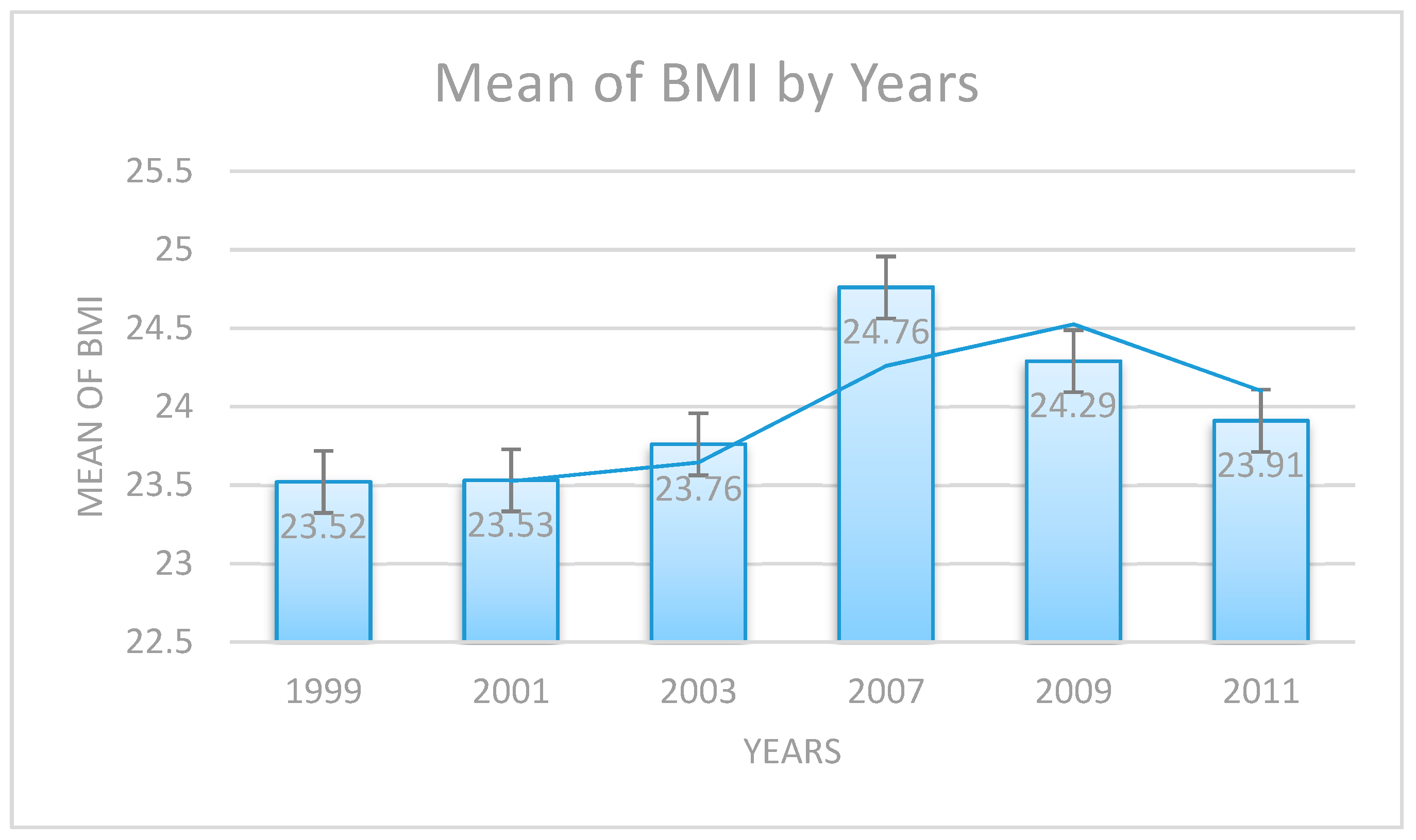
3. Results
Adolescents’ Obesity and Multivariable Logistic Regression
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Waxman, A. WHO’s global strategy on diet, physical activity and health. Scan J. Nut. 2004, 48, 58–60. [Google Scholar] [CrossRef]
- Centers for Disease Control and Prevention. Prevalence of Overweight among Children and Adolescents Ages 6–19 Years; NCHS: Hyattsville, MD, USA, 2009.
- Ogden, C.; Carroll, M.; Kit, B.; Flegal, K. Prevalence of obesity and trends in body mass index among US children and adolescents, 1999–2010. J. Am. Med. Assoc. 2012, 307, 483–490. [Google Scholar] [CrossRef] [PubMed]
- Lobstein, T.T.; Baur, L.L.; Uauy, R.R. Obesity in children and young people: A crisis in public health. Obes. Rev. 2004, 5, 4–85. [Google Scholar] [CrossRef]
- Hedley, A.A.; Ogden, C.L.; Johnson, C.L.; Carroll, M.D.; Curtin, L.R.; Flegal, K.M. Prevalence of overweight and obesity among US children, adolescents, and adults, 1999–2002. J. Am. Med. Assoc. 2004, 291, 2847–2850. [Google Scholar] [CrossRef] [PubMed]
- Van Cleave, J.; Gortmaker, S.L.; Perrin, J.M. Dynamics of obesity and chronic health conditions among children and youth. J. Am. Med. Assoc. 2010, 303, 623–630. [Google Scholar] [CrossRef] [PubMed]
- Russell-Mayhew, S.; McVey, G.; Bardick, A.; Ireland, A. Mental health, wellness, and childhood overweight/obesity. J. Obes. 2012, 2012, 281–801. [Google Scholar] [CrossRef] [PubMed]
- Sinha, R.; Fisch, G.; Teague, B.; Tamborlane, W.; Banyas, B.; Allen, K.; Caprio, S. Prevalence of impaired glucose tolerance among children and adolescents with marked obesity. N. Engl. J. Med. 2002, 346, 802–810. [Google Scholar] [CrossRef]
- Yeste, D.; Carrascosa, A. Complicaciones metabólicas de la obesidad infantil. An. Pediatría 2011, 75, 135.e1–135.e9. [Google Scholar] [CrossRef]
- Lloyd, L.J.; Langley-Evans, S.C.; McMullen, S.S. Childhood obesity and risk of the adult metabolic syndrome: A systematic review. Int. J. Obes. 2012, 36, 1–11. [Google Scholar] [CrossRef]
- Neumark-Sztainer, D.; Wall, M.; Guo, J.; Story, M.; Haines, J.; Eisenberg, M. Obesity, disordered eating, and eating disorders in a longitudinal study of adolescents: How do dieters fare 5 years later? J. Am. Diet. Assoc. 2006, 106, 559–568. [Google Scholar] [CrossRef]
- Villarejo, C.C.; Fernández-Aranda, F.F.; Jiménez-Murcia, S.S.; Peñas-Lledó, E.E.; Granero, R.R.; Penelo, E.E.; Menchón, J.M. Lifetime obesity in patients with eating disorders: Increasing prevalence, clinical and personality correlates. Eur. Eat. Disord. Rev. 2012, 20, 250–254. [Google Scholar] [CrossRef] [PubMed]
- Berenson, G.; Srinivasan, S.; Bao, W.; Newman, W.; Tracy, R.; Wattigney, W. Association between multiple cardiovascular risk factors and atherosclerosis in children and young adults. N. Engl. J. Med. 1998, 338, 1650–1656. [Google Scholar] [CrossRef] [PubMed]
- Cornette, R. The emotional impact of obesity on children. Worldviews Evid. Based Nurs. 2008, 5, 136–141. [Google Scholar] [CrossRef] [PubMed]
- He, X.; Baker, D. Body mass index, physical activity, and the risk of decline in overall health and physical functioning in late middle age. Am. J. Public Health 2004, 94, 1567–1573. [Google Scholar] [CrossRef]
- Okosun, I.S.; Choi, S.S.; Matamoros, T.T.; Dever, G.A. Obesity is associated with reduced self-rated general health status: Evidence from a representative sample of white, black, and Hispanic Americans. Prev. Med. 2001, 32, 429–436. [Google Scholar] [CrossRef]
- Calle, E.E.; Rodriguez, C.; Walker-Thurmond, K.; Thun, M.J. Overweight, Obesity, and Mortality from Cancer in a Prospectively Studied Cohort of U.S. Adults. N. Engl. J. Med. 2003, 348, 1625–1638. [Google Scholar] [CrossRef]
- Flegal, K.M.; Graubard, B.I.; Williamson, D.F.; Gail, M.H. Excess deaths associated with underweight, overweight, and obesity. JAMA J. Am. Med. Assoc. 2005, 293, 1861–1867. [Google Scholar] [CrossRef]
- Reilly, J.J.; Kelly, J.J. Long-term impact of overweight and obesity in childhood and adolescence on morbidity and premature mortality in adulthood: Systematic review. Int. J. Obes. 2011, 35, 891–898. [Google Scholar] [CrossRef]
- National Conference of State Legislatures. Childhood Obesity—2007 Update of Legislative Policy Options; National Conference of State Legislatures: Washington, DC, USA, 2012. [Google Scholar]
- Chen, X.; Ren, Y.; Lin, F.; MacDonell, K.; Jiang, Y. Exposure to school and community based prevention programs and reductions in cigarette smoking among adolescents in the United States, 2000–2008. Eval. Program Plan. 2012, 35, 321–328. [Google Scholar] [CrossRef]
- Bronfenbrenner, U. The Ecology of Human Development; Harvard University Press: Cambridge, MA, USA, 1979. [Google Scholar]
- Bronfenbrenner, U. Ecological systems theory. Encycl. Psychol. 2000, 3, 129–133. [Google Scholar]
- Boonpleng, W.; Park, C.; Gallo, A.M.; Corte, C.; McCreary, L.; Bergren, M. Ecological Influences of Early Childhood Obesity: A Multilevel Analysis. West. J. Nurs. Res. 2013, 35, 742–759. [Google Scholar] [CrossRef] [PubMed]
- Davison, K.K.; Birch, L.L. Childhood overweight: A contextual model and recommendations for future research. Obes. Rev. 2001, 2, 159–171. [Google Scholar] [CrossRef] [PubMed]
- U.S. Department of Health and Human Services. Healthy People 2020; Government Printing Office: Washington, DC, USA, 2010.
- Tabachnick, B.G.; Fidell, L.S. Using Multivariate Statistics, 5th ed.; Allyn & Bacon/Pearson Education: Boston, MD, USA, 2007. [Google Scholar]
- Chomitz, V.R.; McGowan, R.J.; Wendel, J.M.; Williams, S.A.; Cabral, H.J.; King, S.E.; Hacker, K.A. Healthy Living Cambridge Kids: A community-based participatory effort to promote healthy weight and fitness. Obesity 2010, 18 (Suppl. S1), S45–S53. [Google Scholar] [CrossRef] [PubMed]
- Millar, L.; Robertson, N.; Allender, S.; Nichols, M.; Bennett, C.; Swinburn, B. Increasing community capacity and decreasing prevalence of overweight and obesity in a community based intervention among Australian adolescents. Prev. Med. 2013, 56, 379–384. [Google Scholar] [CrossRef]
- Brown, T.T.; Summerbell, C.C. Systematic review of school-based interventions that focus on changing dietary intake and physical activity levels to prevent childhood obesity: An update to the obesity guidance produced by the National Institute for Health and Clinical Excellence. Obes. Rev. 2009, 10, 110–141. [Google Scholar] [CrossRef]
- Cullen, K.; Watson, K.; Zakeri, I. Improvements in middle school student dietary intake after implementation of the Texas Public School Nutrition Policy. Am. J. Public Health 2008, 98, 111–117. [Google Scholar] [CrossRef]
- Metos, J.; Nanney, M.S. The Strength of School Wellness Policies: One State’s Experience. J. Sch. Health 2007, 77, 367–372. [Google Scholar] [CrossRef]
- O’Brien, M.M.; Nader, P.R.; Houts, R.M.; Bradley, R.R.; Friedman, S.L.; Belsky, J.J.; Susman, E.E. The ecology of childhood overweight: A 12-year longitudinal analysis. Int. J. Obes. 2007, 31, 1469–1478. [Google Scholar] [CrossRef][Green Version]
- Gortmaker, S.; Cheung, L.; Peterson, K.; Chomitz, G.; Cradle, J.; Dart, H.; Laird, N. Impact of a school-based interdisciplinary intervention on diet and physical activity among urban primary school children: Eat well and keep moving. Arch. Pediatr. Adolesc. Med. 1999, 153, 975–983. [Google Scholar] [CrossRef]
- Slusser, W.M.; Cumberland, W.G.; Browdy, B.L.; Lange, L.L.; Neumann, C.C. A school salad bar increases frequency of fruit and vegetable consumption among children living in low-income households. Public Health Nutr. 2007, 10, 1490–1496. [Google Scholar] [CrossRef]
- Eaton, D.; Kann, L.; Kinchen, S.; Shanklin, S.; Ross, J.; Hawkins, J.; Wechsler, H. Youth risk behavior surveillance—United States, 2007. MMWR Surveill. Summ. 2008, 57 (Suppl. S4), 1–131. [Google Scholar] [PubMed]
- Field, A.; Austin, S.; Taylor, C.; Malspeis, S.; Rosner, B.; Rockett, H.; Gillman, M.W.; Colditz, G.A. Relation between dieting and weight change among preadolescents and adolescents. Pediatrics 2003, 112, 900–906. [Google Scholar] [CrossRef] [PubMed]
- Dietz, W.H.; Gortmaker, S.L. Preventing obesity in children and adolescents. Annu. Rev. Public Health 2001, 22, 337–353. [Google Scholar] [CrossRef]
- Andersen, R.E.; Crespo, C.J.; Bartlett, S.J.; Cheskin, L.J.; Pratt, M.M. Relationship of physical activity and television watching with body weight and level of fatness among children. Results from the Third National Health and Nutrition Examination Survey. JAMA J. Am. Med. Assoc. 1998, 279, 938–942. [Google Scholar] [CrossRef]
- Berkey, C.; Rockett, H.; Field, A.; Gillman, M.; Frazier, A.; Camargo, C.; Colditz, G. Activity, dietary intake, and weight changes in a longitudinal study of preadolescent and adolescent boys and girls. Pediatrics 2000, 105, E56. [Google Scholar] [CrossRef]
- Sisson, S.B.; Broyles, S.T.; Baker, B.L.; Katzmarzyk, P.T. Television, reading, and computer time: Correlates of school-day leisure-time sedentary behavior and relationship with overweight in children in the U.S. J. Phys. Act. Health 2011, 8, S188–S197. [Google Scholar] [CrossRef] [PubMed]
- Nishida, C.; Uauy, R.; Kumanyika, S.; Shetty, P. The joint WHO/FAO expert consultation on diet, nutrition and the prevention of chronic diseases: Process, product and policy implications. Public Health Nutr. 2004, 7, 245–250. [Google Scholar] [CrossRef] [PubMed]
- U.S. Department of Health and Human Services. 2008 Physical Activity Guidelines for Americans; U.S. Government Printing Office: Washington, DC, USA, 2008.
- McKenzie, T.; Lounsbery, M.A. School physical education: The pill not taken. Am. J. Lifestyle Med. 2009, 3, 219–225. [Google Scholar] [CrossRef]
- Story, M.; Kaphingst, K.M.; French, S. The role of schools in obesity prevention. Future Child. 2006, 16, 109–142. [Google Scholar] [CrossRef]
- Casazza, K.; Ciccazzo, M. Improving the dietary patterns of adolescents using a computer-based approach. J. Sch. Health 2006, 76, 43–46. [Google Scholar] [CrossRef]
- Heckman, J. Policies to foster human capital. Res. Econ. 2000, 54, 3–56. [Google Scholar] [CrossRef]

| Age | 16.21 Years (SD = 1.23) | Variables | ||||
|---|---|---|---|---|---|---|
| Overall % (N) | Body Mass Index | Consumption of Fruits and Vegetables | Sedentary Behavior | Physical Activity | Abusive Behavior to Lose Weight | |
| Sex: | t(8859) −7.41 ** | t(8860) −6.79 ** | t(8844) −1.80 | t(8860) −23.84 ** | t(8860) −13.52 ** | |
| Male | 46.2% (4095) | |||||
| Female | 53.8% (4767) | |||||
| Ethnicity: | F(2, 8785) 90.34 ** | F(2, 8786) 26.92 ** | F(2, 8772) 491.16 ** | F(2, 8776) 36.55 ** | F(2, 8786) 15.48 ** | |
| White | 46.5% (4118) | |||||
| Black | 46.7% (4137) | |||||
| Others | 6.0% (534) | |||||
| Education: | F(4, 8848) 12.35 ** | F(4, 8845) 1.98 | F(4, 8829) 8.82 ** | F(4, 8845) 69.65 ** | F(4, 8845) 0.95 | |
| 9th grade | 29.0% (2573) | |||||
| 10th grade | 21.7% (1922) | |||||
| 11th grade | 24.1% (2133) | |||||
| 12th grade | 24.5% (2169) | |||||
| Variables | Year | p-Value | ||||||
|---|---|---|---|---|---|---|---|---|
| 1999 | 2001 | 2003 | 2007 | 2009 | 2011 | |||
| Consumption of fruits and vegetables | N | 1355 | 1501 | 1234 | 1425 | 1638 | 1709 | p < 0.01 ** |
| M | 13.61 | 13.67 | 13.73 | 13.63 | 13.76 | 14.37 | ||
| SD | 5.321 | 5.044 | 5.175 | 5.644 | 5.384 | 5.758 | ||
| Sedentary behavior | N | 1354 | 1500 | 1231 | 1423 | 1633 | 1705 | p < 0.01 ** |
| M | 4.75 | 4.66 | 4.59 | 4.41 | 4.25 | 4.15 | ||
| SD | 1.825 | 1.888 | 1.791 | 1.945 | 1.888 | 1.587 | ||
| Physical activity | N | 1355 | 1501 | 1234 | 1425 | 1638 | 1709 | p < 0.01 ** |
| M | 4.06 | 4.24 | 4.17 | 4.34 | 4.44 | 4.78 | ||
| SD | 2.540 | 2.697 | 2.676 | 2.652 | 2.751 | 2.715 | ||
| Abusive behavior to lose weight | N | 1355 | 1501 | 1234 | 1425 | 1638 | 1709 | p < 0.01 ** |
| M | 0.504 | 0.291 | 0.269 | 0.275 | 0.209 | 0.221 | ||
| SD | 1.122 | 0.653 | 0.628 | 0.596 | 0.535 | 0.555 | ||
| Variable | Adjusted Odds Ratios | 95% Confidence Interval | p-Value |
|---|---|---|---|
| Consumption of fruits and vegetables | 1.00 | (1.00, 1.01) | 0.226 |
| Watching TV | 1.05 | (1.02, 1.07) | 0.001 ** |
| Physical activity | 0.97 | (0.96, 0.99) | 0.003 ** |
| Abusive behavior to lose weight | 1.37 | (1.29, 1.46) | <0.001 ** |
| Age | 0.92 | (0.88, 0.95) | <0.001 ** |
| Ethnicity | |||
| White | |||
| Black | 0.642 | (0.582, 0.709) | <0.001 ** |
| Other | 0.942 | (0.774, 1.147) | 0.553 |
| Sex | |||
| Male | |||
| Female | 1.585 | (1.443, 1.742) | <0.001 ** |
| Year | |||
| 1999 | |||
| 2001 | 0.951 | (0.809, 1.119) | 0.548 |
| 2003 | 0.853 | (0.720, 1.010) | 0.065 |
| 2007 | 0.686 | (0.583, 0.807) | <0.001 ** |
| 2009 | 0.739 | (0.631, 0.867) | <0.001 ** |
| 2011 | 0.760 | (0.649, 0.891) | 0.001 ** |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jang, C.-Y.; Gim, N.-G.; Kim, Y.; Kim, T. Multi-Year Examination of School-Based Programs in Preventing Childhood Obesity: A Case of a State Policy in the U.S. Int. J. Environ. Res. Public Health 2020, 17, 9425. https://doi.org/10.3390/ijerph17249425
Jang C-Y, Gim N-G, Kim Y, Kim T. Multi-Year Examination of School-Based Programs in Preventing Childhood Obesity: A Case of a State Policy in the U.S. International Journal of Environmental Research and Public Health. 2020; 17(24):9425. https://doi.org/10.3390/ijerph17249425
Chicago/Turabian StyleJang, Chang-Yong, Nam-Gyeong Gim, Yoonhee Kim, and TaeEung Kim. 2020. "Multi-Year Examination of School-Based Programs in Preventing Childhood Obesity: A Case of a State Policy in the U.S." International Journal of Environmental Research and Public Health 17, no. 24: 9425. https://doi.org/10.3390/ijerph17249425
APA StyleJang, C.-Y., Gim, N.-G., Kim, Y., & Kim, T. (2020). Multi-Year Examination of School-Based Programs in Preventing Childhood Obesity: A Case of a State Policy in the U.S. International Journal of Environmental Research and Public Health, 17(24), 9425. https://doi.org/10.3390/ijerph17249425





