Prevalence and Associated Factors of Self-Reported Gingival Bleeding: A Multicenter Study in France
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Interview
2.3. Statistical Methods
3. Results
3.1. Characteristics of the Population
3.2. Self-Reported Prevalence of Gingival Bleeding
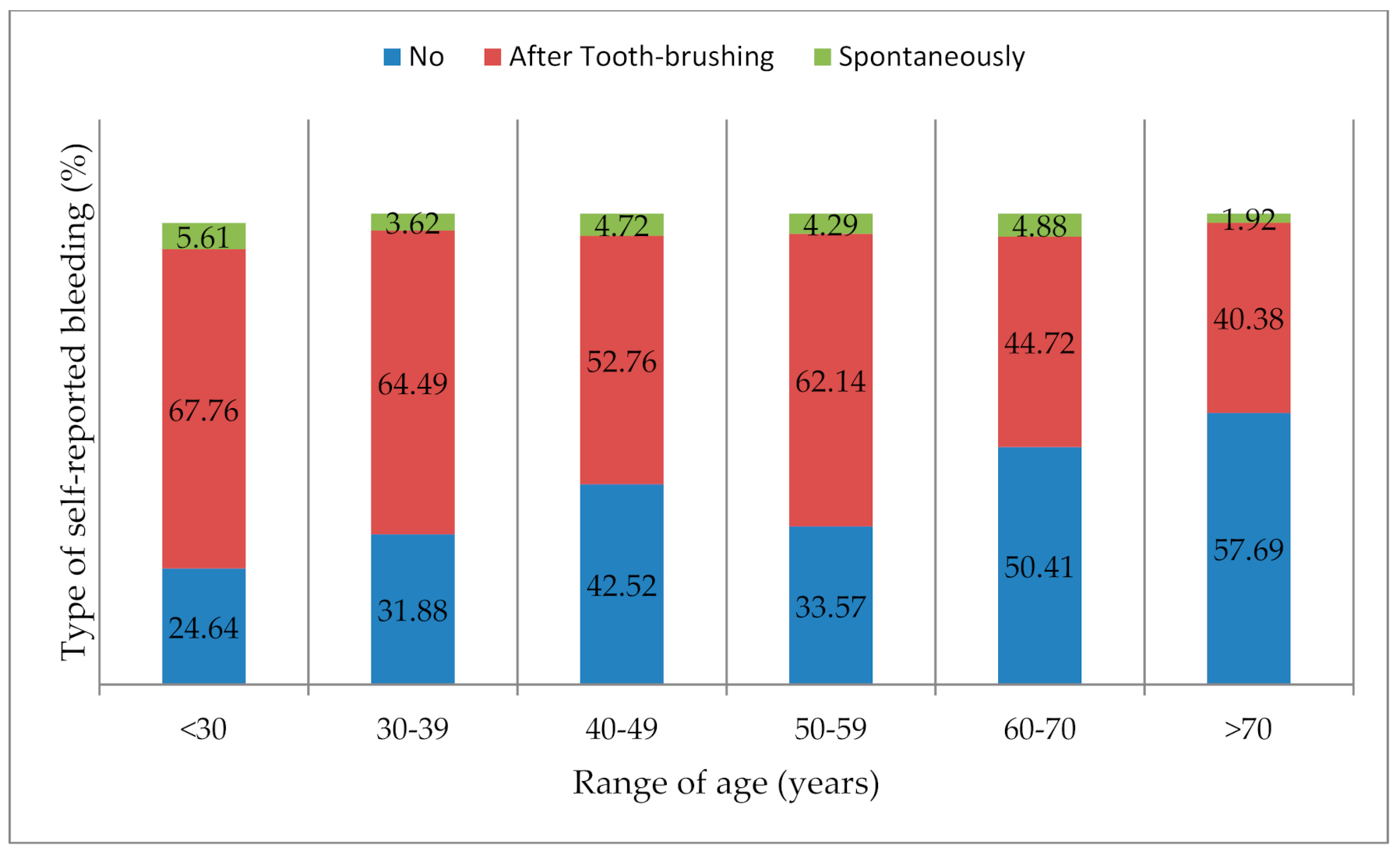
3.3. Factors Associated with Self-Reported Gingival Bleeding
3.3.1. Relationship between GB and Socioeconomic, Medical, and Dental Variables
3.3.2. Relationship between Self-Reported GB and Toothbrushing Variables
3.3.3. Factors Associated with Self-Reported GB
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Appendix A. Material and Method-Interview
Appendix B. Statistical Methods
Appendix C. Results: Characteristics of the Population
Appendix D. Results Self-Reported Gingival Bleeding Prevalence
Appendix E. Relations between Self-Reported GB and the Type and Frequency of Toothbrushing
References
- Marcenes, W.; Kassebaum, N.J.; Bernabé, E.; Flaxman, A.; Naghavi, M.; Lopez, A.; Murray, C.J. Global burden of oral conditions in 1990–2010: A systematic analysis. J. Dent. Res. 2013, 92, 592–597. [Google Scholar] [CrossRef] [PubMed]
- Canton, J.G.; Armitage, G.; Berglundh, T.; Chapple, I.L.C.; Jepsen, S.; Kornman, K.S.; Mealey, B.L.; Papapanou, P.N.; Sanz, M.; Tonetti, M.S. A new classification scheme for periodontal and peri-implant diseases and conditions-Introduction and key changes from the 1999 classification. J. Periodontol. 2018, 89, S1–S8. [Google Scholar] [CrossRef] [PubMed]
- Lang, N.P.; Tonetti, M.S. Periodontal risk assessment (PRA) for patients in supportive periodontal therapy (SPT). Oral Health Prev. Dent. 2003, 1, 7–16. [Google Scholar] [PubMed]
- Zini, A.; Sgan-Cohen, H.D.; Marcenes, W. Socio-economic position, smoking, and plaque: A pathway to severe chronic periodontitis. J. Clin. Periodontol. 2011, 38, 229–235. [Google Scholar] [CrossRef] [PubMed]
- Guentsch, A.; Stier, C.; Raschke, G.F.; Peisker, A.; Fahmy, M.D.; Kuepper, H.; Schueler, I. Oral health and dental anxiety in a German practice-based sample. Clin. Oral Investig. 2017, 21, 1675–1680. [Google Scholar] [CrossRef] [PubMed]
- Kitagawa, M.; Kurahashi, T.; Matsukubo, T. Relationship between general health, lifestyle, oral health and periodontal disease in adults: A large cross-sectional study in Japan. Bull. Tokyo Dent. Coll. 2017, 58, 1–8. [Google Scholar] [CrossRef]
- Bondon-Guitton, E.; Mourgues, T.; Rousseau, V.; Cousty, S.; Cottin, J.; Drablier, G.; Micallef, J.; Montastruc, J.L. Gingival bleeding, a possible “serious” adverse drug reaction: An observational study in the French pharmacovigilance database. J. Clin. Periodontol. 2017, 44, 898–904. [Google Scholar] [CrossRef]
- Bourgeois, D.; Hescot, P.; Doury, J. Periodontal conditions in 35–44-yr-old adults in France, 1993. J. Periodontal Res. 1997, 32, 570–574. [Google Scholar] [CrossRef] [PubMed]
- Bourgeois, D.; Doury, J.; Hescot, P. Periodontal conditions in 65–74-year-old adults in France, 1995. Int. Dent. J. 1999, 49, 182–186. [Google Scholar] [CrossRef] [PubMed]
- Bourgeois, D.; Bouchard, P.; Mattout, C. Epidemiology of periodontal status in dentate adults in France, 2002–2003. J. Periodontal Res. 2007, 42, 219–227. [Google Scholar] [CrossRef]
- Blicher, B.; Joshipura, K.; Eke, P. Validation of self-reported periodontal disease: A systematic review. J. Dent. Res. 2005, 84, 881–891. [Google Scholar] [CrossRef] [PubMed]
- Ramos, R.Q.; Bastos, J.L.; Peres, M.A. Diagnostic validity of self-reported oral health outcomes in population surveys: Literature review. Rev. Bras. Epidemiol. 2013, 16, 716–728. [Google Scholar] [CrossRef] [PubMed]
- Carra, M.C.; Gueguen, A.; Thomas, F.; Pannier, B.; Caligiuri, G.; Steg, P.G.; Zins, M.; Bouchard, P. Self-report assessment of severe periodontitis: Periodontal screening score development. J. Clin. Periodontol. 2018, 45, 818–831. [Google Scholar] [CrossRef] [PubMed]
- Saka-Herrán, C.; Jané-Salas, E.; González-Navarro, B.; Estrugo-Devesa, A.; López-López, J. Validity of a self-reported questionnaire for periodontitis in Spanish population. J. Periodontol. 2020, 91, 1027–1038. [Google Scholar] [CrossRef] [PubMed]
- Vandenbroucke, J.P.; Von Elm, E.; Altman, D.G.; Gøtzsche, P.C.; Mulrow, C.D.; Pocock, S.J.; Poole, C.; Schlesselman, J.J.; Egger, M. Strengthening the Reporting of Observational Studies in Epidemiology (STROBE). Epidemiology 2007, 18, 805–835. [Google Scholar] [CrossRef]
- The PLOS Medicine Editors. Observational Studies: Getting Clear about Transparency. PLoS Med. 2014, 11, 1001711. [Google Scholar] [CrossRef]
- Institut National des Statistiques et des Etudes Economiques (INSEE). 2018. Available online: https://statistiqueslocales.insee.fr/#c=indicator&i=pop_depuis_1876.pop&i2=pop_depuis_1876.dens&s=2016&s2=2016&view=map2 (accessed on 5 March 2020).
- Pinelli, C.; de Castro Monteiro, L.L. Reproducibility and validity of self-perceived oral health conditions. Clin. Oral Investig. 2007, 11, 431–437. [Google Scholar] [CrossRef]
- Gilbert, A.D.; Nuttall, N.M. Self-reporting of Periodontal Health Status. Br. Dent. J. 1999, 186, 241–244. [Google Scholar] [CrossRef]
- Genco, R.J.; Falkner, K.L.; Grossi, S.; Dunford, R.; Trevisan, M. Validity of Self-Reported Measures for Surveillance of Periodontal Disease in Two Western New York Population-Based Studies. J. Periodontol. 2007, 78S7, 1439–1454. [Google Scholar] [CrossRef] [PubMed]
- Rolstad, S.; Adler, J.; Rydén, A. Response burden and questionnaire length: Is shorter better? A review and meta-analysis. Value Health 2011, 14, 1101–1108. [Google Scholar] [CrossRef]
- Sahlqvist, S.; Song, Y.; Bull, F.; Adams, E.; Preston, J.; Ogilvie, D.; iConnect Consortium. Effect of questionnaire length, personalisation and reminder type on response rate to a complex postal survey: Randomised controlled trial. BMC Med. Res. Methodol. 2011, 11, 62. [Google Scholar] [CrossRef] [PubMed]
- Taylor, G.W.; Borgnakke, W.S. Self-reported periodontal disease: Validation in an epidemiological survey. J. Periodontol. 2007, 78S7, 1407–1420. [Google Scholar] [CrossRef] [PubMed]
- Dietrich, T.; Stosch, U.; Dietrich, D.; Schamberger, D.; Bernimoulin, J.P.; Joshipura, K. The accuracy of individual self-reported items to determine periodontal disease history. Eur. J. Oral Sci. 2005, 113, 135–140. [Google Scholar] [CrossRef] [PubMed]
- Vered, Y.; Sgan-Cohen, H.D. Self-perceived and clinically diagnosed dental and periodontal health status among young adults and their implications for epidemiological surveys. BMC Oral Health 2003, 3, 3. [Google Scholar] [CrossRef]
- Yamamoto, T.; Koyama, R.; Tamaki, N.; Maruyama, T.; Tomofuji, T.; Ekuni, D.; Yamanaka, R.; Azuma, T.; Morita, M. Validity of a questionnaire for periodontitis screening of Japanese employees. J. Occup. Health 2009, 51, 137–143. [Google Scholar] [CrossRef]
- Nadanovsky, P.; Dos Santos, A.P.P.; Bloch, K.V. Prevalence of self-reported gingival bleeding in a, representative sample of the Brazilian adolescent population. J. Clin. Periodontol. 2018, 45, 952–958. [Google Scholar] [CrossRef]
- Lintula, T.; Laitala, V.; Pesonen, P.; Sipilä, K.; Laitala, M.L.; Taanila, A.; Anttonen, V. Self-reported oral health and associated factors in the North Finland 1966 birth cohort at the age of 31. BMC Oral Health 2014, 14, 155. [Google Scholar] [CrossRef][Green Version]
- Kim, H.N.; Jang, Y.E.; Kim, C.B.; Kim, N.H. Socioeconomic status and self-reported periodontal symptoms in community-dwelling individuals: Data from the Korea Community Health Surveys of 2011 and 2013. Int. Dent. J. 2018, 68, 411–419. [Google Scholar] [CrossRef]
- Kallio, P.; Uutela, A.; Nordblad, A.; Alvesalo, I.; Murtomaa, H.; Croucher, R. Self-assessed bleeding and plaque as methods for improving gingival health in adolescents. Int. Dent. J. 1997, 47, 205–212. [Google Scholar] [CrossRef]
- Romano, F.; Perotto, S.; Bianco, L.; Parducci, F.; Mariani, G.M.; Aimetti, M. Self-Perception of Periodontal Health and Associated Factors: A Cross-Sectional Population-Based Study. Int. J. Environ. Res. Public Health 2020, 17, 2758. [Google Scholar] [CrossRef]
- Bruers, J.J.; van Rossum, G.M. Dental care frequency of female patients in the Netherlands. Ned. Tijdschr. Tandheelkd. 1998, 105, 412–415. [Google Scholar] [PubMed]
- Zachariasen, R.D. Ovarian hormones and gingivitis. J. Dent. Hygiene 1991, 65, 146–150. [Google Scholar]
- Buhlin, K.; Gustafsson, A.; Andersson, K.; Håkansson, J.; Klinge, B. Validity and Limitations of Self-Reported Periodontal Health. Community Dent. Oral Epidemiol. 2002, 30, 431–437. [Google Scholar] [CrossRef] [PubMed]
- Ebersole, J.L.; Graves, C.L.; Gonzalez, O.A.; Dawson, D.; Morford, L.A.; Huja, P.E.; Hartsfield, J.K., Jr.; Huja, S.S.; Pandruvada, S.; Wallet, S.M. Aging, inflammation, immunity and periodontal disease. Periodontology 2016, 72, 54–75. [Google Scholar] [CrossRef] [PubMed]
- Kawachi, I.; Kennedy, B.P. Income inequality and health: Pathways and mechanisms. Health Serv. Res. 1999, 34, 215–227. [Google Scholar] [PubMed]
- Braveman, P.A.; Cubbin, C.; Egerter, S.; Chideya, S.; Marchi, K.S.; Metzler, M.; Posner, S. Socioeconomic status in health research: One size does not fit all. JAMA 2005, 294, 2879–2888. [Google Scholar] [CrossRef] [PubMed]
- Tack, D.A.; Rogers, R.S. Oral drug reactions. Dermatol. Ther. 2002, 15, 236–250. [Google Scholar] [CrossRef]
- Bascones-Martinez, A.; Muñoz-Corcuera, M.; Bascones-Ilundain, C. Side effects of drugs on the oral cavity. Med. Clin. 2015, 144, 126–131. [Google Scholar] [CrossRef]
- Dietrich, T.; Ower, P.; Tank, M.; West, N.X.; Walter, C.; Needleman, I.; Hughes, F.J.; Wadia, R.; Milward, M.R.; Hodge, P.J.; et al. Periodontal diagnosis in the context of the 2017 classification system of periodontal diseases and conditions-implementation in clinical practice. Br. Dent. J. 2019, 226, 16–22. [Google Scholar] [CrossRef]
- Müller, H.P.; Heinecke, A.; Eger, T. Site-specific association between supragingival plaque and bleeding upon probing in young adults. Clin. Oral Investig. 2000, 4, 212–218. [Google Scholar] [CrossRef]
- Mullally, B.H. The influence of tobacco smoking on the onset of periodontitis in young Persons. Tob. Induc. Dis. 2004, 2, 53–65. [Google Scholar] [CrossRef] [PubMed]
- Al-Bayaty, F.H.; Baharuddin, N.; Abdulla, M.A.; Ali, H.M.; Arkilla, M.B.; Al-Bayaty, M.F. The influence of cigarette smoking on gingival bleeding and serum concentrations of haptoglobin and Alpha 1-Antitrypsin. Biomed. Res. Int. 2013, 2013, 684154. [Google Scholar] [CrossRef] [PubMed]
- Müller, H.P.; Stadermann, S.; Heinecke, A. Gingival recession in smokers and non-smokers with minimal periodontal disease. J. Clin. Periodontol. 2002, 29, 129–136. [Google Scholar] [CrossRef] [PubMed]
- Müller, H.P.; Stadermann, S. Multivariate multilevel models for repeated measures in the study of smoking effects on the association between plaque and gingival bleeding. Clin. Oral Investig. 2006, 10, 311–316. [Google Scholar] [CrossRef] [PubMed]
- Akcali, A.; Huck, O.; Tenenbaum, H.; Davideau, J.L.; Buduneli, N. Periodontal diseases and stress: A brief review. J. Oral Rehabil. 2013, 40, 60–68. [Google Scholar] [CrossRef]
- Herrera, D.; Alonso, B.; de Arriba, L.; Santa Cruz, I.; Serrano, C.; Sanz, M. Acute periodontal lesions. Periodontology 2014, 65, 149–177. [Google Scholar] [CrossRef] [PubMed]
- Breivik, T.; Thrane, P.S.; Murison, R.; Gjermo, P. Emotional stress effects on immunity, gingivitis and periodontitis. Eur. J. Oral Sci. 1996, 104, 327–334. [Google Scholar] [CrossRef]
- Hugo, F.N.; Hilgert, J.B.; Bozzetti, M.C.; Bandeira, D.R.; Gonçalves, T.R.; Pawlowski, J.; de Sousa, M.L. Chronic stress, depression, and cortisol levels as risk indicators of elevated plaque and gingivitis levels in individuals aged 50 years and older. J. Periodontol. 2006, 77, 1008–1014. [Google Scholar] [CrossRef]
- Deinzer, R.; Rüttermann, S.; Möbes, O.; Herforth, A. Increase in gingival inflammation under academic stress. J. Clin. Periodontol. 1998, 25, 431–433. [Google Scholar] [CrossRef]
- Ravishankar, T.L.; Ain, T.S.; Gowhar, O. Effect of academic stress on plaque and gingival health among dental students of Moradabad, India. J. Int. Acad. Periodontol. 2014, 16, 115–120. [Google Scholar]
- Ueno, M.; Shimazu, T.; Sawada, N.; Tsugane, S.; Kawaguchi, Y. Validity of Self-Reported Periodontitis in Japanese Adults: The Japan Public HealthCenter–Based Prospective Study for the Next-Generation Oral Health Study. Asia Pac. J. Public Health 2020, 32, 346–353. [Google Scholar] [CrossRef] [PubMed]
- Walsh, M.M.; Heckman, B.H.; Moreau-Diettinger, R. Use of gingival bleeding for reinforcement of oral home care behavior. Community Dent Oral Epidemiol. 1985, 13, 133–135. [Google Scholar] [CrossRef] [PubMed]
- Corah, N.L. Development of a dental anxiety scale. J. Dent. Res. 1969, 48, 596. [Google Scholar] [CrossRef] [PubMed]
- Nicolas, E.; Collado, V.; Faulks, D.; Bullier, B.; Hennequin, M. A national cross-sectional survey of dental anxiety in the French adult population. BMC Oral Health 2007, 7, 12. [Google Scholar] [CrossRef] [PubMed]
- Peduzzi, P.; Concato, J.; Kemper, E.; Holford, T.R.; Feinstein, A.R. A simulation study of the number of events per variable in logistic regression analysis. J. Clin. Epidemiol. 1996, 49, 1973–1979. [Google Scholar] [CrossRef]
| Sociodemographic and Dental Characteristics | Total N = 794 | Preventive Medicine | Railway Station or Mall | ||||
|---|---|---|---|---|---|---|---|
| N = 399 (50.3%) | N = 395 (49.7%) | ||||||
| N | % | N | % | N | % | p * | |
| Age (class) | 0.039 | ||||||
| 18–40 years | 367 | 46.2 | 198 | 54.0 | 169 | 46.0 | |
| 41–60 years | 267 | 33.6 | 134 | 50.2 | 133 | 49.8 | |
| >60 years | 160 | 20.2 | 67 | 41.9 | 93 | 58.1 | |
| Sex | 0.40 | ||||||
| Male | 376 | 47.4 | 183 | 48.7 | 193 | 51.3 | |
| Female | 418 | 52.6 | 216 | 51.7 | 202 | 48.3 | |
| Smoker | 0.0032 | ||||||
| No | 558 | 70.3 | 266 | 47.7 | 292 | 52.3 | |
| Yes <10 cig/day | 130 | 16.4 | 83 | 63.8 | 47 | 36.2 | |
| >10 cig/day | 106 | 13.4 | 50 | 47.2 | 56 | 52.8 | |
| Education level (class) | 0.0001 | ||||||
| None/low level | 280 | 35.3 | 169 | 60.4 | 111 | 39.6 | |
| Medium level | 143 | 18.0 | 61 | 42.7 | 82 | 57.3 | |
| High level | 371 | 46.7 | 169 | 45.6 | 202 | 54.4 | |
| Occupation (class) | 0.001 | ||||||
| None, unemployed, student, other | 233 | 29.3 | 123 | 52.8 | 110 | 47.2 | |
| Retired | 141 | 17.8 | 55 | 39.0 | 86 | 61.0 | |
| Manual worker, employee, artisan, retailer, administrative | 301 | 37.9 | 171 | 56.8 | 130 | 43.2 | |
| Teachers, liberal profession, executive | 119 | 15.0 | 50 | 42.0 | 69 | 58.0 | |
| Type of toothbrush | 0.082 | ||||||
| Unknown | 84 | 10.6 | 44 | 52.4 | 40 | 47.6 | |
| Soft | 272 | 34.3 | 120 | 44.1 | 152 | 55.9 | |
| Medium | 328 | 41.3 | 173 | 52.7 | 155 | 47.3 | |
| Hard | 110 | 13.9 | 62 | 56.4 | 48 | 43.6 | |
| Technique of toothbrushing (class) | 0.085 | ||||||
| Horizontal | 151 | 19.0 | 75 | 49.7 | 76 | 50.3 | |
| Vertical | 242 | 30.5 | 107 | 44.2 | 135 | 55.8 | |
| Circular brushing | 172 | 21.7 | 89 | 51.7 | 83 | 48.3 | |
| Combination of at least 2 techniques | 229 | 28.8 | 128 | 55.9 | 101 | 44.1 | |
| Frequency of toothbrushing (class) | 0.038 | ||||||
| ≤1 time/day | 172 | 21.7 | 101 | 58.7 | 71 | 41.3 | |
| 2 times/day | 466 | 58.7 | 226 | 48.5 | 240 | 51.5 | |
| 3 times/day | 156 | 19.6 | 72 | 46.2 | 84 | 53.8 | |
| Self-Reported Gingival Bleeding * | N | % | |
|---|---|---|---|
| No | 292 | 36.8 | |
| Yes | 502 | 63.2 | |
| After toothbrushing | 466 | 58.7 | |
| Spontaneously | 33 | 4.5 | |
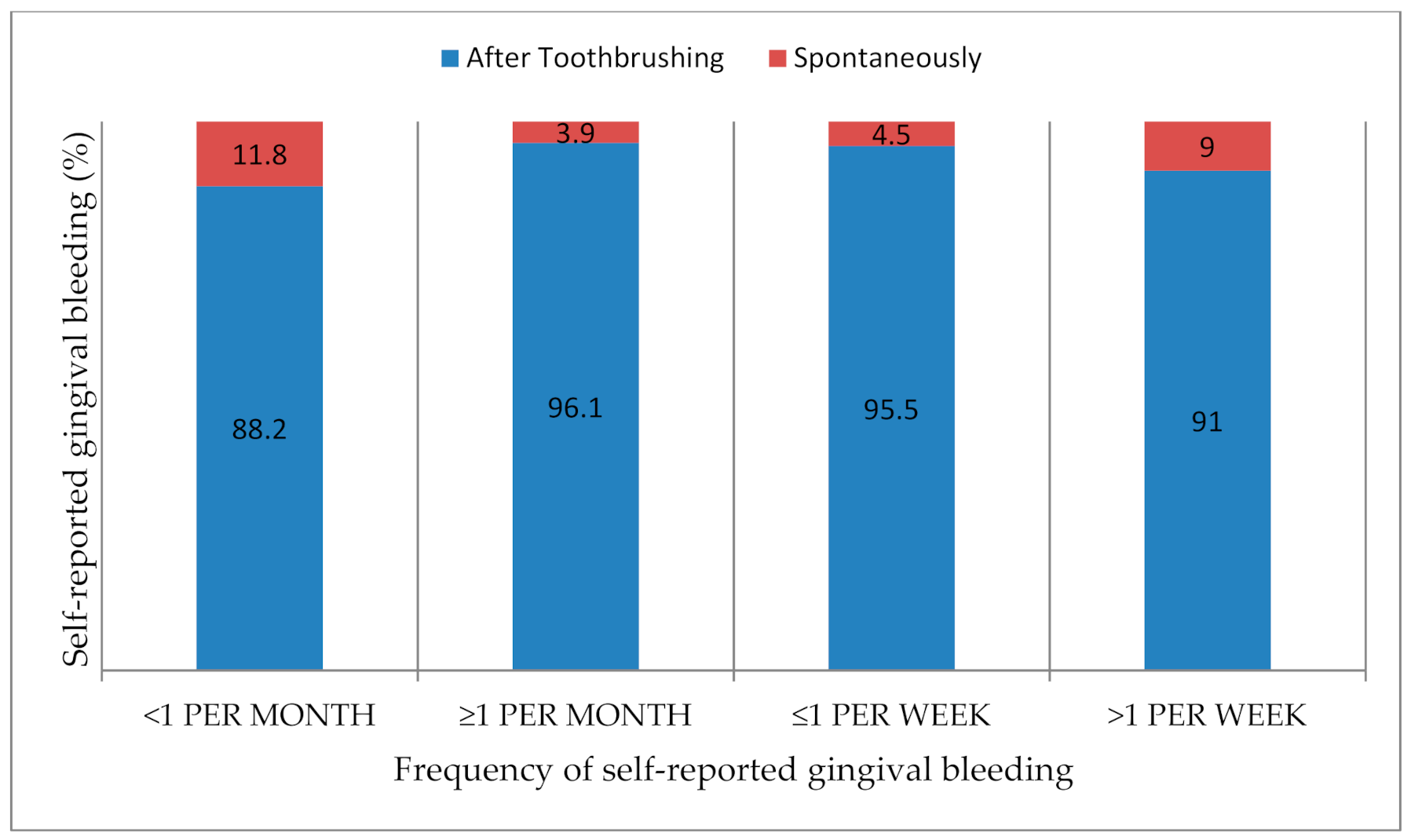
| Frequency of self-reported gingival bleeding (class) | |||
| No | 292 | ||
| Yes <1 per month | 136 | 27.1 | |
| ≥1 per month | 155 | 30.9 | |
| ≤1 per week | 111 | 22.1 | |
| >1 per week | 100 | 19.9 | |
| Self-reported gingival bleeding (women N = 418) | |||
| No bleeding | 140 | 33.5 | |
| Hormonal bleeding ** | No | 226 | 54.1 |
| Yes | 52 | 18.7 | |
| Total N = 794 | Preventive Medicine N = 399 (50.3%) | Railway and Mall N = 395 (49.7%) | p * | ||||
|---|---|---|---|---|---|---|---|
| N | % | N | % | N | % | ||
| Self-reported gingival bleeding | |||||||
| No | 292 | 36.8 | 116 | 39.7 | 176 | 60.3 | <0.0001 |
| Yes | 502 | 63.2 | 283 | 56.4 | 219 | 43.6 | |
| Frequency of self-reported GB among people bleeding (Class) | |||||||
| <1 per month | 136 | 27.1 | 85 | 62.5 | 51 | 37.5 | 0.28 |
| ≥1 per month | 155 | 30.9 | 80 | 51.6 | 75 | 48.4 | |
| ≤1 per week | 111 | 22.1 | 64 | 57.7 | 47 | 42.3 | |
| >1 per week | 100 | 19.9 | 54 | 54.0 | 46 | 46.0 | |
| Self-reported hormonal bleeding among women with bleeding | |||||||
| No | 226 | 81.3 | 133 | 58.9 | 93 | 41.2 | 0.09 |
| Yes | 52 | 18.7 | 24 | 46.2 | 28 | 53.9 | |
| Sociodemographic Characteristics and Drug Information | Total | Self-Reported Gingival Bleeding | |||||
|---|---|---|---|---|---|---|---|
| N = 794 | No N = 292 (36.8%) | Yes N = 502 (63.2%) | |||||
| N | % | N | % | N | % | p * | |
| Age (class) | <0.0001 | ||||||
| 18–40 years | 367 | 46.2 | 107 | 29.2 | 260 | 70.8 | |
| 41–60 years | 267 | 33.6 | 98 | 36.7 | 169 | 63.3 | |
| >60 years | 160 | 20.2 | 87 | 54.4 | 73 | 45.6 | |
| Sex | 0.043 | ||||||
| Male | 376 | 47.4 | 152 | 40.4 | 224 | 59.6 | |
| Female | 418 | 52.6 | 140 | 33.5 | 278 | 66.5 | |
| Smokers | 0.19 | ||||||
| No | 558 | 70.3 | 196 | 35.1 | 362 | 64.9 | |
| Yes <10 cig/day | 130 | 16.4 | 49 | 37.7 | 81 | 62.3 | |
| >10 cig/day | 106 | 13.4 | 47 | 44.3 | 59 | 55.7 | |
| Education level | 0.78 | ||||||
| None/low level | 280 | 35.3 | 101 | 36.1 | 179 | 63.9 | |
| Medium level | 143 | 18.0 | 50 | 35.0 | 93 | 65.0 | |
| High level | 371 | 46.7 | 141 | 38.0 | 230 | 62.0 | |
| Occupations | <0.0001 | ||||||
| None, unemployed, student, other | 233 | 29.3 | 68 | 29.2 | 165 | 70.8 | |
| Retired | 141 | 17.8 | 74 | 52.5 | 67 | 47.5 | |
| Manual worker, employee, artisan, retailer, administrative | 301 | 37.9 | 96 | 31.9 | 205 | 68.1 | |
| Teacher, liberal profession, executive | 119 | 15.0 | 54 | 45.4 | 65 | 54.6 | |
| Medicines with hemorragic risk (oral anticoagulant/PAA/AVK/heparin/NSAID) | 0.87 | ||||||
| No | 733 | 92.3 | 269 | 36.7 | 464 | 63.3 | |
| Yes | 61 | 7.7 | 23 | 37.7 | 38 | 62.3 | |
| Anxiolytic or antidepressant drugs | 0.067 | ||||||
| No | 765 | 96.3 | 286 | 37.4 | 479 | 62.6 | |
| Yes | 29 | 3.7 | 6 | 20.7 | 23 | 79.3 | |
| Cholesterol-lowering | 0.16 | ||||||
| No | 749 | 94.3 | 271 | 36.2 | 478 | 63.8 | |
| Yes | 45 | 5.7 | 21 | 46.7 | 24 | 53.3 | |
| Anti-hypertensive drugs | 0.39 | ||||||
| No | 719 | 90.6 | 261 | 36.3 | 458 | 63.7 | |
| Yes | 75 | 9.4 | 31 | 41.3 | 44 | 58.7 | |
| Anxiety (class) | 0.0004 | ||||||
| No anxiety | 438 | 55.2 | 185 | 42.2 | 253 | 57.8 | |
| Moderate | 197 | 24.8 | 67 | 34.0 | 130 | 66.0 | |
| High/severe | 159 | 20.0 | 40 | 25.2 | 119 | 74.8 | |
| Covariables | Odds-Ratio Confidence Limits | p-Value |
|---|---|---|
| Occupation | <0.0001 | |
| None, unemployed, student, other | 2.1 [1.3; 3.4] | |
| Retired | 0.7 [0.4; 1.1 | |
| Manual worker, employee, artisan, retailer, administrative | 1.8 [1.1; 2.8] | |
| Teacher, liberal profession, executive | 1 | |
| Smoking status | 0.0012 | |
| No | 1 | |
| Yes | 0.6 [0.4; 0.8] | |
| Brushing frequency | 0.0047 | |
| ≤2 times/day | 1.7 [1.2; 2.5] | |
| 3 times/day | 1 | |
| Anxiety level | 0.0031 | |
| No anxiety | 1 | |
| Moderate | 1.3 [0.9; 1.9] | |
| High/severe | 2.0 [1.3; 3.1] |
| Covariables | Spontaneous GB vs. Lack GB Odds-Ratio Confidence Limits | Toothbrushing GB vs. Lack GB Odds-Ratio Confidence Limits | p-Value |
|---|---|---|---|
| Occupation | <0.0001 | ||
| None, unemployed, student, other | 4.0 [0.8; 19.3] | 2.0 [1.3; 3.3] | |
| Retired | 1.8 [0.3; 9.6] | 0.6 [0.4; 1.1] | |
| Manual worker, employee, artisan, retailer, administrative | 5.1 [1.1; 22.9] | 1.7 [1.1; 2.6] | |
| Teacher, liberal profession, executive | 1 | 1 | |
| Smoking status | 0.0036 | ||
| No | 1 | 1 | |
| Yes | 0.8 [0.4; 1.7] | 0.6 [0.4; 0.8] | |
| Brushing frequency | 0.0065 | ||
| ≤2 times/day | 5.5 [1.3;23.7] | 1.6 [1.1;2.3] | |
| 3 times/day | 1 | 1 | |
| Anxiety level | 0.0130 | ||
| No anxiety | 1 | 1 | |
| Moderate | 0.9 [0.4;2.4] | 1.3 [0.9;1.9] | |
| High/severe | 2.4 [1.1; 5.6] | 2.0 [1.3; 3.1] |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Veynachter, T.; Orti, V.; Moulis, E.; Rousseau, H.; Thilly, N.; Anagnostou, F.; Jeanne, S.; Bisson, C. Prevalence and Associated Factors of Self-Reported Gingival Bleeding: A Multicenter Study in France. Int. J. Environ. Res. Public Health 2020, 17, 8563. https://doi.org/10.3390/ijerph17228563
Veynachter T, Orti V, Moulis E, Rousseau H, Thilly N, Anagnostou F, Jeanne S, Bisson C. Prevalence and Associated Factors of Self-Reported Gingival Bleeding: A Multicenter Study in France. International Journal of Environmental Research and Public Health. 2020; 17(22):8563. https://doi.org/10.3390/ijerph17228563
Chicago/Turabian StyleVeynachter, Thomas, Valérie Orti, Estelle Moulis, Hélène Rousseau, Nathalie Thilly, Fani Anagnostou, Sylvie Jeanne, and Catherine Bisson. 2020. "Prevalence and Associated Factors of Self-Reported Gingival Bleeding: A Multicenter Study in France" International Journal of Environmental Research and Public Health 17, no. 22: 8563. https://doi.org/10.3390/ijerph17228563
APA StyleVeynachter, T., Orti, V., Moulis, E., Rousseau, H., Thilly, N., Anagnostou, F., Jeanne, S., & Bisson, C. (2020). Prevalence and Associated Factors of Self-Reported Gingival Bleeding: A Multicenter Study in France. International Journal of Environmental Research and Public Health, 17(22), 8563. https://doi.org/10.3390/ijerph17228563





