Analysis of Emergency Department Visits and Hospital Activity during Influenza Season, COVID-19 Epidemic, and Lockdown Periods in View of Managing a Future Disaster Risk: A Multicenter Observational Study
Abstract
1. Introduction
2. Methods
2.1. Study Design and Setting
2.2. Definitions and Outcomes
2.3. Ethics Statement
2.4. Analysis
3. Results
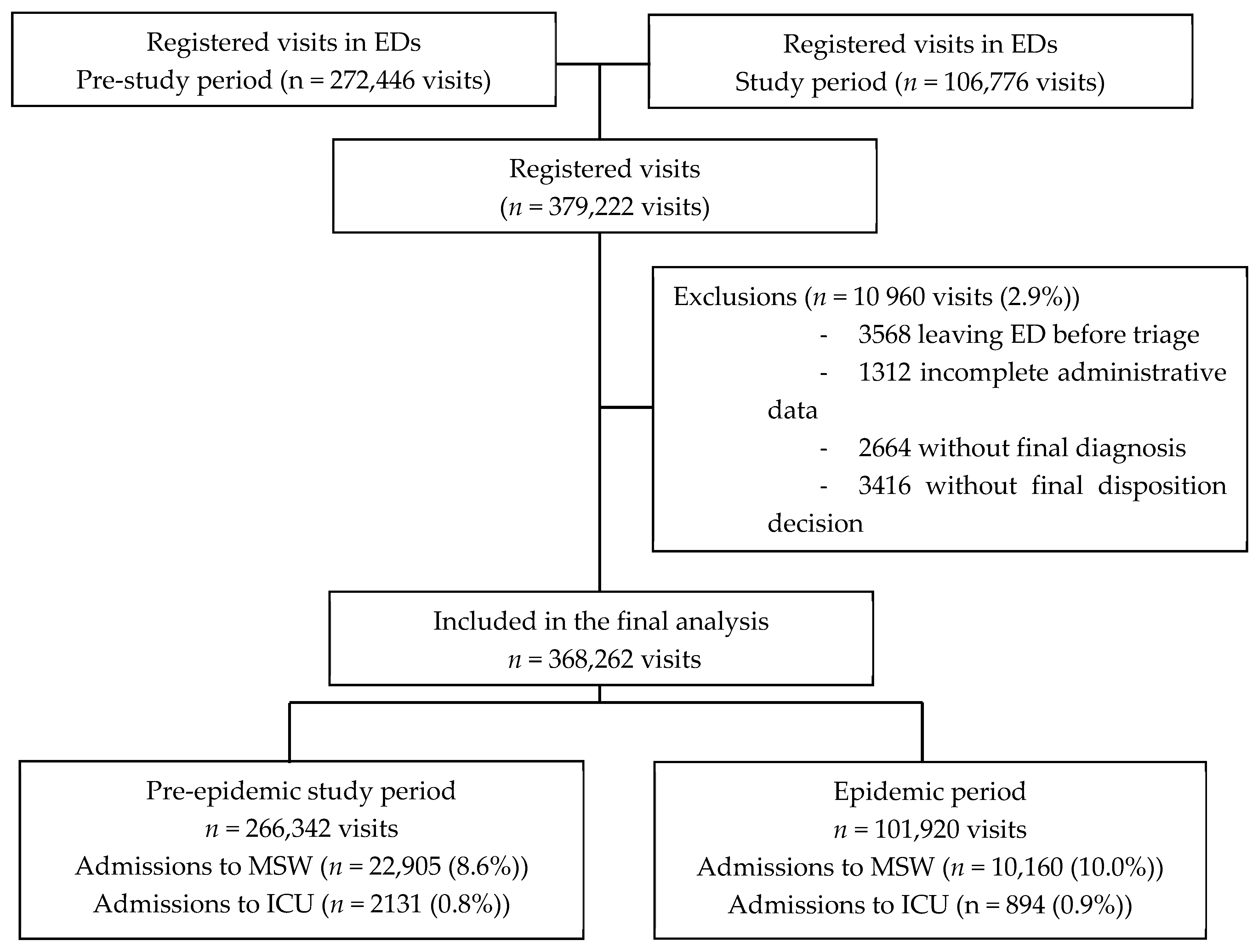
3.1. Trends in ED Visits and Through-ED Admissions to MSW and ICU
3.2. Impact of Influenza, COVID-19 Epidemic, and Lockdown on ED and through-ED Admissions to MSW and ICU
3.3. Multifaceted Analysis Model: Predictors of Daily ED Visits and through-ED Admissions to MSW and ICU
3.4. Trends on ED Main Characteristics and Diagnosis Groups
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Appendix A

References
- Sohrabi, C.; Alsafi, Z.; O’Neill, N.; Khan, M.; Kerwan, A.; Al-Jabir, A.; Iosifidis, C.; Agha, R. World Health Organization declares global emergency: A review of the 2019 novel coronavirus (COVID-19). Int. J. Surg. 2020, 76, 71–76. [Google Scholar] [CrossRef]
- World Economic Forum. The Economic, Geopolitical and Health Consequences of COVID-19. 2012. Available online: https://www.weforum.org/agenda/2020/03/the-economic-geopolitical-and-health-consequences-of-covid-19/ (accessed on 24 September 2020).
- Elston, J.W.; Cartwright, C.; Ndumbi, P.; Wright, J. The health impact of the 2014-15 Ebola outbreak. Public Health 2017, 143, 60–70. [Google Scholar] [CrossRef]
- McQuilkin, P.A.; Udhayashankar, K.; Niescierenko, M.; Maranda, L. Health-Care Access during the Ebola Virus Epidemic in Liberia. Am. J. Trop. Med. Hygiene 2017, 97, 931–936. [Google Scholar] [CrossRef] [PubMed]
- Wilhelm, J.A.; Helleringer, S. Utilization of non-Ebola health care services during Ebola outbreaks: A systematic review and meta-analysis. J. Glob. Health 2019, 9, 010406. [Google Scholar] [CrossRef] [PubMed]
- Vygen, S.; Tiffany, A.; Rull, M.; Ventura, A.; Wolz, A.; Jambai, A.; Porten, K. Changes in Health-Seeking Behavior Did Not Result in Increased All-Cause Mortality During the Ebola Outbreak in Western Area, Sierra Leone. Am. J. Trop. Med. Hyg. 2016, 95, 897–901. [Google Scholar] [CrossRef] [PubMed]
- Giamello, J.D.; Abram, S.; Bernardi, S.; Lauria, G. The emergency department in the COVID-19 era. Who are we missing? Eur. J. Emerg. Med. 2020. [Google Scholar] [CrossRef]
- Westgard, B.C.; Morgan, M.W.; Vazquez, G.-B.; Erickson, L.O.; Zwank, M.D. An analysis of changes in emergency department visits after a state declaration during the time of COVID-19. Ann. Emerg. Med. 2020, 76, 595–601. [Google Scholar] [CrossRef]
- Hartnett, K.P.; Kite-Powell, A.; DeVies, J.; Coletta, M.A.; Boehmer, T.K.; Adjemian, J.; Gundlapalli, A.V.; National Syndromic Surveillance Program Community of Practice. Impact of the COVID-19 Pandemic on Emergency Department Visits—United States, January 1, 2019–May 30, 2020. MMWR Morb. Mortal. Wkly. Rep. 2020, 69, 699–704. [Google Scholar] [CrossRef]
- Mantica, G.; Riccardi, N.; Terrone, C.; Gratarola, A. Non-COVID-19 visits to emergency departments during the pandemic: The impact of fear. Public Health 2020, 183, 40–41. [Google Scholar] [CrossRef]
- Lien, W.C.; Wu, J.L.; Tseng, W.P.; Ko, P.C.-I.; Chen, S.Y.; Tsai, M.S.; Chang, W.T.; Huang, C.H.; Chen, S.C. Fight COVID-19 Beyond the Borders: Emergency Department Patient Diversion in Taiwan. Ann. Emerg. Med. 2020, 75, 785–787. [Google Scholar] [CrossRef]
- Hautz, W.E.; Sauter, T.C.; Exadakytlos, A.K.; Krummrey, G.; Schauber, S.; Müller, M. Barriers to seeking emergency care during the COVID-19 pandemic may lead to higher morbidity and mortality—A retrospective study from a Swiss university hospital. Swiss Med. Wkly. 2020, 150, 20331. [Google Scholar] [CrossRef] [PubMed]
- Nuñez, J.H.; Sallent, A.; Lakhani, K.; Guerra-Farfana, E.; Vidala, N.; Ekhtiarid, S.; Minguell, J. Impact of the COVID-19 Pandemic on an Emergency Traumatology Service: Experience at a Tertiary Trauma Centre in Spain. Injury 2020, 51, 1414–1418. [Google Scholar] [CrossRef] [PubMed]
- Madanelo, M.; Ferreira, C.; Nunes, D.-C.; Pinto, A.; Rocha, M.A.; Correia, J.; Teixeira, B.; Mendes, G.; Tavares, C.; Mesquita, S.; et al. The impact of the coronavirus disease 2019 pandemic on the utilisation of emergency urological services. BJU Int. 2020, 126, 256–258. [Google Scholar] [CrossRef] [PubMed]
- Cano, O.-V.; Morales, X.; Ferrigni, C.J.; Martín, E.-A.; Turrado, V.; García, A.; Cuñarro, Y.-L.; Zarain, L.-O.; Duran, M.-P.; Balibrea, J.M.; et al. Reduction in emergency surgery activity during COVID-19 pandemic in three Spanish hospitals. Br. J. Surg. 2020, 107, e239. [Google Scholar] [CrossRef] [PubMed]
- Metzler, B.; Siostrzonek, P.; Binder, R.K.; Bauer, A.; Reinstadler, S.J. Decline of acute coronary syndrome admissions in Austria since the outbreak of COVID-19: The pandemic response causes cardiac collateral damage. Eur. Heart. J. 2020, 41, 1852–1853. [Google Scholar] [CrossRef]
- Santé Publique France. Bulletin épidémiologique grippe. Saison 2019–2020. Paris; Ministère de la Santé. 18 March 2020. Available online: https://www.santepubliquefrance.fr/maladies-et-traumatismes/maladies-a-prevention-vaccinale/grippe/donnees/#tabs (accessed on 24 September 2020).
- Nielsen, J.; Vestergaard, L.S.; Richter, L.; Schmid, D.; Bustos, N.; Asikainen, T.; Trebbien, R.; Denissov, G.; Innos, K.; Virtanen, M.J.; et al. European all-cause excess and influenza-attribuTable mortality in the 2017/18 season: Should the burden of influenza B be reconsidered? Clin. Microbiol. Infect. 2019, 25, 1266–1276. [Google Scholar] [CrossRef]
- Menec, V.H.; Black, C.; MacWilliam, L.; Aoki, F.; Peterson, S.; Friesen, D. The Impact of Influenza-Like Illness on the Winnipeg Health Care System: Is an Early Warning System Possible? Manitoba Centre for Health Policy and Evaluation. March 2001. Available online: http://mchp-appserv.cpe.umanitoba.ca/reference/flu-like.pdf (accessed on 24 September 2020).
- Menec, V.H.; Black, C.; MacWilliam, L.; Aoki, F. The impact of influenza-associated respiratory illnesses on hospitalizations, physician visits, emergency room visits, and mortality. Can. J. Public Health 2003, 94, 59–63. [Google Scholar] [CrossRef]
- Rosano, A.; Bella, A.; Gesualdo, F.; Acampora, A.; Pezzotti, P.; Marchetti, S.; Ricciardi, W.; Rizzo, C. Investigating the impact of influenza on excess mortality in all ages in Italy during recent seasons (2013/14-2016/17 seasons). Int. J. Infect. Dis. 2019, 88, 127–134. [Google Scholar] [CrossRef]
- Jeffery, M.M.; D’Onofrio, G.; Paek, H.; Platts-Mills, T.F.; Soares, W.E.; Hoppe, J.A.; Genes, N.; Nath, B.; Melnick, E.R. Trends in Emergency Department Visits and Hospital Admissions in Health Care Systems in 5 States in the First Months of the COVID-19 Pandemic in the US. JAMA Intern. Med. 2020, 180, 1328–1333. [Google Scholar] [CrossRef]
- Birkmeyer, J.D.; Barnato, A.; Birkmeyer, N.; Bessler, R.; Skinner, J. The Impact of The COVID-19 Pandemic On Hospital Admissions In The United States. Health Aff. 2020, 2020. [Google Scholar] [CrossRef]
- Song, X.; Delaney, M.; Shah, R.K.; Campos, J.M.; Wessel, D.L.; DeBiasi, R.L. Comparison of Clinical Features of COVID-19 vs Seasonal Influenza A and B in US Children. JAMA Netw. Open 2020, 3, e2020495. [Google Scholar] [CrossRef] [PubMed]
- Institut National de la Statistique et des Etudes Economiques (INSEE). The Consequences of the COVID-19 Health Crisis. Economic, Demographic and Societal Impacts (Les Conséquences de la Crise Sanitaire du Covid-19. Impacts Économiques, Démographiques et Sociétaux); Montrouge. 18 May 2020. Available online: https://www.insee.fr/fr/information/4479280 (accessed on 31 August 2020).
- Di Domenico, L.; Pullano, G.; Sabbatini, C.E.; Boëlle, P.Y.; Colizza, V. Impact of lockdown on COVID-19 epidemic in Île-de-France and possible exit strategies. BMC Med. 2020, 18, 240. [Google Scholar] [CrossRef] [PubMed]
- Santé Publique France. Bulletin épidémiologique du Covid-19. Paris; Ministère de la santé, 13 March 2020. Available online: https://www.santepubliquefrance.fr/presse/2020/surveillance-epidemiologique-du-covid-19 (accessed on 24 September 2020).
- Info Coronavirus Covid 19—Carte et Donnees Covid 19 en France; Données au. 27 October 2020. Available online: https://www.gouvernement.fr/info-coronavirus/carte-et-donnees (accessed on 28 October 2020).
- Bouzid, D.; Lucet, J.C.; Duval, X.; Houhou-Fidouh, N.; Casalino, E.; Visseaux, B. ED Influenza Management Study Group. Multiplex PCR implementation as point-of-care testing in a French emergency department. J. Hosp. Infect. 2020, 105. [Google Scholar] [CrossRef] [PubMed]
- Visseaux, B.; Le Hingrat, Q.; Collin, G.; Bouzid, D.; Lebourgeois, S.; Le Pluart, D.; Deconinck, L.; Lescure, F.X.; Lucet, J.C.; Bouadma, L.; et al. Evaluation of the QIAstat-Dx Respiratory SARS-CoV-2 Panel, the First Rapid Multiplex PCR Commercial Assay for SARS-CoV-2 Detection. J. Clin. Microbiol. 2020, 58, e00630-20. [Google Scholar] [CrossRef]
- Murray, M.J. The Canadian Triage and Acuity Scale: A Canadian perspective on emergency department triage. Emerg. Med. 2003, 15, 6–10. [Google Scholar] [CrossRef]
- Casalino, E.; Antoniol, S.; Fidouh, N.; Choquet, C.; Lucet, J.-C.; Duval, X.; Visseaux, B.; Pereira, L. Influenza virus infections among patients attending emergency department according to main reason to presenting to ED: A 3-year prospective observational study during seasonal epidemic periods. PLoS ONE 2017, 12, e0182191. [Google Scholar] [CrossRef]
- Wang, J.; Zhu, X.; Xu, Z.; Yang, G.; Mao, G.; Jia, Y.; Xie, Z.; Wang, J.; Ao, W.-Q. Clinical and CT findings of COVID-19: Differences among three age groups. BMC Infect. Dis. 2020, 20, 1–11. [Google Scholar] [CrossRef]
- Box, G.E.P.; Tiao, G.C. Intervention analysis with applications to economic and environmental problems. J. Am. Stat. Assoc. 1975, 70, 70–92. [Google Scholar] [CrossRef]
- Cochrane Effective Practice and Organisation of Care (EPOC). Interrupted Time Series (ITS) Analyses (plus SPSS Time Series Analysis). EPOC Resources for Review Authors, 2017; Norwegian Institute of Public Health: Oslo, Norway, 2017. Available online: https://epoc.cochrane.org/resources/epoc-resources-review-authors (accessed on 24 September 2020).
- Beard, E.; Marsden, J.; Brown, J.; Tombor, I.; Stapleton, J.; Michie, S.; West, R. Understanding and using time series analyzes in addiction research. Addiction 2019, 114, 1866–1884. [Google Scholar] [CrossRef]
- Ramsay, C.R.; Matowe, L.; Grilli, R.; Grimshaw, J.M.; Thomas, R.E. Interrupted time series designs in health technology assessment: Lessons from two systematic reviews of behavior change strategies. Int. J. Technol. Assess. Health Care 2003, 19, 613–623. [Google Scholar] [CrossRef]
- Hiller, K.M.; Stoneking, L.; Min, A.; Rhodes, S.M. Syndromic Surveillance for Influenza in the Emergency Department–A Systematic Review. PLoS ONE 2013, 8, e73832. [Google Scholar] [CrossRef] [PubMed]
- Jaarsma, T.; Cameron, J.; Riegel, B.; Stromberg, A. Factors Related to Self-Care in Heart Failure Patients According to the Middle-Range Theory of Self-Care of Chronic Illness: A Literature Update. Curr. Hear. Fail. Rep. 2017, 14, 71–77. [Google Scholar] [CrossRef] [PubMed]
- Kilianski, A.; Evans, N.G. Effectively Communicating the Uncertainties Surrounding Ebola Virus Transmission. PLoS Pathog. 2015, 11, e1005097. [Google Scholar] [CrossRef]
- Rosenbaum, L. Communicating Uncertainty—Ebola, Public Health, and the Scientific Process. N. Engl. J. Med. 2015, 372, 7–9. [Google Scholar] [CrossRef] [PubMed]
- Carter, P.; Anderson, M.; Mossialos, E. Health system, public health, and economic implications of managing COVID-19 from a cardiovascular perspective. Eur. Hear. J. 2020, 41, 2516–2518. [Google Scholar] [CrossRef]
- Centers for Medicare & Medicaid Services (CMS). Recommendations Re-opening Facilities to Provide Non-emergent Non-COVID-19 Healthcare: Phase I. Baltimore; Department of Health and Human Services (HHS). 19 April 2020. Available online: https://www.cms.gov/files/document/covid-flexibility-reopen-essential-non-covid-services.pdf (accessed on 24 September 2020).
- Geraghty, J. Non-COVID Patients Need Care, Too; National Review. 20 April 2020. Available online: https://www.nationalreview.com/the-morning-jolt/non-covid-patients-need-care-too/ (accessed on 24 September 2020).
- Barnes, M.; Heywood, A.E.; Mahimbo, A.; Rahman, B.; Newall, A.T.; Macintyre, C.R. Acute myocardial infarction and influenza: A meta-analysis of case-control studies. Heart 2015, 101, 1738–1747. [Google Scholar] [CrossRef]
- Skajaa, N.; Horváth-Puhó, E.; Adelborg, K.; Prandoni, P.; Rothman, K.J.; Sørensen, H.T. Venous Thromboembolism in Denmark: Seasonality in Occurrence and Mortality. TH Open 2019, 3, e171–e179. [Google Scholar] [CrossRef]
- Helms, J.; Tacquard, C.; Severac, F.; Leonard-Lorant, I.; Ohana, M.; Delabranche, X.; Merdji, H.; Clere-Jehl, R.; Schenck, M.; Fagot Gandet, F.; et al. High risk of thrombosis in patients with severe SARS-CoV-2 infection: A multicenter prospective cohort study. Intensive Care Med. 2020, 46, 1089–1098. [Google Scholar] [CrossRef]
- Barnes, G.D.; Burnett, A.; Allen, A.; Blumenstein, M.; Clark, N.P.; Cuker, A.; Dager, W.E.; Deitelzweig, S.B.; Ellsworth, S.; Garcia, D.; et al. Thromboembolism and anticoagulant therapy during the COVID-19 pandemic: Interim clinical guidance from the anticoagulation forum. J. Thromb. Thrombolysis 2020, 50, 72–81. [Google Scholar] [CrossRef]
- Moe, J.; Kirkland, S.W.; Rawe, E.; Ospina, M.B.; VanderMeer, B.; Campbell, S.; Rowe, B.H. Effectiveness of Interventions to Decrease Emergency Department Visits by Adult Frequent Users: A Systematic Review. Acad. Emerg. Med. 2017, 24, 40–52. [Google Scholar] [CrossRef]
- Li, Y.; Campbell, H.; Kulkarni, D.; Harpur, A.; Nundy, M.; Wang, X.; Nair, H.; The Usher Network for COVID-19 Evidence Reviews (UNCOVER) group. The temporal association of introducing and lifting non-pharmaceutical interventions with the time-varying reproduction number (R) of SARS-CoV-2: A modelling study across 131 countries. Lancet Infect. Dis. 2020. [Google Scholar] [CrossRef]
- Davies, N.G.; Kucharski, A.J.; Eggo, R.M.; Gimma, A.; Edmunds, W.J.; Jombart, T.; O’Reilly, K.; Endo, A.; Hellewell, J.; Nightingale, E.S.; et al. Effects of non-pharmaceutical interventions on COVID-19 cases, deaths, and demand for hospital services in the UK: A modelling study. Lancet Public Health 2020, 5, e375–e385. [Google Scholar] [CrossRef]
- Maringe, C.; Spicer, J.; Morris, M.; Purushotham, A.; Nolte, E.; Sullivan, R.; Rachet, B.; Aggarwal, A. The impact of the COVID-19 pandemic on cancer deaths due to delays in diagnosis in England, UK: A national, population-based, modelling study. Lancet Oncol. 2020, 21, 1023–1034. [Google Scholar] [CrossRef]
 Infuenza like related cases;
Infuenza like related cases;  non-COVID related cases;
non-COVID related cases;  COVID-19 related cases; ED, emergency department; ICU, intensive care unit; MSW, medical/surgical wards.
COVID-19 related cases; ED, emergency department; ICU, intensive care unit; MSW, medical/surgical wards.
 Infuenza like related cases;
Infuenza like related cases;  non-COVID related cases;
non-COVID related cases;  COVID-19 related cases; ED, emergency department; ICU, intensive care unit; MSW, medical/surgical wards.
COVID-19 related cases; ED, emergency department; ICU, intensive care unit; MSW, medical/surgical wards.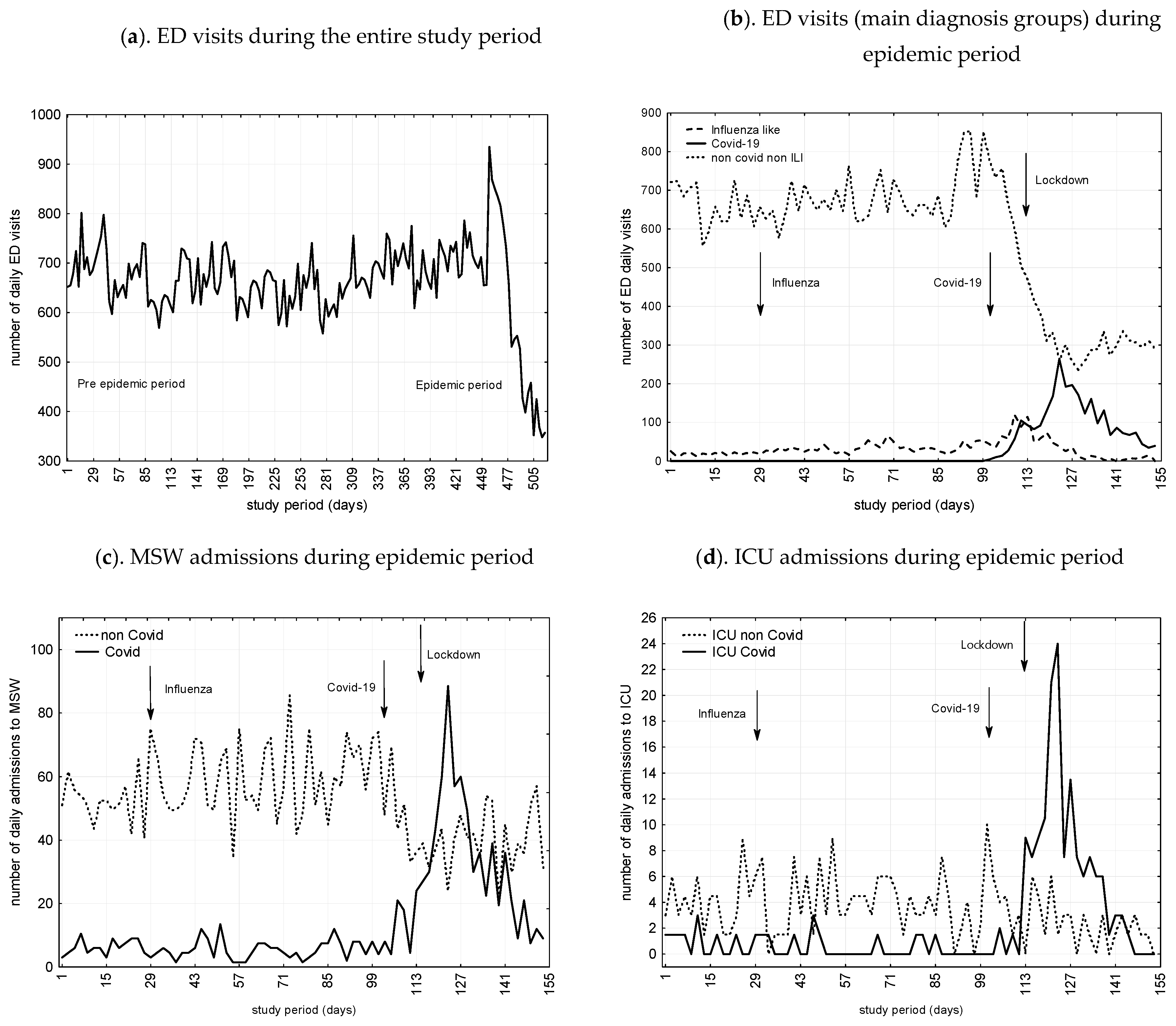
| Variables- | Parameter | SE | t (150) | p | CI 95% | |
|---|---|---|---|---|---|---|
| Daily visits to ED | ||||||
| Influenza epidemic period | ||||||
| Omega | 160.8 | 51.7 | 3.1 | 0.002 | 58.5 | 263.0 |
| Delta | 0.98 | 0.006 | 176.4 | <0.001 | 0.97 | 0.99 |
| COVID-19 epidemic period | ||||||
| Omega | 124.7 | 110.8 | 1.1 | 0.3 | −94.3 | 343.7 |
| Delta | 0.6 | 0.3 | 1.9 | 0.06 | −0.03 | 1.3 |
| Lockdown period | ||||||
| Omega | −160.2 | 23.8 | −6.7 | <0.001 | <0.001 | −113.1 |
| Delta | 1.0 | 0.005 | 210.6 | <0.001 | 1.01 | 1.03 |
| Daily through ED admissions to MSW | ||||||
| Influenza epidemic period | ||||||
| Omega | 6.2 | 5.4 | 1.1 | 0.2 | −4.4 | 16.8 |
| Delta | 1.0 | 0.006 | 177.6 | <0.001 | 0.99 | 1.02 |
| COVID-19 epidemic period | ||||||
| Omega | −31.7 | 15.4 | −2.1 | 0.04 | 1.2 | 62.2 |
| Delta | 0.5 | 0.3 | 2.0 | 0.05 | −1.1 | −0.007 |
| Lockdown period | ||||||
| Omega | −14.6 | 7.6 | 1.9 | 0.05 | −0.4 | 29.6 |
| Delta | 1.0 | 0.02 | 48.2 | <0.001 | 0.9 | 1.0 |
| Daily through ED admissions to ICU | ||||||
| Influenza epidemic period | ||||||
| Omega | 0.7 | 0.8 | 0.9 | 0.4 | −0.8 | 2.1 |
| Delta | −1.0 | 0.02 | −39.7 | <0.001 | −1.0 | −0.9 |
| COVID-19 epidemic period | ||||||
| Omega | 13.9 | 2.1 | 1.8 | 0.05 | −0.3 | 8.1 |
| Delta | 0.8 | 0.1 | −7.5 | <0.001 | −1.0 | −0.6 |
| Lockdown period | ||||||
| Omega | −13.2 | 2.3 | 5.3 | <0.001 | 8.78 | 17.7 |
| Delta | 0.9 | 0.01 | 79.52 | <0.001 | 0.9 | 1.0 |
| Beta | SE of Beta | CI 95% | F | P | Adjusted R2 | |
|---|---|---|---|---|---|---|
| ED daily visits number | ||||||
| Number of patients aged <65 years | 0.2 | 0.02 | 0.09–0.2 | 28.9 | <0.001 | 0.6 |
| Lockdown period | 0.3 | 0.1 | 0.1–1.0 | 130.1 | <0.001 | 0.6 |
| Number of triage level 4/5 | 0.2 | 0.05 | 0.1–0.3 | 26.2 | <0.001 | 0.8 |
| Number of arrival mode by own resources | 0.6 | 0.05 | 0.5–0.7 | 179.5 | <0.001 | 0.9 |
| Trough ED daily admitted patients to MSW | ||||||
| Number of COVID proved cases | 0.9 | 0.1 | 0.7–1.1 | 76.9 | <0.001 | 0.3 |
| Number of triage level 1 to 3 | 0.5 | 0.07 | 0.4–0.7 | 51.5 | <0.001 | 0.4 |
| Number of ILI/COVID suspected cases | −0.7 | 0.1 | −0.9–−0.5 | 51.7 | <0.001 | 0.5 |
| Trough ED daily admitted patients to ICU | ||||||
| Number of triage level 1 to 3 | 0.3 | 0.07 | 0.1–0.4 | 14.3 | <0.001 | 0.3 |
| Number of admitted cases to MSW | 0.2 | 0.07 | 0.05–0.3 | 6.8 | 0.01 | 0.4 |
| Number of COVID proved cases | 0.4 | 0.07 | 0.2–0.5 | 26.2 | <0.001 | 0.4 |
| Variables- | Influenza Epidemic Period | COVID-19 Epidemic Period | Lockdown Period | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Trend (%) | CI 95% | p | Trend (%) | CI95% | p | Trend (%) | CI 95% | p | ||||
| ED and hospital activities | ||||||||||||
| ED visits | 10.6 | 7.3 | 13.9 | 0.01 | −36.9 | −43.0 | −30.7 | <0.001 | −49.6 | −55.7 | −43.4 | <0.001 |
| Admission to MSW | 12.8 | 9.2 | 16.4 | 0.003 | 33.9 | 28.1 | 39.7 | <0.001 | −16.8 | −21.2 | −11.4 | 0.001 |
| non-COVID ED admissions to MSW | - | - | - | - | −29.9 | −22.1 | −36.3 | <0.001 | −24.2 | −29.3 | 19.5 | <0.001 |
| COVID admissions to MSW | - | - | - | - | 366.0 | 248.0 | 435.0 | <0.001 | −68.0 | −79.6 | −52.1 | <0.001 |
| Admissions to ICU | 4.6 | 2.5 | 6.7 | 0.05 | 277.0 | 260.4 | 293.6 | <0.001 | −15.5 | −18.2 | 11.8 | −0.02 |
| non-COVID ED admissions to ICU | - | - | - | - | −71.1 | −76.3 | −64.9 | <0.001 | −13.8 | −18.2 | 8.4 | 0.03 |
| COVID admissions to ICU | - | - | - | - | 406.0 | 377.0 | 486.0 | <0.001 | −22.4 | −26.3 | −18.7 | 0.001 |
| ED visits number as a function of main case characteristics | ||||||||||||
| Age <65 years | 7.6 | 4.8 | 10.4 | 0.008 | −18.3 | −22.5 | −14.1 | 0.001 | −68.3 | −75.9 | −60.5 | <0.001 |
| Male | 8.8 | 5.8 | 11.8 | 0.001 | 9.2 | 6.2 | 12.2 | 0.03 | −62.6 | −70.3 | −54.3 | <0.001 |
| Frequent users | 128.5 | 117.2 | 139.8 | <0.001 | 221 | 206.1 | 235.9 | <0.001 | 188.9 | 174.3 | 201.7 | <0.001 |
| Arrival mode Own resources | 22.6 | 17.8 | 27.4 | <0.001 | −28.4 | 23.1 | 33.7 | <0.001 | −52.6 | −59.7 | −44.8 | <0.001 |
| Arrival mode Ambulance | 5.9 | 3.5 | 8.3 | 0.005 | 52.6 | 45.3 | 59.9 | <0.001 | 16.6 | 12.5 | 20.7 | 0.001 |
| Triages 1 to 3 | 16.7 | 12.6 | 20.8 | 0.05 | 74.4 | 65.8 | 83.0 | <0.001 | −21.6 | −26.4 | −16.8 | 0.001 |
| Triages 4 and 5 | 17.4 | 13.2 | 21.6 | <0.001 | 5.2 | 2.9 | 7.5 | 0.09 | −63.1 | −71.0 | −55.1 | <0.001 |
| Main Diagnosis- | Influenza Epidemic Period | COVID-19 Epidemic Period | Lockdown Period | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Trend (%) | CI 95% | p | Trend (%) | CI 95% | p | Trend (%) | CI 95% | p | ||||
| ILI | 161.0 | 148.3 | 173.7 | <0.001 | 225.0 | 210.0 | 240.0 | <0.001 | −42.1 | −48.1 | −36.0 | <0.001 |
| ILI plus COVID-19 suspected cases | 244.0 | 228.4 | 259.6 | <0.001 | 865.0 | 835.6 | 894.4 | <0.001 | 31.6 | 26.0 | 37.2 | <0.001 |
| COVID-19 proved cases | 125.0 | 97.0 | 199.0 | <0.001 | 388.0 | 296.0 | 477.0 | <0.001 | −69.0 | 33.0 | 109.0 | <0.001 |
| Acute coronary syndrome | 13.7 | 10.0 | 17.4 | 0.007 | −1.1 | −2.0 | 0.1 | 1 | −51.2 | −52.1 | −50.0 | <0.001 |
| Atrial fibrillation | −26.8 | −32.1 | −21.1 | 0.01 | −34.2 | −39.5 | −28.5 | 0.001 | −71.3 | −76.6 | −65.6 | <0.001 |
| Thoracic pain | 8.4 | 5.5 | 11.3 | 0.05 | −19.2 | −23.7 | −14.7 | 0.02 | −40.8 | −45.3 | −36.3 | <0.001 |
| Pulmonary embolism/deep vein thrombosis | 31.1 | 25.5 | 36.7 | 0.001 | 42.4 | 35.9 | 44.8 | <0.001 | 33.5 | 27.7 | 35.9 | <0.001 |
| Stroke | 1.9 | 0.5 | 3.3 | 0.6 | −5.8 | −8.2 | −3.4 | 0.09 | −57.1 | −64.6 | −49.4 | <0.001 |
| Seizures | 3.8 | 1.9 | 5.7 | 0.2 | 1.1 | 0.1 | 2.1 | 0.7 | −48.1 | −55.0 | −41.2 | <0.001 |
| Diabetes | 4.2 | 2.3 | 6.8 | 0.3 | 2.1 | 1.7 | 2.8 | 0.6 | −47.2 | −53.8 | −42.1 | 0.001 |
| Hip fracture | 5.1 | 2.8 | 7.4 | 0.1 | 1.9 | 0.5 | 3.3 | 0.6 | −44.6 | −51.2 | −38.0 | <0.001 |
| Hand wound | 6.9 | 4.3 | 9.5 | 0.1 | −1.9 | −3.4 | −0.5 | 0.3 | −51.3 | −52.8 | −49.9 | 0.001 |
| Head trauma | -0.8 | −1.7 | 0.5 | 0.9 | −6.6 | −7.5 | −5.3 | 0.06 | −59.7 | −67.4 | −52.1 | <0.001 |
| Headaches | 14.8 | 11.0 | 18.6 | 0.01 | 5.9 | 3.5 | 8.3 | 0.04 | −42.9 | −49.2 | −36.4 | <0.001 |
| Abdominal pain | 3.4 | 1.6 | 5.2 | 0.6 | 2.6 | 1.0 | 4.2 | 0.09 | −52.2 | −59.5 | −45.0 | <0.001 |
| Renal colic | 12.8 | 9.2 | 16.4 | 0.05 | −3.9 | −5.9 | −1.9 | 0.2 | −54.3 | −56.3 | −52.3 | <0.001 |
| Low back pain | −11.6 | −15.1 | −8.2 | 0.04 | −22.4 | −25.9 | −19.0 | 0.001 | −73.6 | −81.7 | −65.3 | <0.001 |
| Appendicitis | 14.6 | 10.8 | 18.4 | 0.05 | 1.9 | 0.5 | 3.3 | 0.6 | −57.4 | −64.5 | −49.6 | <0.001 |
| Urinary tract infection | −18.4 | −22.8 | −14.2 | 0.01 | −31.3 | −36.9 | −25.7 | <0.001 | −62.5 | −68.1 | −56.9 | <0.001 |
| Alcoholic intoxication | −7.9 | −10.7 | −5.1 | 0.07 | −24.8 | −27.6 | −19.8 | <0.001 | −73.4 | −81.6 | −65.0 | <0.001 |
| Psychiatric disorders | 7.8 | 5.0 | 10.6 | 0.07 | −8.4 | −11.3 | −5.5 | 0.005 | −23.8 | −28.5 | −18.9 | <0.001 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Casalino, E.; Choquet, C.; Bouzid, D.; Peyrony, O.; Curac, S.; Revue, E.; Fontaine, J.-P.; Plaisance, P.; Chauvin, A.; Ghazali, D.A. Analysis of Emergency Department Visits and Hospital Activity during Influenza Season, COVID-19 Epidemic, and Lockdown Periods in View of Managing a Future Disaster Risk: A Multicenter Observational Study. Int. J. Environ. Res. Public Health 2020, 17, 8302. https://doi.org/10.3390/ijerph17228302
Casalino E, Choquet C, Bouzid D, Peyrony O, Curac S, Revue E, Fontaine J-P, Plaisance P, Chauvin A, Ghazali DA. Analysis of Emergency Department Visits and Hospital Activity during Influenza Season, COVID-19 Epidemic, and Lockdown Periods in View of Managing a Future Disaster Risk: A Multicenter Observational Study. International Journal of Environmental Research and Public Health. 2020; 17(22):8302. https://doi.org/10.3390/ijerph17228302
Chicago/Turabian StyleCasalino, Enrique, Christophe Choquet, Donia Bouzid, Olivier Peyrony, Sonja Curac, Eric Revue, Jean-Paul Fontaine, Patrick Plaisance, Anthony Chauvin, and Daniel Aiham Ghazali. 2020. "Analysis of Emergency Department Visits and Hospital Activity during Influenza Season, COVID-19 Epidemic, and Lockdown Periods in View of Managing a Future Disaster Risk: A Multicenter Observational Study" International Journal of Environmental Research and Public Health 17, no. 22: 8302. https://doi.org/10.3390/ijerph17228302
APA StyleCasalino, E., Choquet, C., Bouzid, D., Peyrony, O., Curac, S., Revue, E., Fontaine, J.-P., Plaisance, P., Chauvin, A., & Ghazali, D. A. (2020). Analysis of Emergency Department Visits and Hospital Activity during Influenza Season, COVID-19 Epidemic, and Lockdown Periods in View of Managing a Future Disaster Risk: A Multicenter Observational Study. International Journal of Environmental Research and Public Health, 17(22), 8302. https://doi.org/10.3390/ijerph17228302






