Community Based Interventions for Problematic Substance Use in Later Life: A Systematic Review of Evaluated Studies and Their Outcomes
Abstract
1. Introduction
1.1. Problematic Substance Use in Later Life
1.2. What Works for Older People with PSU?
1.3. Aims and Objectives
- To identify community-based interventions including preventative and early intervention programmes used with older people with problematic substance use.
- To collate evidence on the range and type of interventions used.
- To identify methods used to evaluate the programmes, interventions used and their effectiveness.
- To describe the findings on programme effectiveness and utilization in different care settings.
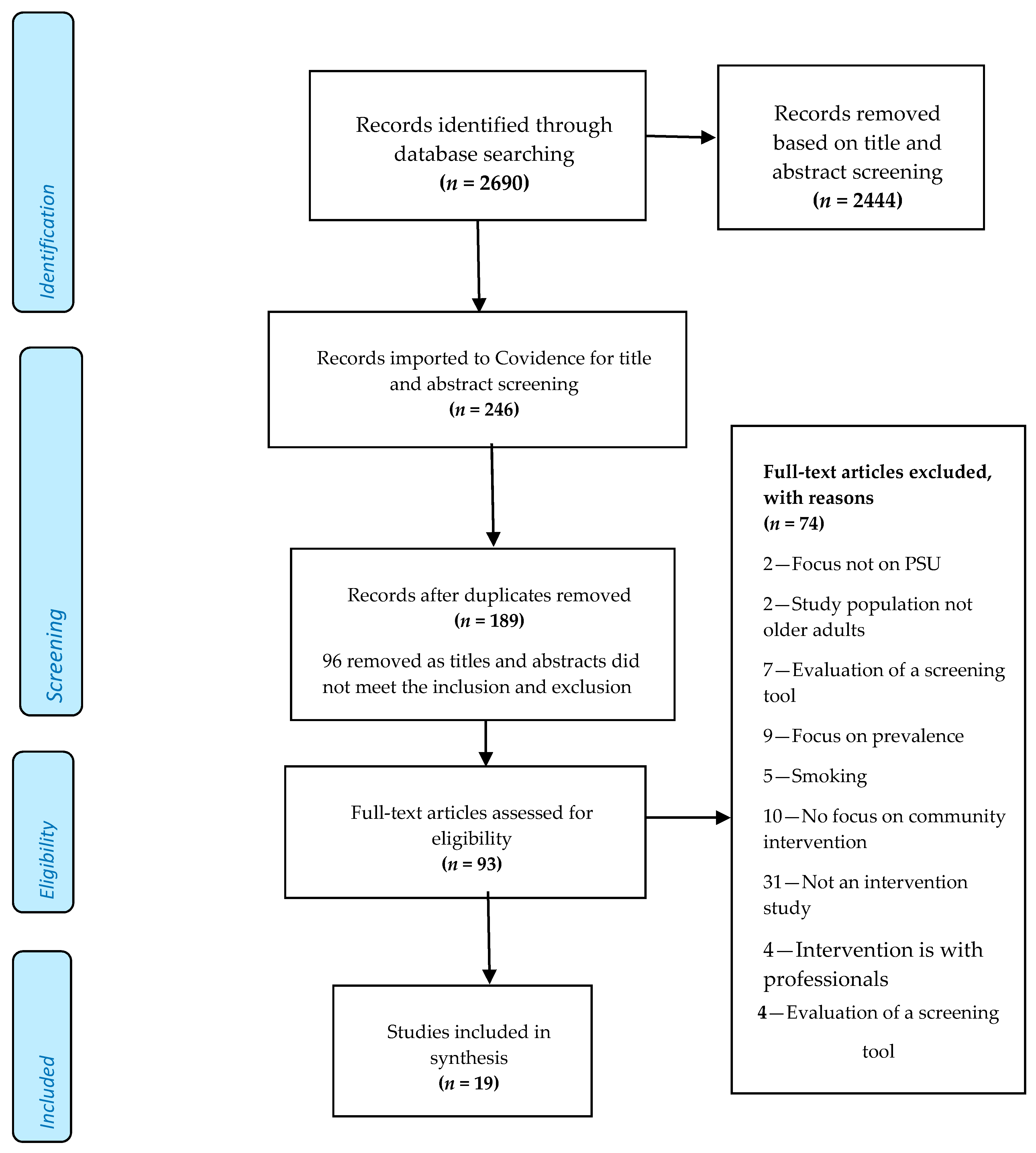
2. Materials and Methods
2.1. Search Strategy
2.2. Inclusion and Exclusion Criteria
2.3. Study Selection
2.4. Data Extraction and Synthesis
2.5. Quality Assessment
3. Results
3.1. Overview of Study Characteristics
3.2. Quality Assessment
3.2.1. MERSQI Assessment
- Michigan Alcoholism Screening Test-Geriatric Version (MAST-G)
- Global Assessment of Functioning (GAF)
- Health Screening Survey (HSS)
- Alcohol Use Disorder Identification Test (AUDIT)
- Mental Health Inventory (MHI)
- MOS SF-12, Basis 32, and Substance Abuse Inventory (SAI)
- Older American Research and Service Centre Instrument (OARS)
3.2.2. CASP Randomised Controlled Trial Checklist
3.3. Defining and Assessing Problematic Use
3.4. Populations Studied
3.5. Overview of Interventions and Key Outcomes Measured
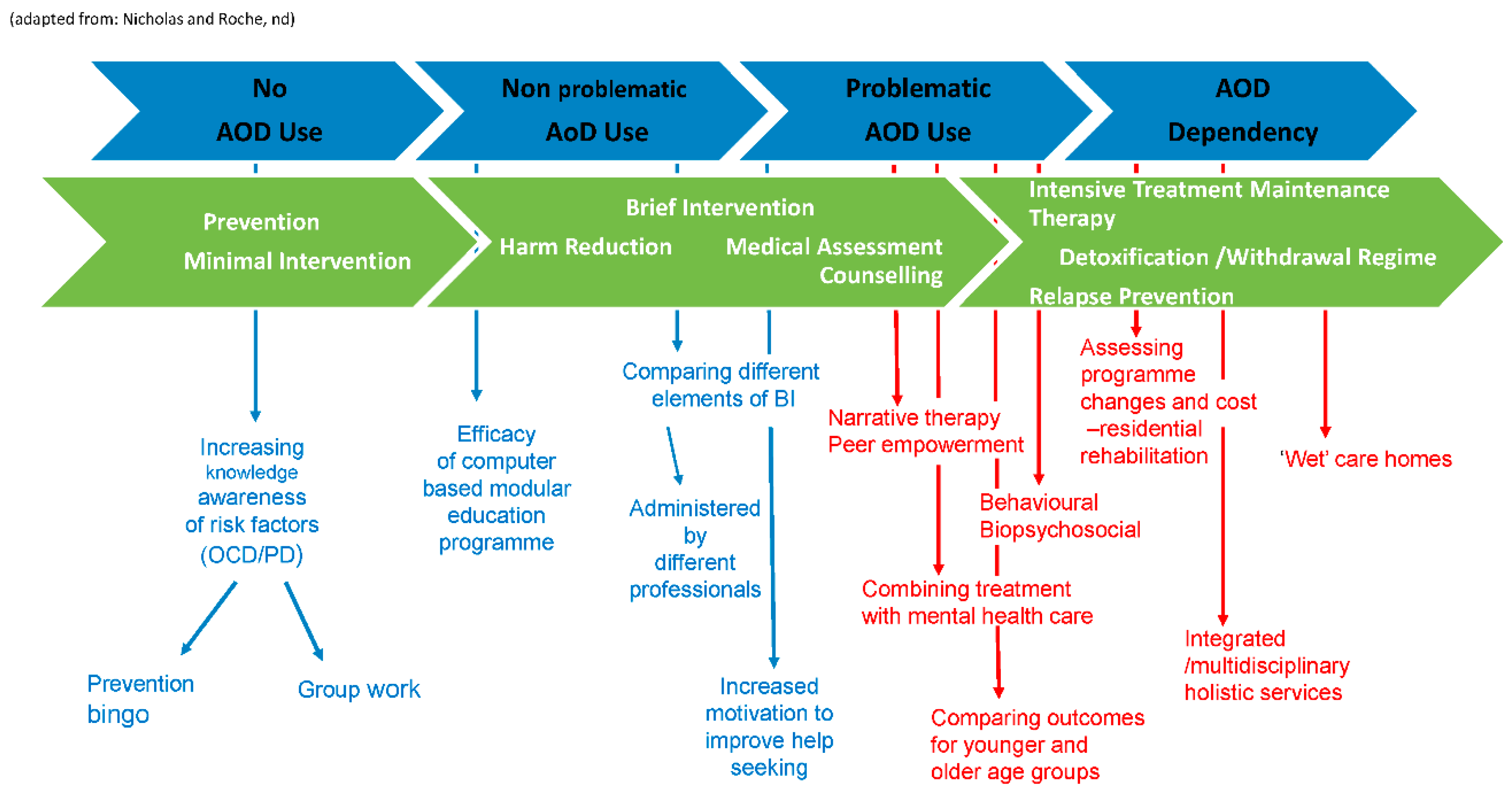
3.5.1. Interventions
3.5.2. Educational Interventions
3.5.3. Brief Interventions
3.5.4. Treatment Approaches Provided in Community-Based Facilities
3.5.5. Holistic Interventions through Service Design and Delivery
3.6. Key Outcomes Measured
3.6.1. Education and Brief Interventions
3.6.2. Older People’s Experiences
3.6.3. Studies Addressing Drugs
4. Discussion
5. Limitations
6. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Koechl, B.; Unger, A.; Fischer, G. Age-related aspects of addiction. Gerontology 2012, 58, 540–544. [Google Scholar] [CrossRef] [PubMed]
- Kydd, A.; Fleming, A.; Paoletti, I.; Touzery, S.H. Exploring terms used for the oldest old in the gerontological literature. J. Aging Soc. Chang. 2020, 10. [Google Scholar] [CrossRef]
- World Health Organization. Global Status Report on Alcohol and Health; World Health Organization Press: Geneva, Switzerland, 2014. [Google Scholar]
- Crome, I.B.; Rao, R.; Crome, P. Substance misuse and older people: Better information, better care. Age Ageing 2015, 44, 729–731. [Google Scholar] [CrossRef] [PubMed][Green Version]
- United Nations. World Population Ageing Report. UN; Department of Economic and Social Affairs Press: Geneva, Switzerland, 2018. [Google Scholar]
- Royal College of Psychiatrist. Suffering in Silence: Age Inequality in Older People’s Mental Health Care CR221; Royal College of Psychiatrist Press: London, UK, 2018. [Google Scholar]
- Griffiths, P.; Lopez, D.; Götz, W. Monitoring trends in illicit drug use in Europe: An overview of the work of the European Monitoring Centre for Drugs and Drug Addiction (EMCDDA). Psychiatr. Psychother. 2008, 4, 58–65. [Google Scholar] [CrossRef]
- Pirona, A.; Guarita, B.; Montanari, L.; Noor, A. Ageing and addiction: Challenges for treatment systems. In Proceedings of the Lisbon Addictions Conference, Lisbon, Portugal, 23–25 September 2015. [Google Scholar]
- Duncan, D.F.; Nicholson, T.; White, J.B.; Bradley, D.B.; Bonaguro, J. The baby boomer effect: Changing patterns of substance abuse among adults ages 55 and older. J. Aging Soc. Policy 2010, 22, 237–248. [Google Scholar] [CrossRef]
- Seddon, J.L.; Wadd, S.; Wells, E.; Elliott, L.; Madoc-Jones, I.; Breslin, J. Drink wise, age well; reducing alcohol related harm among people over 50: A study protocol. BMC Public Health 2019, 19, 240. [Google Scholar] [CrossRef]
- Hafford-Letchfield, T.; Thom, B.; Herring, R. Community Based Care for Older People with Alcohol-Related Harm: Findings from a Consultation Workshop with Practitioners in Social Work and Social Care; Alcohol Research: London, UK, 2018. [Google Scholar]
- Vossius, C.; Testad, I.; Skjæveland, R.; Nesvåg, S. The use and costs of health and social services in patients with longstanding substance abuse. BMC Health Serv. Res. 2013, 13, 185. [Google Scholar] [CrossRef]
- Kouimtsidis, C.; Padhi, A. A case of late-onset dependence on cocaine and crack. Addiction 2007, 102, 666–667. [Google Scholar] [CrossRef]
- Heuberger, R.A. Alcohol and the older adult: A comprehensive review. J. Nutr. Elder. 2009, 28, 203–235. [Google Scholar] [CrossRef]
- NHS Digital. Part of Statistics on Drug Misuse: Statistics on Drug Misuse; NHS Digital Press: Leeds, UK, 2018; Available online: https://digital.nhs.uk/data-and-information/publications/statistical/statistics-on-drug-misuse/2018 (accessed on 29 October 2020).
- Rao, R.; Crome, I.; Crome, P.; Iliffe, S. Substance misuse in later life: Challenges for primary care: A review of policy and evidence. Prim. Health Care Res. Dev. 2019, 20. [Google Scholar] [CrossRef]
- Burton, R.; Henn, C.; Lavoie, D.; O’Connor, R.; Perkins, C.; Sweeney, K.; Musto, V. The Public Health Burden of Alcohol and the Effectiveness and Cost-Effectiveness of Alcohol Control Policies: An Evidence Review; Public Health England Press: London, UK, 2016. [Google Scholar]
- Livingston, W. Towards a comprehensive typology of knowledge for social work and alcohol. Soc. Work. Educ. 2014, 33, 774–787. [Google Scholar] [CrossRef]
- Kertesz, S.G.; Crouch, K.; Milby, J.B.; Cusimano, R.E.; Schumacher, J.E. Housing first for homeless persons with active addiction: Are we overreaching? Milbank Q. 2009, 87, 495–534. [Google Scholar] [CrossRef] [PubMed]
- MacGregor, S. Proposals for policy development: Drugs. Subst. Use Older People 2015, 353. [Google Scholar] [CrossRef]
- Care Quality Commission. The State of Health Care and Adult Social Care in England; Care Quality Commission Press: London, UK, 2019. [Google Scholar]
- Roy, A.; Buchanan, J. The paradoxes of recovery policy: Exploring the impact of austerity and responsibilisation for the citizenship claims of people with drug problems. Soc. Policy Adm. 2015, 50, 398–413. [Google Scholar] [CrossRef]
- Nicholas, R.; Roche, A.; Lee, N.; Bright, S.; Walsh, K. Preventing and Reducing Alcohol and other Drug-Related Harm among Older People: A Practical Guide for Health and Welfare Professionals. National Centre for Education and Training on Addiction (NCETA); Flinders University Press: Adelaide, Australia, 2015. [Google Scholar]
- Rao, R.; Roche, A. Substance misuse in older people. BMJ 2017, 358, j3885. [Google Scholar] [CrossRef]
- O’Mara-Eves, A.; Brunton, G.; McDaid, D.; Oliver, S.; Kavanagh, J.; Jamal, F.; Matosevic, T.; Hardenberg, A.; Thomas, J. Community engagement to reduce inequalities in health: A systematic review, meta-analysis and economic analysis. Public Heal. Res. 2013, 1, 1–526. [Google Scholar] [CrossRef]
- PROSPERO. Available online: https://www.crd.york.ac.uk/prospero/display_record.php?RecordID=152273 (accessed on 29 October 2020).
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; Prisma Group. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. Int. J. Surg 2010, 8, 336–341. [Google Scholar] [CrossRef]
- Neugarten, B.L. Age groups in American society and the rise of the young-old. Ann. Am. Acad. Politi- Soc. Sci. 1974, 415, 187–198. [Google Scholar] [CrossRef]
- Hannes, K.; Lockwood, C. Pragmatism as the philosophical foundation for the Joanna Briggs meta-aggregative approach to qualitative evidence synthesis. J. Adv. Nurs. 2011, 67, 1632–1642. [Google Scholar] [CrossRef]
- Reed, D.A.; Cook, D.A.; Beckman, T.J.; Levine, R.B.; Kern, D.E.; Wright, S.M. Association between funding and quality of published medical education research. JAMA 2007, 298, 1002–1009. [Google Scholar] [CrossRef]
- Singh, J. Critical appraisal skills programme. J. Pharmacol. Pharmacother. 2013, 4, 76. [Google Scholar] [CrossRef]
- Brennan, N.; Mattick, K. A systematic review of educational interventions to change behaviour of prescribers in hospital settings, with a particular emphasis on new prescribers. Br. J. Clin. Pharmacol. 2013, 75, 359–372. [Google Scholar] [CrossRef]
- Smith, R.P.; Learman, L.A. A plea for MERSQI: The medical education research study quality instrument. Obstet. Gynecol. 2017, 130, 686–690. [Google Scholar] [CrossRef] [PubMed]
- Kothari, D.; Gourevitch, M.N.; Lee, J.D.; Grossman, E.; Truncali, A.; Ark, T.K.; Kalet, A.L. Undergraduate medical education in substance abuse: A review of the quality of the literature. Acad. Med. 2011, 86, 98–112. [Google Scholar] [CrossRef] [PubMed]
- Alemagno, S.A.; Niles, S.A.; Treiber, E.A. Using computers to reduce medication misuse of community-based seniors: Results of a pilot intervention program. Geriatr. Nurs. 2004, 25, 281–285. [Google Scholar] [CrossRef]
- Barnes, A.J.; Xu, H.; Tseng, C.-H.; Ang, A.; Tallen, L.; Moore, A.A.; Marshall, D.C.; Mirkin, M.; Ransohoff, K.; Duru, O.K.; et al. The effect of a patient-provider educational intervention to reduce at-risk drinking on changes in health and health-related quality of life among older adults: The project share study. J. Subst. Abus. Treat. 2015, 60, 14–20. [Google Scholar] [CrossRef][Green Version]
- Benza, A.T.; Calvert, S.; McQuown, C.B. Prevention BINGO: Reducing medication and alcohol use risks for older adults. Aging Ment. Heal. 2010, 14, 1008–1014. [Google Scholar] [CrossRef]
- Copeland, L.A.; Blow, F.C.; Barry, K.L. Health care utilization by older alcohol-using veterans: Effects of a brief intervention to reduce at-risk drinking. Health Educ. Behav. 2003, 30, 305–321. [Google Scholar] [CrossRef]
- D’Agostino, C.S.; Barry, K.L.; Blow, F.C.; Podgorski, C. Community interventions for older adults with comorbid substance abuse: The Geriatric Addictions Program (GAP). J. Dual Diagn. 2006, 2, 31–45. [Google Scholar] [CrossRef]
- Eliason, M.J.; Skinstad, A.H. Drug & alcohol intervention for older women. J. Gerontol. Nurs. 2001, 27, 18–24. [Google Scholar] [CrossRef]
- Fink, A.; Elliott, M.N.; Tsai, M.; Beck, J.C. An evaluation of an intervention to assist primary care physicians in screening and educating older patients who use alcohol. J. Am. Geriatr. Soc. 2005, 53, 1937–1943. [Google Scholar] [CrossRef] [PubMed]
- Fleming, M.; Manwell, L.B.; Barry, K.L.; Adams, W.; A Stauffacher, E. Brief physician advice for alcohol problems in older adults: A randomized community-based trial. J. Fam. Pr. 1999, 48, 378–386. [Google Scholar]
- Hansen, A.; Becker, U.; Nielsen, A.S.; Grønbæk, M.; Tolstrup, J.S. Brief alcohol intervention by newly trained workers versus leaflets: Comparison of effect in older heavy drinkers identified in a population health examination survey: A randomized controlled trial. Alcohol Alcohol. 2011, 47, 25–32. [Google Scholar] [CrossRef][Green Version]
- Kuerbis, A.; Hayes, M.; Morgenstern, J. Exploratory single-system analyses of moderation-based brief treatments with middle-aged and older heavy drinkers. J. Soc. Work. Pract. Addict. 2013, 13, 393–416. [Google Scholar] [CrossRef]
- Lee, H.; Mericle, A.A.; Ayalon, L.; Arean, P.A. Harm reduction among at-risk elderly drinkers: A site-specific analysis from the multi-site Primary Care Research in Substance Abuse and Mental Health for Elderly (PRISM-E) study. Int. J. Geriatr. Psychiatry 2009, 24, 54–60. [Google Scholar] [CrossRef]
- McCann, M.; Wadd, S.; Crofts, G. ’Wet’ Care Homes for Older People with Refractory Alcohol Problems: A Qualitative Study; Alcohol Research UK Press: London, UK, 2017. [Google Scholar]
- Oslin, D.W.; Thompson, R.; Kallan, M.J.; Tenhave, T.; Blow, F.C.; Bastani, R.; Gould, R.L.; Maxwell, A.E.; Rosansky, J.; Van Stone, W.; et al. Treatment effects from UPBEAT: A randomized trial of care management for behavioral health problems in hospitalized elderly patients. J. Geriatr. Psychiatry Neurol. 2004, 17, 99–106. [Google Scholar] [CrossRef]
- Oslin, D.W.; Slaymaker, V.J.; Blow, F.C.; Owen, P.L.; Colleran, C. Treatment outcomes for alcohol dependence among middle-aged and older adults. Addict. Behav. 2005, 30, 1431–1436. [Google Scholar] [CrossRef]
- Outlaw, F.H.; Marquart, J.M.; Roy, A.; Luellen, J.K.; Moran, M.; Willis, A.; Doub, T. Treatment outcomes for older adults who abuse substances. J. Appl. Gerontol. 2010, 31, 78–100. [Google Scholar] [CrossRef]
- Poole, J.M.; Gardner, P.; Flower, M.C.; Cooper, C. Narrative therapy, older adults, and group work?: Practice, research, and recommendations. Soc. Work. Groups 2009, 32, 288–302. [Google Scholar] [CrossRef]
- Rao, T. The role of community nursing in providing integrated care for older people with alcohol misuse. Br. J. Community Nurs. 2014, 19, 80–84. [Google Scholar] [CrossRef]
- Schonfeld, L.; Hazlett, R.W.; Hedgecock, D.K.; Duchene, D.M.; Burns, L.V.; Gum, A.M. Screening, brief intervention, and referral to treatment for older adults with substance misuse. Am. J. Public Health 2015, 105, 205–211. [Google Scholar] [CrossRef] [PubMed]
- Watson, J.; Crosby, H.; Dale, V.M.; Tober, G.; Wu, Q.; Lang, J.; McGovern, R.; Newbury-Birch, D.; Parrott, S.; Bland, J.M.; et al. AESOPS: A randomised controlled trial of the clinical effectiveness and cost-effectiveness of opportunistic screening and stepped care interventions for older hazardous alcohol users in primary care. Health Technol. Assess. 2013, 17, 1–158. [Google Scholar] [CrossRef]
- Nicholas, R.; Roche, A.M. Information Sheet 3: The Silver Tsunami: The Impact of Australia’s Ageing Population.; National Centre for Education and Training in Addiction (NCETA), Flinders University Press: Adelaide, Australia, 2005. [Google Scholar]
- Han, B.H.; Moore, A.A. Prevention and screening of unhealthy substance use by older adults. Clin. Geriatr. Med. 2018, 34, 117–129. [Google Scholar] [CrossRef]
- Clancy, C.; Oyefeso, A. Getting addiction into the nursing education “water supply”. J. Addict. Nurs. 2019, 30, 149–158. [Google Scholar] [CrossRef]
- Thom, B.; Herring, R.; Bayley, M.; Hafford-Letchfield, T. Delivering Alcohol IBA in Housing, Probation and Social Work Settings: Opportunities and Constraints; Alcohol Research UK Press: London, UK, 2016. [Google Scholar]
- Thom, B.; Herring, R.; Bayley, M.; Hafford-Letchfield, T.; Luger, L.; Annand, F.; Bristow, A. The Role of Training in Delivering Alcohol IBA in Non-Medical Settings: Broadening the Base of IBA Delivery; Alcohol Research UK Press: London, UK, 2016. [Google Scholar]
- Kaner, E.; Beyer, F.; Dickinson, H.; Pienaar, E.; Campbell, F.; Schlesinger, C.; Bernand, B. Brief interventions for excessive drinkers in primary health care settings. Cochrane Database Syst. Rev. 2007, 2. [Google Scholar] [CrossRef]
- Wutzke, S.E.; Conigrave, K.M.; Saunders, J.B.; Hall, W.D. The long-term effectiveness of brief interventions for unsafe alcohol consumption: A 10-year follow-up. Addiction 2002, 97, 665–675. [Google Scholar] [CrossRef]
- Riper, H.; Van Straten, A.; Keuken, M.; Smit, F.; Schippers, G.; Cuijpers, P. Curbing problem drinking with personalized-feedback interventions. Am. J. Prev. Med. 2009, 36, 247–255. [Google Scholar] [CrossRef]
- Wadd, S.; Galvani, S. Working with older people with alcohol problems: Insight from specialist substance misuse professionals and their service users. Soc. Work. Educ. 2014, 33, 656–669. [Google Scholar] [CrossRef]
- Sorocco, K.H.; Ferrell, S.W. Alcohol use among older adults. J. Gen. Psychol. 2006, 133, 453–467. [Google Scholar] [CrossRef]
- Blazer, D.G.; Wu, L.-T. The epidemiology of at-risk and binge drinking among middle-aged and elderly community adults: National Survey on Drug Use and Health. Am. J. Psychiatry 2009, 166, 1162–1169. [Google Scholar] [CrossRef]
- Ojeda, V.D.; McGuire, T.G. Gender and racial/ethnic differences in use of outpatient mental health and substance use services by depressed adults. Psychiatr. Q. 2006, 77, 211–222. [Google Scholar] [CrossRef]
| Databases searched | BioMed Central; CINHAL; Emerald; International Bibliography of the Social Sciences (IBSS); NICE evidence; OVID full text; PsycINFO; PubMed; Web of Science; MEDLINE; COCHRANE; British Nursing and social care online. |
| Keyword search terms | “old* people” or “old* adults” or elderly or ageing or aging or geriat* or geron* or mature AND addict* or “problematic substance use” or “substance misuse” or “alcohol misuse” or “alcoholism” or “drug misuse” or “drug abuse” or “alcohol abuse” or AOD or alcohol or “other drugs” or polypharmacy or “prescription drugs” or “non-prescription drugs” or narcotics or addiction or “dual diagnosis” or “drug depend*” or “alcohol depend*” |
| MeSH terms | “aged, 80 and over” or “aged” AND“substance dependence” or “substance addiction consequences” or “alcoholism” or “street drugs” |
| Inclusion | Exclusion |
|---|---|
| Focuses on programmes for problematic substance use | Does not have problematic substance use as its key focus |
| Describes older people as the target population specifically or in comparison to the majority population | Target population is people under 45 years |
| The intervention delivered within community-based provision. | Is focused on ‘in-patient’ hospital only treatment |
| Has a clear description of the interventions used | Is not peer reviewed research |
| Has a clear empirical evaluation of the intervention/s | Does not contain evaluation of the intervention described |
| Qualitative, quantitative, review or mixed methods papers | Discussion documents |
| Describes outcomes of the intervention in its findings | Where the focus was on tobacco use only |
| Published in English | Published in a language other than English |
| Published between 1990 and 2019 | Published before 1990 |
| Source | Study Design | Country | Participants Age Range | Aims of Study | Substances Targeted |
|---|---|---|---|---|---|
| Alemagno et al. (2004) [35] | PP | USA | 59–97 | Test efficacy of educational computer programme to reduce medication misuse. | Prescription medication & OTC drugs |
| Barnes et al. (2016) [36] | RCT | USA | 60+ | To examine changes in health-related quality of life. Project SHARE interventions vs. TAU | Alcohol |
| Benza et al. (2010) [37] | PP | USA | 60+ | To develop and evaluate an educational programme to increase older adults’ knowledge of PSU. | Alcohol and OTC drugs |
| Copeland, Blow, Barry (2003) [38] | CS | USA | 55+ | Effect of BI on services use for older veterans who were at-risk drinkers. | Alcohol |
| D’Agostino et al. (2006) [39] | RCT | USA | 51–91 | To evaluate the Geriatric Addictions Program (GAP), designed to assist OA with PSU and DD. | Alcohol and OTC drugs |
| Eliason, Skinstad. (2001) [40] | PP | USA | 54–91 | Prevalence of AoD interactions in older women and if a BI would change knowledge. | Alcohol and OTC drugs |
| Fink et al. (2005) [41] | PCS | USA | 65+ | To evaluate whether providing physicians and older patients in primary care with personalized reports of drinking risks and benefits and patient education reduces alcohol related risks and problems. | Alcohol |
| Fleming et al. (1999) [42] | RCT | USA | 65–75 | To test the efficacy of BI in reducing alcohol use in older problem drinkers. | Alcohol |
| Gottlieb Hansen et al. (2012) [43] | RCT | Denmark | 48–65 | To test if a BI in a non-treatment seeking population of heavy drinkers results in reduced alcohol intake. | Alcohol |
| Kuerbis et al. (2013) [44] | Secondary analysis of data from 3 RCTs | USA | 54+ | Secondary data analysis of cases in three RCT’s that recruited problem drinkers, examining the effectiveness of BI. Additional comparisons to different age cohorts were made. | Alcohol |
| Lee et al. (2009) [45] | Secondary analysis of RCT | USA | 65+ | To assess the efficacy of a harm-reduction based intervention to enhance access to treatment and clinical outcomes among elderly at-risk drinkers. | Alcohol |
| McCann, Wadd & Gill Crofts. (2017) [46] | QS | UK & Norway | 46–77 | To describe the harm reduction models developed in two wet care homes in England and one in Norway. | Alcohol |
| Oslin et al. (2004) [47] | RCT | USA | 60+ | To examine the impact of the Unified Psychogeriatric Biopsychosocial Evaluation and Treatment (UPBEAT) Program, for elderly veterans | Alcohol |
| Oslin et al. (2005) [48] | PP | USA | 50+ | To examine differences in the clinical presentation and treatment outcomes of older adults with a diagnosis of alcohol dependence compared to middle-aged adults. | Alcohol |
| Outlaw et al. (2012) [49] | PP | USA | 50+ | To determine the effectiveness of the cognitive-behavioral and self-management treatment approaches targeted to older adults. | Alcohol, Prescription medication & OTC drugs & ID |
| Poole et al. (2009) [50] | QS | Canada | 55–70 | To review the effect of narrative therapy on OA coping with mental health and PSU. | Alcohol |
| Rao. (2014) [51] | CS | UK | 65–85 | To examine the outcomes of an integrated community nursing team for older adults with alcohol misuse. | Alcohol |
| Schonfeld et al. (2015) [52] | PP | USA | Mean age 66.5 | Rolling the Florida Brief intervention and treatment for elders (BRITE project) out across 75 different sites. | Alcohol and ID |
| Watson et al. (2013) [53] | RCT | UK | 55+ | To compare the clinical effectiveness and cost-effectiveness of a stepped care intervention against a minimal intervention in primary care. | Alcohol |
| Source | Intervention Description | Setting | Participant | # | Outcome Measured | Results |
|---|---|---|---|---|---|---|
| 1. Alemagno et al. (2004) | Education | Nine community senior centres | Majority female and white | 412 | Enhanced knowledge of PSU. | OA were more likely to use a medication reminder checklist and one third visited their doctor to discuss their medication misuse. No significance difference mentioned |
| 2. Barnes et al. (2016) | Education | Primary care clinic | Majority white male | 1049 | Health and health related quality of life (HRQL) | A statistically significant effect on health and HRQL in the intervention group. Effects were most prominent for patients who received physician discussions. |
| 3. Benza et al. (2010) | Education | Nursing homes and senior centres | Majority female | 348 | Enhanced knowledge of PSU. | A significant increase in knowledge regarding the risks related to medication and alcohol use. |
| 4. Copeland, Blow, Barry. (2003) | BI | Primary care private sector and VA clinic | Majority white | 205 | Engagement with services | Significantly more veterans accessed medical outpatient services than those in the control group. |
| 5. D’Agostino et al. (2006) | Targeted service for dual diagnosis | Community network/referral system | 41 men (41.4%) 58 women | 120 | Treatment completion rates | The multidimensional motivational approach were more likely to result in treatment completion than the traditional referral approach. No significance difference mentioned |
| 6. Eliason, Skinstad. (2001) | Education | Community senior day centre | All white Majority women | 26 | Enhanced knowledge of PSU | Participants’ knowledge increased post-test. The difference was statistically different. |
| 7. Fink et al. (2005) | Education | Community primary care | All female Majority white | 711 | Alcohol consumption | Patients in the intervention group significantly decreased their alcohol consumption. |
| 8. Fleming et al. (1999) | BI | Community based primary care practices | Majority male | 158 | Alcohol consumption. Number of binge drinking episodes. Health status. | Participants who received the BI demonstrated a significant reduction in 7-day alcohol use, episodes of binge drinking, and frequency of excessive drinking. |
| 9. Gottlieb-Hansen et al. (2012) | BI | Community alcohol service | Mix of men and women | 772 | Alcohol consumption | There was no statistically significant effect of BI reducing alcohol consumption. |
| 10. Kuerbis et al. (2013) | BI | Secondary data analysis of three RCTs | Male White | 38 | Alcohol consumption | OA responded to most interventions. Those who received brief evidence supported treatments were variable but mostly responsive. OA responded more strongly than MA with the exception of MI. |
| 11. Lee et al. (2009) | Harm reduction vs. 12 step model | Community based alcohol service | Male 58% 50% non-Hispanic white; 35% African American | 34 | Engagement with services, alcohol consumption | Participants in the harm reduction arm showed a significant decrease in the number of drinks and number of binge drinking episodes. No significant changes in these outcomes in the 12-step model. Participants more likely to access treatment in the harm reduction group. |
| 12. McCann, Wadd & Gill Crofts. (2017) | Provision of wet care home | Residential care homes | Mix of men and women | 54 | Impact of harm reduction, what works and why it works on wellbeing of residents | Themes included; Safety and security offered from risky and chaotic lifestyles. Regular health checks, reduced use of emergency services, lower risk of falls, Reduced alcohol use with some residents becoming abstinent and others moved on to detox and community alcohol treatment. |
| 13. Oslin et al. (2004) | Unified Psychogeriatric Biopsychosocial Evaluation and Treatment | Department of Veterans Affairs Medical Centres | Majority white and male | 2637 | Behavioural health symptoms of older veterans. | No differences between UPBEAT and usual care patients on symptom or functional outcomes at any follow-up point Exploratory analyses suggested greater improvements in depressive symptoms in those assigned to UPBEAT care. |
| 14. Oslin et al. (2005) | Targeted rehabilitation service | Community Residential Rehab facility | Male = 56% White = 97.5% | 1358 | Abstinence, addiction severity and MH | No significantly different outcomes in abstinence rates at 1-month, older adults engaged informal post-discharge aftercare less than MA adults. |
| 15. Outlaw et al. (2012) | CBT and self-management | Dual diagnosis service for OA public housing | Majority male and white | 199 | Alcohol consumption, binge drinking, stress levels | Program completers significantly decreased use of nonmedical prescription drugs, improved cognitive functioning, MH, vitality, and lack of bodily pain. |
| 16. Poole et al. (2009) | Group therapy | Community clinic setting | Majority men and Canadian | 12 | Mental health and substance use. | Themes - acceptance, befriending, guilt, power, and holding on. Narrative therapy is well suited to older adults coping with mental health and substance use |
| 17. Rao. (2014) | Targeted community nursing service | Community mental health | None mentioned | 108 | Alcohol consumption | 108 patients aged 65 and over with alcohol misuse were identified. 50 patients were taken on by community MH teams, of whom 19 patients had achieved abstinence from alcohol or controlled drinking at the 6 months follow up 38%. |
| 18. Schonfeld et al. (2015) | BI | Services targeting older people: | Majority females and white | 85 001 | Substance use | 8165 clients were at moderate or high risk. Most received brief intervention for alcohol or medication misuse. Six-month follow-ups revealed a significant decrease in substance use. |
| 19. Watson et al. (2013) | Stepped care vs. BI | Primary care | Majority male | 529 | Alcohol consumption | Stepped care does not confer an advantage over minimal intervention in terms of reduction in alcohol consumption Cost-effectiveness analysis suggested stepped care intervention is more likely to generate greater health benefits. |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hafford-Letchfield, T.; McQuarrie, T.; Clancy, C.; Thom, B.; Jain, B. Community Based Interventions for Problematic Substance Use in Later Life: A Systematic Review of Evaluated Studies and Their Outcomes. Int. J. Environ. Res. Public Health 2020, 17, 7994. https://doi.org/10.3390/ijerph17217994
Hafford-Letchfield T, McQuarrie T, Clancy C, Thom B, Jain B. Community Based Interventions for Problematic Substance Use in Later Life: A Systematic Review of Evaluated Studies and Their Outcomes. International Journal of Environmental Research and Public Health. 2020; 17(21):7994. https://doi.org/10.3390/ijerph17217994
Chicago/Turabian StyleHafford-Letchfield, Trish, Tricia McQuarrie, Carmel Clancy, Betsy Thom, and Briony Jain. 2020. "Community Based Interventions for Problematic Substance Use in Later Life: A Systematic Review of Evaluated Studies and Their Outcomes" International Journal of Environmental Research and Public Health 17, no. 21: 7994. https://doi.org/10.3390/ijerph17217994
APA StyleHafford-Letchfield, T., McQuarrie, T., Clancy, C., Thom, B., & Jain, B. (2020). Community Based Interventions for Problematic Substance Use in Later Life: A Systematic Review of Evaluated Studies and Their Outcomes. International Journal of Environmental Research and Public Health, 17(21), 7994. https://doi.org/10.3390/ijerph17217994






