Clinical Behavior of Ceramic, Hybrid and Composite Onlays. A Systematic Review and Meta-Analysis
Abstract
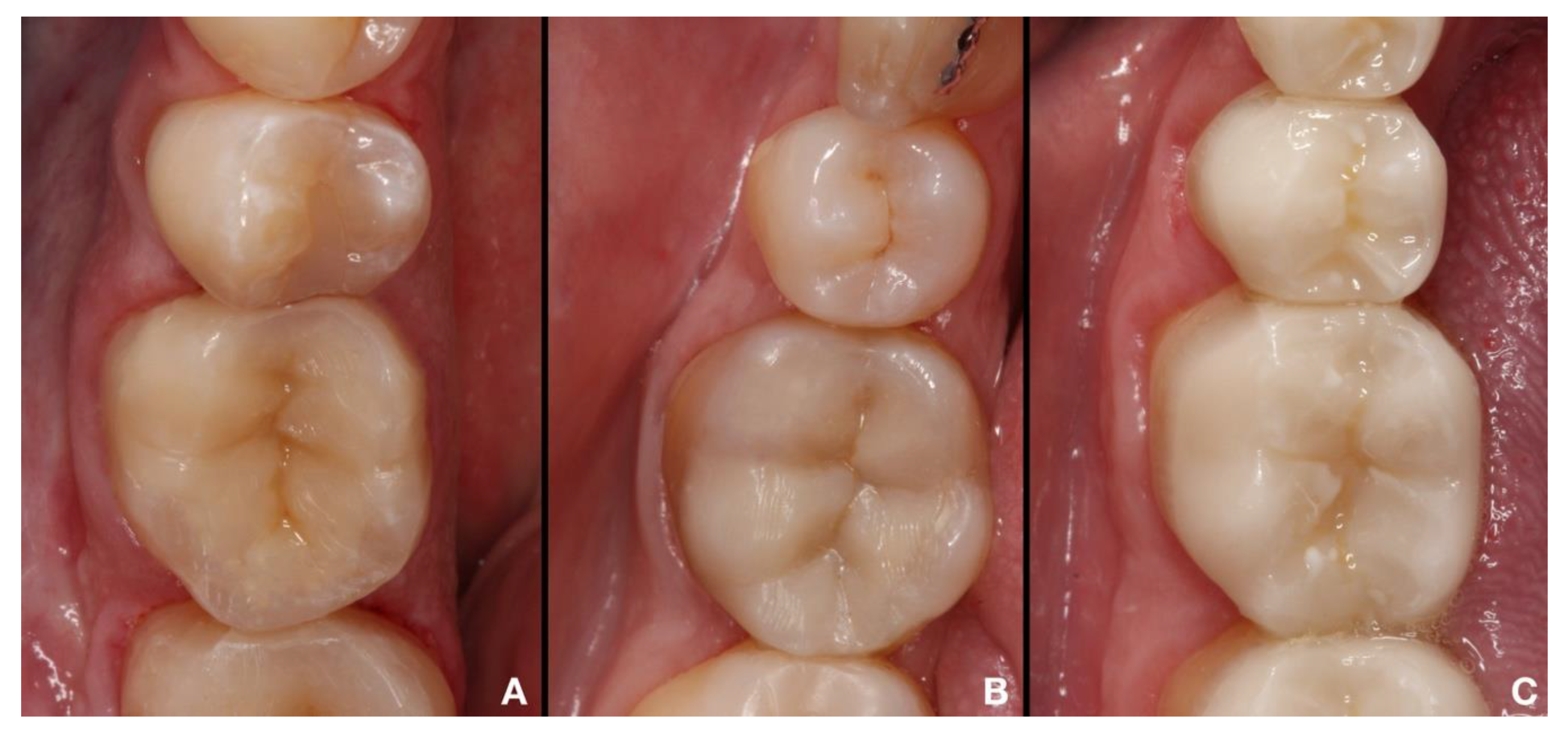
1. Introduction
2. Materials and Methods
3. Results
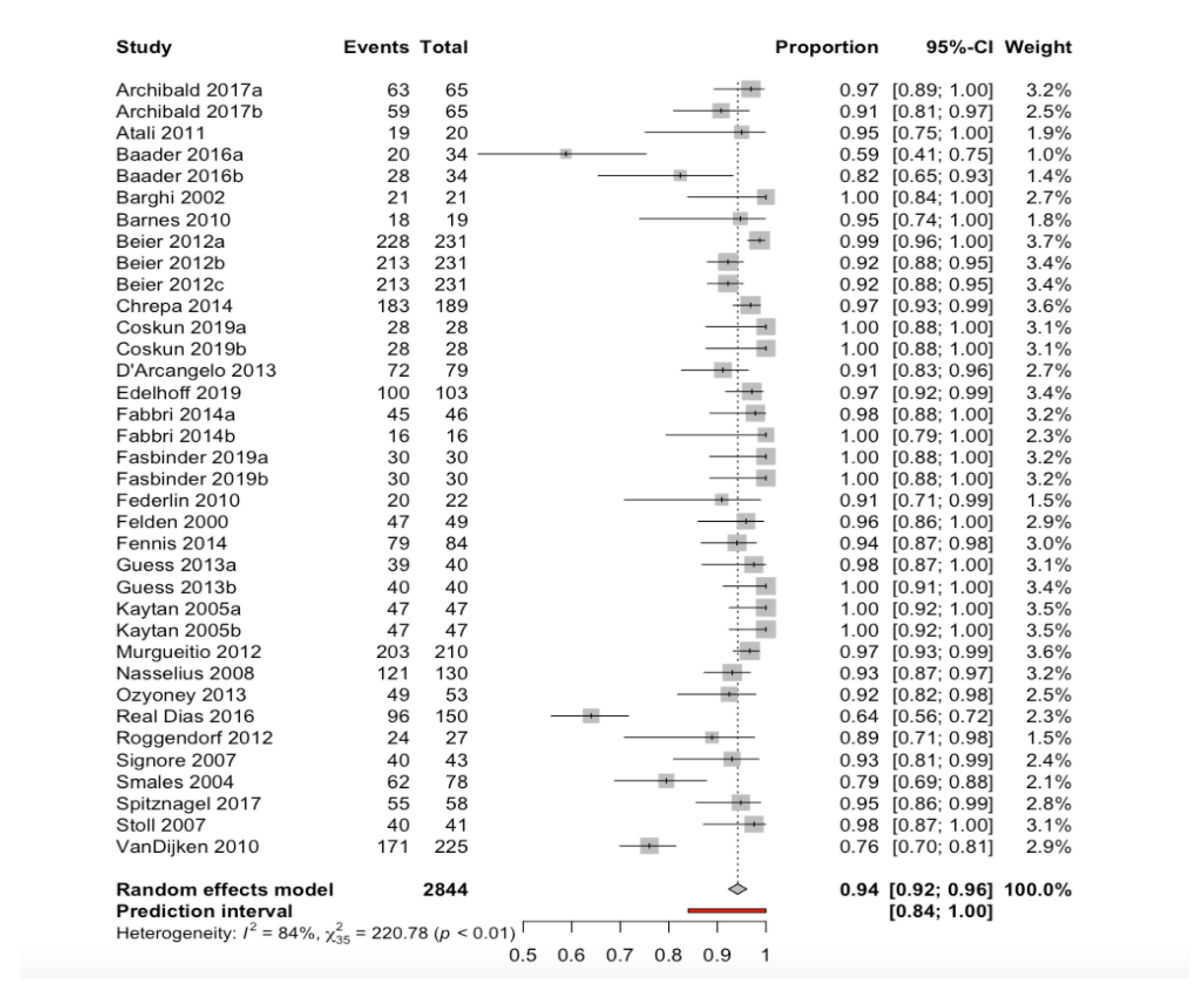
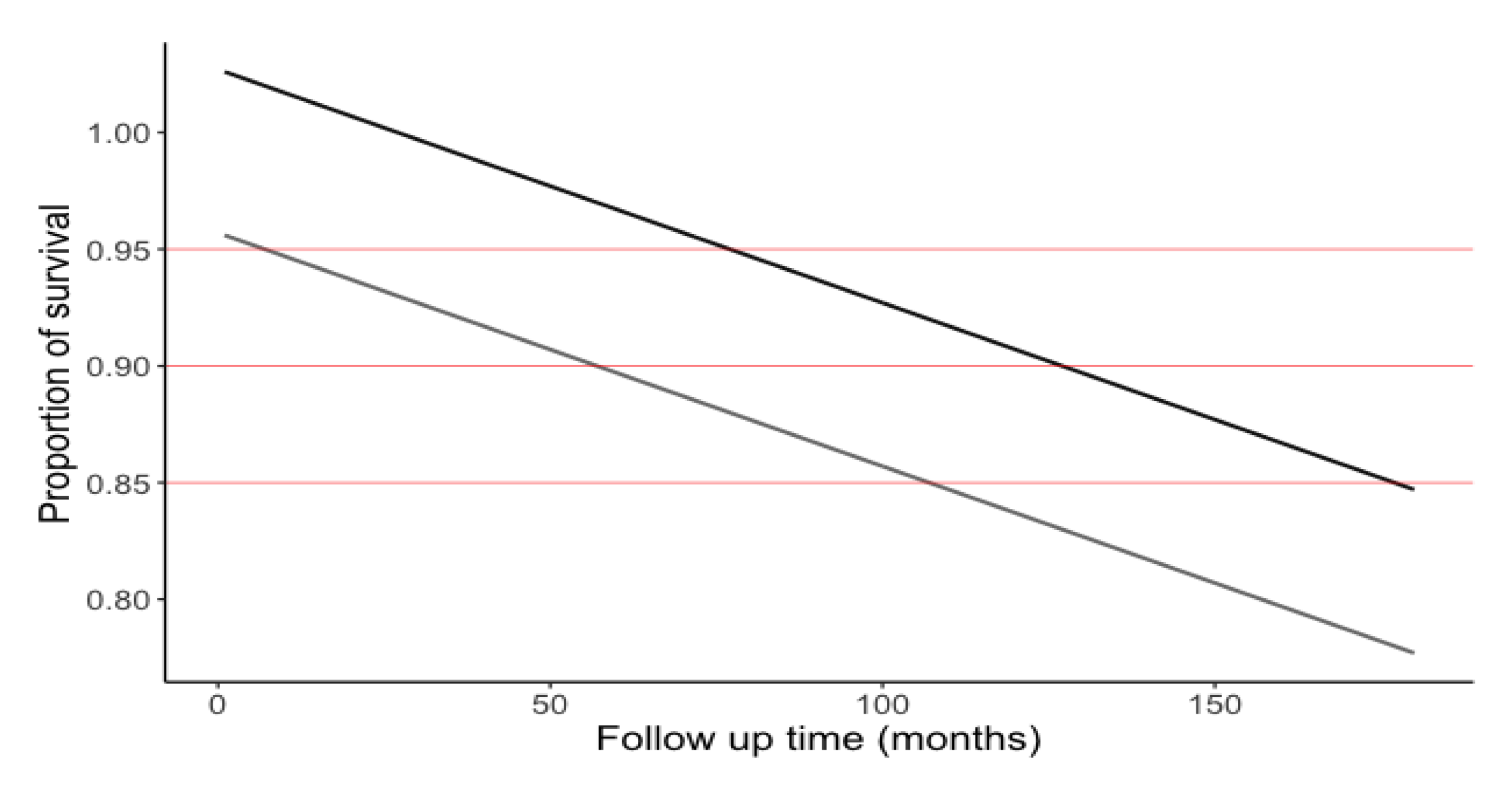
3.1. Percentage Survival of the Restorations
3.2. Reasons for Restoration Failure
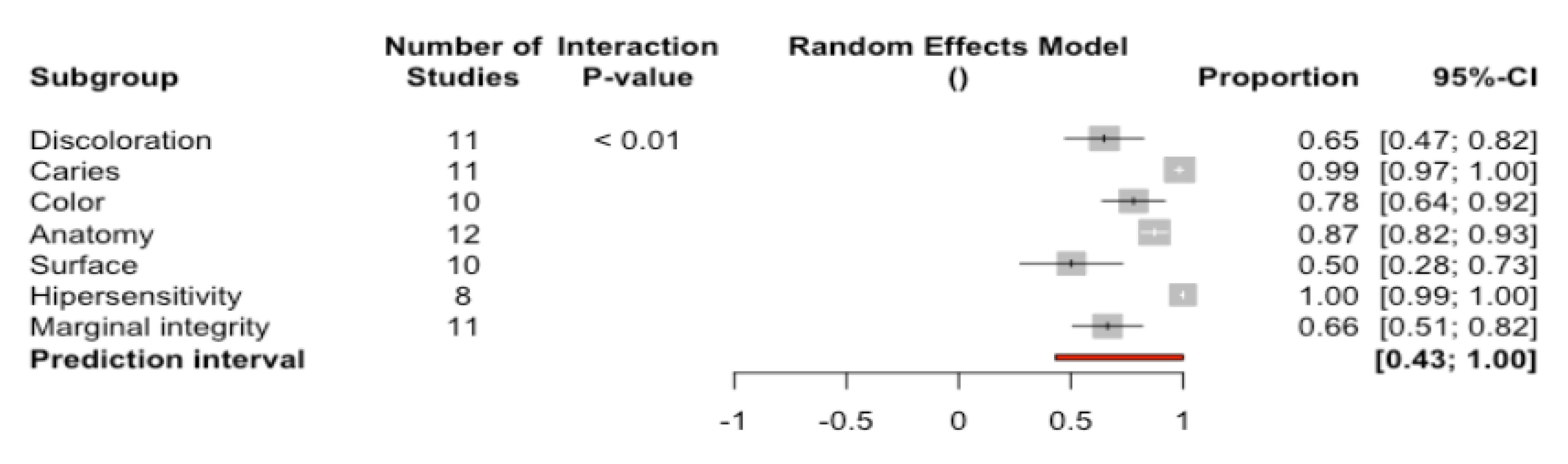
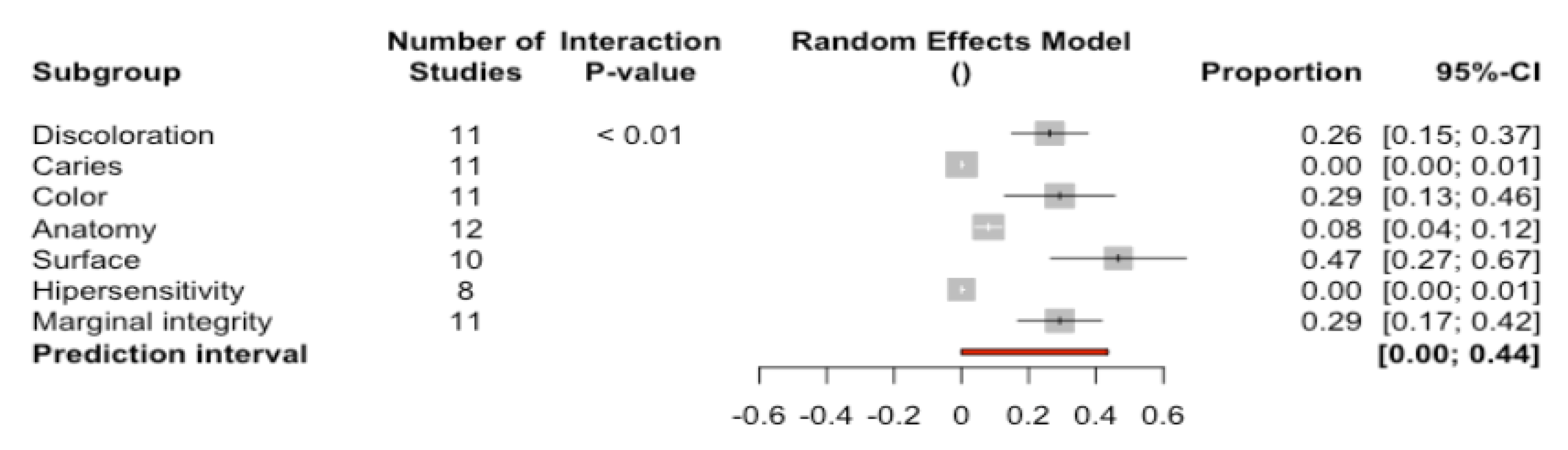
3.3. Clinical Evaluation of the Restorations Using the Modified USPHS Criteria
3.4. Clinical Evaluation of the Restorations as Success, Survival or Failure
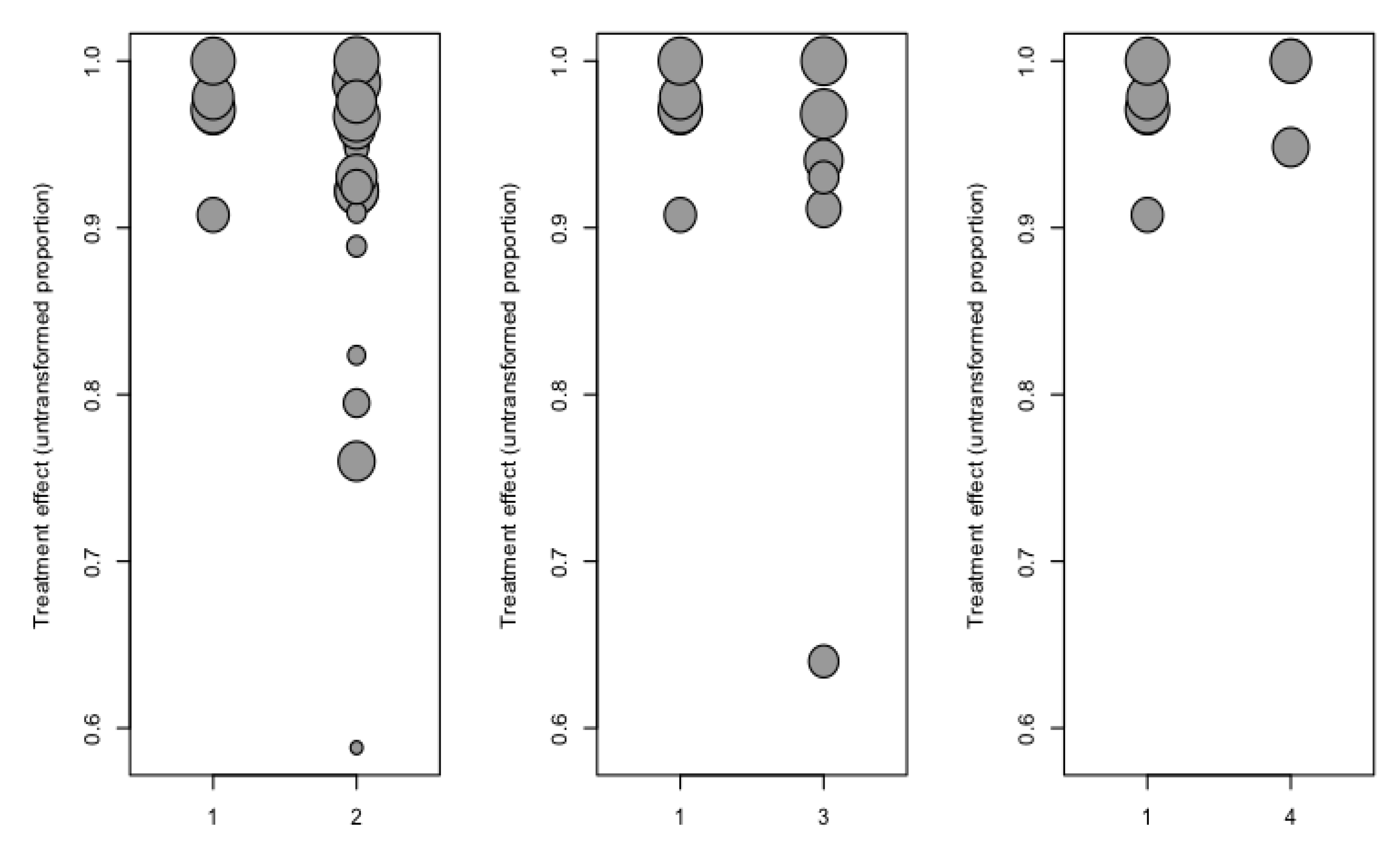
3.5. Publication Bias
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Fron Chabouis, H.; Smail Faugeron, V.; Attal, J.-P. Clinical Efficacy of Composite versus Ceramic Inlays and Onlays: A Systematic Review. Dent. Mater. 2013, 29, 1209–1218. [Google Scholar] [CrossRef]
- Höland, W.; Schweiger, M.; Watzke, R.; Peschke, A.; Kappert, H. Ceramics as Biomaterials for Dental Restoration. Exp. Rev. Med. Dev. 2008, 5, 729–745. [Google Scholar] [CrossRef] [PubMed]
- Terry, D.; Leinfelder, K.; Maragos, C. Developing Form, Function, and Natural Aesthetics with Laboratory-Processed Composite Resin—Part I. Pract. Proced. Aesthet. Dent. 2005, 17, 313–320. [Google Scholar] [PubMed]
- Jaeggi, T.; Lussi, A. Erosionen Bei Kindern Im Frühen Schulalter [Erosion in Early School-Age Children]. Schweiz Monatsschr Zahnmed. 2004, 114, 876–881. [Google Scholar]
- Lussi, A.; Carvalho, T.S. Erosive Tooth Wear: A Multifactorial Condition of Growing Concern and Increasing Knowledge. In Monographs in Oral Science; Lussi, A., Ganss, C., Eds.; S. KARGER AG: Basel, Switzerland, 2014; Volume 25, pp. 1–15. [Google Scholar] [CrossRef]
- Loomans, B.; Opdam, N.; Attin, T.; Bartlett, D.; Edelhoff, D.; Frankenberger, R.; Benic, G.; Ramseyer, S.; Wetselaar, P.; Sterenborg, B.; et al. Severe Tooth Wear: European Consensus Statement on Management Guidelines. J. Adhes. Dent. 2017, 19, 111–119. [Google Scholar]
- Edelhoff, D.; Güth, J.F.; Erdelt, K.; Brix, O.; Liebermann, A. Clinical Performance of Occlusal Onlays Made of Lithium Disilicate Ceramic in Patients with Severe Tooth Wear up to 11 Years. Dent. Mater. 2019, 35, 1319–1330. [Google Scholar] [CrossRef]
- Vagropoulou, G.I.; Klifopoulou, G.L.; Vlahou, S.G.; Hirayama, H.; Michalakis, K. Complications and Survival Rates of Inlays and Onlays vs Complete Coverage Restorations: A Systematic Review and Analysis of Studies. J. Oral. Rehabil. 2018, 45, 903–920. [Google Scholar] [CrossRef]
- Coşkun, E.; Aslan, Y.U.; Özkan, Y.K. Evaluation of Two Different CAD-CAM Inlay-onlays in a Split-mouth Study: 2-year Clinical Follow-up. J. Esthet. Restor. Dent. 2020, 32, 244–250. [Google Scholar] [CrossRef] [PubMed]
- Frankenberger, R.; Taschner, M.; Garcia-Godoy, F.; Petschelt, A.; Krämer, N. Leucite-Reinforced Glass Ceramic Inlays and Onlays after 12 Years. J. Adhes. Dent. 2008, 10, 393–398. [Google Scholar]
- Guess, P.C.; Selz, C.F.; Steinhart, Y.-N.; Stampf, S.; Strub, J.R. Prospective Clinical Split-Mouth Study of Pressed and CAD/CAM All-Ceramic Partial-Coverage Restorations: 7-Year Results. Int. J. Prosthodont 2013, 26, 21–25. [Google Scholar] [CrossRef]
- Pjetursson, B.E.; Lang, N.P. Prosthetic Treatment Planning on the Basis of Scientific Evidence. J. Oral. Rehabil. 2008, 35, 72–79. [Google Scholar] [CrossRef] [PubMed]
- Raedel, M.; Hartmann, A.; Priess, H.-W.; Bohm, S.; Samietz, S.; Konstantinidis, I.; Walter, M.H. Re-Interventions after Restoring Teeth—Mining an Insurance Database. J. Dent. 2017, 57, 14–19. [Google Scholar] [CrossRef] [PubMed]
- Krämer, N.; Taschner, M.; Lohbauer, U.; Petschelt, A.; Frankenberger, R. Totally Bonded Ceramic Inlays and Onlays after Eight Years. J. Adhes. Dent. 2008, 10, 307–314. [Google Scholar] [PubMed]
- Santos, G.J.; Santos, M.J.; Rizkalla, A.; Madani, D.; El-Mowafy, O. Overview of CEREC CAD/CAM Chairside System. Gen. Dent. 2013, 61, 36–41. [Google Scholar]
- Krämer, N.; Frankenberger, R.; Pelka, M.; Petschelt, A. IPS Empress Inlays and Onlays after Four Years—A Clinical Study. J. Dent. 1999, 27, 325–331. [Google Scholar] [CrossRef]
- The Glossary of Prosthodontic Terms. J. Prosthet. Dent. 2017, 117, C1–e105. [CrossRef]
- Felden, A.; Schmalz, G.; Federlin, M.; Hiller, K.-A. Retrospective Clinical Investigation and Survival Analysis on Ceramic Inlays and Partial Ceramic Crowns: Results up to 7 Years. Clin. Oral. Investig. 1998, 2, 161–167. [Google Scholar] [CrossRef]
- Fuzzi, M.; Rappelli, G. Survival Rate of Ceramic Inlays. J. Dent. 1998, 26, 623–626. [Google Scholar] [CrossRef]
- Schulz, P.; Johansson, A.; Arvidson, K.; Schulz, P.; Johansson, A.; Arvidson, K. A Retrospective Study of Mirage Ceramic Inlays over up to 9 Years. Int. J. Prosthodont. 2003, 16, 510–514. [Google Scholar] [PubMed]
- Morimoto, S.; Rebello de Sampaio, F.; Braga, M.; Sesma, N.; Özcan, M. Survival Rate of Resin and Ceramic Inlays, Onlays, and Overlays: A Systematic Review and Meta-Analysis. J. Dent. Res. 2016, 95, 985–994. [Google Scholar] [CrossRef]
- Wassell, R.; Walls, A.; McCabe, J. Direct Composite Inlays versus Conventional Composite Restorations: Three-Year Clinical Results. Br. Dent. J. 1995, 179, 343–349. [Google Scholar] [CrossRef] [PubMed]
- Angeletaki, F.; Gkogkos, A.; Papazoglou, E.; Kloukos, D. Direct versus Indirect Inlay/Onlay Composite Restorations in Posterior Teeth. A Systematic Review and Meta-Analysis. J. Dent. 2016, 53, 12–21. [Google Scholar] [CrossRef] [PubMed]
- Duquia, R.C.S.; Osinaga, P.W.R.; Demarco, F.F.; Habekost, L.V.; Conceição, E.N. Cervical Microleakage in MOD Restorations: In Vitro Comparison of Indirect and Direct Composite. OP-DENT 2006, 31, 682–687. [Google Scholar] [CrossRef] [PubMed]
- Barone, A.; Derchi, G.; Rossi, A.; Marconcini, S.; Covani, U. Longitudinal Clinical Evaluation of Bonded Composite Inlays: A 3-Year Study. Quintessence Int. 2008, 39, 65–71. [Google Scholar]
- Mangani, F.; Marini, S.; Barabanti, N.; Preti, A.; Cerutti, A. The Success of Indirect Restorations in Posterior Teeth: A Systematic Review of the Literature. Minerva Stomatol. 2015, 64, 11. [Google Scholar]
- Fabianelli, A. A Clinical Trial of Empress II Porcelain Inlays Luted to Vital Teeth with a Dual-Curing Adhesive System and a Self-Curing Resin Cement. J. Adhes. Dent. 2006, 8, 427–431. [Google Scholar]
- Guess, P.C.; Strub, J.R.; Steinhart, N.; Wolkewitz, M.; Stappert, C.F.J. All-Ceramic Partial Coverage Restorations—Midterm Results of a 5-Year Prospective Clinical Splitmouth Study. J. Dent. 2009, 37, 627–637. [Google Scholar] [CrossRef]
- Spitznagel, F.A.; Scholz, K.J.; Strub, J.R.; Vach, K.; Gierthmuehlen, P.C. Polymer-Infiltrated Ceramic CAD/CAM Inlays and Partial Coverage Restorations: 3-Year Results of a Prospective Clinical Study over 5 Years. Clin. Oral. Investig. 2018, 22, 1973–1983. [Google Scholar] [CrossRef]
- Goujat, A.; Abouelleil, H.; Colon, P.; Jeannin, C.; Pradelle, N.; Seux, D.; Grosgogeat, B. Marginal and Internal Fit of CAD-CAM Inlay/Onlay Restorations: A Systematic Review of in Vitro Studies. J. Prosthet. D. 2019, 121, 590–597.e3. [Google Scholar] [CrossRef]
- Cappare, P.; Sannino, G.; Minoli, M.; Montemezzi, P.; Ferrini, F. Conventional versus Digital Impressions for Full Arch Screw-Retained Maxillary Rehabilitations: A Randomized Clinical Trial. IJERPH 2019, 16, 829. [Google Scholar] [CrossRef]
- Cattoni, F.; Teté, G.; Calloni, A.M.; Manazza, F.; Gastaldi, G.; Capparè, P. Milled versus Moulded Mock-Ups Based on the Superimposition of 3D Meshes from Digital Oral Impressions: A Comparative in Vitro Study in the Aesthetic Area. BMC Oral. Health. 2019, 19, 230. [Google Scholar] [CrossRef]
- Mante, F.; Ozer, F.; Walter, R.; Atlas, A.; Saleh, N.; Dietschi, D.; Blatz, M. The Current State of Adhesive Dentistry: A Guide for Clinical Practice. Comp. Contin. Educ. Dent. 2013, 34, 2–8. [Google Scholar]
- Kawai, K.; Isenberg, B.; Leinfelder, K. Effect of Gap Dimension on Composite Resin Cement Wear. Quintessence Int. 1994, 25, 53–58. [Google Scholar] [PubMed]
- Peumans, M.; Voet, M.; De Munck, J.; Van Landuyt, K.; Van Ende, A.; Van Meerbeek, B.; Peumans, M.; Voet, M.; De Munck, J. Four-Year Clinical Evalua- Tion of a Self-Adhesive Luting Agent for Ceramic Inlays. Clin Oral Investig. Clin. Oral. Investig. 2013, 17, 739–750. [Google Scholar] [CrossRef]
- Abduo, J.; Sambrook, R.J. Longevity of Ceramic Onlays: A Systematic Review. J. Esthet. Restor. Dent. 2018, 30, 193–215. [Google Scholar] [CrossRef] [PubMed]
- Amesti-Garaizabal; Agustín-Panadero; Verdejo-Solá; Fons-Font; Fernández-Estevan; Montiel-Company; Solá-Ruíz. Fracture Resistance of Partial Indirect Restorations Made With CAD/CAM Technology. A Systematic Review and Meta-Analysis. JCM 2019, 8, 1932. [Google Scholar] [CrossRef]
- Gracis, S.; Thompson, V.; Ferencz, J.; Silva, N.; Bonfante, E. A New Classification System for All-Cermic and Ceramic-like Restorative Materials. Int. J. Prosthodont. 2015, 23, 227–235. [Google Scholar]
- Solá-Ruíz, M.F.; Baima-Moscardó, A.; Selva-Otaolaurruchi, E.; Montiel-Company, J.M.; Agustín-Panadero, R.; Fons-Badal, C.; Fernández-Estevan, L. Wear in Antagonist Teeth Produced by Monolithic Zirconia Crowns: A Systematic Review and Meta-Analysis. JCM 2020, 9, 997. [Google Scholar] [CrossRef] [PubMed]
- Bergman, M. The Clinical Performance of Ceramic Inlays: A Review. Aust. Dent. J. 1999, 44, 157–168. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Tagtekin, D.; Özyöney, G.; Yanikoglu, F. Two-Year Clinical Evaluation of IPS Empress II Ceramic Onlays/Inlays. Oper. Dent. 2009, 34, 369–378. [Google Scholar] [CrossRef] [PubMed]
- Sampaio, F.B.W.R.; Özcan, M.; Gimenez, T.C.; Moreira, M.S.N.A.; Tedesco, T.K.; Morimoto, S. Effects of Manufacturing Methods on the Survival Rate of Ceramic and Indirect Composite Restorations: A Systematic Review and Meta-analysis. J. Esthet. Restor. Dent. 2019, 31, 561–571. [Google Scholar] [CrossRef] [PubMed]
- Wells, G.; Shea, B.; O’Connell, D.; Peterson, J.; Welch, V.; Losos, M.; Tugwell, P.; Wells, G.A.; Shea, B.; O’Connell, D.; et al. The Newcastle—Ottawa Scale (NOS) for Assessing the Quality of Non-Randomized Studies in Metanalyses. Available online: Http://Www.Ohri.ca/Programs/Clinical_epidemiology/Oxford.Asp (accessed on 20 December 2019).
- Verhagen, A.; de Vet, H.; de Bie, R.; Kessels, A.; Boers, M.; Bouter, L.; Knipschild, P. The Delphi List: A Criteria List for Quality Assessment of Randomized Clinical Trials for Conducting Systematic Reviews Developed by Delphi Consensus. J. Clin. Epidemiol. 1998, 51, 1235–1241. [Google Scholar] [CrossRef]
- Kaytan, B.; Onal, B.; Pamir, T.; Tezel, H. Clinical Evaluation of Indirect Resin Composite and Ceramic Onlays over a 24-Month Period. Gen. Dent. 2005, 53, 329–334. [Google Scholar] [PubMed]
- Schulte, A.G.; Vöckler, A.; Reinhardt, R. Longevity of Ceramic Inlays and Onlays Luted with a Solely Light-Curing Composite Resin. J. Dent. 2005, 33, 433–442. [Google Scholar] [CrossRef]
- Signore, A.; Benedicenti, S.; Covani; Ravera, G. A 4- to 6-Year Retrospective Clinical Study of Cracked Teeth Restored with Bonded Indirect Resin Composite Onlays. Prim. Dent. Care 2008, 15, 152. [Google Scholar] [CrossRef]
- Beier, U.; Kapferer, I.; Burtscher, D.; Giesinger, J.; Dumfahrt, H. Clinical Performance of All-Ceramic Inlay and Onlay Restorations in Posterior Teeth. Int. J. Prosthodont. 2012, 25, 395–402. [Google Scholar]
- Murgueitio, R.; Bernal, G. Three-Year Clinical Follow-Up of Posterior Teeth Restored with Leucite-Reinforced IPS Empress Onlays and Partial Veneer Crowns: Three-Year Clinical Follow-Up of Ceramic Onlays and Partial Crowns. J. Prosthodont. 2012, 21, 340–345. [Google Scholar] [CrossRef]
- D’Arcangelo, C.; Zarow, M.; De Angelis, F.; Vadini, M.; Paolantonio, M.; Giannoni, M.; D’Amario, M. Five-Year Retrospective Clinical Study of Indirect Composite Restorations Luted with a Light-Cured Composite in Posterior Teeth. Clin. Oral. Investig. 2014, 18, 615–624. [Google Scholar] [CrossRef]
- Fabbri, G.; Zarone, F.; Dellificorelli, G.; Cannistraro, G.; Lorenzi, M.D.; Mosca, A.; Sorrentino, R. Clinical Evaluation of 860 Anterior and Posterior Lithium Disilicate Restorations: Retrospective Study with a Mean Follow-up of 3 Years and a Maximum Observational Period of 6 Years. Restor. Dent. 2014, 34, 14. [Google Scholar] [CrossRef]
- Chrepa, V.; Konstantinidis, I.; Kotsakis, G.A.; Mitsias, M.E. The Survival of Indirect Composite Resin Onlays for the Restoration of Root Filled Teeth: A Retrospective Medium-Term Study. Int. Endod. J. 2014, 47, 967–973. [Google Scholar] [CrossRef]
- Belli, R.; Petschelt, A.; Hofner, B.; Hajtó, J.; Scherrer, S.S.; Lohbauer, U. Fracture Rates and Lifetime Estimations of CAD/CAM All-Ceramic Restorations. J. Dent. Res. 2016, 95, 67–73. [Google Scholar] [CrossRef]
- Baader, K.; Hiller, K.; Buchalla, W.; Federlin, M. Self-Adhesive Luting of Partial Ceramic Crowns: Selective Enamel Etching Leads to Higher Survival after 6.5 Years In Vivo. J. Adhes. Dent. 2016, 18, 69–79. [Google Scholar] [CrossRef] [PubMed]
- Archibald, J.J.; Santos, G.C.; Moraes Coelho Santos, M.J. Retrospective Clinical Evaluation of Ceramic Onlays Placed by Dental Students. J. Prosthet. Dent. 2018, 119, 743–748. [Google Scholar] [CrossRef] [PubMed]
- Felden, A.; Schmalz, G.; Hiller, K.-A. Retrospective Clinical Study and Survival Analysis on Partial Ceramic Crowns: Results up to 7 Years. Clin. Oral. Investig. 2000, 4, 199–205. [Google Scholar] [CrossRef]
- Barghi, N.; Berry, T. Clinical Evaluation of Etched Porcelain Onlays: A 4-Year Report. Comp. Contin. Educ. Dent. 2002, 23, 657–674. [Google Scholar]
- Smales, R.J.; Etemadi, S. Survival of Ceramic Onlays Placed with and without Metal Reinforcement. J. Prosthet. Dent. 2004, 91, 548–553. [Google Scholar] [CrossRef] [PubMed]
- Stoll, R.; Cappel, I.; Jablonski-Momeni, A.; Pieper, K.; Stachniss, V. Survival of Inlays and Partial Crowns Made of IPS Empress After a 10-Year Observation Period and in Relation to Various Treatment Parameters. OP-DENT 2007, 32, 556–563. [Google Scholar] [CrossRef]
- Naeselius, K.; Arnelund, C.; Molin, M. Clinical Evaluation of Allceramic Onlays: A 4-Year Retrospective Study. Int. J. Prosthodont. 2008, 21, 40–44. [Google Scholar]
- Federlin, M.; Hiller, K.; Schmalz, G. Controlled, Prospective Clinical Split-Mouth Study of Cast Gold vs. Ceramic Partial Crowns: 5.5 Year Results. Am. J. Dent. 2010, 23, 161–167. [Google Scholar]
- Van Dijken, J.W.V.; Hasselrot, L. A Prospective 15-Year Evaluation of Extensive Dentin–Enamel-Bonded Pressed Ceramic Coverages. Dent. Mater. 2010, 26, 929–939. [Google Scholar] [CrossRef]
- Barnes, D.; Gingell, J.; George, D.; Adachi, E.; Jefferies, S.; Sundar, V. Clinical Evaluation of an Allceramic Restorative System: A 36-Month Clinical Evaluation. Am. J. Dent. 2010, 23, 87–92. [Google Scholar] [PubMed]
- Atali, P.; Cakmakcioglu, O.; Topbasi, B.; Turkmen, C.; Suslen, O. IPS Empress Onlays Luted with Two Dual-Cured Resin Cements for Endodontically Treated Teeth: A 3-Year Clinical Evaluation. Int. J. Prosthodont. 2011, 24, 40–42. [Google Scholar] [PubMed]
- Roggendorf, M.J.; Kunzi, B.; Ebert, J.; Roggendorf, H.C.; Frankenberger, R.; Reich, S.M. Seven-Year Clinical Performance of CEREC-2 All-Ceramic CAD/CAM Restorations Placed within Deeply Destroyed Teeth. Clin. Oral. Investig. 2012, 16, 1413–1424. [Google Scholar] [CrossRef] [PubMed]
- Ozyoney, G.; Yan Koğlu, F.; Tağtekin, D.; Hayran, O. The Efficacy of Glass-Ceramic Onlays in the Restoration of Morphologically Compromised and Endodontically Treated Molars. Int. J. Prosthodont. 2013, 26, 230–234. [Google Scholar] [CrossRef]
- Fennis, W.; Kuijs, R.; Roeters, F.; Creugers, N.; Kreulen, C. Randomized Control Trial of Composite Cuspal Restorations: Five-Year Results. J. Dent. Res. 2014, 93, 36–41. [Google Scholar] [CrossRef]
- Dias, M.C.R.; Martins, J.N.R.; Chen, A.; Quaresma, S.A.; Luís, H.; Caramês, J. Prognosis of Indirect Composite Resin Cuspal Coverage on Endodontically Treated Premolars and Molars: An In Vivo Prospective Study: Prognosis of Indirect Composite Resin Cuspal Coverage. J. Prosthodont. 2018, 27, 598–604. [Google Scholar] [CrossRef]
- Fasbinder, D.J.; Neiva, G.F.; Heys, D.; Heys, R. Clinical Evaluation of Chairside Computer Assisted Design/Computer Assisted Machining Nano-ceramic Restorations: Five-year Status. J. Esthet. Restor. Dent. 2020, 32, 193–203. [Google Scholar] [CrossRef]
- Zimmer, S.; Göhlich, O.; Rüttermann, S.; Lang, H.; Raab, W.H.-M.; Barthel, C.R. Long-Term Survival of Cerec Restorations: A 10-Year Study. OP-DENT 2008, 33, 484–487. [Google Scholar] [CrossRef]
- Bayne, S. Correlation of Clinical Performance with in Vitro Test of Restorative Dental Materials That Use Polymer-Based Matrices. Dent. Mater. 2009, 28, 52–71. [Google Scholar] [CrossRef]
- Lee, A.; He, L.H.; Lyons, K.; Swain, M.V. Tooth Wear and Wear Investigations in Dentistry: TOOTH WEAR. J. Oral Rehabil. 2012, 39, 217–225. [Google Scholar] [CrossRef]
- Van Dijken, J. Direct Resin Composite Inlays/Onlays: An 11 Year Follow-Up. J. Dent. 2000, 28, 299–306. [Google Scholar] [CrossRef]
- Manhart, J.; Neuerer, P.; Scheibenbogen-Fuchsbrunner, A.; Hickel, R. Three-Year Clinical Evaluation of Direct and Indirect Composite Restorations in Posterior Teeth. J. Prosthet. Dent. 2000, 84, 289–296. [Google Scholar] [CrossRef] [PubMed]





| AUTHOR (Year) | SELECTION | COMPARABILITY | OUTCOMES | TOTAL | |||||
|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5–6 | 7 | 8 | 9 | ||
| Kaytan et al. (2005) [45] | * | * | * (Ceramic/composite) | * | * | * | * | * | 8/9 |
| Schulte et al. (2005) [46] | * | NA | - | * | - | * | * | * | 5/9 |
| Signore et al. (2007) [47] | * | NA | - | * | - | * | * | * | 5/9 |
| Beier et al. (2012) [48] | * | NA | * (bruxism yes/no) | * | * | * | * | * | 7/9 |
| Murgueitio et al. (2012) [49] | * | NA | - | * | - | * | * | * | 5/9 |
| Guess et al. (2013) [11] | * | * | * (pressed/CAD-CAM) | * | * | * | * | * | 8/9 |
| D’Arcangelo et al. (2014) [50] | * | NA | - | * | - | * | * | * | 5/9 |
| Fabbri et al. (2014) [51] | * | * | * (veneered/monolithic) | * | * | * | * | * | 8/9 |
| Chrepa et al. (2014) [52] | * | NA | - | * | - | * | * | * | 5/9 |
| Belli et al. (2016) [53] | * | * | * (emax CAD/empress CAD) | * | * | * | * | * | 8/9 |
| Baader et al. (2016) [54] | * | * | * (selective etching yes/no) | * | * | * | * | * | 8/9 |
| Archibald et al. (2017) [55] | * | * | * (emax press/emax CAD) | * | * | * | * | * | 8/9 |
| AUTHOR (Year) | Criteria | Total | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | ||
| Felden et al. (2000) [56] | No | No | No | No | No | No | No | Yes | Yes | Yes | Yes | 4 |
| Barghi et al. (2002) [57] | Yes | No | No | No | No | No | No | Yes | Yes | Yes | Yes | 5 |
| Smales et al. (2004) [58] | No | No | No | No | No | No | No | Yes | Yes | Yes | Yes | 4 |
| Stoll et al. (2007) [59] | No | No | No | No | No | No | No | Yes | Yes | Yes | Yes | 4 |
| Naeselius et al. (2008) [60] | Yes | No | No | No | No | No | Yes | Yes | Yes | Yes | Yes | 6 |
| Federlin et al. (2010) [61] | Yes | Yes | No | Yes | No | No | Yes | Yes | Yes | Yes | Yes | 8 |
| Van Djken et al. (2010) [62] | Yes | No | No | No | No | No | No | Yes | Yes | Yes | Yes | 5 |
| Barnes et al. (2010) [63] | Yes | No | No | No | No | No | No | Yes | Yes | Yes | Yes | 5 |
| Atali et al. (2011) [64] | Yes | Yes | No | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | 10 |
| Roggendorf et al. (2012) [65] | Yes | No | No | No | No | No | No | Yes | Yes | Yes | Yes | 5 |
| Ozyoney et al. (2013) [66] | Yes | No | No | No | No | No | No | Yes | Yes | Yes | Yes | 5 |
| Fennis et al. (2014) [67] | Yes | Yes | No | Yes | No | No | No | Yes | Yes | Yes | Yes | 7 |
| Real Dias et al. (2016) [68] | Yes | No | No | No | No | No | No | Yes | Yes | Yes | Yes | 5 |
| Spitznagel et al. (2017) [29] | Yes | No | No | No | No | No | No | Yes | Yes | Yes | Yes | 5 |
| Cosçkun et al. (2019) [9] | Yes | Yes | No | Yes | No | No | No | Yes | Yes | Yes | Yes | 7 |
| Fasbinder et al. (2019) [69] | Yes | Yes | No | Yes | No | No | Yes | Yes | Yes | Yes | Yes | 8 |
| Edelhoff et al. (2019) [7] | Yes | No | No | No | No | No | No | Yes | Yes | Yes | Yes | 5 |
| Subgroup | Number of Studies | Interaction p-Value | Proportion | 95%CI |
|---|---|---|---|---|
| Lithium disilicate | 8 | <0.01 | 0.98 | [0.96; 1.00] |
| Feldspathic ceramic | 18 | 0.93 | [0.90; 0.96] | |
| Composites | 5 | 0.90 | [0.83; 0.98] | |
| Hybrids | 3 | 0.99 | [0.96; 1.00] | |
| Prediction interval | [0.84; 1.00] |
| Covariate | Beta Coefficient | 95%CI | Z-Value | p-Value |
|---|---|---|---|---|
| Intercept | 1.027 | 0.979, 1.075 | 42.3 | <0.001 |
| Follow-up time | −0.001 | −0.002, −0.001 | −3.49 | 0.001 * |
| Material: Feldspathic ceramic | −0.022 | −0.069, 0.025 | −0.93 | 0.353 |
| Material: Composites | −0.064 | −0.121, −0.007 | −2.19 | 0.028 * |
| Material: Hybrids | −0.003 | −0.073, 0.067 | −0.08 | 0.940 |
| Author, Year | Title, Journal | Material | Luting Agent in Cementation |
|---|---|---|---|
| Fabbri et al. (2014) [51] | Clinical evaluation of 860 anterior and posterior lithium disilicate restorations: Retrospective study with a mean follow-up of 3 years and a maximum observational period of 6 years The International Journal of Periodontics & Restorative Dentistry | Feldspathic ceramic reinforced with lithium disilicate | Restoration: HF 20 sec. 4.5% (IPS ceramic gel) Monobond S. Optibond FL Tooth: Orthophosphoric ac. 37% 30 sec. Optibond FL Fluid composite resin (Gradia Direct Flow; Tetric EvoFlow) or dual cure composite systems (Variolink II) |
| Federlin et al. (2010) [61] | Controlled, prospective clinical split-mouth study of cast gold vs. ceramic partial crowns: 5.5 year results American Journal of Dentistry | Conventional feldspathic ceramic CAD-CAM (Vita 3D Master CEREC Mark II) | Dual cure composite cement (Variolink IIg/high viscosity) |
| D’Arcangelo et al. (2014) [50] | Five-year retrospective clinical study of indirect composite restorations luted with a light-cured composite in posterior teeth Clin Oral Invest | Composite | Restoration: EnaBond light-curing Aluminum oxide powder 50 μm Tooth: Immediate dentin sealing Orthophosphoric ac. 37% 30 sec. EnaBond light-curing EnaHeat Pre-heated (55 °C) photopolymerizing composite |
| Belli et al. (2016) [53] | Fracture Rates and Lifetime Estimations of CAD/CAM All-ceramic Restorations Journal of Dental Research | Feldspathic ceramic reinforced with lithium disilicate (emax CAD)/Leucite-reinforced ceramic (Empres CAD) | NR |
| Murgueitio et al. (2012) [49] | Three-Year Clinical Follow-Up of Posterior Teeth Restored with Leucite-Reinforced IPS Empress Onlays and Partial Veneer Crowns American College of Prosthodontists | Leucite-reinforced ceramic (IPS Empress) | Restoration: HF 20 sec. 5% (Ivoclar Vivadent) Monobond S. Excite DSC. Tooth: Orthophosphoric ac. 37% 20 sec. (selective enamel etching) Excite DSC. Dual cure resin cement (Variolink II) |
| Chrepa et al. (2014) [52] | The survival of indirect composite resin onlays for the restoration of root filled teeth: a retrospective medium-term study International Endodontic Journal | Composite (Gradia GC) | Dual cure, self-etching resin cement TotalCem |
| Archibald et al. (2017) [55] | Retrospective clinical evaluation of ceramic onlays placed by dental students The Journal of Prosthetic Dentistry | Feldspathic ceramic reinforced with lithium disilicate IPS emax Press/IPS emax CAD | Restoration: HF 20 sec. 10% (Prosthetic Etchant Gel) Monobond S. Multilink Primer or Excite DSC/or Scotchbond Universal Adhesive Tooth: Orthophosphoric ac. 35% 30 sec. Multilink Primer or Excite DSC/or Scotchbond Universal Adhesive Dual polymerizing cement (Variolink II or RelyX Ultimate) |
| Fennis et al. (2014) [67] | Randomized Control Trial of Composite Cuspal Restorations: Five-year Results Journal of Dental Research | Composite (Essentia, Kuraray) | Restoration: Blasting 15 sec. with aluminum oxide 50 μm Orthophosphoric ac. 37% Clearfil SE Bond primer mixed with Clearfil bond Activator Tooth: Orthophosphoric ac. 37% 20 sec. in enamel ED primer (self-etching primer) applied to enamel and dentin 60 sec. Dual cure composite resin (Panavia F) |
| Schulte et al. (2005) [46] | Longevity of ceramic inlays and onlays luted with a solely light-curing composite resin Journal of Dentistry | Leucite-reinforced ceramic (IPS Empress) | Restoration: HF (Vita ceramics etch) Monobond S. Heliobond. Tooth: Orthophosphoric ac. 37% Syntac classic Heliobond Photopolymerizing composite resin (Tetric) |
| Spitznagel et al. (2018) [29] | Polymer-infiltrated ceramic CAD/CAM inlays and partial coverage restorations: 3-year results of a prospective clinical study over 5 years Clinical Oral Investigations | Hybrid ceramic material (Vita Enamic CAD-CAM) | Restoration: HF 4.9% (IPS ceramic gel) Monobond S. Optibond FL Tooth: Orthophosphoric ac. 37% enamel 40 sec./dentin 15 sec. Syntac Primer Sytac Adhesive Heliobond Dual cure resin cement (Variolink II) |
| Guess et al. (2013) [11] | Prospective Clinical Split-Mouth Study of Pressed and CAD/CAM All-Ceramic Partial-Coverage Restorations: 7-Year Results International Journal of Prosthodontics | Feldspathic ceramic reinforced with lithium disilicate (IPS emax Press)/Leucite-reinforced ceramic (ProCAD) CAD-CAM | Photopolymerizing hybrid resin cement (Tetric/Syntac Classic) |
| Roggendorf et al. (2012) [65] | Seven-year clinical performance of CEREC-2 all-ceramic CAD/CAM restorations placed within deeply destroyed teeth Clinical Oral Ivestigation | Conventional feldspathic ceramic (VITABLOCS Mark II for CEREC)/Leucite-reinforced ceramic (ProCAD) | Restoration: HF 4.9% (IPS ceramic gel) Monobond S. Optibond FL Tooth: Orthophosphoric ac. 35% Sytac Photopolymerizing hybrid resin cement (Tetric Ceram) dual cure (Variolink Ultra) |
| Stoll et al. (2007) [59] | Survival of Inlays and Partial Crowns Made of IPS Empress After a 10-year Observation Period and in Relation to Various Treatment Parameters Operative Dentistry | Leucite-reinforced ceramic (IPS Empress) | Restoration: HF 4.9% (IPS ceramic gel) Monobond S. Optibond FL Tooth: Orthophosphoric ac. 35% Sytac Resin cement (Variolink cement or Variolink Ultra) |
| Beier et al. (2012) [48] | Clinical Performance of All-Ceramic Inlay and Onlay Restorations in Posterior Teeth The International Journal of Prosthodontics | Conventional feldspathic ceramic, sintered | Optibond FL Syntac Classic Optec cement 3M Cement Dual Zement Variolink High Viscosity (Dual cure composite cements) |
| Signore et al. (2008) [47] | A 4- to 6-Year Retrospective Clinical Study of Cracked Teeth Restored with Bonded Indirect Resin Composite Onlays Int J Prosthodont | Composite (Sculpture and Sculpture Plus) | Restoration: Monobond S. Tooth: Orthophosphoric ac. 15 sec. Ecusit PrimerMono (dentin adhesive) Orthophosphoric ac. 37% (total etch) Ecusit PrimerMono Dual resin cement (Variolink cement) |
| Real Dias et al. (2016) [68] | Prognosis of Indirect Composite Resin Cuspal Coverage on Endodontically Treated Premolars and Molars: An In Vivo Prospective Study Journal of Prosthodontics | Composite (Adoro System) | Cement RelyX Unicem-Tr |
| Felden et al. (2000) [56] | Retrospective clinical study and survival analysis on partial ceramic crowns: results up to 7 years. Clin Oral Investig. | Feldspathic ceramic reinforced with lithium disilicate (IPS Empress II) | Composite cement (dual cure, photopolymerizing cure) |
| Van Dijken et al. (2010) [62] | A prospective 15-year evaluation of extensive dentin-enamel-bonded pressed ceramic coverages. Dent Mater. | Leucite-reinforced ceramic, pressed | Restoration: HF 9.5% 2–3 sec. Orthophosphoric ac. 36% 20 sec. Monobond S Tooth: Orthophosphoric ac. 36% (enamel 10 sec., enamel and dentin 5 sec.) Composite cement (dual cure, photopolymerizing cure) |
| Barghi et al. (2002) [57] | Clinical evaluation of etched porcelain onlays: a 4-year report. Compend Contin Educ Dent. | Conventional feldspathic ceramic, sintered | Dual cure composite cement |
| Smales et al. (2004) [58] | Survival of ceramic onlays placed with and without metal reinforcement. J Prosthet Dent. | Conventional feldspathic ceramic, sintered (Mirage) | Dual cure composite cement (Mirage and Ultra-bond) |
| Kaytan et al. (2005) [45] | Clinical evaluation of indirect resin composite and ceramic onlays over a 24-month period. Gen Dent. | Leucite-reinforced ceramic, pressed | Dual cure composite cement |
| Naeselius et al. (2008) [60] | Clinical evaluation of all-ceramic onlays: a 4-year retrospective study. Gen Dent. | Leucite-reinforced ceramic, pressed | Dual cure and photopolymerizing cure composite cement |
| Barnes et al. (2010) [63] | Clinical evaluation of an all-ceramic restorative system: a 36-month clinical evaluation. Am J Dent. | Leucite-reinforced ceramic, pressed (Finesse All-Ceramic) with an ultra-low fusing porcelain (Finesse) | Dual cure composite cements (Esthetic resin cements, Enforce & Calibra) |
| Atali et al. (2011) [64] | IPS Empress onlays luted with two dual-cured resin cements for endodontically treated teeth: a 3-year clinical evaluation. Int J Prosthodont | Leucite-reinforced ceramic, pressed | Dual cure composite cements (Maxcem or Clearfil Esthetic Cement and DC Bond Kit luting systems) |
| Ozyoney et al. (2013) [66] | The efficacy of glass-ceramic onlays in the restoration of morphologically compromised and endodontically treated molars. Int J Prosthodont. | Feldspathic ceramic reinforced with lithium disilicate (IPS Empress II) | Restoration: HF 5% (IPS Empress ceramic etch) Tooth: Orthophosphoric ac. 35% Dentin bonding system: Solobond Plus Primer and Adhesive Dual cure high-viscosity composite cement (Bifix) |
| Baader et al. (2016) [54] | Self-adhesive Luting of Partial Ceramic Crowns: Selective Enamel Etching Leads to Higher Survival after 6.5 Years In Vivo. J Adhes. Dent. | Conventional feldspathic ceramic CAD-CAM (Vita Mark II) | Restoration: HF 5% (HF Vita ceramics etch) Monobond S (silano) Tooth:Orthophosphoric ac. 37% Auto-cure composite cement and auto-cure cement with selective etching (RelyX Unicem) |
| Edelhoff et al. (2019) [7] | Clinical performance of occlusal onlays made of lithium disilicate ceramic in patients with severe tooth wear up to 11 years. Dental Materials. | Feldspathic ceramic reinforced with lithium disilicate (IPS emax Press) | Syntac Total etch & rinse technique, Variolink II Professional Set, low viscosity, light-curing |
| Coskun et al. (2020) [9] | Evaluation of two different CAD-CAM inlay-onlays in a split-mouth study: 2-year clinical follow-up J Esthet Restor Dent. | Feldspathic ceramic reinforced with lithium disilicate (IPS emax CAD)/Hybrid ceramic material (Cerasmart) | Restoration (Cerasmart): Internal surface etched with 5% hydrofluoric acid (IPS Etching gel) 60 sec. Restoration (IPS emax CAD): Internal surface etched with 5% hydrofluoric acid (IPS Etching gel) 20 sec. Rinsed and silanized with Monobond Plus + Unfilled resin (Adhese Universal). Tooth: phosphoric acid gel 37% (Total Etch). Enamel 30 sec./dentin 15 sec. Adhese Universal 20 sec. Resin cement (Variolink Esthetic) |
| Fasbinder et al. (2020) [69] | Clinical evaluation of chairside Computer Assisted Design/Computer Assisted Machining nanoceramic restorations: Five-year status J Esthet Restor Dent. | Leucite reinforced ceramic (IPS Empress CAD)/Hybrid resin nanoceramic material (Lava Ultimate) | Restoration (IPS Empress CAD): 4.9% hydrofluoric acid gel 60 sec. Monobond Plus Scotchbond Universal Adhesive (3M) Restoration (Lava Ultimate): lightly air abraded with 30-μm silica (CoJet Sand; 3M) Scotchbond Universal Adhesive (3M) Tooth (Variolink II cement): phosphoric acid 37% 20 sec. Excite (Ivoclar) dentin bonding agent Tooth (RelyX Ultimate cement): Scotchbond Universal Adhesive Cement Variolink II and RelyX Ultimate |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bustamante-Hernández, N.; Montiel-Company, J.M.; Bellot-Arcís, C.; Mañes-Ferrer, J.F.; Solá-Ruíz, M.F.; Agustín-Panadero, R.; Fernández-Estevan, L. Clinical Behavior of Ceramic, Hybrid and Composite Onlays. A Systematic Review and Meta-Analysis. Int. J. Environ. Res. Public Health 2020, 17, 7582. https://doi.org/10.3390/ijerph17207582
Bustamante-Hernández N, Montiel-Company JM, Bellot-Arcís C, Mañes-Ferrer JF, Solá-Ruíz MF, Agustín-Panadero R, Fernández-Estevan L. Clinical Behavior of Ceramic, Hybrid and Composite Onlays. A Systematic Review and Meta-Analysis. International Journal of Environmental Research and Public Health. 2020; 17(20):7582. https://doi.org/10.3390/ijerph17207582
Chicago/Turabian StyleBustamante-Hernández, Naia, Jose María Montiel-Company, Carlos Bellot-Arcís, José Félix Mañes-Ferrer, María Fernanda Solá-Ruíz, Rubén Agustín-Panadero, and Lucía Fernández-Estevan. 2020. "Clinical Behavior of Ceramic, Hybrid and Composite Onlays. A Systematic Review and Meta-Analysis" International Journal of Environmental Research and Public Health 17, no. 20: 7582. https://doi.org/10.3390/ijerph17207582
APA StyleBustamante-Hernández, N., Montiel-Company, J. M., Bellot-Arcís, C., Mañes-Ferrer, J. F., Solá-Ruíz, M. F., Agustín-Panadero, R., & Fernández-Estevan, L. (2020). Clinical Behavior of Ceramic, Hybrid and Composite Onlays. A Systematic Review and Meta-Analysis. International Journal of Environmental Research and Public Health, 17(20), 7582. https://doi.org/10.3390/ijerph17207582






