Lessons Learned from Battling COVID-19: The Korean Experience
Abstract
1. Introduction
2. Relevant Literature
2.1. Global Infectious Diseases and COVID-19
2.2. Cases of COVID-19 among Healthcare Facilities in Korea
2.2.1. Hospital A
2.2.2. Hospital B
2.2.3. Hospital C
2.2.4. Hospital D
2.2.5. Hospital E
3. Korean’s Innovative Response Strategies to the COVID-19 Pandemic
3.1. Innovative Testing System
3.2. Innovative Approaches to Addressing the Shortage of Healthcare Facilities
3.3. Expansion of “Untact” (Non-Face-to-Face) Services
3.4. Strategies for Pandemic Management
3.4.1. Plans, Procedures, and Control
3.4.2. Governance
3.4.3. Integration of Healthcare Delivery Systems
3.4.4. An Effective Logistics System
3.4.5. Devolution of Control and Execution
4. Lessons Learned from COVID-19
4.1. Government’s Response Capacity
4.2. Information Sharing and Utilization of Digital Devices
4.3. Community and Civic Consciousness
4.4. Innovative Application of Technologies
5. Conclusions
5.1. Implications of the Study Results
5.2. Limitations and Future Research Needs
Author Contributions
Funding
Conflicts of Interest
References
- Cohen, O.; Fox, B.; Mills, N.; Wright, P. COVID-19 and Commercial Pharma: Navigating an Uneven Recovery; McKinsey & Company: New York, NY, USA, 2020. [Google Scholar]
- Sneader, K.; Singhal, S. Beyond Coronavirus: The Path to the Next Normal; McKinsey & Company: New York, NY, USA, 2020. [Google Scholar]
- Cucinotta, D.; Vanelli, M. WHO Declares COVID-19 a Pandemic. Acta Biomed. 2020, 91, 157–160. [Google Scholar]
- Liu, L. Sustainable COVID-19 Mitigation: Wuhan Lockdowns, Health Inequities, and Patient Evacuation. Int. J. Health Policy Manag. 2020, 1–4. [Google Scholar] [CrossRef] [PubMed]
- Shokoohi, M.; Osooli, M.; Stranges, S. COVID-19 pandemic: What can the west learn from the east. Int. J. Health Policy Manag. 2020, 9, 1–3. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization (WHO). Coronavirus. 2020. Available online: https://www.who.int/health-topics/coronavirus#tab=tab_1 (accessed on 10 April 2020).
- OCHA (United Nations Office for the Coordination of Humanitarian Affairs). Global Humanitarian Response Plan (GHRP): COVID-19; OCHA: Geneva, Switzerland, 2020. [Google Scholar]
- Chadha, S.; Ennen, M.; Parekh, R.; Pellumbi, G. Reimagining Medtech for a COVID-19 World; McKinsey & Company: New York, NY, USA, 2020. [Google Scholar]
- World Economic Forum (WEF). Global Risks Report 2020; World Economic Forum: Geneva, Switzerland, 2020. [Google Scholar]
- Bae, J. A Study on Improvement of National Disaster Management System through the MERS Outbreak in Korea. J. Gov. Stud. 2016, 11, 27–54. [Google Scholar]
- Choi, E.; Lee, J. Changes of Global Infectious Disease Governance in 2000s: Rise of Global Health Security and Transformation of Infectious Disease Control System in South Korea. Korean J. Med. Hist. 2016, 25, 489–517. [Google Scholar] [CrossRef] [PubMed]
- Dolan, S.; Raich, M.; Garti, A.; Landau, A. “The COVID-19 Crisis” as an Opportunity for Introspection: A Multi-level rReflection on Values, Needs, Trust and Leadership in the Future. Available online: https://www.europeanbusinessreview.com/the-covid-19-crisis-as-an-opportunity-for-introspection/ (accessed on 10 June 2020).
- Lee, D.; Lee, J. Testing on the Move South Korea’s Rapid Response to the COVID-19 Pandemic. Transportation Research Interdisciplinary Perspectives. 2020. Available online: https://www.sciencedirect.com/science/article/pii/S2590198220300221?via%3Dihub (accessed on 10 May 2020).
- WEF. South Korea’s Foreign Minister Explains How the Country Contained COVID-19. 2020. Available online: https://www.weforum.org/agenda/2020/03/south-korea-covid-19-containment-testing/ (accessed on 10 May 2020).
- Tonby, O.; Woetzel, J.; Kaka, N.; Choi, W.; Seong, J.; Carson, B.; Ma, L. How Technology is Safeguarding Health and Livelihoods in Asia; McKinsey & Company: New York, NY, USA, 2020. [Google Scholar]
- van Houwelingen-Snippe, J.; van Rompay, T.; Allouch, S. Feeling Connected after Experiencing Digital Nature: A Survey Study. Int. J. Environ. Res. Public Health 2020, 17, 6879. [Google Scholar] [CrossRef]
- Lee, S.; Lee, D. “Untact”: A New Customer Service Strategy in the digital age. Serv. Bus. 2020, 14, 1–22. [Google Scholar] [CrossRef]
- Cha, A. Hospitals Consider Universal do-not-Resuscitate Orders for Coronavirus Patients. The Washington Post. 25 March 2020. Available online: https://www.washingtonpost.com/health/2020/03/25/coronavirus-patients-do-not-resucitate/ (accessed on 10 May 2020).
- Errett, N.; Howarth, M.; Shoaf, K.; Couture, M.; Ramsey, S.; Rosselli, R.; Webb, S.; Bennett, A.; Miller, A. Developing an Environmental Health Sciences COVID-19 Research Agenda: Results from the NIEHS Disaster Research Response (DR2) Work Group’s Modified Delphi Method. Int. J. Environ. Res. Public Health 2020, 17, 6842. [Google Scholar] [CrossRef]
- WHO. Infectious Diseases. 2020. Available online: https://www.who.int/topics/infectious_diseases/en/ (accessed on 10 April 2020).
- WHO. What Is a Pandemic? 2010. Available online: https://www.who.int/csr/disease/swineflu/frequently_asked_questions/pandemic/en/ (accessed on 10 April 2020).
- Lederberg, J.; Shope, R., Jr.; Oaks, S. Emerging Infections: Microbial Threats to Health in the United States; National Academies Press: Washington, DC, USA, 1992. [Google Scholar]
- WHO. Global Health Security: Epidemic Alert and Response. 2001. Available online: https://www.who.int/ihr/alert_and_response/outbreak-network/en/ (accessed on 10 April 2020).
- Fidler, D. Germs, Governance, and Global Public Health in the Wake of SARS. J. Clin. Investig. 2004, 113, 799–804. [Google Scholar] [CrossRef]
- Wright, A.; Meyer, A.; Reay, T.; Staggs, J. Maintaining Places of Social Inclusion: Ebola and the Emergency Department. Adm. Sci. Q. 2020. [Google Scholar] [CrossRef]
- Festinger, L. A Theory of Cognitive Dissonance; Stanford University Press: Stanford, CA, USA, 1957. [Google Scholar]
- Rousseau, D. Psychological Contracts in Organizations: Understanding Written and Unwritten Agreements; Sage: Thousand Oaks, CA, USA, 1995. [Google Scholar]
- Adams, J.S. Inequality in Social Exchange. Adv. Exp. Soc. Psychol. 1965, 2, 267–299. [Google Scholar]
- Smith, A.; Bolton, R.; Wagner, J. A Model of Customer Satisfaction with Service Encounters Involving Failure and rRecovery. J. Mark. Res. 1999, 36, 356–372. [Google Scholar] [CrossRef]
- Tax, S.; Brown, S.; Chandrashekaran, M. Customer Evaluations of Service Complaint Experiences: Implications for Relationship Marketing. J. Mark. 1998, 62, 60–76. [Google Scholar] [CrossRef]
- Jang, B. A study on the National Crisis Management System in the Case of the New Infection Diseases: Focusing on School Infection Prevention Activities. Korean Political Sci. Assoc. 2017, 25, 69–89. [Google Scholar] [CrossRef]
- Korea Centers for Disease Control and Prevention (KCDC). Available online: https://www.cdc.go.kr/board/board.es?mid=a30402000000&bid=0030 (accessed on 10 April 2020).
- The Korea Economic Daily. Daegu, the Initial Response was Fast. It Was Different from New York, Bergamo. 2020. Available online: https://www.hankyung.com/society/article/202004021243i (accessed on 10 May 2020).
- Campbell, C. South Korea’s Health Minister on How His Country is Beating Coronavirus without a Lockdown. Time. 2020. Available online: https://time.com/5830594/south-korea-covid19-coronavirus/ (accessed on 30 April 2020).
- Daegu Operated a Public-Private Partnership Network. Available online: https://daegucidcp.kr/main/ (accessed on 30 April 2020).
- Kwon, K.; Ko, J.; Shin, H.; Sung, M.; Kim, J. Drive-through Screening Center for COVID-19: A Safe and Efficient Screening System against Massive Community Outbreak. J. Korean Med. Sci. 2020, 35, e123. [Google Scholar] [CrossRef]
- MBN News. Corona 19 ‘Drive through’ Topic… ‘Wonderful Idea… Innovation’. 2020. Available online: https://www.mbn.co.kr/news/society/4071136 (accessed on 10 May 2020).
- COVID-19 Pandemic Data Sources. Available online: https://coronavirus.jhu.edu/ (accessed on 3 June 2020).
- COVID-19 Pandemic in Mainland China. Available online: https://en.wikipedia.org/wiki/COVID-19_pandemic_in_mainland_China (accessed on 3 June 2020).
- COVID-19 Pandemic in Italy. Available online: https://en.wikipedia.org/wiki/2020_coronavirus_pandemic_in_Italy (accessed on 3 June 2020).
- COVID-19 Pandemic in Spain. Available online: https://en.wikipedia.org/wiki/2020_coronavirus_pandemic_in_Spain (accessed on 3 June 2020).
- COVID-19 Pandemic in South Korea. Available online: https://en.wikipedia.org/wiki/2020_coronavirus_pandemic_in_South_Korea (accessed on 3 June 2020).
- COVID-19 Pandemic in the United States. Available online: https://en.wikipedia.org/wiki/2020_coronavirus_pandemic_in_the_United_States (accessed on 3 June 2020).
- Terhune, C.; Levine, D.; Jin, H.; Lee, J. Special Report: How Korea Trounced U.S. in Race to Test People for Coronavirus. Reuter, 2020. Available online: https://www.reuters.com/article/us-health-coronavirus-testing-specialrep/special-report-how-korea-trounced-u-s-in-race-to-test-people-for-coronavirus-idUSKBN2153BW (accessed on 10 May 2020).
- COVID-19 Pandemic Data Sources. Available online: https://coronavirus.jhu.edu/data/mortality (accessed on 7 September 2020).
- Lee, D.; Lee, D. Healthcare Service Justice and Community Engagement in Crisis Situation: Focusing on Failure Cases in Response to COVID-19. J. Korea Serv. Manag. Soc. 2020, 21, 293–312. [Google Scholar] [CrossRef]
- Davis, Z.; Zobel, C.; Khansa, L.; Glick, R. Emergency Department Resilience to Disaster-level Overcrowding: A Component Resilience Framework for Analysis and Predictive Modeling. J. Oper. Manag. 2020, 66, 54–66. [Google Scholar] [CrossRef]
- Kuhn, A. South Korea’s Drive-through Testing for Coronavirus is Fast—and Free. National Public Radio. 2020. Available online: https://www.npr.org/sections/goatsandsoda/2020/03/13/815441078/south-koreas-drive-through-testing-for-coronavirus-is-fast-and-free (accessed on 10 April 2020).
- Yamey, G. What the U.S. Needs to do Today to Follow South Korea’s Model for Fighting Coronavirus Time. 2020. Available online: https://time.com/5804899/u-s-coronavirus-needs-follow-s-korea/ (accessed on 20 April 2020).
- Weekly Dong-A. COVID-19: Community Treatment Center. Weekly Dong-A 2020, 1230, 18–19. Available online: https://weekly.donga.com/3/search/11/2001829/1 (accessed on 10 May 2020).
- Durante, R.; Guiso, L.; Gulino, G. Civic Capital and Social Distancing: Evidence from Italians’ Response to COVID-19. Vox CEPR Policy Portal. 2020. Available online: https://voxeu.org/article/civic-capital-and-social-distancing (accessed on 10 May 2020).
- Kim, K. Uncertainties of International Standards in the Mers CoV Outbreak in Korea: Multiplicity of Uncertainties. Korean Assoc. Environ. Soc. 2016, 20, 317–351. [Google Scholar]
- Lee, K.; Jung, K. Factors Influencing the Response to Infectious Diseases: Focusing on the Case of SARS and MERS in South Korea. Int. J. Environ. Res. Public Health 2019, 16, 1432. [Google Scholar] [CrossRef] [PubMed]
- Woodward, A. South Korea Controlled Its Coronavirus Outbreak in Just 20 Days. Here are the Highlights from Its 90-Page Playbook for Flattening the Curve. Business Insider. 2020. Available online: https://www.businessinsider.com/how-south-korea-controlled-its-coronavirus-outbreak-2020-4 (accessed on 10 May 2020).
- New York Times. Worldwide Confirmed Coronavirus Cases Top 2 Million. 2020. Available online: https://www.nytimes.com/2020/04/15/world/coronavirus-cases-world.html (accessed on 10 May 2020).
- Johnson, C.; McGinley, L.; Sun, L. A Faulty CDC Coronavirus Test Delays Monitoring of Disease’s Spread. The Philadelphia Inquirer. 2020. Available online: https://www.inquirer.com/health/coronavirus-test-problems-us-diagnosis-outbreak-20200225.html (accessed on 10 May 2020).
- Health Korea News. Korean Government’s Response to Corona 19. 2020. Available online: https://engnews24h.com/korean-governments-response-to-corona19/ (accessed on 10 May 2020).
- Greiner, A.; Angelo, K.; McCollum, A.; Mirkovic, K.; Arthur, R.; Angulo, F. Addressing Contact Tracing Challenges-Critical to Halting Ebola Virus Disease Transmission. Int. J. Infect. Dis. 2015, 41, 53–55. [Google Scholar] [CrossRef] [PubMed]
- Huang, Y. Implications of SARS Epidemic for China’s Public Health Infrastructure and Political System. Available online: https://www.cecc.gov/sites/chinacommission.house.gov/files/documents/roundtables/2003/CECC%20Roundtable%20Testimony%20-%20Yanzhong%20Huang%20-%205.12.03.pdf (accessed on 16 October 2020).
- Ferretti, L.; Wymant, C.; Kendall, M.; Zhao, L.; Nurtay, A.; Abeler-Dörner, L.; Parker, M.; Bonsall, D.; Fraser, C. Quantifying SARS-CoV-2 Transmission Suggests Epidemic Control with Digital Contact Tracing. Science 2020. [Google Scholar] [CrossRef] [PubMed]
- The Washington Post. South Korea Shows that Democracies Can Succeed against the Coronavirus. 2020. Available online: https://www.washingtonpost.com/opinions/2020/03/11/south-korea-shows-that-democracies-can-succeed-against-coronavirus/ (accessed on 10 May 2020).
- BBC NEWS. Coronavirus: What could the West Learn from Asia? 2020. Available online: https://www.bbc.com/news/world-asia-51970379 (accessed on 10 May 2020).
- Fendos, J. Lessons from South Korea’s COVID-19 Outbreak: The Good, Bad, and Ugly. The Diplomat. 2020. Available online: https://thediplomat.com/2020/03/lessons-from-south-koreas-covid-19-outbreak-the-good-bad-and-ugly/ (accessed on 10 May 2020).
- Ahmed, F.; Zviedrite, N.; Uzicanin, A. Effectiveness of Workplace Social Distancing Measures in Reducing Influenza Transmission. BMC Public Health 2018, 18, 518. [Google Scholar] [CrossRef] [PubMed]
- Yonhap News. Drive-Thrus Booming in Korean Society amid Virus Scare. 2020. Available online: https://en.yna.co.kr/view/AEN20200320007100315 (accessed on 20 April 2020).
- Diebner, R.; Silliman, E.; Ungerman, K.; Vancauwenberghe, M. Adapting Customer Experience in the Time of Coronavirus; McKinsey & Company: New York, NY, USA, 2020. [Google Scholar]
- Kennedy, J.F. John F. Kennedy Quotations; John F. Kennedy Presidential Residential; Library and Museum: Boston, MA, USA, 1962. [Google Scholar]
- BrainyQuote.com. Winston Churchill Quotes. 2020. Available online: https://www.brainyquote.com/quotes/winston_churchill_156899 (accessed on 21 April 2020).
| Major City (Country) | Number of Confirmed Cases | Number of Deaths | Mortality Rate | Response Strategies Implemented by Daegu to Deal with the Pandemic |
|---|---|---|---|---|
| Worldwide | 6,263,632 | 375,542 | 6.00% |
|
| New York (US): From 20 Jan. 2020 | 373,040 (1,811,360) | 24,023 (105,165) | 6.44% (5.81%) | |
| Madrid (Spain): From 31 Jan. 2020 | 68,852 (239,638) | 8691 (27,127) | 12.62% (11.32%) | |
| Lombardy (Italy): From 31 Jan. 2020 | 89,205 (233,197) | 16,143 (33,475) | 18.10% (14.35%) | |
| Hubei (China): From 31 Dec. 2019 | 68,135 (84,154) | 4512 (4638) | 6.62% (5.51%) | |
| Daegu (Korea): From 20 Jan. 2020 | 6885 (11,541) | 188 (272) | 2.76% (2.36%) |
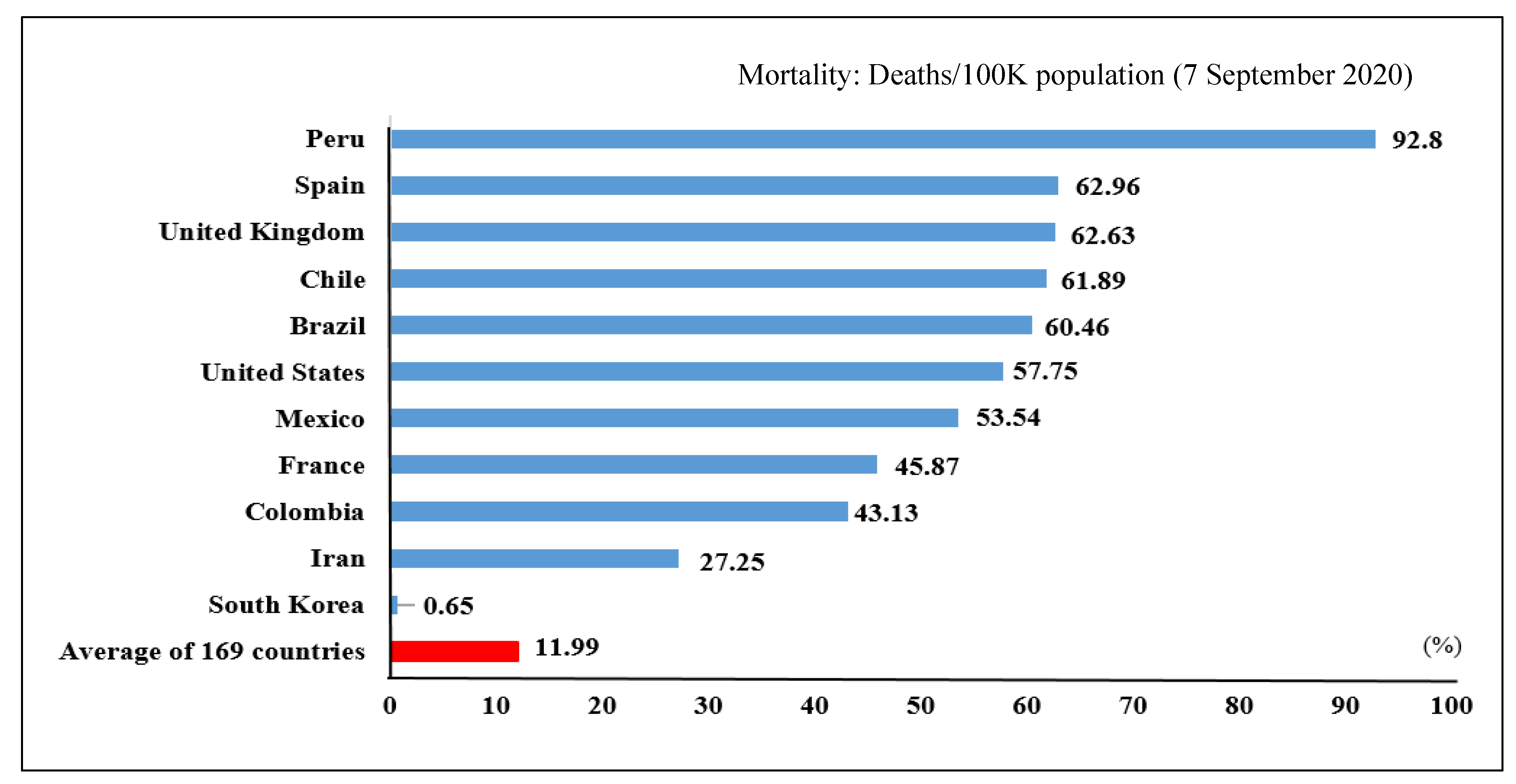
| Ranking Based on Confirmed Cases | Country | Confirmed Case | Deaths | Death/Case | Mortality: Deaths/100k Population |
|---|---|---|---|---|---|
| 1 | United States | 6,276,365 | 188,941 | 3.00% | 57.75 |
| 2 | India | 4,204,613 | 71,642 | 1.70% | 5.30 |
| 3 | Brazil | 4,137,521 | 126,650 | 3.10% | 60.46 |
| 4 | Russia | 1,022,228 | 17,768 | 1.70% | 12.30 |
| 5 | Peru | 683,702 | 29,687 | 4.30% | 92.80 |
| 6 | Colombia | 666,521 | 21,412 | 3.20% | 43.13 |
| 7 | South Africa | 638,517 | 14,889 | 2.30% | 25.77 |
| 8 | Mexico | 634,023 | 67,558 | 10.70% | 53.54 |
| 9 | Spain | 498,989 | 29,418 | 5.90% | 62.96 |
| 10 | Argentina | 478,792 | 9859 | 2.10% | 22.16 |
| 11 | Chile | 422,510 | 11,592 | 2.70% | 61.89 |
| 12 | Iran | 386,658 | 22,293 | 5.80% | 27.25 |
| 13 | United Kingdom | 349,500 | 41,640 | 11.90% | 62.63 |
| 14 | France | 347,268 | 30,730 | 8.80% | 45.87 |
| 15 | Bangladesh | 325,157 | 4479 | 1.40% | 2.78 |
| 16 | Saudi Arabia | 320,688 | 4081 | 1.30% | 12.11 |
| 17 | Pakistan | 298,903 | 6345 | 2.10% | 2.99 |
| 19 | Italy | 277,634 | 35,541 | 12.80% | 58.81 |
| 35 | China | 90,058 | 4730 | 5.30% | 0.34 |
| 75 | South Korea | 21,296 | 336 | 1.60% | 0.65 |
| Average of 169 countries | 160,365 | 5227 | 2.91% | 11.99 | |
| Case | Cause | Response | Lesson |
|---|---|---|---|
| Hospital A | Noncompliance with regulation by a patient aid |
|
|
| Hospital B | False statement by a patient |
|
|
| Hospital C | Blithe response |
|
|
| Hospital D | Secondary mass infection following initial patient infection |
|
|
| Hospital E | Implemented proactive measures |
|
|
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lee, S.M.; Lee, D. Lessons Learned from Battling COVID-19: The Korean Experience. Int. J. Environ. Res. Public Health 2020, 17, 7548. https://doi.org/10.3390/ijerph17207548
Lee SM, Lee D. Lessons Learned from Battling COVID-19: The Korean Experience. International Journal of Environmental Research and Public Health. 2020; 17(20):7548. https://doi.org/10.3390/ijerph17207548
Chicago/Turabian StyleLee, Sang M., and DonHee Lee. 2020. "Lessons Learned from Battling COVID-19: The Korean Experience" International Journal of Environmental Research and Public Health 17, no. 20: 7548. https://doi.org/10.3390/ijerph17207548
APA StyleLee, S. M., & Lee, D. (2020). Lessons Learned from Battling COVID-19: The Korean Experience. International Journal of Environmental Research and Public Health, 17(20), 7548. https://doi.org/10.3390/ijerph17207548





