The Promotion of Eating Behaviour Change through Digital Interventions
Abstract
1. Introduction
1.1. Changing Eating Behaviour
1.2. Digital Behaviour Change Interventions
1.3. Rationales behind the Study
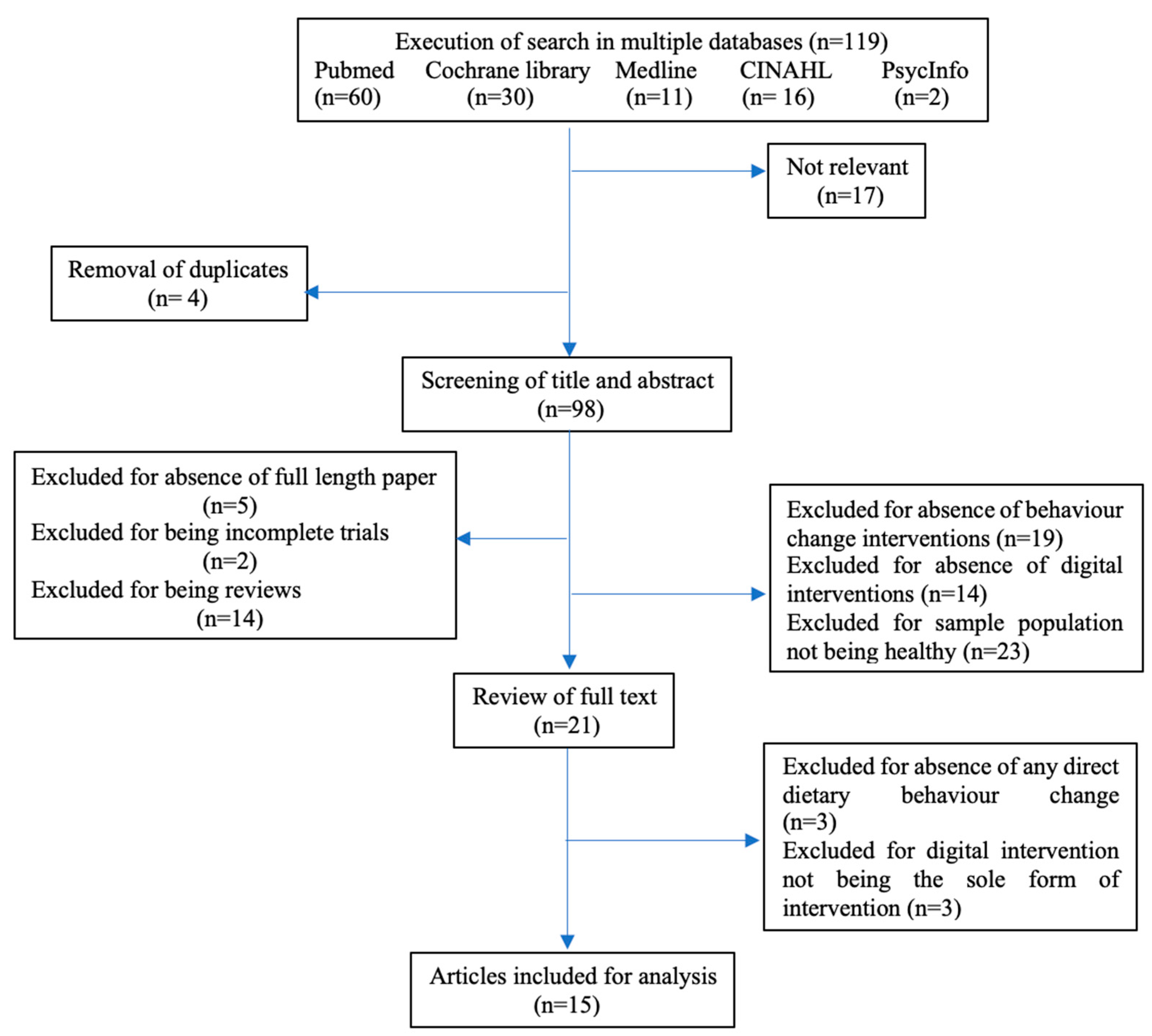
2. Materials and Methods
2.1. Search Strategy
2.2. Inclusion and Exclusion Criteria
2.3. Data Extraction and Analysis
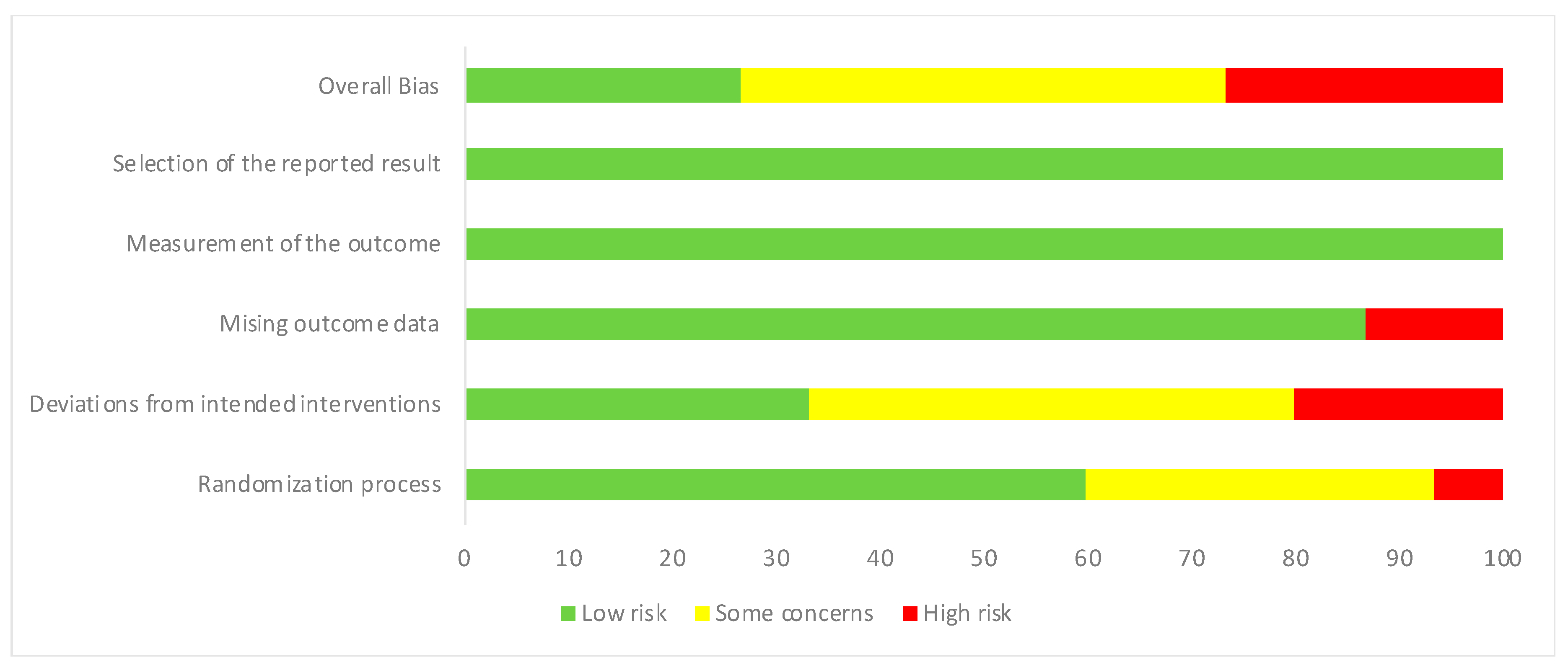
2.4. Quality Assessment
| Author, Year | Target Population | Intervention Type | Eating Behaviour Change | Effect Size |
|---|---|---|---|---|
| Personal Digital Assistant (PDA) as intervention | ||||
| Acharya et al., 2011 [48] | 192 people with a mean age of 49 years and BMI of 34.0 kg/m2 | Self-monitoring PDA | Increased consumption of fruits, vegetables and decreased intake of refined grains | Effect size for fat intake was 0.25; for fruit servings 0.36; vegetable servings 0.32; whole grain servings 0.1 and refined grain servings 0.2 |
| Ambeba et al., 2015 [49] | 210 overweight adults (BMI ≥ 34.0 kg/m2) | Daily tailored feedback on diet intake using a PDA | Significant improvements in intake of fats and carbohydrates | Effect size calculated between groups receiving feedback versus not receiving feedback (i) 0.32 for reduction of fat intake (ii) 0.34 for reduction of energy intake |
| Burke et al., 2010 [50] | Healthy adults (18–59 years of age) with a BMI between 27 and 43 kg/m2 | Self-monitoring diet and exercise using a PDA with or without feedback | Higher proportion of the group using PDA and feedback had a significant weight loss (5%) after 6 months by monitoring calorie intake in their diets | An effect size of 0.3 in change in total fat intake was observed between the paper record group and group using PDA + feedback |
| Atienza et al., 2008 [51] | 27 healthy adults aged ≥ 50 years | PDA monitoring their daily diet, providing feedback and answering questions | Target population reported higher intake of vegetables and dietary fibre in their daily diet | Effect size of 0.9 for vegetable serving and 0.7 for dietary fibre intake was calculated |
| Olson et al., 2008 [52] | Adolescents visiting 5 rural primary care practices in the USA | PDA-mediated questionnaires, health behaviour assessments and counselling | Increased intake of milk | Effect size of change in milk intake between the PDA group and non-PDA group was 0.365 |
| Online education as intervention | ||||
| Schwarzer et al., 2017 #1 [53] | 454 adults (18–65 years of age) | Online platform delivering a lifestyle intervention following Mediterranean diet | Overall improvements in Mediterranean diet | Various effect sizes on dietary behaviour were observed; R2 = 0.14 for positive outcome expectancies; R2 = 0.12 for dietary action control; R2 = 0.13 for dietary planning and R2 = 0.17 for stages of changes |
| Kattelmann et al., 2014 [54] | 1639 college students | 10-week intensive intervention focussing on eating behaviour, physical activity, stress management via e-mail and the internet | Small changes were observed in fat intake and inclusion of fruits and vegetables in the diet | Effect size of fruit and vegetable consumption between control and experimental group was 0.05 |
| O’Donnell et al., 2014 [55] | Students from 8 participating institutions in the USA (18–24 years of age), BMI ≥ 18.5 | 10 online lessons with feedback, facts and interactive questions | Setting of goals increased intake of fruits and vegetables by the participants | Effect size of fruit intake before goal setting and after 10 weeks of goal setting is η2 = 0.09 |
| Grimes et al., 2018 [56] | Child–parent dyads from 5 government schools in Australia | 5-week intervention programme delivered weekly via an online education programme to reduce salt intake | Increased knowledge, self-efficacy and behaviours related to salt in children but no reduction in salt intake was observed | An effect size of 1.08 was reported in change in dietary behaviour pre- and post-intervention |
| Video games as intervention | ||||
| Zurita-Ortega et al., 2018 [57] | 47 university students, average age 22.53 years | 12-week intervention by active video and motor games | Quality of diet was improved | Effect size of diet change post intervention versus pre-intervention was 0.68. |
| Shiyko et al., 2016 [58] | 47 healthy, highly educated women, average age 29.8 years, average BMI 26.98 | Computer game called Spaplay with real world play patterns and linked to real-life activities like healthy snacking | 60% of participants were contemplating, 34% were preparing to and 4% demonstrated nutritional behaviour change | Effect size of nutritional knowledge gain was 0.86 |
| Smart phone applications (apps) as intervention | ||||
| Duncan et al., 2014 [59] | 301 adult male participants age 35–54 years | IT based 9 month intervention called ManUp influencing dietary behaviour and physical activity | Increased intake of high fibre bread and low-fat milk | Effect size was 0.07 for low fat milk intake and 0.2 for high fibre bread intake |
| Ipjian and Johnston, 2017 #2 [60] | 30 healthy adults, average age 34.4 + 15.7 years, average BMI 25.3 + 4.3 kg/m2 | App called MyFitnessPal aiding in reduced sodium intake | Those using the app reported lower urinary sodium levels | Effect size for the study was reported as η2 = 0.234 |
| Mummah et al., 2017 #3 [61] | 135 overweight adults 18–50 years of age, BMI 28–40 kg/m2 | Vegethon mobile app enabling setting goals, self-monitoring and feedback | Significant increase in daily vegetable consumption in the intervention group | Effect size Cohen’s d = 0.18 for primary outcome measures after the 8-week trial and d = 0.2 for 24 h recalls |
| Wharton et al., 2014 [62] | 57 healthy adults 18–65 years of age, BMI 25–40 kg/m2 | Use of ‘LoseIt!’ diet tracking app | Weight loss was similar across groups using the app, memos or papers; healthy eating habit values decreased for app users; more app users completed the trial | Effect size of healthy eating index was 0.089 |
3. Results
3.1. PDA
3.2. Online Education
3.3. Video Games
3.4. Smartphone Apps
3.5. Study Quality Assessment
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- 2015–2020 Dietary Guidelines for Americans. Available online: https://health.gov/our-work/food-nutrition/2015-2020-dietary-guidelines/guidelines/ (accessed on 13 March 2020).
- Myplate.gov. Available online: https://www.choosemyplate.gov/MyPlate (accessed on 13 March 2020).
- CDC Nutrition Facts. Available online: https://www.cdc.gov/healthyschools/nutrition/facts.htm (accessed on 13 April 2020).
- Lee, J.; Herman, W.; McPheeters, M.; Gurney, J. An Epidemiologic Profile of Children with Diabetes in the U.S. Diabetes Care 2006, 29, 420–421. [Google Scholar] [CrossRef][Green Version]
- Gable, S.; Krull, J.; Chang, Y. Implications of Overweight Onset and Persistence for Social and Behavioral Development between Kindergarten Entry and Third Grade. Appl. Dev. Sci. 2009, 13, 88–103. [Google Scholar] [CrossRef]
- Observatory, N.O. Obesity and Mental Health. Available online: https://khub.net/documents/31798783/32039025/Obesity+and+Mental+Health.pdf/18cd2173-408a-4322-b577-6aba3354b7ca?download=true (accessed on 13 October 2020).
- Fontaine, K.R.; Redden, D.T.; Wang, C.; Westfall, A.O.; Allison, D.B. Years of Life Lost Due to Obesity. JAMA J. Am. Med Assoc. 2003, 289, 187–193. [Google Scholar] [CrossRef]
- Simmonds, M.; Burch, J.; Llewellyn, A.; Griffiths, C.; Yang, H.; Owen, C.; Duffy, S.; Woolacott, N. The use of measures of obesity in childhood for predicting obesity and the development of obesity-related diseases in adulthood: A systematic review and meta-analysis. Health Technol. Assess. 2015, 19, 1–336. [Google Scholar] [CrossRef]
- Digital, N. Statistics on Obesity, Physical Activity and Diet. England 2018. Available online: https://files.digital.nhs.uk/publication/0/0/obes-phys-acti-diet-eng-2018-rep.pdf (accessed on 13 March 2020).
- OECD Healthier Lifestyles and Better Health Policies Drive Life Expectancy Gains. Available online: http://www.oecd.org/newsroom/healthier-lifestyles-and-better-health-policies-drive-life-expectancy-gains.htm (accessed on 13 April 2020).
- Centre, H. National Child Measurement Programme: England 2013/14; Public Health England Wellington House: London, UK, 2014. [Google Scholar]
- Contento, I.; Balch, G.; Bronner, Y.; Lytle, L.; Maloney, S.K.; Olson, C.; Swadener, S. The Effectiveness of Nutrition Education and Implications for Nutrition Education Policy, Programs, and Research: A Review of Research; SAGE: Thousand Oaks, CA, USA, 1995; pp. 277–418. [Google Scholar]
- Baranowski, T.; Lin, L.S.; Wetter, D.W.; Resnicow, K.; Hearn, M.D. Theory as mediating variables: Why aren’t community interventions working as desired? Ann. Epidemiol. 1997, 7, S89–S95. [Google Scholar] [CrossRef]
- Baranowski, T.; Davis, M.; Resnicow, K.; Baranowski, J.; Doyle, C.; Lin, L.S.; Smith, M.; Wang, D.T. Gimme 5 Fruit, Juice, and Vegetables for Fun and Health: Outcome Evaluation. Health Educ. Behav. 2016, 27, 96–111. [Google Scholar] [CrossRef]
- Hearn, M.D.; Baranowski, T.; Baranowski, J.; Doyle, C.; Smith, M.; Lin, L.S.; Resnicow, K. Environmental Influences on Dietary Behavior among Children: Availability and Accessibility of Fruits and Vegetables Enable Consumption. J. Health Educ. 1998, 29, 26–32. [Google Scholar] [CrossRef]
- Cullen, K.W.; Baranowski, T.; Owens, E.; Marsh, T.; Rittenberry, L.; de Moor, C. Availability, Accessibility, and Preferences for Fruit, 100% Fruit Juice, and Vegetables Influence Children’s Dietary Behavior. Health Educ. Behav. 2003, 30, 615–626. [Google Scholar] [CrossRef] [PubMed]
- Kirby, S.D.; Baranowski, T.; Reynolds, K.D.; Taylor, G.; Binkley, D. Children’s fruit and vegetable intake: Socioeconomic, adult-child, regional, and urban-rural influences. J. Nutr. Educ. 1995, 27, 261–271. [Google Scholar] [CrossRef]
- Fox, S.; Duggan, M. Mobile Health 2012. Pew Internet & American Life Project. Available online: http://www.pewinternet.org/2012/11/08/mobile-health-2012/ (accessed on 13 April 2020).
- Kontos, E.; Blake, K.D.; Chou, W.-Y.S.; Prestin, A. Predictors of eHealth Usage: Insights on The Digital Divide from the Health Information National Trends Survey 2012. J. Med. Internet Res. 2014, 16, e172. [Google Scholar] [CrossRef]
- Health, R. Digital Health Consumer Adoption: 2015. Available online: http://rockhealth.com/reports/digital-health-consumer-adoption-2015/ (accessed on 13 March 2020).
- West, R.; Michie, S. A Guide to Development and Evaluation of Digital Interventions in Healthcare; Silverback Publishing: London, UK, 2016. [Google Scholar]
- Perski, O.; Blandford, A.; West, R.; Michie, S. Conceptualising engagement with digital behaviour change interventions: A systematic review using principles from critical interpretive synthesis. Transl. Behav. Med. 2016, 7, 254–267. [Google Scholar] [CrossRef]
- Liu, F.; Kong, X.; Cao, J.; Chen, S.; Li, C.; Huang, J.; Gu, D.; Kelly, T.N. Mobile phone intervention and weight loss among overweight and obese adults: A meta-analysis of randomized controlled trials. Am. J. Epidemiol. 2015, 181, 337–348. [Google Scholar] [CrossRef] [PubMed]
- Whittaker, R.; Borland, R.; Bullen, C.; Lin, R.B.; McRobbie, H.; Rodgers, A. Mobile phone-based interventions for smoking cessation. Cochrane Database Syst. Rev. 2009, 4, CD006611. [Google Scholar]
- Civljak, M.; Stead, L.F.; Hartmann-Boyce, J.; Sheikh, A.; Car, J. Internet-based interventions for smoking cessation. Cochrane Database Syst. Rev. 2013, 7, CD007078. [Google Scholar]
- Muntaner, A.; Vidal-Conti, J.; Palou, P. Increasing physical activity through mobile device interventions: A systematic review. Health Inform. J. 2016, 22, 451–469. [Google Scholar] [CrossRef]
- Natasha, K.N.; Nicola, C.N.; Anthony, S.; Paul, W.; Maree, T. A Systematic Review of Digital and Computer-Based Alcohol Intervention Programs in Primary Care. Curr. Drug Abus. Rev. 2015, 8, 111–118. [Google Scholar]
- Jones, K.R.; Lekhak, N.; Kaewluang, N. Using Mobile Phones and Short Message Service to Deliver Self-Management Interventions for Chronic Conditions: A Meta-Review. Worldviews Evid. Based Nurs. 2014, 11, 81–88. [Google Scholar] [CrossRef] [PubMed]
- Donkin, L.; Christensen, H.; Naismith, S.L.; Neal, B.; Hickie, I.B.; Glozier, N. A Systematic Review of the Impact of Adherence on the Effectiveness of e-Therapies. J. Med. Internet Res. 2011, 13, e52. [Google Scholar] [CrossRef]
- Webb, T.L.; Joseph, J.; Yardley, L.; Michie, S. Using the Internet to Promote Health Behavior Change: A Systematic Review and Meta-analysis of the Impact of Theoretical Basis, Use of Behavior Change Techniques, and Mode of Delivery on Efficacy. J. Med. Internet Res. 2010, 12, e4. [Google Scholar] [CrossRef] [PubMed]
- Wantland, D.J.; Portillo, C.J.; Holzemer, W.L.; Slaughter, R.; McGhee, E.M. The Effectiveness of Web-Based vs. Non-Web-Based Interventions: A Meta-Analysis of Behavioral Change Outcomes-0. J. Med. Internet Res. 2011, 10, e40. [Google Scholar] [CrossRef]
- Cugelman, B. Why Digital Behaviour Change Interventions will Transform Public Health. Available online: http://www.ohpe.ca/node/13291 (accessed on 13 March 2020).
- WHO Obesity and Overweight. Available online: http://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight (accessed on 13 March 2020).
- Wang, Y.C.M.D.; McPherson, K.P.; Marsh, T.P.G.D.; Gortmaker, S.L.P.; Brown, M.P. Health and economic burden of the projected obesity trends in the USA and the UK. Lancet 2011, 378, 815–825. [Google Scholar] [CrossRef]
- Brown, K.F.; Rumgay, H.; Dunlop, C.; Ryan, M.; Quartly, F.; Cox, A.; Deas, A.; Elliss-Brookes, L.; Gavin, A.; Hounsome, L.; et al. The fraction of cancer attributable to modifiable risk factors in England, Wales, Scotland, Northern Ireland, and the United Kingdom in 2015. Br. J. Cancer 2018, 118, 1130–1141. [Google Scholar] [CrossRef]
- Jebb, S.A.; Kopelman, P.; Butland, B. Executive Summary: FORESIGHT ‘Tackling Obesities: Future Choices’ project. Obes. Rev. 2007, 8, vi–ix. [Google Scholar] [CrossRef]
- Karnik, S.; Kanekar, A. Childhood obesity: A global public health crisis. Int. J. Prev. Med. 2012, 3, 1–7. [Google Scholar]
- Ebbeling, C.; Pawlak, D.B.; Ludwig, D. Childhood obesity: Public-health crisis, common sense cure. Lancet 2002, 360, 473–482. [Google Scholar] [CrossRef]
- WHO Children’s Environmental Health: Emerging Issues. Available online: http://www.who.int/ceh/risks/cehmobility/en/ (accessed on 13 March 2020).
- Popkin, B.M.; Adair, L.S.; Ng, S.W. Global nutrition transition and the pandemic of obesity in developing countries. Nutr. Rev. 2012, 70, 3–21. [Google Scholar] [CrossRef] [PubMed]
- Gupta, N.; Goel, K.; Shah, P.; Misra, A. Childhood Obesity in Developing Countries: Epidemiology, Determinants, and Prevention. Endocr. Rev. 2012, 33, 48–70. [Google Scholar] [CrossRef]
- National Consumer Council (UK). It’s Our Health! Realising the Potential of Effective Social Marketing; National Consumer Council: London, UK, 2006; p. 45. [Google Scholar]
- Snyder, L.B. Health Communication Campaigns and Their Impact on Behavior. J. Nutr. Educ. Behav. 2007, 39, S32–S40. [Google Scholar] [CrossRef]
- Cugelman, B.; Thelwall, M.; Dawes, P. Online Interventions for Social Marketing Health Behavior Change Campaigns: A Meta-Analysis of Psychological Architectures and Adherence Factors. J. Med. Internet Res. 2011, 13, e17. [Google Scholar] [CrossRef]
- Strecher, V.J.; Shiffman, S.; West, R. Randomized controlled trial of a web-based computer-tailored smoking cessation program as a supplement to nicotine patch therapy. Addiction 2005, 100, 682–688. [Google Scholar] [CrossRef]
- Lipsey, M.; Wilson, D. Practical Meta-Analysis; SAGE: Thousand Oaks, CA, USA, 2000. [Google Scholar]
- Sterne, J.A.C.; Savović, J.; Page, M.J.; Elbers, R.G.; Blencowe, N.S.; Boutron, I.; Cates, C.J.; Cheng, H.-Y.; Corbett, M.S.; Eldridge, S.M.; et al. RoB 2: A revised tool for assessing risk of bias in randomised trials. BMJ 2019, 366, l4898. [Google Scholar] [CrossRef] [PubMed]
- Acharya, S.D.M.S.; Elci, O.U.P.; Sereika, S.M.P.; Styn, M.A.P.; Burke, L.E. Using a Personal Digital Assistant for Self-Monitoring Influences Diet Quality in Comparison to a Standard Paper Record among Overweight/Obese Adults. J. Am. Diet. Assoc. 2011, 111, 583–588. [Google Scholar] [CrossRef] [PubMed]
- Ambeba, E.J.; Ye, L.; Sereika, S.M.; Styn, M.A.; Acharya, S.D.; Sevick, M.A.; Ewing, L.J.; Conroy, M.B.; Glanz, K.; Zheng, Y.; et al. The Use of mHealth to Deliver Tailored Messages Reduces Reported Energy and Fat Intake. J. Cardiovasc. Nurs. 2015, 30, 35–43. [Google Scholar] [CrossRef]
- Burke, L.E.; Conroy, M.B.; Sereika, S.M.; Elci, O.U.; Styn, M.A.; Acharya, S.D.; Sevick, M.A.; Ewing, L.J.; Glanz, K. The Effect of Electronic Self-Monitoring on Weight Loss and Dietary Intake: A Randomized Behavioral Weight Loss Trial. Obesity 2010, 19, 338–344. [Google Scholar] [CrossRef]
- Atienza, A.A.; King, A.C.; Oliveira, B.M.; Ahn, D.K.; Gardner, C.D. Using Hand-Held Computer Technologies to Improve Dietary Intake. Am. J. Prev. Med. 2008, 34, 514–518. [Google Scholar] [CrossRef] [PubMed]
- Olson, A.L.; Gaffney, C.A.; Lee, P.W.; Starr, P. Changing adolescent health behaviors: The healthy teens counseling approach. Am. J. Prev. Med. 2008, 35, S359. [Google Scholar] [CrossRef] [PubMed]
- Schwarzer, R.; Fleig, L.; Warner, L.M.; Gholami, M.; Serra-Majem, L.; Ngo, J.; Roman-Viñas, B.; Ribas-Barba, L.; Distante, A.; Ntzani, E.; et al. Who benefits from a dietary online intervention? Evidence from Italy, Spain and Greece. Public Health Nutr. 2017, 20, 938–947. [Google Scholar] [CrossRef]
- Kattelmann, K.K.; Bredbenner, C.B.; White, A.A.; Greene, G.W.; Hoerr, S.L.; Kidd, T.; Colby, S.; Horacek, T.M.; Phillips, B.W.; Koenings, M.M.; et al. The Effects of Young Adults Eating and Active for Health (YEAH): A Theory-Based Web-Delivered Intervention. J. Nutr. Educ. Behav. 2014, 46, S27–S41. [Google Scholar] [CrossRef]
- O’Donnell, S.; Greene, G.W.; Blissmer, B. The Effect of Goal Setting on Fruit and Vegetable Consumption and Physical Activity Level in a Web-Based Intervention. J. Nutr. Educ. Behav. 2014, 46, 570–575. [Google Scholar] [CrossRef]
- Grimes, C.A.; Booth, A.; Khokhar, D.; West, M.; Margerison, C.; Campbell, K.J.; Nowson, C.A. Digital Education to Limit Salt in the Home (DELISH) Program Improves Knowledge, Self-Efficacy, and Behaviors Among Children. J. Nutr. Educ. Behav. 2018, 50, 547–554. [Google Scholar] [CrossRef]
- Zurita-Ortega, F.; Chacón-Cuberos, R.; Castro-Sánchez, M.; Gutiérrez-Vela, F.L.; González-Valero, G. Effect of an Intervention Program Based on Active Video Games and Motor Games on Health Indicators in University Students: A Pilot Study. Int. J. Environ. Res. Public Health 2018, 15, 1329. [Google Scholar] [CrossRef] [PubMed]
- Shiyko, M.; Hallinan, S.; Seif El-Nasr, M.; Subramanian, S.; Castaneda-Sceppa, C. Effects of Playing a Serious Computer Game on Body Mass Index and Nutrition Knowledge in Women. JMIR Serious Games 2016, 4, e8. [Google Scholar] [CrossRef] [PubMed]
- Duncan, M.; Vandelanotte, C.; Kolt, G.S.; Rosenkranz, R.R.; Caperchione, C.M.; George, E.S.; Ding, H.; Hooker, C.; Karunanithi, M.; Maeder, A.J.; et al. Effectiveness of a Web- and Mobile Phone-Based Intervention to Promote Physical Activity and Healthy Eating in Middle-Aged Males: Randomized Controlled Trial of the ManUp Study. J. Med. Internet Res. 2014, 16, e136. [Google Scholar] [CrossRef] [PubMed]
- Ipjian, M.L.; Johnston, C.S. Smartphone technology facilitates dietary change in healthy adults. Nutrition 2017, 33, 343–347. [Google Scholar] [CrossRef] [PubMed]
- Mummah, S.; Robinson, T.N.; Mathur, M.; Farzinkhou, S.; Sutton, S.; Gardner, C.D. Effect of a mobile app intervention on vegetable consumption in overweight adults: A randomized controlled trial. Int. J. Behav. Nutr. Phys. Act. 2017, 14, 125. [Google Scholar] [CrossRef]
- Wharton, C.M.; Johnston, C.S.; Cunningham, B.K.; Sterner, D. Dietary Self-Monitoring, But Not Dietary Quality, Improves With Use of Smartphone App Technology in an 8-Week Weight Loss Trial. J. Nutr. Educ. Behav. 2014, 46, 440–444. [Google Scholar] [CrossRef]
- Philip, A.; Donald, K. Editorial: The Obesity Epidemic. Science 2004, 304, 1413. [Google Scholar]
- Lopez, A.D.; Mathers, C.D.; Ezzati, M.; Jamison, D.T.; Murray, C.J.L. Global and regional burden of disease and risk factors, 2001: Systematic analysis of population health data. Lancet 2006, 367, 1747–1757. [Google Scholar] [CrossRef]
- Kelly, T.; Yang, W.; Chen, C.; Reynolds, K.; He, J. Global burden of obesity in 2005 and projections to 2030. Int. J. Obes. 2008, 32, 1431–1437. [Google Scholar] [CrossRef] [PubMed]
- Withrow, D.; Alter, D.A. The economic burden of obesity worldwide: A systematic review of the direct costs of obesity. Obes. Rev. 2011, 12, 131–141. [Google Scholar] [CrossRef]
- Lim, S.S.; Vos, T.; Flaxman, A.D.; Danaei, G. A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990–2010: A systematic analysis for the Global Burden of Disease Study 2010. Lancet 2012, 380, 2224–2260. [Google Scholar] [CrossRef]
- Knowler, W.C.; Barrett-Connor, E.; Fowler, S.E.; Hamman, R.F.; Lachin, J.M.; Walker, E.A.; Nathan, D.M. Reduction in the Incidence of Type 2 Diabetes with Lifestyle Intervention or Metformin. New Engl. J. Med. 2002, 346, 393–403. [Google Scholar] [PubMed]
- Kaukua, J.; Pekkarinen, T.; Sane, T.; Mustajoki, P. Health-related quality of life in obese outpatients losing weight with very-low-energy diet and behaviour modification a 2-y follow-up study. Int. J. Obes. 2003, 27, 1233–1241. [Google Scholar] [CrossRef][Green Version]
- Klein, S.; Burke, L.E.; Bray, G.A.; Blair, S.; Allison, D.B.; Pi-Sunyer, X.; Hong, Y.; Eckel, R.H. Clinical implications of obesity with specific focus on cardiovascular disease: A statement for professionals from the American Heart Association Council on Nutrition, Physical Activity, and Metabolism: Endorsed by the American College of Cardiology Foundation. Circulation 2004, 110, 2952–2967. [Google Scholar] [PubMed]
- Ryan, D.H.; Kushner, R. The State of Obesity and Obesity Research. JAMA 2010, 304, 1835–1836. [Google Scholar] [CrossRef] [PubMed]
- Kriska, A.M.; Delahanty, L.M.; Pettee, K.K. Lifestyle intervention for the prevention of type 2 diabetes: Translation and future recommendations. Curr. Diabetes Rep. 2004, 4, 113–118. [Google Scholar] [CrossRef] [PubMed]
- Baker, R.C.; Kirschenbaum, D.S. Self-monitoring may be necessary for successful weight control. Behav. Ther. 1993, 24, 377–394. [Google Scholar] [CrossRef]
- Burke, L.E.; Warziski, M.; Starrett, T.; Choo, J.; Music, E.; Sereika, S.; Stark, S.; Sevick, M.A. Self-Monitoring Dietary Intake: Current and Future Practices. J. Ren. Nutr. 2005, 15, 281–290. [Google Scholar] [CrossRef]
- Wadden, T.A.; Crerand, C.E.; Brock, J. Behavioral Treatment of Obesity. Psychiatr. Clin. North Am. 2005, 28, 151–170. [Google Scholar] [CrossRef] [PubMed]
- Burke, L.E.; Wang, J.; Sevick, M.A. Self-Monitoring in Weight Loss: A Systematic Review of the Literature. J. Am. Diet. Assoc. 2011, 111, 92–102. [Google Scholar] [CrossRef] [PubMed]
- McClung, H.L.; Sigrist, L.D.; Smith, T.J.; Karl, J.P.; Rood, J.C.; Young, A.J.; Bathalon, G.P. Monitoring Energy Intake: A Hand-Held Personal Digital Assistant Provides Accuracy Comparable to Written Records. J. Am. Diet. Assoc. 2009, 109, 1241–1245. [Google Scholar] [CrossRef]
- Beasley, J.; Riley, W.T.; Jean-Mary, J. Accuracy of a PDA-based dietary assessment program. Nutrition 2005, 21, 672–677. [Google Scholar] [CrossRef] [PubMed]
- Glanz, K.; Murphy, S.; Moylan, J.; Evensen, D.; Curb, J.D. Improving Dietary Self-Monitoring and Adherence with Hand-Held Computers: A Pilot Study. Am. J. Health Promot. 2006, 20, 165–170. [Google Scholar] [CrossRef] [PubMed]
- Wiggins, R. Personal Digital Assistants. J. Digit. Imaging Off. J. Soc. Comput. Appl. Radiol. 2004, 17, 5–17. [Google Scholar] [CrossRef] [PubMed]
- Flanders, A.E.; Wiggins, R.H., 3rd; Gozum, M.E. Handheld computers in radiology. Radiographics 2003, 23, 1035–1047. [Google Scholar] [CrossRef][Green Version]
- Wientt, R.; Bill, E.; Wojcik, J.; Winett, S.; Bowden, T. Guide to health: Nutrition and physical activity outcomes of a group-randomized trial of an Internet-based intervention in churches. Ann. Behav. Med. A Publ. Soc. Behav. Med. 2007, 33, 251–261. [Google Scholar] [CrossRef] [PubMed]
- Chen, B.; Lu, Y.-N.; Wang, H.-X.; Ma, Q.-L.; Zhao, X.-M.; Guo, J.-H.; Hu, K.; Wang, Y.-X.; Huang, Y.-R.; Chen, P. Sexual and reproductive health service needs of university/college students: Updates from a survey in Shanghai, China. Asian J. Androl. 2008, 10, 607–615. [Google Scholar] [CrossRef] [PubMed]
- Funk, K.L.; Stevens, V.J.; Appel, L.J.; Bauck, A.; Brantley, P.J.; Champagne, C.M.; Coughlin, J.; Dalcin, A.T.; Harvey-Berino, J.; Hollis, J.F.; et al. Associations of Internet Website Use With Weight Change in a Long-term Weight Loss Maintenance Program. J. Med. Internet Res. 2010, 12, e29. [Google Scholar] [CrossRef]
- Kohl, L.F.M.; Crutzen, R.; de Vries, N.K. Online Prevention Aimed at Lifestyle Behaviors: A Systematic Review of Reviews. J. Med. Internet Res. 2013, 15, e146. [Google Scholar] [CrossRef]
- Koff, R.N.; Moreno, M.A. Older adolescents’ perceptions of personal internet use. Coll. Stud. J. 2013, 47, 390. [Google Scholar]
- Klasnja, P.; Pratt, W. Healthcare in the pocket: Mapping the space of mobile-phone health interventions. J. Biomed. Inform. 2012, 45, 184–198. [Google Scholar] [CrossRef] [PubMed]
- Stephens, J.; Allen, J.K.; Dennison Himmelfarb, C.R. “Smart” Coaching to Promote Physical Activity, Diet Change, and Cardiovascular Health. J. Cardiovasc. Nurs. 2011, 26, 282–284. [Google Scholar] [CrossRef] [PubMed]
- Riley, W.T.; Rivera, D.E.; Atienza, A.A.; Nilsen, W.; Allison, S.M.; Mermelstein, R. Health behavior models in the age of mobile interventions: Are our theories up to the task? Transl. Behav. Med. 2011, 1, 53–71. [Google Scholar] [CrossRef] [PubMed]
- Azar, K.M.J.; Lesser, L.I.; Laing, B.Y.; Stephens, J.; Aurora, M.S.; Burke, L.E.; Palaniappan, L.P. Mobile applications for weight management: Theory-based content analysis. Am. J. Prev. Med. 2013, 45, 583. [Google Scholar] [CrossRef]
- Pagoto, S.; Schneider, K.; Jojic, M.; DeBiasse, M.; Mann, D. Evidence-Based Strategies in Weight-Loss Mobile Apps. Am. J. Prev. Med. 2013, 45, 576–582. [Google Scholar] [CrossRef]
- Foster, R.; Lunn, J. 40th Anniversary Briefing Paper: Food availability and our changing diet. Nutr. Bull. 2007, 32, 187–249. [Google Scholar] [CrossRef]
- Spring, B.; Duncan, J.M.; Janke, E.A.; Kozak, A.T.; McFadden, H.G.; DeMott, A.; Pictor, A.; Epstein, L.H.; Siddique, J.; Pellegrini, C.A.; et al. Integrating Technology Into Standard Weight Loss Treatment: A Randomized Controlled Trial. JAMA Intern. Med. 2013, 173, 105–111. [Google Scholar] [CrossRef]
- Prochaska, J.O.; Velicer, W.F.; Rossi, J.S.; Goldstein, M.G.; Marcus, B.H.; Rakowski, W.; Fiore, C.; Harlow, L.L.; Redding, C.A.; Rosenbloom, D. Stages of change and decisional balance for 12 problem behaviors. Health Psychol. 1994, 13, 39–46. [Google Scholar] [CrossRef] [PubMed]
- Joost, H.-G.; Gibney, M.J.; Cashman, K.D.; Görman, U.; Hesketh, J.E.; Mueller, M.; van Ommen, B.; Williams, C.M.; Mathers, J.C. Personalised nutrition: Status and perspectives. Br. J. Nutr. 2007, 98, 26–31. [Google Scholar] [CrossRef]
- Kolt, G.S.; Rosenkranz, R.R.; Savage, T.N.; Maeder, A.J.; Vandelanotte, C.; Duncan, M.J.; Caperchione, C.M.; Tague, R.; Hooker, C.; Mummery, W.K. WALK 2—Using Web 2.0 applications to promote health-related physical activity: A randomised controlled trial protocol. BMC Public Health 2013, 13, 436. [Google Scholar] [CrossRef]
| Article | Summary of Results | Limitations | Strengths |
|---|---|---|---|
| Atienza et al., 2008 [51] | Greater intake of vegetables per 1000 kcal and increased fibre consumption from grains in the PDA group | Small sample size, self-reported dietary intake, absence of generalisation to middle aged and older populations and low retention rate | First RCT to study the effect of a PDA in dietary behaviour change |
| Olson et al., 2008 [52] | Use of a PDA among teens resulted in increased milk intake; clinicians found PDA helpful in providing necessary counselling | Lack of precision in recall measures may have obscured dietary changes; height and weight were not measured | Use of a PDA helped clinicians in counselling, confirming the role of tailored counselling and monitoring in weight management |
| Acharya et al., 2011 [48] | PDA group exhibited higher consumption of fruits and vegetables and lower intake of refined grains compared to the PR group; self-monitoring combined with PR reduced intake of total fat, saturated and mono-unsaturated fatty acids | Lack of extrapolation of findings to a wider population than the homogenous, predominantly white, educated, full-time employed female population studied | Comparison of PR and PDA system of interventions along with self-monitoring and a 91% rate of participant retention after 6 months |
| Burke, et al., 2010 [50] | Self-monitoring and median adherence were higher in the PDA group than the PR group; PDA group had reduced fat and energy intake after 6 months; PDA+FB group demonstrated highest percentage of weight loss | Only 15.2% male representation in the population; only 6 months of follow-up data were presented | First large RCT studying PR, PDA and PDA + FB with a 91% retention rate |
| Ambeba et al., 2015 [49] | Daily feedback (DFB) group exhibited significant decrease in total fat and energy intake compared to no-DFB group after 2 years, supporting the necessity of feedback | Fewer males, inclusion of participants of particular ages and BMI range and reliance on self-reported dietary intake | Daily, tailored and automated feedback in real time in an ethnically diverse population studied for 2 years with a high retention rate |
| Article | Summary of Results | Limitations | Strengths |
|---|---|---|---|
| Kattelmann et al., 2014 [54] | Experimental group reported small increase in fruit and vegetable intake but increase was not maintained at follow up; no decrease in weight but greater planning was observed in the intervention group | Self-selected attrition rates, self-reported eating measures and physical activity | Intervention content was individually tailored to increase adherence, satisfaction and confidence in the intervention |
| O’Donnell et al., 2014 [55] | Goal-setting using online intervention increased intake of fruits and vegetables; goal-setting was effective for behaviour change but not for maintenance | Goal-setting functions were not assessed; options for goal-setting were limited; self-reporting and choice of a healthy population | One of the few studies where goal achievement was linked to dietary behaviour change |
| Schwarzer et al., 2017 [53] | Significant change to Mediterranean diet; individual psychological preferences and readiness should be considered for an intervention | Lack of control group and randomization; self-reported dietary intake; self-selected participants; no attempt to compare cultural eating habits of different countries | First study to examine effects of online education on 4 social-cognitive constructs and study person-specific effects of interventions |
| Grimes et al., 2018 [56] | No change in salt intake but increase in knowledge about high salt food, salt efficacy and behaviour were improved in children | Lack of a control group, small sample size from one region and self-reporting | Study confirmed that web-based educational programmes can increase awareness and knowledge |
| Article | Summary of Results | Limitations | Strengths |
|---|---|---|---|
| Shiyko et al., 2016 [58] | Nutritional knowledge increased significantly; participants in the action stage of behaviour showed superior effects; need for individualised games; shorter activities were preferred to ones with a longer commitment | Small exclusive group already motivated to lose weight, self-report, and lack of follow-up and a control group | One of a few studies to investigate the effects of video games on BMI and nutritional knowledge |
| Zurita-Ortega et al., 2018 [57] | Decrease in fat mass and a shift toward a Mediterranean diet was observed post-intervention; the problematic effect of video games was not improved | Lack of control group; study limited to university students | Demonstrated the potential of video games in weight management |
| Article | Summary of Results | Limitations | Strengths |
|---|---|---|---|
| Duncan et al., 2014 [59] | Increased consumption of low-fat milk and high fibre bread in both print and IT groups after 3 months; intake returned to baseline levels after 9 months | Very low retention rates, limited number of observations, weight loss was not measured, and use of print materials could not be assessed | Study of IT and print based interventions in men |
| Wharton et al., 2014 [62] | Paper, memo and app group participants lost weight but dietary self-monitoring was highest in the app group | App users may have used other methods for weight loss; feedback given only in the form of calories consumed | Among the few studies that have revealed that smartphone apps can act as good self-monitors |
| Ipjian and Johnston, 2016 [60] | Greater adherence and significant decrease in urinary sodium levels in the app group; body weight remained unchanged | Use of two different data analysis techniques, no direct comparison of sodium intake over time, diet instructions differed between app and print groups and weight loss not observed | Smartphone apps monitoring individual nutrients can effect dietary changes |
| Mummah et al., 2017 [61] | Participants demonstrated high engagement with the app; a significant increase in vegetable consumption and weight loss after 8 weeks; outcome linked to frequency of app usage and individual participant characteristics | Lack of longer follow-up and generalisation of findings to a larger population | Theory driven nature of the app, goal-setting and self-monitoring resulted in greater adherence; substantial sample size, randomised controlled study design, validated FFQs * and 24-h recalls |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chen, Y.; Perez-Cueto, F.J.A.; Giboreau, A.; Mavridis, I.; Hartwell, H. The Promotion of Eating Behaviour Change through Digital Interventions. Int. J. Environ. Res. Public Health 2020, 17, 7488. https://doi.org/10.3390/ijerph17207488
Chen Y, Perez-Cueto FJA, Giboreau A, Mavridis I, Hartwell H. The Promotion of Eating Behaviour Change through Digital Interventions. International Journal of Environmental Research and Public Health. 2020; 17(20):7488. https://doi.org/10.3390/ijerph17207488
Chicago/Turabian StyleChen, Yang, Federico J. A. Perez-Cueto, Agnès Giboreau, Ioannis Mavridis, and Heather Hartwell. 2020. "The Promotion of Eating Behaviour Change through Digital Interventions" International Journal of Environmental Research and Public Health 17, no. 20: 7488. https://doi.org/10.3390/ijerph17207488
APA StyleChen, Y., Perez-Cueto, F. J. A., Giboreau, A., Mavridis, I., & Hartwell, H. (2020). The Promotion of Eating Behaviour Change through Digital Interventions. International Journal of Environmental Research and Public Health, 17(20), 7488. https://doi.org/10.3390/ijerph17207488







