Physical Activity Changes and Its Risk Factors among Community-Dwelling Japanese Older Adults during the COVID-19 Epidemic: Associations with Subjective Well-Being and Health-Related Quality of Life
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Setting
2.2. Participants and Survey Procedures
2.3. Measurement
2.3.1. Social Demographics and Baseline Characteristics
2.3.2. Physical Activity Behavior
2.3.3. Subjective Well-Being
2.3.4. Health-Related Quality of Life
2.4. Statistical Analysis
3. Results
3.1. Selection of Participants
3.2. Social Demographics and Baseline Characteristics
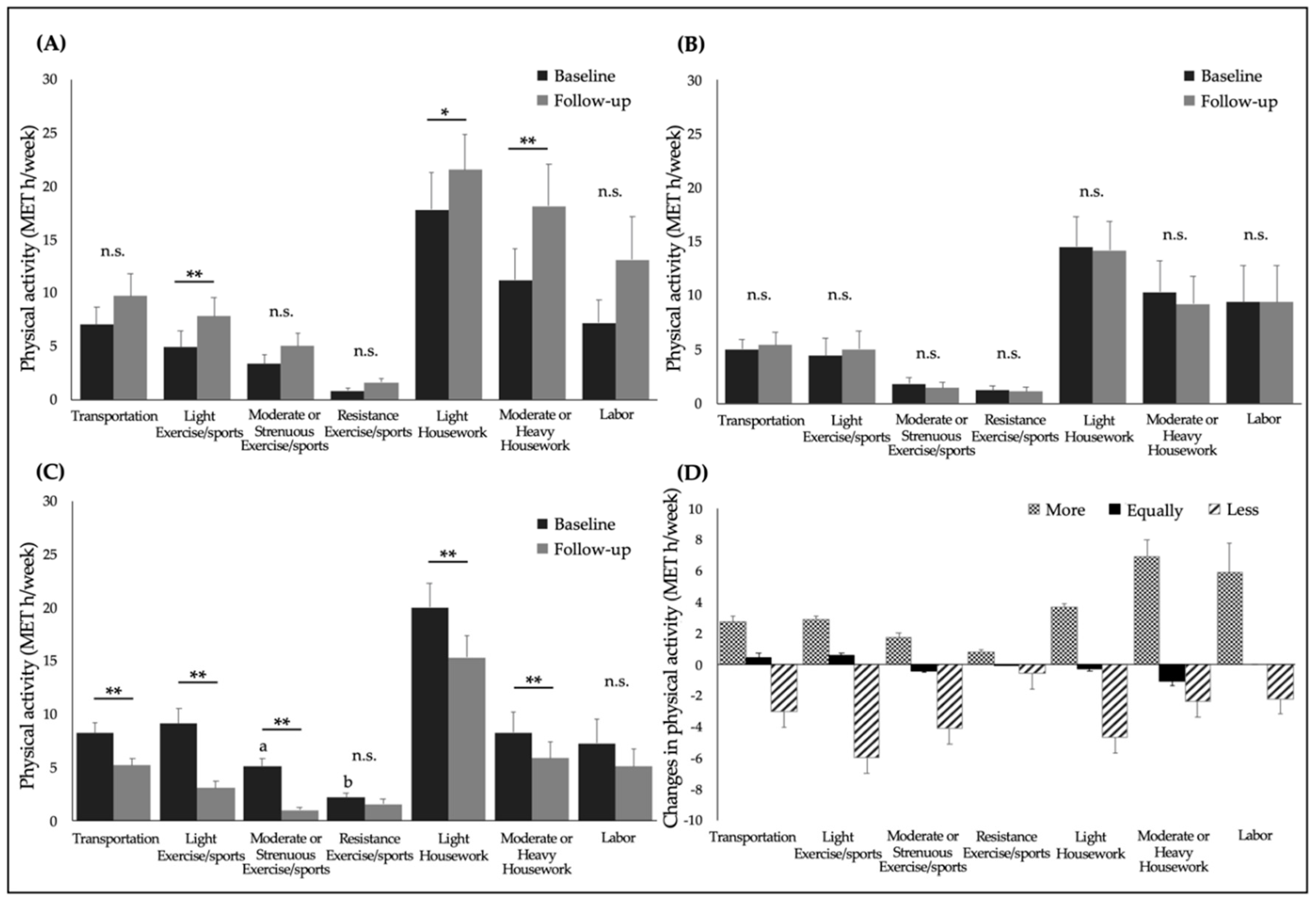
3.3. Changes in Physical Activity before and during COVID-19 Restrictions
3.4. SWB and HRQoL Scores Based on Changes to Physical Activity
3.5. Determinants of Decreased Physical Activity
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Ren, L.L.; Wang, Y.M.; Wu, Z.Q.; Xiang, Z.C.; Guo, L.; Xu, T.; Jiang, Y.Z.; Xiong, Y.; Li, Y.J.; Li, X.W.; et al. Identification of a novel coronavirus causing severe pneumonia in human: A descriptive study. Chin. Med. J. 2020, 133, 1015–1024. [Google Scholar] [CrossRef] [PubMed]
- Prime Minister of Japan and His Cabinet. Declaration of a State of Emergency in Response to the Novel Coronavirus Disease. 16 April. Available online: http://japan.kantei.go.jp/ongoingtopics/_00020.html. (accessed on 24 August 2020).
- Maugeri, G.; Castrogiovanni, P.; Battaglia, G.; Pippi, R.; D’Agata, V.; Palma, A. The impact of physical activity on psychological health during Covid-19 pandemic in Italy. Heliyon 2020, 6, e04315. [Google Scholar] [CrossRef] [PubMed]
- Stanton, R.; To, Q.G.; Khalesi, S.; Williams, S.L.; Alley, S.J.; Thwaite, T.L.; Fenning, A.S.; Vandelanotte, C. Depression, anxiety and stress during COVID-19: Associations with changes in physical activity, sleep, tobacco and alcohol use in australian adults. Int. J. Environ. Res. Public Health 2020, 17, 4065. [Google Scholar] [CrossRef] [PubMed]
- Lesser, I.A.; Nienhuis, C.P. The impact of COVID-19 on physical activity behavior and well-being of canadians. Int. J. Environ. Res. Public Health 2020, 17, 3899. [Google Scholar] [CrossRef] [PubMed]
- Physical Activity Guidelines Advisory Committee. Introducing the physical activity guidelines for Americans. In Physical Activity Guidelines for Americans, 2nd ed.; Department of Human and Health Services: Washington, WA, USA, 2018; p. 21. [Google Scholar] [CrossRef]
- Lautenschlager, N.T.; Almeida, O.P.; Flicker, L.; Janca, A. Can physical activity improve the mental health of older adults? Ann. Gen. Hosp. Psychiatry 2004, 3, 12. [Google Scholar] [CrossRef][Green Version]
- Sun, F.; Norman, I.J.; While, A.E. Physical activity in older people: A systematic review. BMC Public Health 2013, 13, 449. [Google Scholar] [CrossRef]
- Scully, D.; Kremer, J.; Meade, M.M.; Graham, R.; Dudgeon, K. Physical exercise and psychological well being: A critical review. Br. J. Sports Med. 1998, 32, 111–120. [Google Scholar] [CrossRef]
- Cooney, G.M.; Dwan, K.; Greig, C.A.; Lawlor, D.A.; Rimer, J.; Waugh, F.R.; McMurdo, M.; Mead, G.E. Exercise for depression. Cochrane Database Syst. Rev. 2013, 311, 2432–2433. [Google Scholar] [CrossRef]
- Nguyen, H.C.; Nguyen, M.H.; Do, B.N.; Tran, C.Q.; Nguyen, T.T.P.; Pham, K.M.; Pham, L.V.; Tran, K.V.; Duong, T.T.; Tran, T.V.; et al. People with suspected COVID-19 symptoms were more likely depressed and had lower health-related quality of life: The potential benefit of health literacy. J. Clin. Med. 2020, 9, 965. [Google Scholar] [CrossRef]
- Teixeira, P.J.; Carraça, E.V.; Markland, D.; Silva, M.N.; Ryan, R.M. Exercise, physical activity, and self-determination theory: A systematic review. Int. J. Behav. Nutr. Phys. Act. 2012, 9, 78. [Google Scholar] [CrossRef]
- Bauman, A.E.; Reis, R.S.; Sallis, J.F.; Wells, J.C.; Loos, R.J.F.; Martin, B.W. Correlates of physical activity: Why are some people physically active and others not? Lancet 2012, 380, 258–271. [Google Scholar] [CrossRef]
- Inoue, S.; Murase, N.; Shimomitsu, T.; Ohya, Y.; Odagiri, Y.; Takamiya, T.; Ishii, K.; Katsumura, T.; Sallis, J.F. Association of physical activity and neighborhood environment among Japanese adults. Prev. Med. 2009, 48, 321–325. [Google Scholar] [CrossRef] [PubMed]
- Koyano, W.; Shibata, H.; Nakazato, K.; Haga, H.; Suyama, Y. Measurement of competence: Reliability and validity of the TMIG index of Competence. Arch. Gerontol. Geriatr. 1991, 13, 103–116. [Google Scholar] [CrossRef]
- Fujiwara, T.; Kondo, K.; Shirai, K.; Suzuki, K.; Kawachi, I. Associations of childhood socioeconomic status and adulthood height with functional limitations among Japanese older people: Results from the JAGES 2010 project. J. Gerontol. 2014, 69, 852–859. [Google Scholar] [CrossRef] [PubMed]
- Yasunaga, A.; Park, H.; Watanabe, E.; Togo, F.; Park, S.; Shephard, R.J.; Aoyagi, Y. Development and evaluation of the physical activity questionnaire for elderly Japanese: The Nakanojo study. J. Aging Phys. Act. 2007, 15, 398–411. [Google Scholar] [CrossRef]
- Awata, S.; Bech, P.; Yoshida, S.; Hirai, M.; Suzuki, S.; Yamashita, M.; Ohara, A.; Hinokio, Y.; Matsuoka, H.; Oka, Y. Reliability and validity of the Japanese version of the world health organization-five well-being index in the context of detecting depression in diabetic patients. Psychiatry Clin. Neurosci. 2007, 61, 112–119. [Google Scholar] [CrossRef]
- Ware, J.E.; Kosinski, M.; Keller, S.D. A 12-item short-form health survey: Construction of scales and preliminary tests of reliability and validity. Med. Care 1996, 34, 220–233. [Google Scholar] [CrossRef]
- Stults-Kolehmainen, M.A.; Sinha, R. The effects of stress on physical activity and exercise. Sports Med. 2014, 44, 81–121. [Google Scholar] [CrossRef]
- Lau, J.T.F.; Griffiths, S.; Choi, K.C.; Tsui, H.Y. Avoidance behaviors and negative psychological responses in the general population in the initial stage of the H1N1 pandemic in Hong Kong. BMC Infect. Dis. 2010, 10, 139. [Google Scholar] [CrossRef]
- Cleland, V.J.; Ball, K.; Salmon, J.; Timperio, A.F.; Crawford, D.A. Personal, social and environmental correlates of resilience to physical inactivity among women from socio-economically disadvantaged backgrounds. Health Educ. Res. 2010, 25, 268–281. [Google Scholar] [CrossRef]
- Questionnaire of WHO-5-J. Available online: https://www.psykiatri-regionh.dk/who-5/Documents/WHO5_Japanese.pdf (accessed on 15 July 2020).
- Olsen, L.R.; Jensen, D.V.; Noerholm, V.; Martiny, K.; Bech, P. The internal and external validity of the major depression inventory in measuring severity of depressive states. Psychol. Med. 2003, 33, 351–356. [Google Scholar] [CrossRef] [PubMed]
- Bowler, D.E.; Buyung-Ali, L.M.; Knight, T.M.; Pullin, A.S. A systematic review of evidence for the added benefits to health of exposure to natural environments. BMC Public Health 2010, 10, 456. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, J.; Brymer, E. Nature-based guided imagery as an intervention for state anxiety. Front Psychol. 2018, 9, 1858. [Google Scholar] [CrossRef]
- Dwyer, M.J.; Pasini, M.; De Dominicis, S.; Righi, E. Physical activity: Benefits and challenges during the COVID-19 pandemic. Scand J. Med. Sci. Sports 2020, 30, 1291–1294. [Google Scholar] [CrossRef] [PubMed]
- Hammami, A.; Harrabi, B.; Mohr, M.; Krustrup, P. Physical activity and coronavirus disease 2019 (COVID-19): Specific recommendations for home-based physical training. Manag. Sport Leis. 2020. [Google Scholar] [CrossRef]
- Aubertin-Leheudre, M.; Rolland, Y. The importance of physical activity to care for frail older adults during the COVID-19 pandemic. J. Am. Med. Dir. Assoc. 2020, 21, 973–976. [Google Scholar] [CrossRef]
- Loh, R.; Stamatakis, E.; Folkerts, D.; Allgrove, J.E.; Moir, H.J. Effects of interrupting prolonged sitting with physical activity breaks on blood glucose, insulin and triacylglycerol measures: A systematic review and meta-analysis. Sports Med. 2020, 50, 295–330. [Google Scholar] [CrossRef]
- Kim, G.M.; Hong, M.S.; Noh, W. Factors affecting the health-related quality of life in community-dwelling elderly people. Public Health Nurs. 2018, 35, 482–489. [Google Scholar] [CrossRef]
- Jalenques, I.; Rondepierre, F.; Rachez, C.; Lauron, S.; Guiguet-Auclair, C. Health-related quality of life among community-dwelling people aged 80 years and over: A cross-sectional study in France. Health Qual. Life Outcomes 2020, 18, 126. [Google Scholar] [CrossRef]
- Lee, T.W.; Ko, I.S.; Lee, K.J. Health promotion behaviors and quality of life among community-dwelling elderly in Korea: A cross-sectional survey. Int. J. Nurs. Stud. 2006, 43, 293–300. [Google Scholar] [CrossRef]
- Sørensen, K.; Van Den Broucke, S.; Fullam, J.; Doyle, G.; Pelikan, J.; Slonska, Z.; Brand, H. Health literacy and public health: A systematic review and integration of definitions and models. BMC Public Health 2012, 12, 80. [Google Scholar] [CrossRef] [PubMed]
- Ishikawa, H.; Yano, E. Patient health literacy and participation in the health-care process. Heal. Expect. 2008, 11, 113–122. [Google Scholar] [CrossRef] [PubMed]
- Jayasinghe, U.W.; Harris, M.F.; Parker, S.M.; Litt, J.; van Driel, M.; Mazza, D.; Del Mar, C.; Lloyd, J.; Smith, J.; Zwar, N.; et al. The impact of health literacy and life style risk factors on health-related quality of life of Australian patients. Health Qual. Life Outcomes 2016, 14, 68. [Google Scholar] [CrossRef] [PubMed]
| Characteristics of Participants | Total | Man | Women | |
|---|---|---|---|---|
| N (%) | N (%) | N (%) | ||
| Gender | 165 (100.0) | 50 (30.3) | 115 (69.7) | |
| Age | Mean (years) | 78.6 ± 8.0 | 78.8 ± 8.4 | 78.6 ± 7.8 |
| 65–69 | 21 (12.7) | 9 (18.0) | 12 (10.4) | |
| 70–74 | 26 (15.8) | 6 (12.0) | 20 (17.4) | |
| 75–79 | 43 (26.1) | 10 (20.0) | 33 (28.7) | |
| 80–84 | 37 (22.4) | 9 (18.0) | 28 (24.3) | |
| 85–89 | 25 (15.2) | 11 (22.0) | 14 (12.2) | |
| 90 + | 13 (7.9) | 5 (10.0) | 8 (7.0) | |
| Health History | None | 24 (14.5) | 8 (16.0) | 16 (13.9) |
| Diabetes | 26 (15.8) | 9 (18.0) | 17 (14.8) | |
| Hypertension | 84 (50.9) | 23 (46.0) | 61 (53.0) | |
| Cardiovascular | 22 (13.3) | 8 (16.0) | 14 (12.2) | |
| Cerebrovascular | 28 (17.0) | 16 (32.0) | 12 (10.4) | |
| Orthopedic | 76 (78.0) | 17 (34.0) | 59 (51.3) | |
| Employment | Present | 9 (5.5) | 3 (6.0) | 6 (5.2) |
| Absent | 156 (94.5) | 47 (94.0) | 109 (94.8) | |
| Hobby | Present | 78 (47.3) | 25 (50.0) | 53 (46.1) |
| Absent | 87 (52.7) | 25 (50.0) | 62 (53.9) | |
| Family Structure | Alone | 46 (27.9) | 6 (12.0) | 40 (34.8) |
| Elderly couple | 72 (43.6) | 15 (30.0) | 57 (49.6) | |
| With family | 47 (28.5) | 9 (58.0) | 18 (15.7) | |
| Functional Health | Dependent | 96 (58.2) | 33 (66.0) | 63 (54.8) |
| Independent | 69 (41.8) | 17 (34.0) | 52 (45.2) | |
| Residential Density | High | 22 (13.3) | 5 (10.0) | 17 (14.8) |
| Low | 143 (86.7) | 45 (90.0) | 98 (85.2) | |
| Access to shops | Good | 80 (48.5) | 24 (48.0) | 56 (48.7) |
| Poor | 85 (51.5) | 26 (52.0) | 59 (51.3) | |
| Sidewalks | Present | 101 (61.2) | 31 (62.0) | 70 (60.9) |
| Absent | 64 (38.8) | 19 (38.0) | 45 (39.1) | |
| Variables | Changes in PA Since COVID-19 | Interaction Effect (Group × Time) | Main Effect (Time) | ||||
|---|---|---|---|---|---|---|---|
| More Active (n = 38) | Equally Active (n = 49) | Less Active (n = 78) | F Value | p-Value | F Value | p-Value | |
| SWB | |||||||
| Baseline | 14.8 ± 6.1 | 13.5 ± 5.4 | 14.2 ± 5.1 | 6.98 | <0.01 | 24.9 | <0.01 |
| Follow-up | 14.6 ± 5.3 | 13.2 ± 5.6 | 11.7 ± 5.6 a | ||||
| HRQoL | |||||||
| PCS | |||||||
| Baseline | 38.6 ± 12.8 | 35.5 ± 12.5 | 36.9 ± 11.9 | 0.30 | 0.74 | 0.01 | 0.99 |
| Follow-up | 39.0 ± 12.1 | 34.9 ± 13.2 | 37.0 ± 11.8 | ||||
| MCS | |||||||
| Baseline | 53.0 ± 9.6 | 52.4 ± 9.3 | 50.1 ± 10.6 | 0.34 | 0.71 | 17.4 | <0.01 |
| Follow-up | 49.0 ± 10.8 | 49.8 ± 9.9 | 47.5 ± 10.7 | ||||
| Variables | Changes in PA Since COVID-19 | Univariate Analysis | Multivariate Analysis | |||
|---|---|---|---|---|---|---|
| More/Equally Active (n = 87) | Less Active (n = 78) | OR (95%CI) | p-Value | OR (95%CI) | p-Value | |
| PA at Baseline | ||||||
| Transportation | 5.9 ± 8.3 | 8.1 ± 9.0 | 1.03 (0.99, 1.07) | 0.10 | ||
| Light exercise/sports | 4.6 ± 10.4 | 9.1 ± 12.4 | 1.04 (1.01, 1.07) | <0.01 | 1.02 (0.99, 1.06) | 0.18 |
| Moderate or strenuous exercise/sports | 2.4 ± 4.9 | 5.1 ± 7.2 | 1.17 (1.02, 1.23) | <0.01 | 1.12 (1.01, 1.24) | 0.04 |
| Resistance exercise/sports | 1.1 ± 2.4 | 2.2 ± 3.3 | 1.07 (1.03, 1.13) | < 0.01 | 1.05 (0.99, 1.10) | 0.30 |
| Light housework | 16.0 ± 20.3 | 20.0 ± 20.2 | 1.01 (0.99, 1.02) | 0.22 | ||
| Moderate or heavy housework | 10.7 ± 19.1 | 8.3 ± 16.3 | 0.99 (0.97, 1.01) | 0.37 | ||
| Labor | 8.4 ± 19.4 | 7.3 ± 19.2 | 1.00 (0.98, 1.01) | 0.67 | ||
| SWB at Baseline | 14.7 ± 5.6 | 14.2 ± 5.1 | 0.98 (0.93, 1.04) | 0.55 | ||
| HRQoL at Baseline | ||||||
| PCS | 36.8 ± 12.6 | 36.9 ± 11.9 | 0.98 (0.92, 1.05) | 0.57 | ||
| MCS | 52.7 ± 10.4 | 50.1 ± 10.6 | 0.97 (0.94, 0.99) | 0.04 | 0.96 (0.93, 0.99) | 0.03 |
| Gender (for woman) | 61 (70.1) | 54 (69.2) | 0.96 (0.49, 1.90) | 0.91 | ||
| Age | 78.9 ± 7.3 | 78.3 ± 8.8 | 0.99 (0.95, 1.02) | 0.46 | ||
| Health History | ||||||
| Diabetes | 13 (14.9) | 13 (16.7) | 1.14 (0.49, 2.64) | 0.76 | ||
| Hypertension | 42 (48.3) | 45 (57.7) | 1.40 (0.75, 2.59) | 0.29 | ||
| Cardiovascular | 11 (12.6) | 11 (14.1) | 1.14 (0.46, 2.79) | 0.78 | ||
| Cerebrovascular | 18 (20.9) | 10 (13.0) | 0.56 (0.24, 1.31) | 0.12 | ||
| Orthopedic | 39 (45.3) | 37 (48.1) | 1.11 (0.60, 2.07) | 0.73 | ||
| Employment (for presence) | 4 (4.6) | 5 (6.4) | 1.42 (0.37, 5.50) | 0.61 | ||
| Hobby (for presence) | 34 (39.1) | 45 (57.7) | 2.04 (1.09, 3.08) | 0.02 | 1.63 (0.81, 3.30) | 0.17 |
| Family Structure | ||||||
| Alone | 23 (26.4) | 23 (29.5) | 1.10 (0.55, 2.18) | 0.79 | ||
| Elderly couple | 35 (40.2) | 37 (47.4) | 1.35 (0.73, 2.52) | 0.35 | ||
| With family | 29 (33.3) | 18 (23.1) | 1.00 | |||
| Functional Health (for independent) | 33 (37.9) | 36 (46.2) | 1.41 (0.76, 2.63) | 0.28 | ||
| Residential Density (for high) | 9 (10.3) | 13 (16.7) | 1.58 (0.63, 3.98) | 0.33 | ||
| Access to Shops (for good) | 44 (50.6) | 36 (46.2) | 0.84 (0.45, 1.55) | 0.57 | ||
| Sidewalks (for presence) | 50 (57.5) | 51 (65.4) | 1.40 (0.74, 2.63) | 0.30 | ||
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Suzuki, Y.; Maeda, N.; Hirado, D.; Shirakawa, T.; Urabe, Y. Physical Activity Changes and Its Risk Factors among Community-Dwelling Japanese Older Adults during the COVID-19 Epidemic: Associations with Subjective Well-Being and Health-Related Quality of Life. Int. J. Environ. Res. Public Health 2020, 17, 6591. https://doi.org/10.3390/ijerph17186591
Suzuki Y, Maeda N, Hirado D, Shirakawa T, Urabe Y. Physical Activity Changes and Its Risk Factors among Community-Dwelling Japanese Older Adults during the COVID-19 Epidemic: Associations with Subjective Well-Being and Health-Related Quality of Life. International Journal of Environmental Research and Public Health. 2020; 17(18):6591. https://doi.org/10.3390/ijerph17186591
Chicago/Turabian StyleSuzuki, Yuta, Noriaki Maeda, Daigo Hirado, Taizan Shirakawa, and Yukio Urabe. 2020. "Physical Activity Changes and Its Risk Factors among Community-Dwelling Japanese Older Adults during the COVID-19 Epidemic: Associations with Subjective Well-Being and Health-Related Quality of Life" International Journal of Environmental Research and Public Health 17, no. 18: 6591. https://doi.org/10.3390/ijerph17186591
APA StyleSuzuki, Y., Maeda, N., Hirado, D., Shirakawa, T., & Urabe, Y. (2020). Physical Activity Changes and Its Risk Factors among Community-Dwelling Japanese Older Adults during the COVID-19 Epidemic: Associations with Subjective Well-Being and Health-Related Quality of Life. International Journal of Environmental Research and Public Health, 17(18), 6591. https://doi.org/10.3390/ijerph17186591






