Strategies and Measurement Tools in Physical Activity Promotion Interventions in the University Setting: A Systematic Review
Abstract
1. Introduction
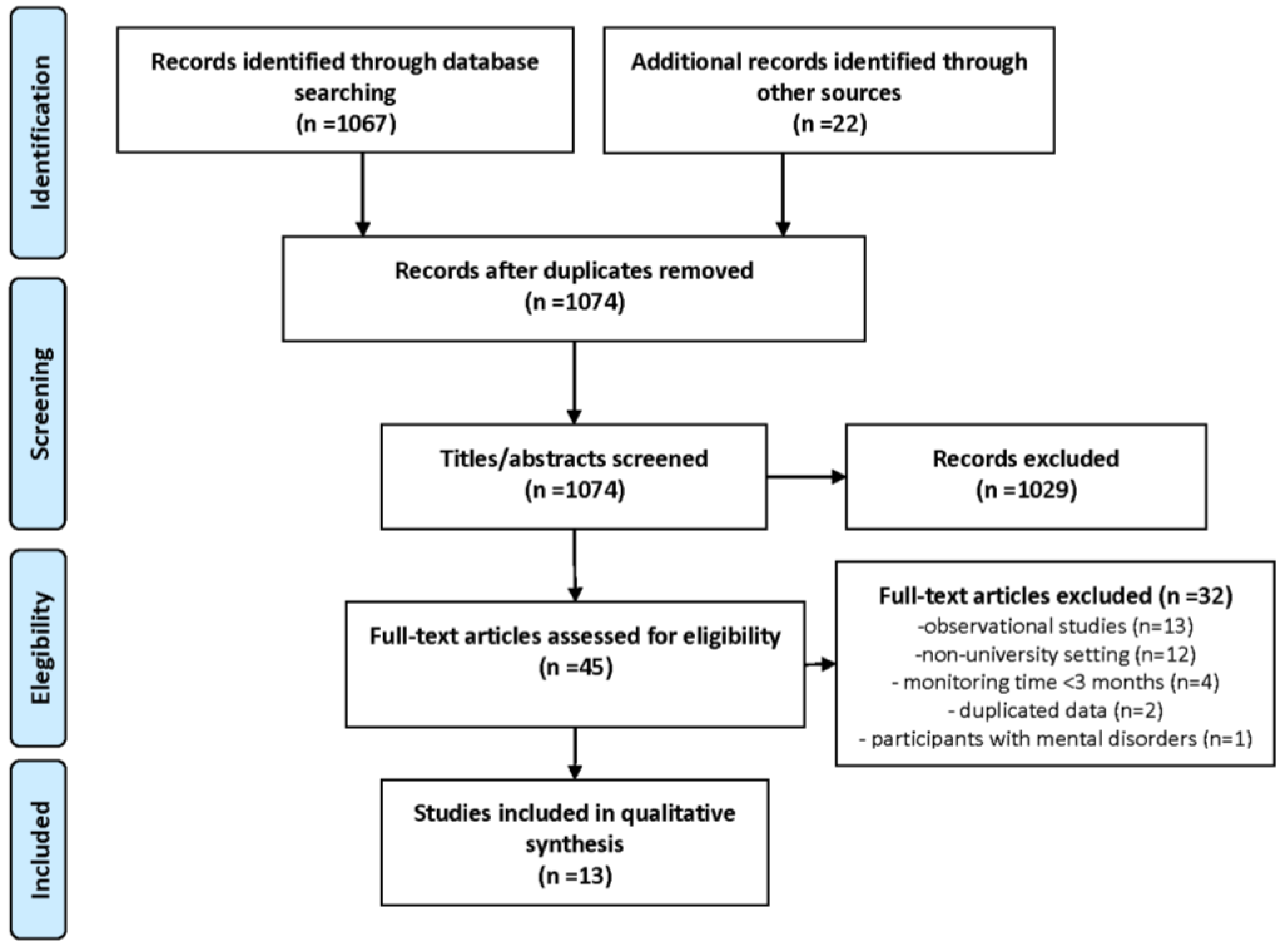
2. Materials and Methods
2.1. Selection of the Studies
2.2. Research Strategies
2.3. Data Extraction
3. Results
3.1. Descriptive Characteristics of the Included Studies
3.2. Strategies for Physical Activity Promotion in the University Setting
3.3. Data Collection Instruments
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
References
- Sallis, J.F.; Bull, F.; Guthold, R.; Heath, G.W.; Inoue, S.; Kelly, P.; Oyeyemi, A.L.; Perez, L.G.; Richards, J.; Hallal, P.C. Progress in physical activity over the Olympic quadrennium. Lancet 2016, 388, 1325–1336. [Google Scholar] [CrossRef]
- Guthold, R.; Stevens, G.A.; Riley, L.M.; Bull, F.C. Worldwide trends in insufficient physical activity from 2001 to 2016: A pooled analysis of 358 population-based surveys with 1, 9 million participants. Lancet Glob. Health 2018, 6, e1077–e1086. [Google Scholar] [CrossRef]
- Kohl, H.W.; Craig, C.L.; Lambert, E.V.; Inoue, S.; Alkandari, J.R.; Leetongin, G.; Kahlmeier, S. The pandemic of physical inactivity: Global action for public health. Lancet 2012, 380, 294–305. [Google Scholar] [CrossRef]
- Telama, R.; Yang, X.; Viikari, J.; Välimäki, I.; Wanne, O.; Raitakari, O. Physical activity from childhood to adulthood: A 21-year tracking study. Am. J. Prev. Med. 2005, 28, 267–273. [Google Scholar] [CrossRef] [PubMed]
- Mechelen, W.V.; Twisk, J.W.; Post, G.B.; Snel, J.; Kemper, H.C. Physical activity of young people: The Amsterdam Longitudinal Growth and Health Study. Med. Sci. Sports Exerc. 2000, 32, 1610–1616. [Google Scholar] [CrossRef]
- Bray, S.R.; Born, H.A. Transition to university and vigorous physical activity: Implications for health and psychological well-being. J. Am. Coll. Health 2004, 52, 181–188. [Google Scholar] [CrossRef]
- Ullrich-French, S.; Cox, A.E.; Bumpus, M.F. Physical activity motivation and behavior across the transition to university. Sport Exerc. Perform. Psychol. 2013, 2, 90–101. [Google Scholar] [CrossRef]
- De Meester, F.; van Lenthe, F.J.; Spittaels, H.; Lien, N.; De Bourdeaudhuij, I. Interventions for promoting physical activity among European teenagers: A systematic review. Int. J. Behav. Nutr. Phys. Act. 2009, 6, 82. [Google Scholar] [CrossRef]
- Newton, J.; Dooris, M.; Wills, J. Healthy universities: An example of a whole-system health-promoting setting. Glob. Health Promot. 2016, 23, 57–65. [Google Scholar] [CrossRef]
- Dooris, M. The “Health Promoting University”: A critical exploration of theory and practice. Health Educ. 2001, 101, 51–60. [Google Scholar] [CrossRef]
- Dooris, M.T.; Cawood, J.; Doherty, S.; Powell, S. Healthy Universities: Concept, Model and Framework for Applying the Healthy Settings Approach within Higher Education in England. University of Central Lancashire. 2010. Available online: https://healthyuniversities.ac.uk/wp-content/uploads/2016/10/HU-Final_Report-FINAL_v21.pdf (accessed on 10 July 2020).
- Ministerio de Sanidad; Servicios Sociales e Igualdad. Red Española de Universidades Saludables—REUS. Available online: https://www.mscbs.gob.es/profesionales/saludPublica/prevPromocion/promocion/UniversidadesSaludables/REUS.htm (accessed on 10 July 2020).
- Plotnikoff, R.C.; Costigan, S.A.; Williams, R.L.; Hutchesson, M.J.; Kennedy, S.G.; Robards, S.L.; Allen, J.; Collins, C.E.; Callister, R.; Germov, J. Effectiveness of interventions targeting physical activity; nutrition and healthy weight for university and college students: A systematic review and meta-analysis. Int. J. Behav. Nutr. Phys. Act. 2015, 1, 45. [Google Scholar] [CrossRef] [PubMed]
- Maselli, M.; Ward, P.B.; Gobbi, E.; Carraro, A. Promoting physical activity among university students: A Systematic review of controlled trials. Am. J. Health Prom. 2018, 32, 1602–1612. [Google Scholar] [CrossRef]
- Liberati, A.; Altman, D.G.; Tetzlaff, J.; Mulrow, C.; Gøtzsche, P.C.; Ioannidis, J.P.; Clarke, M.; Devereaux, P.J.; Kleijnen, J.; Moher, D. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: Explanation and elaboration. Br. Med. J. 2009, 339, 2700. [Google Scholar] [CrossRef] [PubMed]
- Brown, D.M.Y.; Bray, S.R.; Beatty, K.R.; Kwan, M.Y.W. Healthy Active Living: A Residence Community–Based Intervention to Increase Physical Activity and Healthy Eating During the Transition to First-Year University. J. Am. Coll. Health 2014, 62, 234–242. [Google Scholar] [CrossRef]
- Sharp, P.; Caperchione, C. The effects of a pedometer-based intervention on first- year university students: A randomized control trial. J. Am. Coll. Health 2016, 64, 630–638. [Google Scholar] [CrossRef] [PubMed]
- Annesi, J.J.; Porter, K.J.; Hill, G.M.; Goldfine, B.D. Effects of Instructional Physical Activity Courses on Overall Physical Activity and Mood in University Students. Res. Q. Exerc. Sport 2017, 88, 358–364. [Google Scholar] [CrossRef] [PubMed]
- Kattelmann, K.K.; Bredbenner, C.B.; White, A.A.; Greene, G.W.; Hoerr, S.L.; Kidd, T.; Colby, S.; Horacek, T.M.; Phillips, B.W.; Koenings, M.M.; et al. The Effects of Young Adults Eating and Active for Health (YEAH): A Theory-Based Web- Delivered Intervention. J. Nutr. Educ. Behav. 2014, 46, S27–S41. [Google Scholar] [CrossRef] [PubMed]
- Pope, L.; Harvey, J. The Impact of Incentives on Intrinsic and Extrinsic Motives for Fitness-Center Attendance in College First-Year Students. Am. J. Health Promot. 2015, 29, 192–199. [Google Scholar] [CrossRef] [PubMed]
- Pope, L.; Harvey-Berino, J. Burn and earn: A randomized controlled trial incentivizing exercise during fall semester for college first-year students. Prev. Med. 2013, 56, 197–201. [Google Scholar] [CrossRef]
- Kim, Y.; Lumpkin, A.; Lochbaum, M.; Stegemeier, S.; Kitten, K. Promoting physical activity using a wearable activity tracker in college students: A cluster randomized controlled trial. J. Sports Sci. 2018, 36, 1889–1896. [Google Scholar] [CrossRef]
- Nanney, L. Self-Determination Theory and Movement Technology in College Physical Activity Classes. Master’s Thesis, East Carolina University, Greenville, NC, USA, 2014. Available online: http://thescholarship.ecu.edu/handle/10342/4576 (accessed on 10 July 2020).
- Okazaki, K.; Okano, S.; Haga, S.; Seki, A.; Suzuki, H.; Takahashi, K. One-Year outcome of an interactive internet-based physical activity intervention among university students. Int. J. Med. Inf. 2014, 83, 354–360. [Google Scholar] [CrossRef]
- Bang, K.S.; Lee, I.; Kim, S.; Lim, C.S.; Joh, H.K.; Park, B.J.; Song, M.K. The Effects of a Campus Forest-Walking Program on Undergraduate and Graduate Students’ Physical and Psychological Health. Int. J. Environ. Res. Public Health 2017, 14, 728. [Google Scholar] [CrossRef] [PubMed]
- Cameron, D.; Epton, T.; Norman, P.; Sheeran, P.; Harris, P.R.; Webb, T.L.; Julious, S.A.; Brennan, A.; Thomas, C.; Petroczi, A.; et al. A theory-based online health behaviour intervention for new university students (U@Uni:LifeGuide): Results from a repeat randomized controlled trial. Trials 2015, 16, 555. [Google Scholar] [CrossRef] [PubMed]
- Heeren, G.A.; Jemmott, J.B.; Marange, C.S.; Gwaze, A.R.; Batidzirai, J.M.; Ngwane, Z.; Mandeya, A.; Tyler, J.C. Health-Promotion Intervention Increases Self-Reported Physical Activity in Sub-Saharan African University Students: A Randomized Controlled Pilot Study. Behav. Med. 2018, 44, 297. [Google Scholar] [CrossRef]
- Sriramatr, S.; Berry, T.R.; Spence, J.C. An Internet-Based Intervention for Promoting and Maintaining Physical Activity: A Randomized Controlled Trial. Am. J. Health Behav. 2014, 38, 430–439. [Google Scholar] [CrossRef]
- Amireault, S.; Godin, G. The Godin-Shephard Leisure-Time Physical Activity Questionnaire: Validity Evidence Supporting its Use for Classifying Healthy Adults into Active and Insufficiently Active Categories. Percept. Mot. Skills 2015, 120, 604–622. [Google Scholar] [CrossRef]
- Lee, P.H.; Macfarlane, D.J.; Lam, T.; Stewart, S.M. Validity of the international physical activity questionnaire short form (IPAQ-SF): A systematic review. Int. J. Behav. Nutr. Phys. Act. 2011, 8, 115. [Google Scholar] [CrossRef]
- Craig, C.L.; Marshall, A.L.; Sjöström, M.; Bauman, A.E.; Booth, M.L.; Ainsworth, B.E.; Pratt, M.; Ekelund, U.; Yngve, A.; Sallis, J.F.; et al. International Physical Activity Questionnaire: 12-Country Reliability and Validity. Med. Sci. Sports Exerc. 2003, 35, 1381. [Google Scholar] [CrossRef]
- Armstrong, T.; Bull, F. Development of the World Health Organization Global Physical Activity Questionnaire (GPAQ). J. Public Health 2006, 14, 66–70. [Google Scholar] [CrossRef]
- Baumgartner, T.A.; Jackson, A.S. Measurement for Evaluation in Physical Education and Exercise Science, 8th ed.; McGraw-Hill Higher Education: Boston, MA, USA, 2007; ISBN 0697294846. [Google Scholar]
- Jackson, A.W.; Morrow, J.R.; Bowles, H.R.; FitzGerald, S.J.; Blair, S.N. Construct validity evidence for single-response items to estimate physical activity levels in large sample studies. Res. Q. Exerc. Sport 2007, 78, 24–31. [Google Scholar] [CrossRef]
- Steptoe, A.; Wardle, J.; Pollard, T.M.; Canaan, L.; Davies, G.J. Stress, social support and health-related behavior: A study of smoking; alcohol consumption and physical exercise. J. Psychosom. Res. 1996, 41, 171–180. [Google Scholar] [CrossRef]
- Deliens, T.; Deforche, B.; De Bourdeaudhuij, I.; Clarys, P. Determinants of physical activity and sedentary behaviour in university students: A qualitative study using focus group discussions. BMC Public Health 2015, 28, 201. [Google Scholar] [CrossRef] [PubMed]
- Nelson, M.C.; Kocos, R.; Lytle, L.A.; Perry, C.L. Understanding the Perceived Determinants of Weight-related Behaviors in Late Adolescence: A Qualitative Analysis among College Youth. J. Nutr. Educ. Behav. 2009, 41, 287–292. [Google Scholar] [CrossRef] [PubMed]
- Tucker, P.; Gilliland, J. The effect of season and weather on physical activity: A systematic review. Public Health 2007, 121, 909–922. [Google Scholar] [CrossRef] [PubMed]
- Dasgupta, K.; Joseph, L.; Pilote, L.; Strachan, I.; Sigal, R.J.; Chan, C. Daily steps are low year-round and dip lower in fall/winter: Findings from a longitudinal diabetes cohort. Cardiovasc. Diabetol. 2010, 30, 81. [Google Scholar] [CrossRef] [PubMed]
- Rouse, P.C.; Biddle, S.J.H. An ecological momentary assessment of the physical activity and sedentary behaviour patterns of university students. Health Educ. J. 2010, 69, 116–125. [Google Scholar] [CrossRef]
- Buckworth, J.; Nigg, C. Physical activity, exercise and sedentary behavior in college students. J. Am. Coll. Health 2004, 53, 28–34. [Google Scholar] [CrossRef]
- Morales-Asencio, J.M.; Gonzalo-Jiménez, E.; Martín-Santos, J.F.; Morilla-Herrera, J.C. Salud pública basada en la evidencia: Recursos sobre la efectividad de intervenciones en la comunidad. Rev. Esp. Salud Pública 2008, 82, 5–20. [Google Scholar] [CrossRef][Green Version]
- Nebot, M.; Victoria, C. Valorando la efectividad de las intervenciones en salud pública: La fuerza de los «diseños evaluativos débiles». Gac. Sanit. 2011, 25, 1–2. [Google Scholar] [CrossRef]
| Author | Publication (Year) | Country | Population | Intervention Length and Measurement Times (T) |
|---|---|---|---|---|
| Annesi et al. [18] | 2017 | USA | n = 84 students. 69% women. Age (mean ± standard deviation) = 22.0 ± 5.5 years. Controlled non-randomized trial. Control group was selected from the same universities with students non-involved in the intervention. | Intervention: 10 or 15 weeks T1: Basal T2: PI 1 (week 10 or 15 based on the university). |
| Bang et al. [25] | 2017 | South Korea | n = 99 students and graduates from Seoul. 53% graduates 52% women. Age = 24.3 ± 4.2 years. Controlled non-randomized trial. Assignation to intervention or control group was made according to participants’ preference | Intervention: 6 weeks T1: Basal T2: PI. week 6 T3: 3 months after ending intervention. |
| Brown et al. [16] | 2014 | Canada | n = 174 first year students. 58% women Age = 17.97 ± 0.95 years Field trial. Allocation to intervention or control residence was made according to participant’s preference | Intervention: 20 weeks T1: Basal T2: Follow-up. End 2nd semester |
| Cameron et al. [26] | 2015 | United Kingdom | n = 2614 first year students 55% women. Age = 18.9 ± 2.8 years RCT 2 | Intervention: academic year T1: Basal T2: 1 month T3: 6 months |
| Heeren et al. [27] | 2017 | South Africa | n = 176 second year students from a university in a rural area, under 25 years. 53.4% women Age = 20.84 ± 1.49 years RCT | Intervention: 4 weeks T1: Basal T2: Follow-up. 6 months T3: Follow-up. 12 months |
| Kattelmann et al. [19] | 2014 | USA | n = 1639 students from 13 universities, under 25 years. 63% women Age = 19.3 ± 1.1 years RCT | Intervention: 3 months T1: Basal T2: 3 months (PI) T3: 15 months (follow-up). |
| Kim et al. [22] | 2018 | USA | n = 187 students from a public university following a physical activity instructional program. 62% women. Age = intervention 20.32 ± 1.57 y; control 20.09 ± 1.93 y. Cluster RCT | Intervention: 15 weeks T1: Basal T2: Week 7–8 (mid-semester). T3: Week 14–15 (end of semester). |
| Nanney et al [23]. | 2014 | USA | n = 1505 students from a mandatory university course about physical activity, under 25 years. 64% women Age = 19.4 ± 1.4 years, RCT | Intervention: 4 months T1: Basal T2: Week 6 (mid semester). T3: Week 12 (end of semester). |
| Okazaki et al. [24] | 2014 | Japan | n = 77 students. 35% women Age = intervention group 19.1 ± 1.3 years; control group 19.4 ± 1.2 years. RCT | Intervention: 15 weeks T1: Basal T2: 4 months (PI). T3: 12 months (follow-up). |
| Pope et al. [21] | 2013 | USA | n = 117 students from a public university. 53.8% women Age = 18 years RCT | Intervention: 12 weeks T1: Basal T2: Week 12. (end of 1st semester) |
| Pope et al. [20] | 2015 | USA | n = 117 students from a public university. 53.8% women Age = 18 years RCT | Intervention: 24 weeks T1: Basal T2: Week 12 (end of 1st semester) T3: Week 24 (end of 2nd semester) |
| Sharp et al. [17] | 2016 | Canada | n = 184 first year students. 53% women Age = 18 ± 0.69 years RCT | Intervention: 12 weeks T1: Basal T2: Week 12 (end of 1st semester) |
| Sriramatr et al. [28] | 2014 | Thailand | n = 220 female students under 25 years Age = 19 years RCT | Intervention: 3 months T1: Basal T2: Week 12. PI T3: Week 24 (follow-up) |
| Author | Intervention | Variables | Physical Activity Collection Tool |
|---|---|---|---|
| Annesi et al. [18] | INTERVENTION: Instructional elective physical activity course (25 h) including a sport-based (i.e., volleyball, tennis) or physical conditioning-based program (yoga, aerobic/strength training). CONTROL: General education course | Leisure-time PA 1 | Godin-Shephard Leisure-Time Physical Activity Questionnaire |
| Bang et al. [25] | INTERVENTION: A weekly campus forest-walking program during lunchtime for 6 weeks. They were also asked, through a text message, to walk once a week additionally on an individual basis. Participants also received one lecture in small groups. CONTROL: Daily routine | -Physical activity (1) -Health promoting behaviour (2) | (1) International Physical Activity Questionnaire-Short Form (2) Health-Promoting Lifestyle Profile II (Korean version) |
| Brown et al. [16] | INTERVENTION: Healthy Active Living Community including structured activities based on behaviour changes techniques (interactive workshops, help, and assistance regarding organized sport teams, groups of physical exercise such as a hiking club or wall-climbing association, and challenges for healthy meals…). CONTROL: Daily routine in a community not focused on healthy active living | -MVPA 2 (1) -PA Action Planning (2) -PA Outcome expectancies (3) | (1) Global Physical Activity Questionnaire (GPAQ) (2) 3-items questionnaire (3) 7-items questionnaire |
| Cameron et al. [26] | INTERVENTION: An online theory-based intervention. Participants were asked to complete a profile page that contained the self-affirmation manipulation. Students completed four short modules on each of the four health behaviours containing theory-based messages and planning exercises. Participants had access to the full website with further health messages and educational links. CONTROL: Daily routine | Physical activity per week | International Physical Activity Questionnaire (Short-Form) |
| Heeren et al. [27] | INTERVENTION: 8 modules implemented during 4 weekly sessions including interactive exercises, games, role-playing, and group discussions aimed to increase physical activities, healthy diets, and limit alcohol use. Participants practiced aerobic work-out, strength building, flexibility increasing. CONTROL: Same number of sessions focused on HIV 3 risk reduction | Physical activity during the last week | 3 open-ended items to establish if the participant met the physical activity guidelines |
| Kattelmann et al. [19] | INTERVENTION: 21 mini-educational lessons and e-mail messages about eating behavior, physical activity, stress management, and healthy weight management. Implemented through a personalized website and following precede-proceed model. Participants visit the website weekly to set goals, view a graph of their goal and recommendations. During the follow-up phase, website and e-mail remained active but no new lessons were added. CONTROL: Daily routine | Physical activity per week | International Physical Activity Questionnaire |
| Kim et al. [22] | INTERVENTION: Activity tracker was provided to be used daily during the semester and it was linked to an app for smartphones. It provided physical tracking, goal setting, and behavioural feedback, among others. CONTROL: Daily routine | Physical activity per week | Uniaxial accelerometer during 7 days in each measurement time |
| Nanney et al. [23] | INTERVENTION: Instructors of PA course received a need-supportive training during 60-min weekly. Two subgroups were built: one subgroup used a pedometer daily (linked to an app to check their goals and set new goals). The other subgroup used the pedometer just to collect information in three specific weeks (basal mid-term and end of semester). CONTROL: Instructors received conventional training during 60-min sessions weekly | -PA (1, 2, 3) -Steps/day (4) -PA enjoyment (5) -State of Change (6) -Motivation to be active (7) | (1) International Physical Activity Questionnaire-Short Form (IPAQ-SF) (2) 30-Day Physical Activity Recall (3) 8-response Physical activity self-report measure (4) Pedometer (5) 5-item Exercise enjoyment scale (6) 4-item about Physical Activity State of Change (7) Behavioral Regulation in Exercise Questionnaire-modified |
| Okazaki et al. [24] | INTERVENTION: Internet-based PA education course also with four face-to-face sessions. Participants set their goals and a weekly schedule that could be modified by them. Once a week, they received a message and a web-based quiz about physical activity, exercise, and other healthy lifestyles. CONTROL: Non-health related course during the study | -Physical activity per week (1) -State of Change (2) | (1) International Physical Activity Questionnaire (2) Stages of Change Scale for physical activity |
| Pope et al. [21] | INTERVENTION: Weekly monetary incentives during the first semester based on escalating rewards and reset contingency. During week one, they received $5 dollars for each 30-min gym visit. Every week, this amount increased by $0.25 per visit (up to max. of $7.75) as the required number of visits also increased. If they failed to reach the goal, the amount returned to base. They had access to a website displaying average and potential amount. CONTROL: No monetary payments for same goals | Gym center attendance | Identification electronic card |
| Pope et al. [20] | INTERVENTION 1: Continued-incentive condition receiving weekly incentives during the fall semester and incentives on a variable-interval schedule during the spring semester ($40 in four random weeks unknown to the participants). The fitness-center attendance was five 30-min visits per week. INTERVENTION 2: A discontinued-incentive condition receiving weekly incentives during the fall semester and no incentives during the spring semester CONTROL: No monetary payments for same goals | -Gym center attendance (1) -Motivation to be active (2) | (1) Identification electronic card (2) Exercise motivation inventory-2 (51-items) (EMI-2) |
| Sharp et al. [17] | INTERVENTION: Pedometer-based intervention. Participants were asked to wear the pedometer daily during the study and record a step log calendar. They received three monthly e-mails reminding them to record their steps and which provided tips and opportunities to increase their physical activity on campus and some health promotion educational information. CONTROL: Usual daily routines | -Physical activity (1) -Leisure time PA (2) | (1) Pedometer (2) Modified Godin-Shephard Leisure-Time Physical Activity Questionnaire. |
| Sriramatr et al. [28] | INTERVENTION 1: SOC theory-internet intervention with pre-test. Participants received a pedometer and accessed the website to record their physical activity, set goals for the next week, and identify expectative and self-efficacy. Weekly e-mails were sent, reminding them to visit the website and giving personal feedback and providing physical activity information. Participants were encouraged to accumulate at least 90 min of MVPA per week and to increase by 9 min/week. INTERVENTION 2: Intervention without pre-test: same intervention excluding pre-test CONTROL 1: Pre-test CONTROL 2: Daily usual routine (no pre-test) | -Leisure time PA (1) -Steps/day (2) -SOC 4 variables (3) | (1) Godin-Shephard Leisure-Time Physical Activity Questionnaire (Thai version) (2) Pedometer (3) Outcome Expectations; Multi-dimensional Self-Efficacy for Exercise Scale; Self-Regulation Questionnaire |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
García-Álvarez, D.; Faubel, R. Strategies and Measurement Tools in Physical Activity Promotion Interventions in the University Setting: A Systematic Review. Int. J. Environ. Res. Public Health 2020, 17, 6526. https://doi.org/10.3390/ijerph17186526
García-Álvarez D, Faubel R. Strategies and Measurement Tools in Physical Activity Promotion Interventions in the University Setting: A Systematic Review. International Journal of Environmental Research and Public Health. 2020; 17(18):6526. https://doi.org/10.3390/ijerph17186526
Chicago/Turabian StyleGarcía-Álvarez, David, and Raquel Faubel. 2020. "Strategies and Measurement Tools in Physical Activity Promotion Interventions in the University Setting: A Systematic Review" International Journal of Environmental Research and Public Health 17, no. 18: 6526. https://doi.org/10.3390/ijerph17186526
APA StyleGarcía-Álvarez, D., & Faubel, R. (2020). Strategies and Measurement Tools in Physical Activity Promotion Interventions in the University Setting: A Systematic Review. International Journal of Environmental Research and Public Health, 17(18), 6526. https://doi.org/10.3390/ijerph17186526




