Assessment of Alcohol Consumption and Anxiety as Predictors of Risk of Anorexia and Bulimia in Non-Clinicals Samples
Abstract
:1. Introduction
2. Materials and Methods
2.1. Design and Participants
2.2. Instruments
2.3. Procedure
3. Results
3.1. Alcohol Dependence
3.2. Anxiety
3.3. Body Image
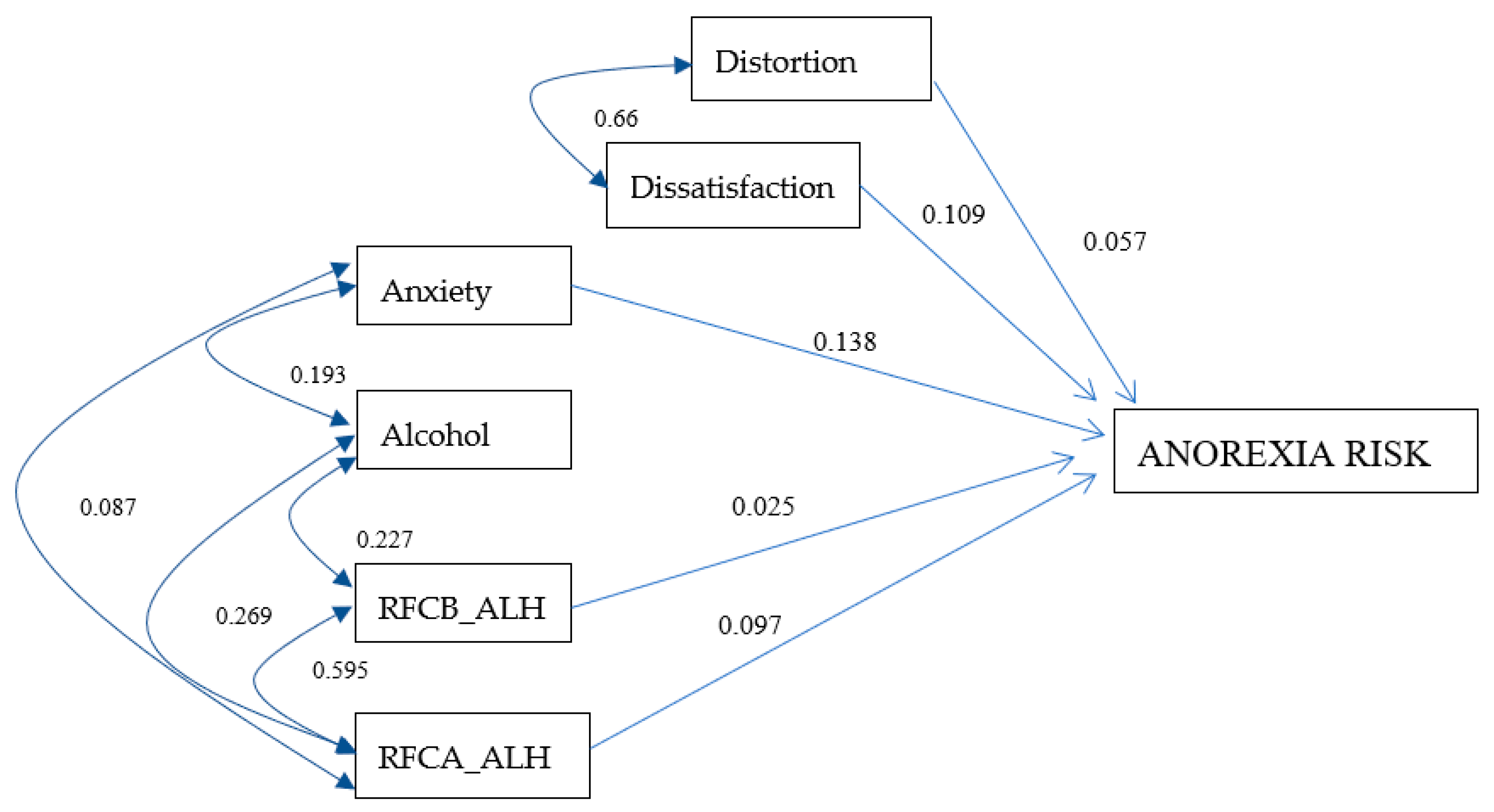
3.4. Anorexia Risk Model for Men
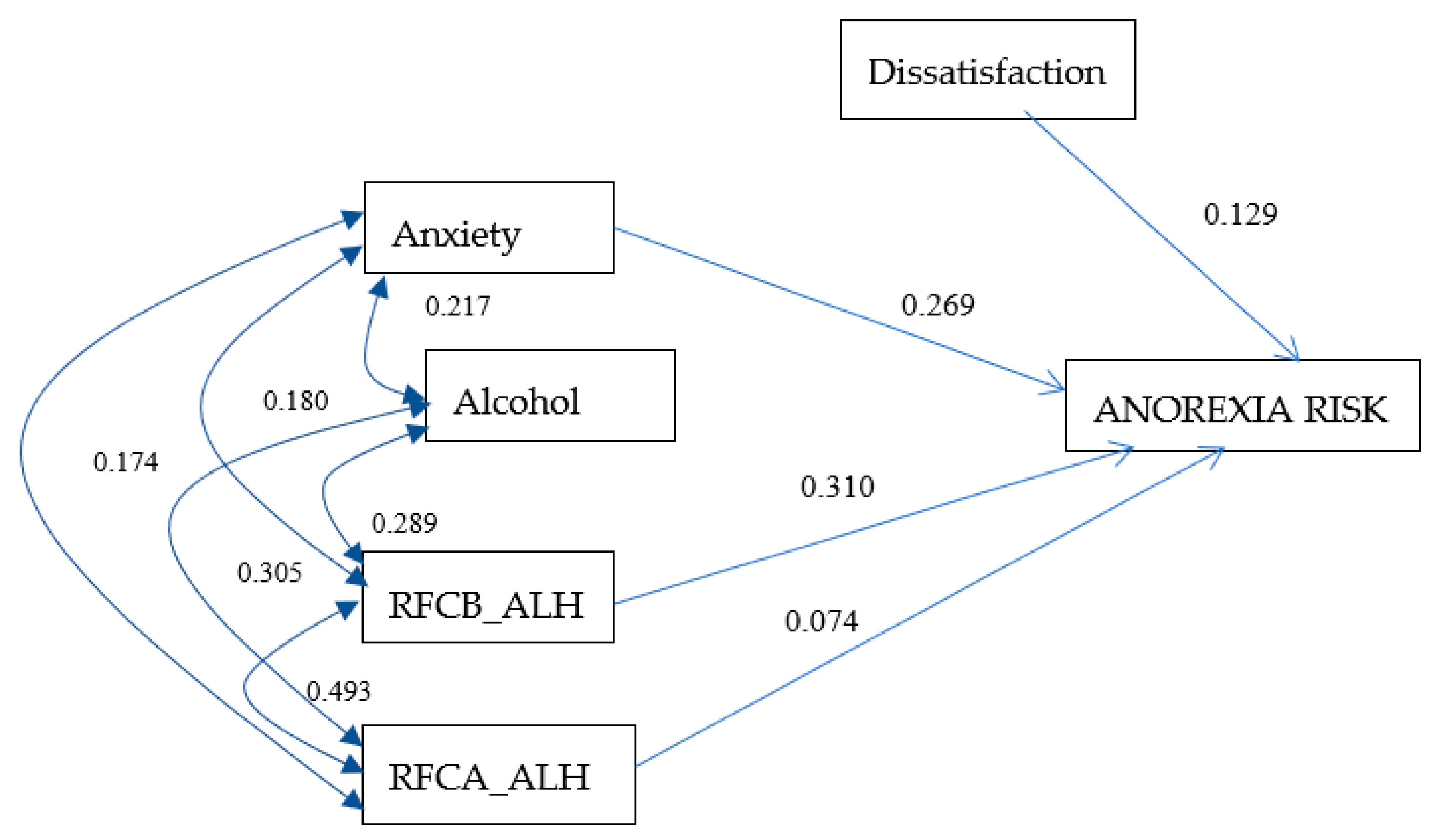
3.5. Anorexia Risk Model for Women
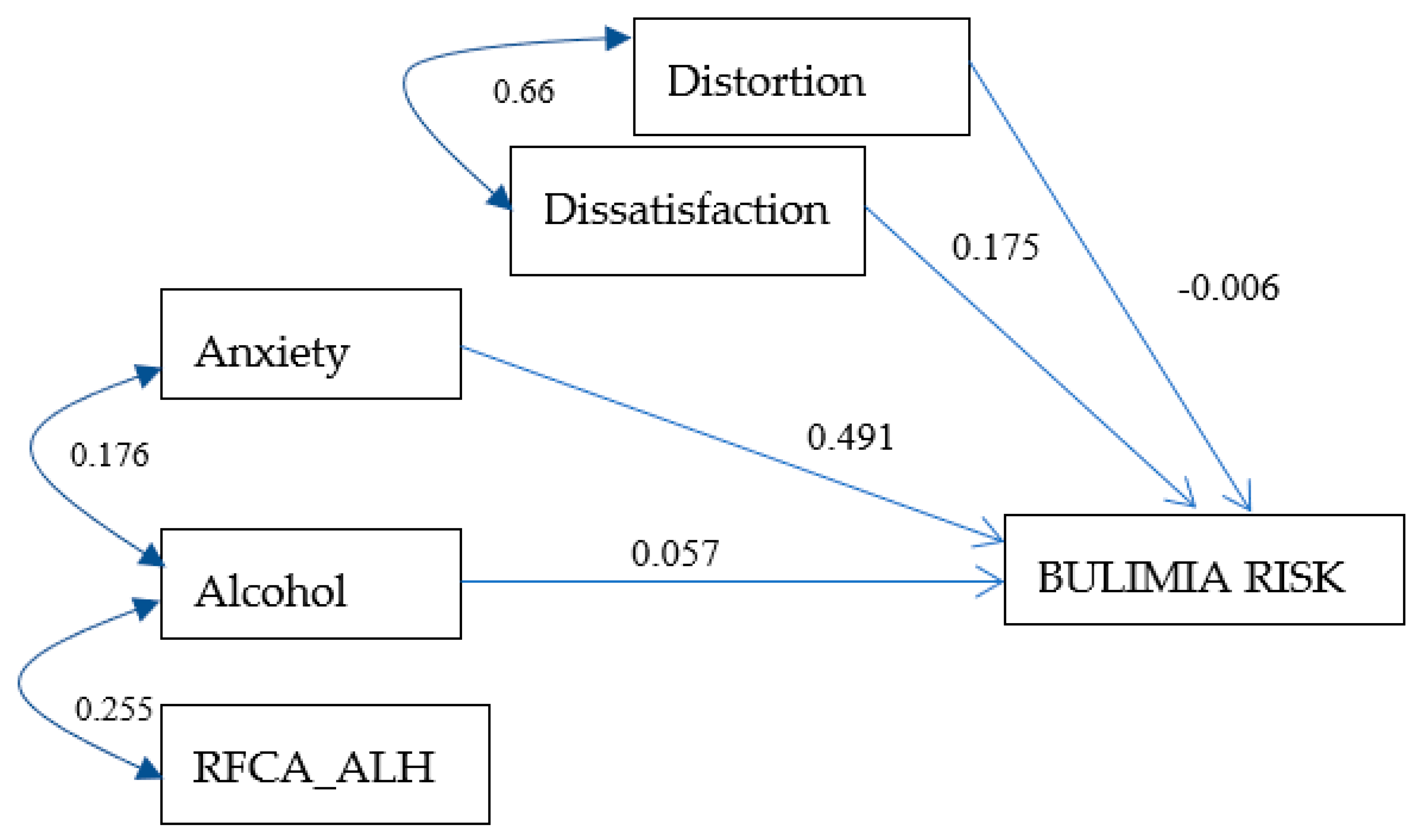
3.6. Bulimia Risk Model for Men
3.7. Bulimia Risk Model for Women
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Global Status Report on Alcohol and Health 2018. Available online: https://www.who.int/substance_abuse/publications/global_alcohol_report/en/#:~:text=21%20September%202018%20%E2%80%93%20Geneva.,represents%201%20in%2020%20deaths (accessed on 15 August 2020).
- Rehm, J.; Maters, C.; Popova, S. Global burden of disease and injury and economic cost attributable to alcohol use and alcohol -use disorders. Lancet 2009, 373, 2223–2228. [Google Scholar] [CrossRef]
- Glantz, M.D.; Bharat, C.; Degenhardt, L.; Sampson, N.A.; Scott, K.M.; Lim, C.C.W.; Kessler, R.C. The epidemiology of alcohol use disorders cross-nationally: Findings from the World Mental Health Surveys. Addict. Behav. 2019, 102, 106–128. [Google Scholar] [CrossRef] [PubMed]
- Encuesta Nacional de Consumo de Drogas, Alcohol y Tabaco, ENCODAT 2016–2017. Available online: https://www.gob.mx/salud|conadic/acciones-y-programas/encuesta-nacional-de-consumo-de-drogas-alcohol-y-tabaco-encodat-2016-2017-136758 (accessed on 15 August 2020).
- Murray, C.J.L.; Barber, R.M.; Foreman, K.J. Global, regional, and national disability-adjusted life years (DALYs) for 306 diseases and injuries and healthy life expectancy (HALE) for 188 countries, 1990–2013: Quantifying the epidemiological transition. Lancet 2015, 386, 2145–2191. [Google Scholar] [CrossRef]
- Hoek, H.W. Review of the worldwide epidemiology of eating disorders. Curr. Opin. Psychiatry 2016, 29, 336–339. [Google Scholar] [CrossRef] [Green Version]
- Encuesta Nacional de Salud y Nutrición 2012. Available online: https://ensanut.insp.mx/encuestas/ensanut2012/index.php (accessed on 15 August 2020).
- Choquette, E.M.; Ordaz, D.L.; Melioli, T.; Delage, B.; Chabrol, H.; Rodgers, R. Food and Alcohol Disturbance (FAD) in the U.S. and France: Nationality and gender effects and relations to drive for thinness and alcohol use. Eat. Behav. 2018, 31, 113–139. [Google Scholar]
- Bryant, J.B.; Darkes, J.; Rahal, C. College students’ compensatory eating and behaviors in response to alcohol consumption. J. Am. Coll. Health 2012, 5, 350–356. [Google Scholar] [CrossRef]
- Starving Themselves, Cocktail in Hand. Available online: https://www.nytimes.com/2008/03/02/fashion/02drunk.html (accessed on 15 August 2020).
- Choquette, E.M.; Rancourt, D.; Thompson, J.K. From fad to FAD: A theoretical formulation and proposed name change for “drunkorexia” to food and alcohol disturbance (FAD). Int. J. Eat. Disord. 2018, 51, 831–834. [Google Scholar] [CrossRef]
- Bohn, K.; Doll, H.A.; Cooper, Z.; Oconnor, M.; Palmer, R.L.; Fairburn, C.G. The measurement of impairment due to eating disorder psychopathology. Behav. Res. Ther. 2008, 46, 1105–1110. [Google Scholar] [CrossRef]
- Pineda-García, G.; Gómez-Peresmitré, G.; Platas, S.; Velasco, V.; Arámburo, V. Riesgo de anorexia y bulimia en función de la ansiedad y edad de la pubertad en universitarios de Baja California-México. Rev. Mex. Trastor. Aliment. 2014, 5, 80–90. [Google Scholar] [CrossRef] [Green Version]
- Asociación Psiquiátrica Americana. Manual Diagnóstico y Estadístico de Los TRASTORNOS MENTALES, 5th ed.; Editorial Médica Panamericana: Madrid, España, 2014; pp. 16–18. [Google Scholar]
- Brytek-Matera, A.; Schiltz, L. Association between attitudes towards body image, negative emotions about one’s own body and self-state representations in a clinical sample of eating disordered women. Arch. Psychiatry Psychother. 2011, 2, 37–43. [Google Scholar]
- Stice, E. A prospective test of the dual pathway model of bulimic pathology: Mediating effects of dieting and negative affect. J. Abnorm. Psychol. 2001, 110, 124–135. [Google Scholar] [CrossRef] [PubMed]
- Park, E. Overestimation and underestimation: Adolescents’ weight perception in comparison to BMI-based weight status and how it varies across socio demographic factors. J. Sch. Health 2011, 81, 57–64. [Google Scholar] [CrossRef]
- Martínez, A.G.; López-Espinoza, A.; Navarro, A.; López-Uriarte, P.; Salazar Estrada, J.G. Trastornos de la conducta de beber: Una propuesta de investigación. Rev. Mex. Trastor. Aliment. 2014, 5, 58–69. [Google Scholar]
- Gómez-Premistré, G.; Ávila, E. Conducta alimentaria y obesidad. Rev. Iberoam. 1998, 6, 10–22. [Google Scholar]
- Davidson, R.; Raistrick, D. The validity of the Short Alcohol Dependence Data (SADD) Questionnaire: A short self-report questionnaire for the assessment of alcohol dependence. Br. J. Addict. 1986, 81, 217–222. [Google Scholar] [CrossRef] [PubMed]
- Beck, A.T.; Steer, R.A. Beck Anxiety Inventory: Manual; Psychological Corporation: San Antonio, TX, USA, 1993; pp. 1–14. [Google Scholar]
- Kearney, M.; Kearney, J.M.; Gibney, M.J. Methods used to conduct the survey on consumers attitudes to food, nutrition and health on nationally. Eur. J. Clin. Nutr. 1997, 51, 417–423. [Google Scholar]
- Gómez-Peresmitré, G.; Acosta, M.V. Valoración de la delgadez: Un estudio transcultural. Psicothema 2002, 14, 221–226. [Google Scholar]
- Body Mass Index BMI. Available online: http://www.euro.who.int/en/health-topics/disease-prevention/nutrition/a-healthy-lifestyle/body-mass-index-bmi (accessed on 15 August 2020).
- Sociedad Mexicana de Psicología. Código Ético del Psicólogo, 5th ed.; Trillas: Mexico City, México, 2010; pp. 55–67. [Google Scholar]
- Ruiz, A.; Pardo, A.; San Martin, R. Modelos de ecuaciones estructurales. Pap. Psicol. 2010, 31, 34–45. [Google Scholar]
- Pineda-García, G.; Gómez-Peresmitré, G.; Platas, A.S.; Velasco, V. The body: Perceived physical attractiveness, dissatisfaction, and body image alteration in adolescents of the northwest Mexican border. Psicol. Salud 2017, 27, 155–166. [Google Scholar]
- Guzmán, S.R. Factores Psicosociales Asociados con Conductas Alimentarias de Riesgo en Adolescentes con Obesidad. Ph.D. Thesis, Universidad Nacional Autónoma de México, Mexico City, México, 2012. [Google Scholar]
- Giles, S.; Champion, H.; Sutfin, E.; McCoy, T.; Wagoner, K. Calorie restriction on drinking days: An examination of drinking consequences among college students. J. Am. Coll. Health 2009, 57, 603–609. [Google Scholar] [CrossRef] [Green Version]
- Barry, A.E.; Whiteman, S.; Piazza-Gardner, A.K.; Jensen, A.C. Gender differences in the associations among body mass index, weight loss, exercise, and drinking among college students. J. Am. Coll. Health 2013, 61, 407–413. [Google Scholar] [CrossRef] [PubMed]
- Peralta, R.L. Alcohol use and the fear of weight gain in college: Reconciling two social norms. Gend. Issues 2002, 20, 23–42. [Google Scholar] [CrossRef]
- Weeden, J.; Sabini, J. Physical attractiveness and health in Western societies: A review. Psychol. Bull. 2005, 131, 635–653. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Smith, J.; Waldorf, V.A.; Trembath, D. Single white male looking for thin, very attractive. Sex Roles 1990, 23, 675–685. [Google Scholar] [CrossRef]
- Leblanc, V.; Begin, C.; Corneau, L.; Dodin, S.; Lemieux, S. Gender differences in dietary intakes: What is the contribution of motivational variables? J. Hum. Nutr. Diet. 2014, 28, 37–46. [Google Scholar] [CrossRef]
- Carter, A.C.; Brandon, K.O.; Goldman, M.S. The college and noncollege experience: A review of the factors that influence drinking behavior in young adulthood. J. Stud. Alcohol Drugs 2010, 71, 742–750. [Google Scholar] [CrossRef]
- Young, A.M.; Morales, M.; McCabe, S.E.; Boyd, C.J.; D’Arcy, H. Drinking like a guy: Frequent binge drinking among undergraduate women. Subst. Use Misuse 2005, 40, 241–267. [Google Scholar] [CrossRef]
- Wilsnack, R.; Wilsnack, S.; Gmel, G.; Wolfgang Kantor, L. Gender differences in binge drinking. Prevalence, predictor, and consequences. Alcohol Res. 2018, 39, 57–76. [Google Scholar]
- Anderson, T. Bulimia and alcohol: Linking and unlinking disordered behavior. Scan’s Pulse 2005, 24, 1–4. [Google Scholar]
- Bulik, C.M.; Sullivan, P.F.; McKee, M.; Weltzin, T.E.; Kaye, W.H. Characteristics of bulimic women with and without alcohol abuse. Am. J. Drug Alcohol Abus. 1994, 20, 273–283. [Google Scholar] [CrossRef]
- Mustelin, L.; Latvala, A.; Raevuori, A.; Rose, R.J.; Kaprio, J.; Keski-Rahkonen, A. Risky drinking behaviors among women with eating disorders—A longitudinal community-based study. Int. J. Eat. Disord. 2016, 49, 563–571. [Google Scholar] [CrossRef] [PubMed]
- Fairburn, C.G.; Brownell, K.D. Eating Disorders and Obesity: A Comprehensive Handbook, 2nd ed.; Guilford Press: New York, NY, USA, 2002; pp. 247–250. [Google Scholar]
- Sassaroli, S.; Fiore, F.; Mezzaluna, C.; Ruggiero, G. Stressful task increases drive for thinness and bulimia: A laboratory study. Front. Psychol. 2015, 6, 591–600. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bandura, A. Self-Efficacy: Toward a unifying theory of behavioral change. Psychol. Rev. 1977, 84, 191–215. [Google Scholar] [CrossRef] [PubMed]
- Zhou, G.; Gan, Y.; Ke, Q.; Knoll, N.; Lonsdale, C.; Schwarzer, R. Avoiding exposure to air pollution by using filtering facemask respirators: An application of the Health Action Process Approach. Health Psychol. 2016, 35, 141–147. [Google Scholar] [CrossRef] [PubMed]
- Williams, M.; Teesdale, J.; Segal, Z.; Kabat-Zinn, J. The Mindful Way through Depression: Freeing Yourself from Chronic Unhappiness, 1st ed.; Guilford Publications: New York, NY, USA, 2007; pp. 11–116. [Google Scholar]
- Festinger, L. A Theory of Cognitive Dissonance, 1st ed.; Stanford University Press: Redwood City, CA, USA, 1957; pp. 1–291. [Google Scholar]
- Stice, E.; Chase, A.; Stormer, S.; Appel, A. A randomized trial of a dissonance-based eating-disorders prevention program. Int. J. Eat. Disord. 2001, 29, 247–262. [Google Scholar] [CrossRef] [PubMed]

| Sex | Total | ||
|---|---|---|---|
| Men | Women | ||
| No dependency | 27.2% | 36.6% | 31.9% |
| Low dependence | 60.5% | 54.7% | 57.6% |
| Medium dependency | 10.0% | 7.9% | 8.9% |
| High dependence | 2.3% | 0.8% | 1.5% |
| Total | 100.0% | 100.0% | 100.0% |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pineda-García, G.; Ochoa-Ruiz, E.; Gómez-Peresmitré, G.; Platas-Acevedo, S. Assessment of Alcohol Consumption and Anxiety as Predictors of Risk of Anorexia and Bulimia in Non-Clinicals Samples. Int. J. Environ. Res. Public Health 2020, 17, 6293. https://doi.org/10.3390/ijerph17176293
Pineda-García G, Ochoa-Ruiz E, Gómez-Peresmitré G, Platas-Acevedo S. Assessment of Alcohol Consumption and Anxiety as Predictors of Risk of Anorexia and Bulimia in Non-Clinicals Samples. International Journal of Environmental Research and Public Health. 2020; 17(17):6293. https://doi.org/10.3390/ijerph17176293
Chicago/Turabian StylePineda-García, Gisela, Estefanía Ochoa-Ruiz, Gilda Gómez-Peresmitré, and Silvia Platas-Acevedo. 2020. "Assessment of Alcohol Consumption and Anxiety as Predictors of Risk of Anorexia and Bulimia in Non-Clinicals Samples" International Journal of Environmental Research and Public Health 17, no. 17: 6293. https://doi.org/10.3390/ijerph17176293






