Evaluation of Physical Activity and Lifestyle Interventions Focused on School Children with Obesity Using Accelerometry: A Systematic Review and Meta-Analysis
Abstract
:1. Introduction
2. Materials and Methods
2.1. Criteria for Considering Studies for Inclusion in the Review
2.2. Protocol for Electronic Searching
2.3. Study Selection and Data Collection
2.4. Risk of Bias in Individual Studies
2.5. Statistical Analysis
3. Results
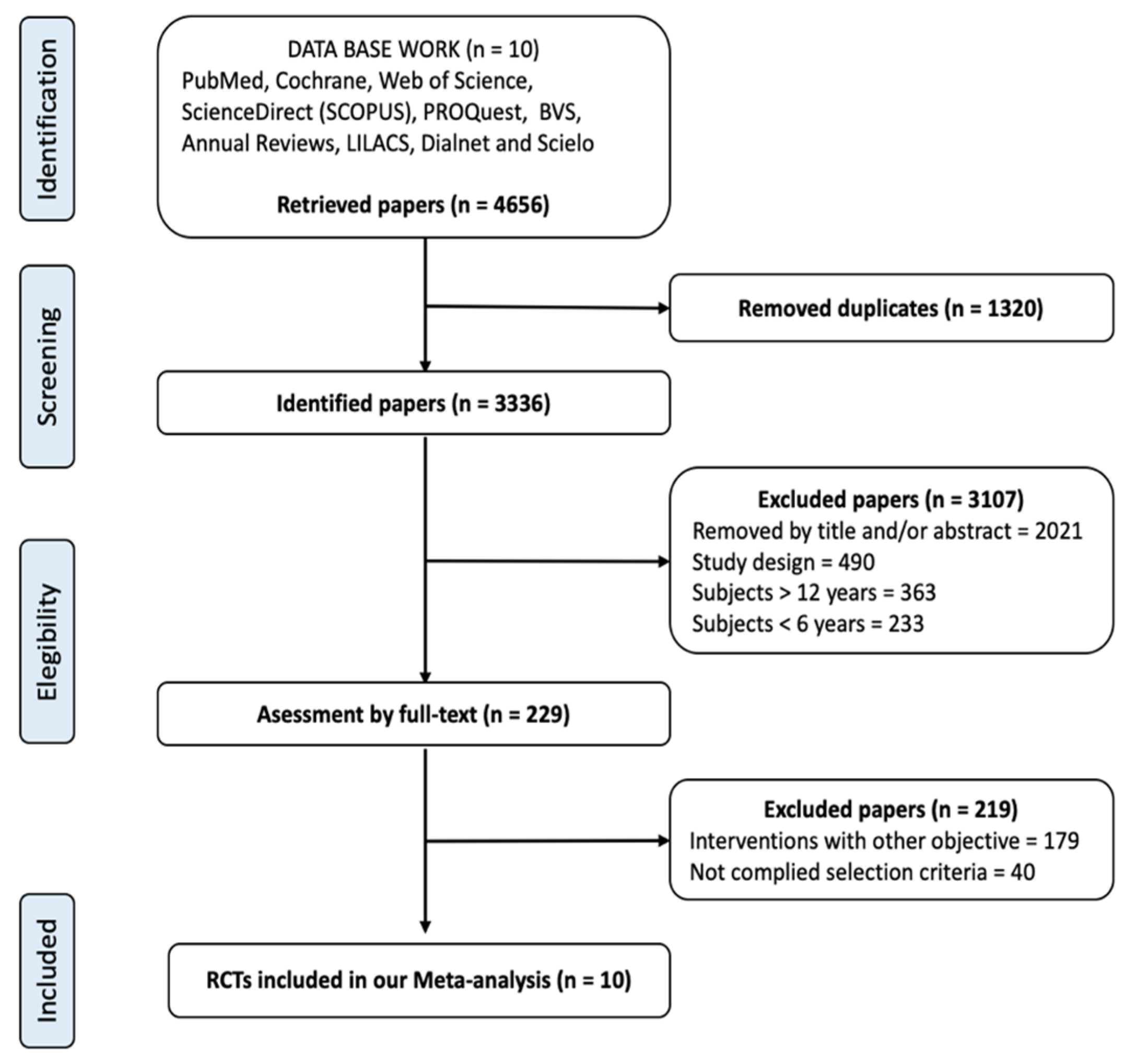
3.1. Studies Selected
3.2. Description of Selected Studies
3.3. Risk of Bias in Included Studies
3.4. Effects of the Interventions
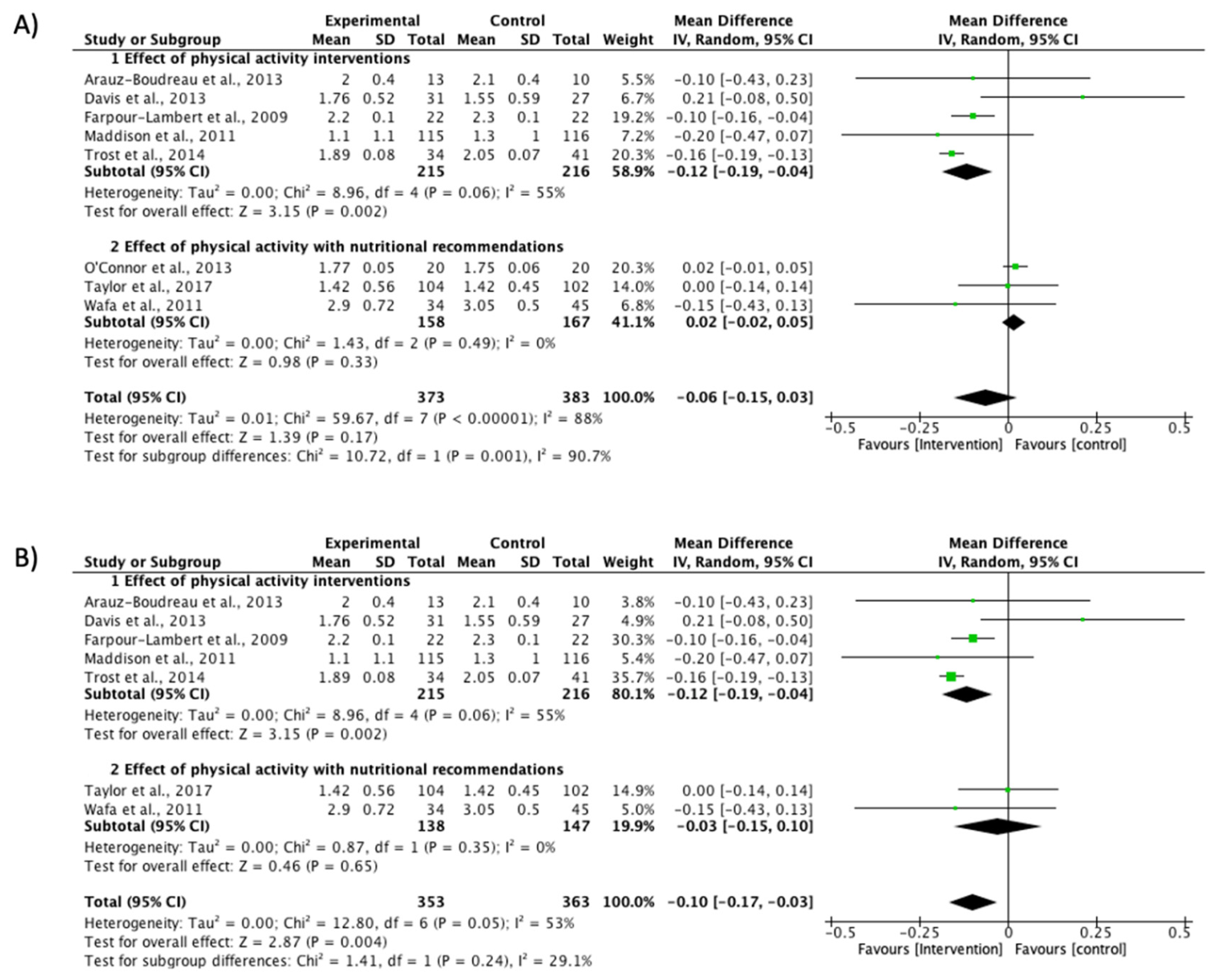
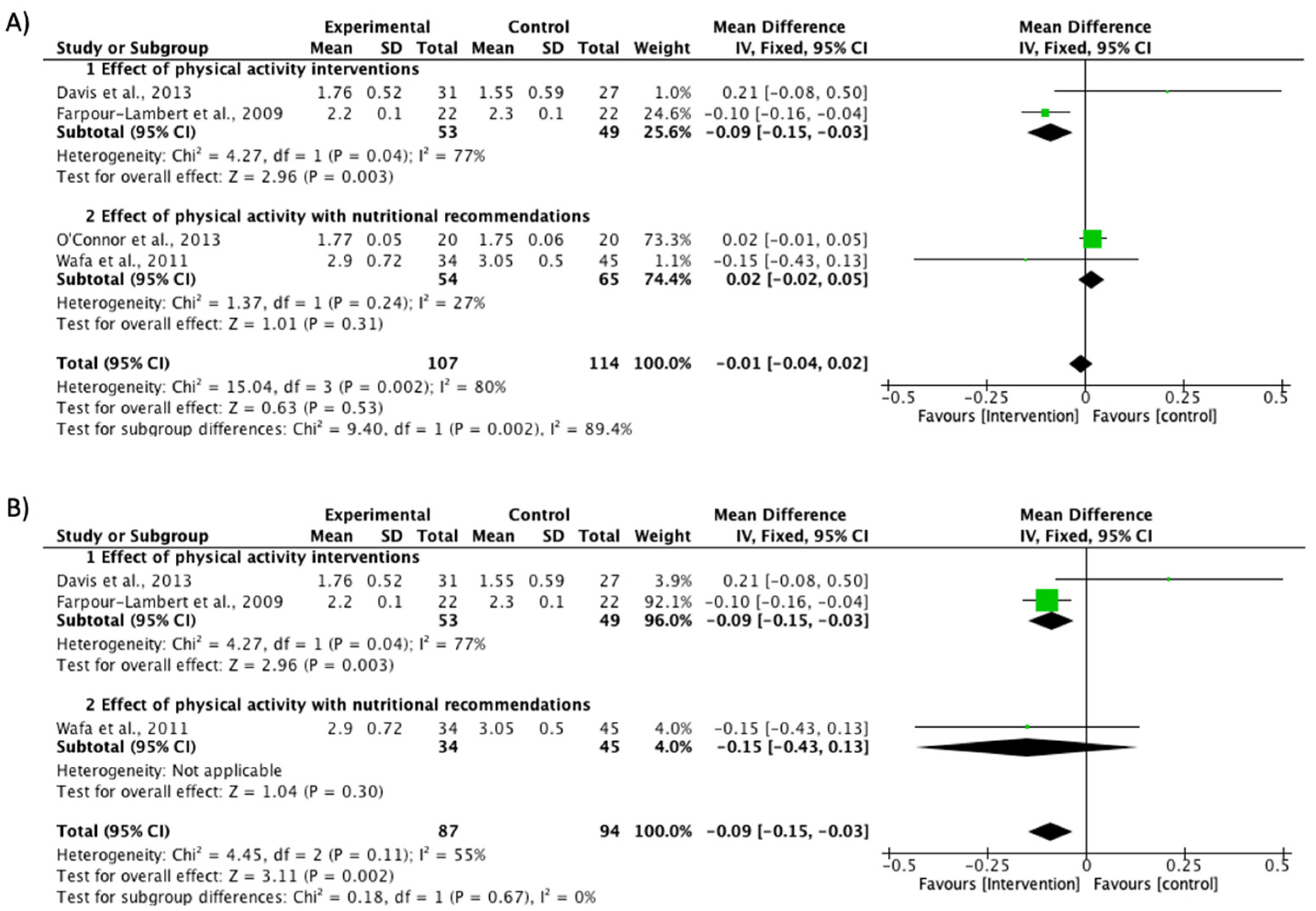
3.4.1. BMI Reduction
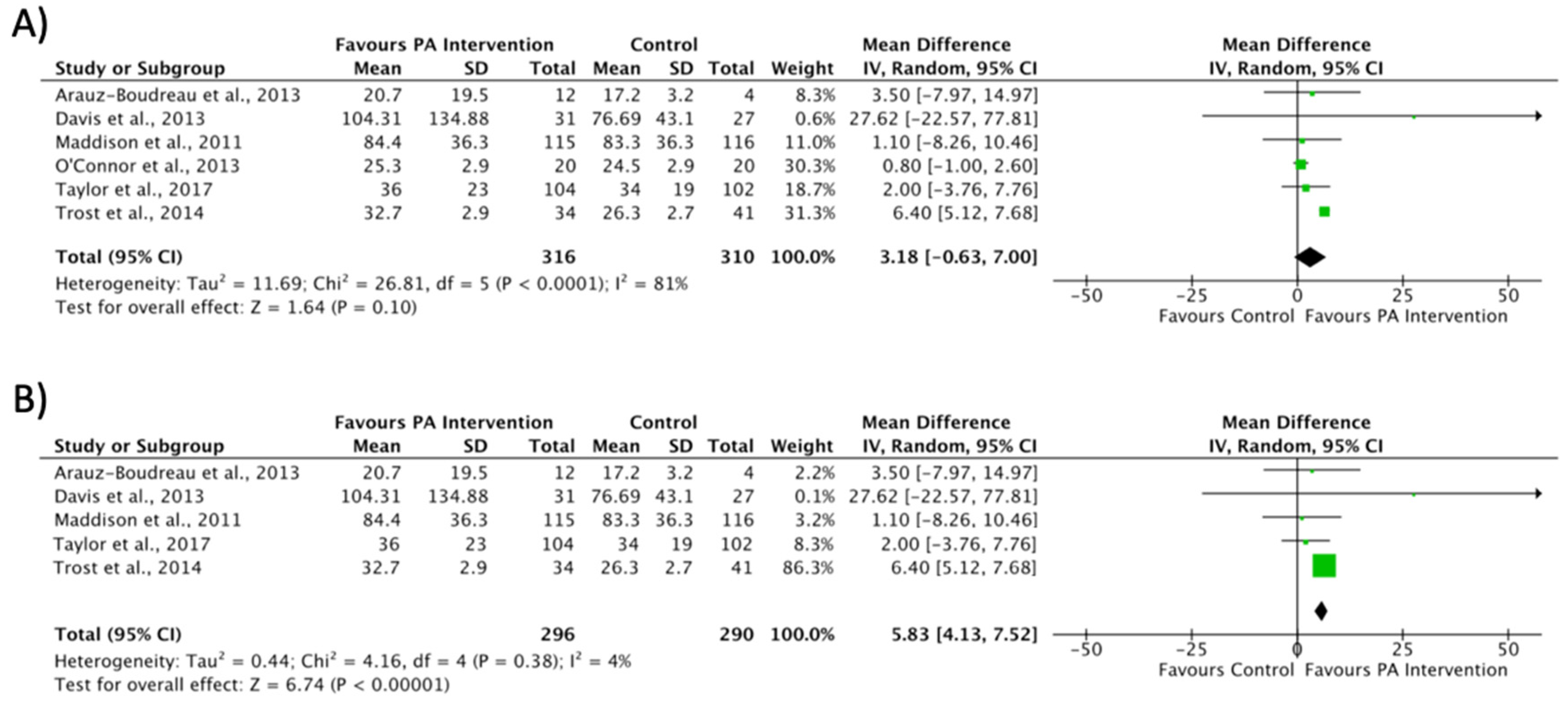
3.4.2. Engagement in Physical Activity
4. Discussion
5. Limitations
6. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Katzmarzyk, P.T.; Chaput, J.-P.; Fogelholm, M.; Hu, G.; Maher, C.; Maia, J.; Olds, T.; Sarmiento, O.L.; Standage, M.; Tremblay, M.; et al. International Study of Childhood Obesity, Lifestyle and the Environment (ISCOLE): Contributions to Understanding the Global Obesity Epidemic. Nutrients 2019, 11, 848. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Daniels, S.R. The consequences of childhood overweight and obesity. Future Child. 2006, 16, 47–67. [Google Scholar] [CrossRef] [PubMed]
- Gaziano, J.M. Fifth phase of the epidemiologic transition: The age of obesity and inactivity. JAMA 2010, 303, 275–276. [Google Scholar] [CrossRef]
- August, G.P.; Caprio, S.; Fennoy, I.; Freemark, M.; Kaufman, F.R.; Lustig, R.H.; Silverstein, J.H.; Speiser, P.W.; Styne, D.M.; Montori, V.M.; et al. Prevention and treatment of pediatric obesity: An endocrine society clinical practice guideline based on expert opinion. J. Clin. Endocrinol. Metab. 2008, 93, 4576–4599. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Matson, K.L.; Fallon, R.M. Treatment of Obesity in Children and Adolescents. J. Pediatr. Pharmacol. Ther. 2012, 17, 45–57. [Google Scholar]
- Khambalia, A.Z.; Dickinson, S.; Hardy, L.L.; Gill, T.; Baur, L.A. A synthesis of existing systematic reviews and meta-analyses of school-based behavioural interventions for controlling and preventing obesity. Obes. Rev. 2011, 13, 214–233. [Google Scholar] [CrossRef] [PubMed]
- Nooijen, C.F.J.; Galanti, M.R.; Engström, K.; Möller, J.; Forsell, Y. Effectiveness of interventions on physical activity in overweight or obese children: A systematic review and meta-analysis including studies with objectively measured outcomes. Obes. Rev. 2017, 18, 195–213. [Google Scholar] [CrossRef]
- Stice, E.; Shaw, H.; Marti, C.N. A meta-analytic review of obesity prevention programs for children and adolescents: The skinny on interventions that work. Psychol. Bull. 2006, 132, 667–691. [Google Scholar] [CrossRef] [Green Version]
- Cliff, D.P.; Okely, A.D.; Morgan, P.J.; Jones, R.A.; Steele, J.R. The impact of child and adolescent obesity treatment interventions on physical activity: A systematic review. Obes. Rev. 2009, 11, 516–530. [Google Scholar] [CrossRef]
- Biddle, S.J.H.; Braithwaite, R.; Pearson, N. The effectiveness of interventions to increase physical activity among young girls: A meta-analysis. Prev. Med. 2014, 62, 119–131. [Google Scholar] [CrossRef] [Green Version]
- Love, R.; Adams, J.; Van Sluijs, E.M.F. Are school-based physical activity interventions effective and equitable? A meta-analysis of cluster randomized controlled trials with accelerometer-assessed activity. Obes. Rev. 2019, 20, 859–870. [Google Scholar] [CrossRef] [PubMed]
- Migueles, J.H.; Cadenas-Sanchez, C.; Ekelund, U.; Nyström, C.D.; Mora-Gonzalez, J.; Löf, M.; Labayen, I.; Ruiz, J.R.; Ortega, F.B. Accelerometer Data Collection and Processing Criteria to Assess Physical Activity and Other Outcomes: A Systematic Review and Practical Considerations. Sports Med. 2017, 47, 1821–1845. [Google Scholar] [CrossRef] [PubMed]
- Oude Luttikhuis, H.; Baur, L.; Jansen, H.; Shrewsbury, V.A.; O’Malley, C.; Stolk, R.P.; Summerbell, C.D. Interventions for treating obesity in children. Cochrane Database Syst. Rev. 2009, 4, 1571–1729. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pinto, R.M.; Silva, J.V.P.; Monteiro, G.M.C.; de Resende, R.C.; Clemente, R.D.; De Souza, C. Physical Activity: Benefits for Prevention and Treatment of Childhood Obesity. J. Child Obes. 2018, 3, S2-003. [Google Scholar] [CrossRef]
- Oliveira, R.G.; Guedes, D.P. Physical Activity, Sedentary Behavior, Cardiorespiratory Fitness and Metabolic Syndrome in Adolescents: Systematic Review and Meta-Analysis of Observational Evidence. PLoS ONE 2016, 11, e0168503. [Google Scholar] [CrossRef]
- Shrestha, R.; Copenhaver, M. Long-Term Effects of Childhood Risk Factors on Cardiovascular Health During Adulthood. Clin. Med. Rev. Vasc. Health 2015, 7, 1–5. [Google Scholar] [CrossRef] [Green Version]
- Ness, A.R.; Leary, S.D.; Mattocks, C.; Blair, S.N.; Reilly, J.J.; Wells, J.C.; Ingle, S.; Tilling, K.; Smith, G.D.; Riddoch, C. Objectively Measured Physical Activity and Fat Mass in a Large Cohort of Children. PLoS Med. 2007, 4, e97. [Google Scholar] [CrossRef] [Green Version]
- World Health Organization. Global Action Plan on Physical Activity 2018–2030: More Active People for a Healthier World; WHO: Geneva, Switzerland, 2018. [Google Scholar]
- Guthold, R.; Stevens, G.A.; Riley, L.M.; Bull, F.C. Global trends in insufficient physical activity among adolescents: A pooled analysis of 298 population-based surveys with 1·6 million participants. Lancet Child Adolesc. Health 2020, 4, 23–35. [Google Scholar] [CrossRef]
- McGuire, S. Institute of Medicine. 2012. Accelerating Progress in Obesity Prevention: Solving the Weight of the Nation. Washington, DC: The National Academies Press. Adv. Nutr. 2012, 3, 708–709. [Google Scholar] [CrossRef] [Green Version]
- Schwarzfischer, P.; Totzauer, M.; Gruszfeld, D.; Socha, P.; Luque, V.; Escribano, J.; Xhonneux, A.; Verduci, E.; Mariani, B.; Koletzko, B.; et al. BMI and recommended levels of physical activity in school children. BMC Public Health 2017, 17, 595. [Google Scholar] [CrossRef] [Green Version]
- Gori, D.; Guaraldi, F.; Cinocca, S.; Moser, G.; Rucci, P.; Fantini, M.P. Effectiveness of educational and lifestyle interventions to prevent paediatric obesity: Systematic review and meta-analyses of randomized and non-randomized controlled trials. Obes. Sci. Pract. 2017, 3, 235–248. [Google Scholar] [CrossRef] [PubMed]
- Metcalf, B.; Henley, W.; Wilkin, T. Effectiveness of intervention on physical activity of children: Systematic review and meta-analysis of controlled trials with objectively measured outcomes (EarlyBird 54). BMJ 2012, 345, e5888. [Google Scholar] [CrossRef] [Green Version]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G. Preferred Reporting Items for Systematic reviews and Meta-Analyses: The PRISMA Statement. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hendrix, I.C. RefWorks. J. Med. Libr. Assoc. 2004, 92, 111. [Google Scholar]
- Higgins, J.P.; Altman, D.G.; Gøtzsche, P.C.; Jüni, P.; Moher, D.; Oxman, A.D.; Savović, J.; Schulz, K.F.; Weeks, L.; Sterne, J.A.C. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ 2011, 343, d5928. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Takkouche, B.; Cadarso-Suárez, C.; Spiegelman, D. Evaluation of old and new tests of heterogeneity in epidemiologic meta-analysis. Am. J. Epidemiol. 1999, 150, 206–215. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Copas, J. Meta-analysis, funnel plots and sensitivity analysis. Biostatistics 2000, 1, 247–262. [Google Scholar] [CrossRef] [Green Version]
- Cochrane, T. Review Manager (RevMan) 5.3; The Nordic Cochrane Centre: Copenhagen, Denmark, 2008. [Google Scholar]
- Boudreau, A.D.A.; Kurowski, D.S.; Gonzalez, W.I.; Dimond, M.A.; Oreskovic, N.M. Latino families, primary care, and childhood obesity: A randomized controlled trial. Am. J. Prev. Med. 2013, 44, S247–S257. [Google Scholar] [CrossRef] [Green Version]
- Davis, A.M.; Sampilo, M.; Gallagher, K.S.; Landrum, Y.; Malone, B. Treating rural pediatric obesity through telemedicine: Outcomes from a small randomized controlled trial. J. Pediatr. Psychol. 2013, 38, 932–943. [Google Scholar] [CrossRef] [Green Version]
- O’Connor, T.M.; Hilmers, A.; Watson, K.; Baranowski, T.; Giardino, A.P. Feasibility of an obesity intervention for paediatric primary care targeting parenting and children: Helping HAND. Child Care Health Dev. 2011, 39, 141–149. [Google Scholar] [CrossRef]
- Trost, S.G.; Sundal, D.; Foster, G.D.; Lent, M.R.; Vojta, D. Effects of a Pediatric Weight Management Program With and Without Active Video Games. JAMA Pediatr. 2014, 168, 407. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Maddison, R.; Foley, L.; Ni Mhurchu, C.; Jiang, Y.; Jull, A.; Prapavessis, H.; Hohepa, M.; Rodgers, A. Effects of active video games on body composition: A randomized controlled trial. Am. J. Clin. Nutr. 2011, 94, 156–163. [Google Scholar] [CrossRef] [Green Version]
- Taylor, R.W.; Cox, A.; Knight, L.; Brown, D.A.; Meredith-Jones, K.; Haszard, J.J.; Dawson, A.M.; Taylor, B.J.; Williams, S.M. A Tailored Family-Based Obesity Intervention: A Randomized Trial. Pediatrics 2015, 136, 281–289. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Farpour-Lambert, N.J.; Aggoun, Y.; Marchand, L.M.; Martin, X.E.; Herrmann, F.R.; Beghetti, M. Physical Activity Reduces Systemic Blood Pressure and Improves Early Markers of Atherosclerosis in Pre-Pubertal Obese Children. J. Am. Coll. Cardiol. 2009, 54, 2396–2406. [Google Scholar] [CrossRef] [PubMed]
- Cliff, D.P.; Okely, A.D.; Morgan, P.J.; Steele, J.R.; Jones, R.A.; Colyvas, K.; Baur, L.A. Movement Skills and Physical Activity in Obese Children. Med. Sci. Sports Exerc. 2011, 43, 90–100. [Google Scholar] [CrossRef] [PubMed]
- Wafa, S.W.; Talib, R.A.; Hamzaid, N.H.; McColl, J.H.; Rajikan, R.; Ng, L.O.; Ramli, A.H.; Reilly, J.J. Randomized controlled trial of a good practice approach to treatment of childhood obesity in Malaysia: Malaysian Childhood Obesity Treatment Trial (MASCOT). Pediatr. Obes. 2011, 6, e62–e69. [Google Scholar] [CrossRef] [Green Version]
- Serra-Payá, N.; Ensenyat, A.; Castro-Viñuales, I.; Real, J.; Sinfreu-Bergues, X.; Zapata, A.; Mur, J.M.; Galindo-Ortego, G.; Solé-Mir, E.; Teixido, C. Effectiveness of a Multi-Component Intervention for Overweight and Obese Children (Nereu Program): A Randomized Controlled Trial. PLoS ONE 2015, 10, e0144502. [Google Scholar] [CrossRef] [Green Version]
- Ogden, C.L.; Kuczmarski, R.J.; Flegal, K.M.; Mei, Z.; Guo, S.; Wei, R.; Grummer-Strawn, L.M.; Curtin, L.R.; Roche, A.F.; Johnson, C.L. Centers for Disease Control and Prevention 2000 growth charts for the United States: Improvements to the 1977 National Center for Health Statistics version. Pediatrics 2002, 109, 45–60. [Google Scholar] [CrossRef] [Green Version]
- Cole, T.J.; Bellizzi, M.C.; Flegal, K.M.; Dietz, W.H. Establishing a standard definition for child overweight and obesity worldwide: International survey. BMJ 2000, 320, 1240. [Google Scholar] [CrossRef] [Green Version]
- Kromeyer-Hauschild, K.; Zellner, K. Trends in overweight and obesity and changes in the distribution of body mass index in schoolchildren of Jena, East Germany. Eur. J. Clin. Nutr. 2006, 61, 404–411. [Google Scholar] [CrossRef] [Green Version]
- Trost, S.G.; McIver, K.L.; Pate, R.R. Conducting Accelerometer-Based Activity Assessments in Field-Based Research. Med. Sci. Sports Exerc. 2005, 37, S531–S543. [Google Scholar] [CrossRef] [PubMed]
- Freedson, P.S.; Sirard, J.; Debold, E.; Pate, R.; Dowda, M.; Trost, S.; Sallis, J. Calibration of the computer science and applications, inc.(CSA) accelerometer 256. Med. Sci. Sports Exerc. 1997, 29, 45. [Google Scholar] [CrossRef]
- Sirard, J.R.; Melanson, E.L.; Li, L.; Freedson, P.S. Field evaluation of the Computer Science and Applications, Inc. physical activity monitor. Med. Sci. Sports Exerc. 2000, 32, 695–700. [Google Scholar] [CrossRef] [PubMed]
- Ekelund, U.L.; Sjöström, M.; Yngve, A.; Poortvliet, E.; Nilsson, A.; Froberg, K.A.; Wedderkopp, N.; Westerterp, K. Physical activity assessed by activity monitor and doubly labeled water in children. Med. Sci. Sports Exerc. 2001, 33, 275–281. [Google Scholar] [CrossRef] [PubMed]
- Freedson, P.S.; Pober, D.; Janz, K.F. Calibration of Accelerometer Output for Children. Med. Sci. Sports Exerc. 2005, 37, S523–S530. [Google Scholar] [CrossRef] [PubMed]
- Treuth, M.S.; Schmitz, K.; Catellier, D.J.; McMurray, R.G.; Murray, D.M.; Almeida, M.J.; Going, S.; Norman, J.E.; Pate, R. Defining accelerometer thresholds for activity intensities in adolescent girls. Med. Sci. Sports Exerc. 2004, 36, 1259–1266. [Google Scholar] [PubMed]
- Evenson, K.R.; Catellier, D.J.; Gill, K.; Ondrak, K.S.; McMurray, R.G. Calibration of two objective measures of physical activity for children. J. Sports Sci. 2008, 26, 1557–1565. [Google Scholar] [CrossRef]
- Reilly, J.J.; Coyle, J.; Kelly, L.; Burke, G.; Grant, S.; Paton, J.Y. An Objective Method for Measurement of Sedentary Behavior in 3- to 4-Year Olds. Obes. Res. 2003, 11, 1155–1158. [Google Scholar] [CrossRef]
- Puyau, M.R.; Adolph, A.L.; Vohra, F.A.; Butte, N.F. Validation and Calibration of Physical Activity Monitors in Children. Obes. Res. 2002, 10, 150–157. [Google Scholar] [CrossRef]
- Tremblay, M.S.; LeBlanc, A.G.; Kho, M.E.; Saunders, T.J.; Larouche, R.; Colley, R.C.; Goldfield, G.; Gorber, S.C. Systematic review of sedentary behaviour and health indicators in school-aged children and youth. Int. J. Behav. Nutr. Phys. Act. 2011, 8, 98. [Google Scholar] [CrossRef] [Green Version]
- LeBlanc, A.G.; Chaput, J.-P.; McFarlane, A.; Colley, R.C.; Thivel, D.; Biddle, S.J.H.; Maddison, R.; Leatherdale, S.T.; Tremblay, M.S. Active Video Games and Health Indicators in Children and Youth: A Systematic Review. PLoS ONE 2013, 8, e65351. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Okely, A.D.; Collins, C.E.; Morgan, P.J.; Jones, R.A.; Warren, J.M.; Cliff, D.P.; Burrows, T.L.; Colyvas, K.; Steele, J.R.; Baur, L.A. Multi-Site Randomized Controlled Trial of a Child-Centered Physical Activity Program, a Parent-Centered Dietary-Modification Program, or Both in Overweight Children: The HIKCUPS Study. J. Pediatr. 2010, 157, 388–394. [Google Scholar] [CrossRef]
- Shalitin, S.; Ashkenazi-Hoffnung, L.; Yackobovitch-Gavan, M.; Nagelberg, N.; Karni, Y.; Hershkovitz, E.; Loewenthal, N.; Shtaif, B.; Gat-Yablonski, G.; Phillip, M. Effects of a Twelve-Week Randomized Intervention of Exercise and/or Diet on Weight Loss and Weight Maintenance, and Other Metabolic Parameters in Obese Preadolescent Children. Horm. Res. 2009, 72, 287–301. [Google Scholar] [CrossRef] [PubMed]
- Hamid, M.S.A.; Sazlina, S.G. Interventions for obesity among schoolchildren: A systematic review and meta-analyses. PLoS ONE 2019, 14, e0209746. [Google Scholar] [CrossRef] [PubMed]
- Faigenbaum, A.D.; Rebullido, T.R.; MacDonald, J.P. Pediatric Inactivity Triad: A risky PIT. Curr. Sports Med. Rep. 2018, 17, 45–47. [Google Scholar] [CrossRef]
| Study | Group | Sample (n) | Included Only Obese Children (Yes/No) /Obese Children (%) | Gender (%F) | Treatment Length | Intervention Type | Treatment Content PA | Accelerometer | Accelerometer Time | Author Accelerometer Protocol |
|---|---|---|---|---|---|---|---|---|---|---|
| Arauz-Boudreau et al. (2013) | Control Intervention | 12 14 | No/NR | 61% | 6 months | Lifestyle educational classes and PA training sessions | 5 consecutive weekly sessions, increased to six 3 months later. | ActiGraph GT1M | Complete week; ≥8 hours on ≥4 days | Trost, 2005 |
| Cliff et al. (2011) | Control Intervention | 42 60 | No/78% | 58% | 12 months | PA skill development program and dietary modification programs aimed at parents | 6 months intervention divided into two components: 10-week face to face and 3 months with minimal contact. The first phase of treatment included weekly 2 h group sessions (90 min PA per session) and weekly ‘‘home challenge’’ activities. | ActiGraph 7164 | ≥8 consecutive days during waking hours | Freedson, 1997 |
| Davis et al. (2013) | Control Intervention | 27 31 | Yes/100% | 39% | 8 months | Multidisciplinary actions based on psychoeducational group sessions delivered via telemedicine | Session over the phone with parents to encourage healthy habits. 1-h duration for 8 weeks | ActiGraph | Complete week; ≥6 h on ≥3 days | Sirard, 2000 |
| Farpour-Lambert et al. (2009) | Control Intervention | 22 22 | Yes/100% | 64% | 3 months (3 months post-intervention) | PA training sessions | The exercise group trained 60 min 3 times/week for 3 months. | ActiGraph MT 6471 | Complete week; 24 h/day on ≥4 days (including 1 weekend day) | Ekelund, 2001 |
| Maddison et al. (2011) | Control Intervention | 162 160 | No/NR | 37% | 6 months | Active video games | Children were encouraged to meet the current PA recommendations by supplementing periods of inactivity or substituting periods of traditional non-active video games for playing AVG. | ActiGraph AM7164-2.2C | Complete week | Freedson, 2005 |
| O’Connor et al. (2013) | Control Intervention | 20 20 | Yes/100% | 80% | 7 months | Healthy family activity and nutritional recommendations | Promote healthy child lifestyle behavior with effective behavior-specific parenting practices | ActiGraph 7064 | ≥5 days; ≥800 min/day | Treuth, 2004 |
| Serra-Paya et al. (2015) | Control Intervention | 59 54 | No/NR | 44% | 8 months | PA sessions, theoretical and practical sessions for parents, behavior strategy sessions for both children and parents, and weekend activities. | 90 min PA session—3 ses/w for 8 months | ActiGraph GT3X+ | ≥8 consecutive days during waking hours | NR |
| Taylor et al. (2015) | Control Intervention | 102 104 | No/NR | 55% | 24 months | Family-based intervention with specific goals based on dietary intake and PA | Families attended monthly multidisciplinary sessions to develop specific goals suitable for the first year. Thereafter, every third month for another 12 months to discuss progress and provide support. | ActiGraph GT3X | Complete week; ≥8 hours on ≥4 days | Evenson, 2008 |
| Trost et al. (2014) | Control Intervention | 41 34 | No/35,7% | 55% | 4 months | Lifestyle educational parents and programmed active gaming | 24 session topics about aspects of nutrition, sleep hygiene, PA, screen time, and AVG 60 min PA AVG session | ActiGraph GT3X / GT3X+ | Complete week; ≥9 h on ≥3 days | Evenson, 2008 |
| Wafa et al. (2011) | Control Intervention | 55 52 | Yes/100% | 50% | 6 months | Information based nutrition and health education | 60 min PA intervention sessions (8 sessions for 6 months) | ActiGraph GT1M | 5 days; ≥10 h on ≥4 days | Reilly, 2003 |
| Puyau, 2002 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jurado-Castro, J.M.; Gil-Campos, M.; Gonzalez-Gonzalez, H.; Llorente-Cantarero, F.J. Evaluation of Physical Activity and Lifestyle Interventions Focused on School Children with Obesity Using Accelerometry: A Systematic Review and Meta-Analysis. Int. J. Environ. Res. Public Health 2020, 17, 6031. https://doi.org/10.3390/ijerph17176031
Jurado-Castro JM, Gil-Campos M, Gonzalez-Gonzalez H, Llorente-Cantarero FJ. Evaluation of Physical Activity and Lifestyle Interventions Focused on School Children with Obesity Using Accelerometry: A Systematic Review and Meta-Analysis. International Journal of Environmental Research and Public Health. 2020; 17(17):6031. https://doi.org/10.3390/ijerph17176031
Chicago/Turabian StyleJurado-Castro, Jose Manuel, Mercedes Gil-Campos, Hugo Gonzalez-Gonzalez, and Francisco Jesus Llorente-Cantarero. 2020. "Evaluation of Physical Activity and Lifestyle Interventions Focused on School Children with Obesity Using Accelerometry: A Systematic Review and Meta-Analysis" International Journal of Environmental Research and Public Health 17, no. 17: 6031. https://doi.org/10.3390/ijerph17176031






