Physical Activity, Ability to Walk, Weight Status, and Multimorbidity Levels in Older Spanish People: The National Health Survey (2009–2017)
Abstract
:1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Material and Testing
2.3. Statistical Analysis
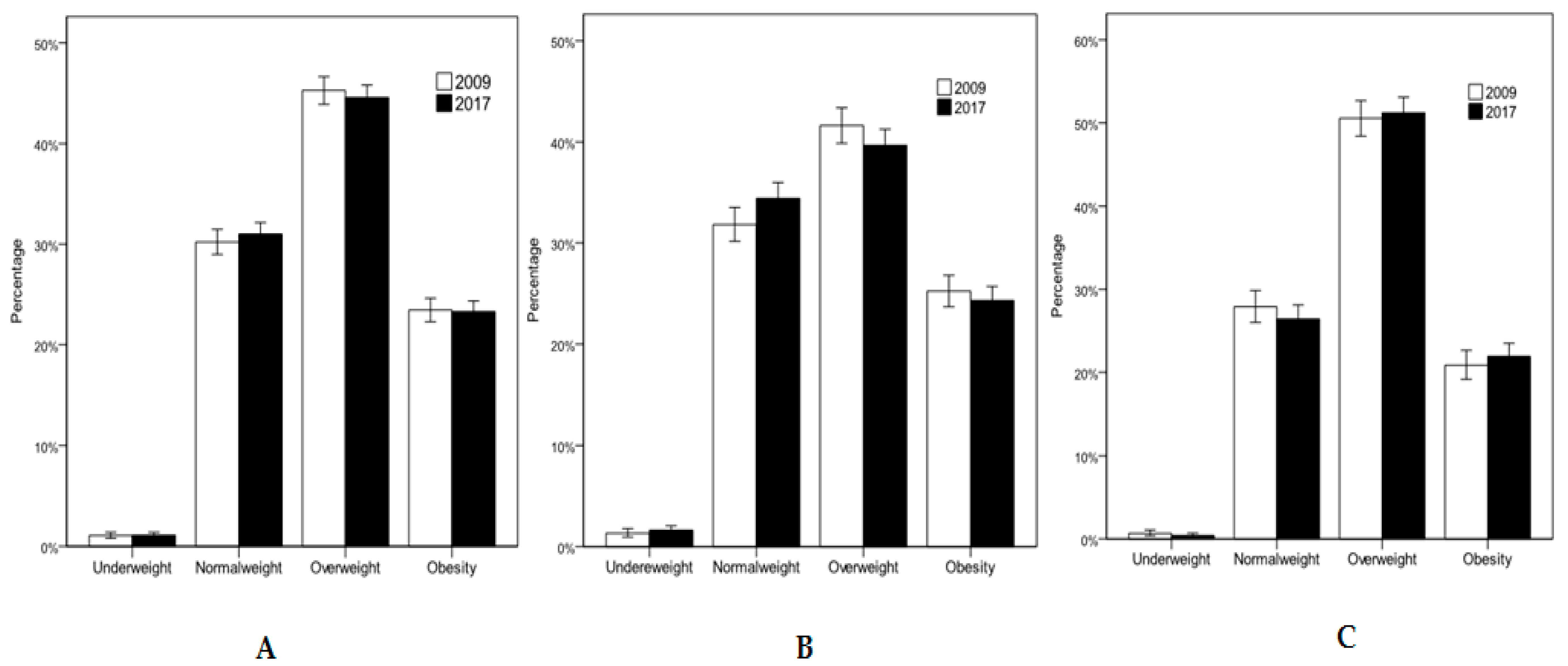
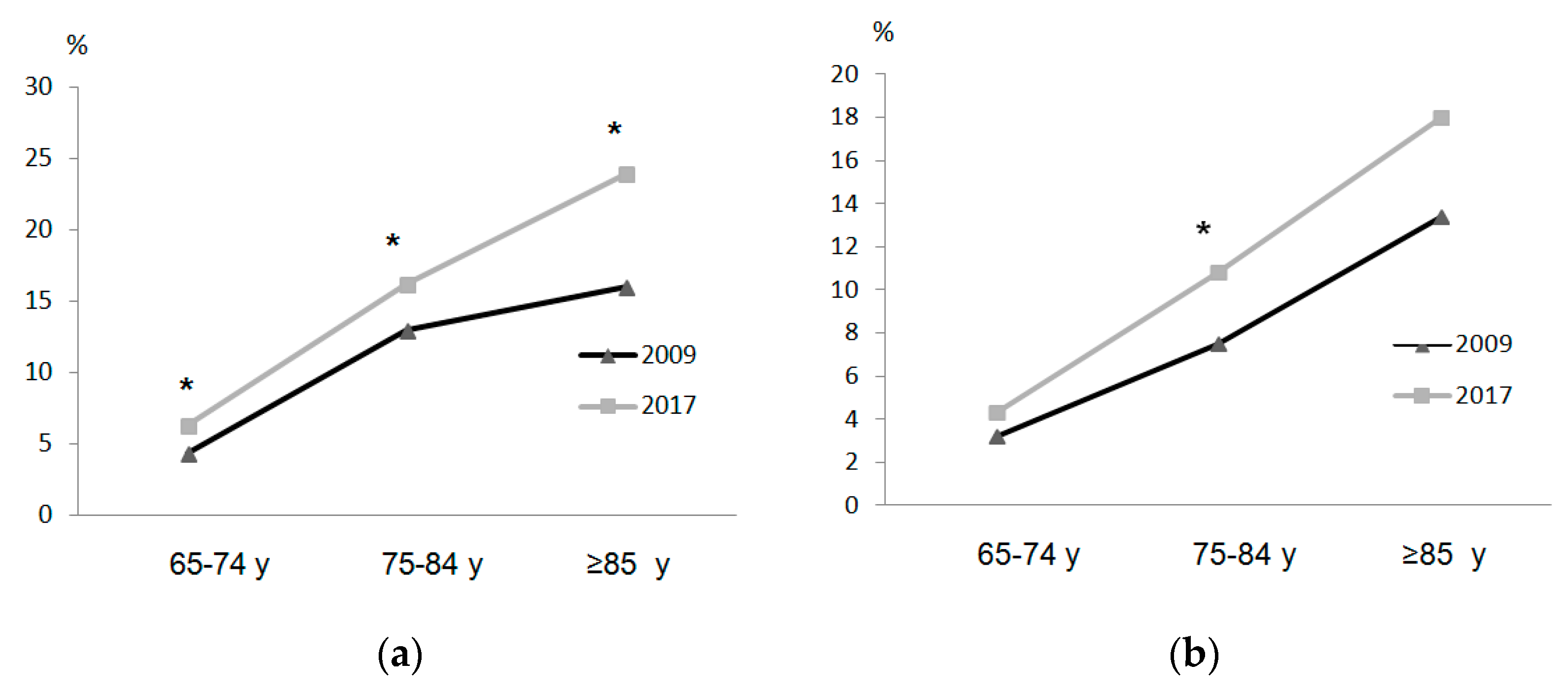
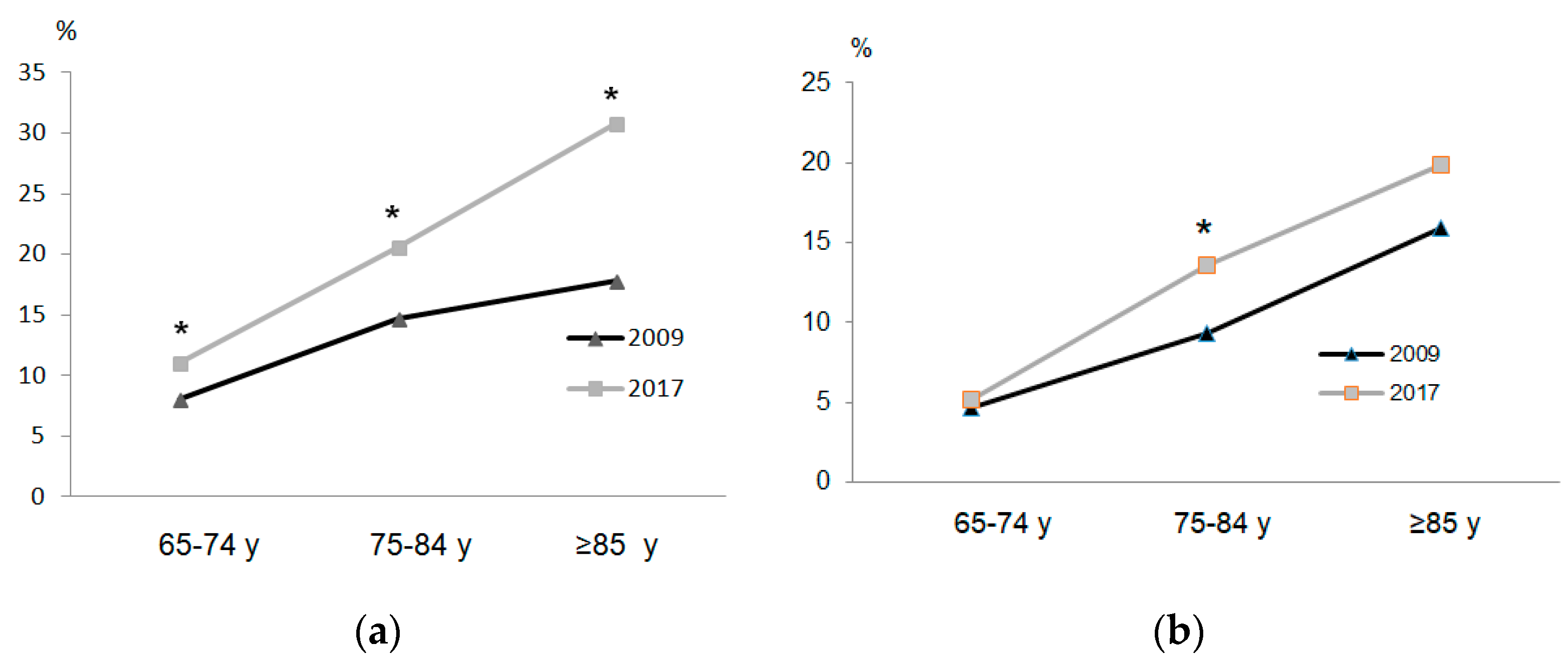
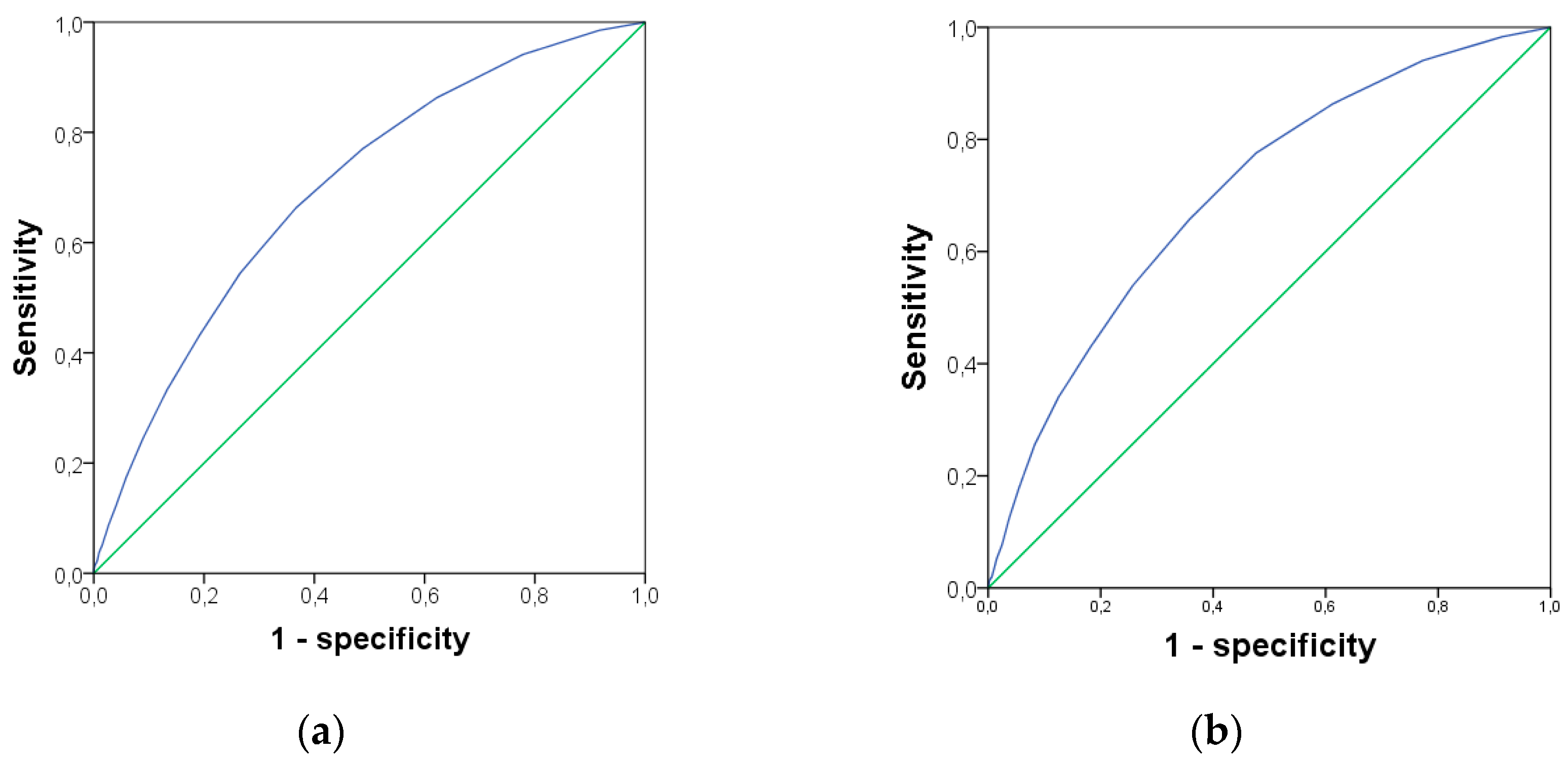
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- United Nations, Department of Economic and Social Affairs, P.D. World Population Ageing 2017—Highlights. Available online: https://www.un.org/en/development/desa/population/publications/pdf/ageing/WPA2017_Highlights.pdf (accessed on 15 June 2020).
- Landi, F.; Calvani, R.; Picca, A.; Tosato, M.; Martone, A.M.; D’Angelo, E.; Serafini, E.; Bernabei, R.; Marzetti, E. Impact of habitual physical activity and type of exercise on physical performance across ages in community-living people. PLoS ONE 2018, 13, e0191820. [Google Scholar] [CrossRef] [Green Version]
- INE. Esperanza de vida. Available online: https://www.ine.es/ (accessed on 21 January 2020).
- Vetrano, D.L.; Rizzuto, D.; Calderón-Larrañaga, A.; Onder, G.; Welmer, A.K.; Qiu, C.; Bernabei, R.; Marengoni, A.; Fratiglioni, L. Walking Speed Drives the Prognosis of Older Adults with Cardiovascular and Neuropsychiatric Multimorbidity. Am. J. Med. 2019, 132, 1207–1215. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Laredo-Aguilera, J.A.; Carmona-Torres, J.M.; García-Pinillos, F.; Latorre-Román, P.Á. Effects of a 10-week functional training programme on pain, mood state, depression, and sleep in healthy older adults. Psychogeriatrics 2018, 18, 292–298. [Google Scholar] [CrossRef] [PubMed]
- WHO. Technical Series on Safer Primary Care. Available online: https://www.who.int/patientsafety/topics/primary-care/technical_series/en/ (accessed on 16 June 2020).
- Jernigan, T.L.; Archibald, S.L.; Fennema-Notestine, C.; Gamst, A.C.; Stout, J.C.; Bonner, J.; Hesselink, J.R. Effects of age on tissues and regions of the cerebrum and cerebellum. Neurobiol. Aging 2001, 22, 581–594. [Google Scholar] [CrossRef] [Green Version]
- Wise, R.A. Dopamine, learning and motivation. Nat. Rev. Neurosci. 2004, 5, 483–494. [Google Scholar] [CrossRef] [PubMed]
- Rittweger, J.; Kwiet, A.; Felsenberg, D. Physical performance in aging elite athletes-Challenging the limits of Physiology. J. Musculoskelet. 2004, 4, 159–160. [Google Scholar]
- Casas Herrero, A.; Izquierdo, M. Ejercicio fisico como intervencion eficaz en el anciano fragil. An. Sist. Sanit. Navar. 2012, 35, 69–85. [Google Scholar] [CrossRef]
- Chodzko-Zajko, W.J.; Proctor, D.N.; Fiatarone Singh, M.A.; Minson, C.T.; Nigg, C.R.; Salem, G.J.; Skinner, J.S. American College of Sports Medicine position stand. Exercise and Physical Activity for Older Adults. Med. Sci. Sport. Exerc. 2009, 41, 1510–1530. [Google Scholar] [CrossRef]
- Guillet, C.; Boirie, Y. Insulin resistance: A contributing factor to age-related muscle mass loss? Diabetes Metab. 2005, 31, S20–S25. [Google Scholar] [CrossRef]
- Strait, J.B.; Lakatta, E.G. Aging-Associated Cardiovascular Changes and Their Relationship to Heart Failure. Heart Fail. Clin. 2012, 8, 143–164. [Google Scholar] [CrossRef] [Green Version]
- Nelson, M.; Rejeski, W.; Blair, S.; Duncan, P.; Judge, J.; King, A.; Macera, C.; Castaneda-Sceppa, C. Physical Activity and Public Health in Older Adults: Recommendation From the American College of Sports Medicine and the American Heart Association. Med. Sci. Sport. Exerc. 2007, 39, 1435–1445. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Klompstra, L.; Ekdahl, A.W.; Krevers, B.; Milberg, A.; Eckerblad, J. Factors related to health-related quality of life in older people with multimorbidity and high health care consumption over a two-year period. BMC Geriatr. 2019, 19, 187. [Google Scholar] [CrossRef] [PubMed]
- McPhee, J.S.; French, D.P.; Jackson, D.; Nazroo, J.; Pendleton, N.; Degens, H. Physical activity in older age: Perspectives for healthy ageing and frailty. Biogerontology 2016, 17, 567–580. [Google Scholar] [CrossRef]
- WHO. Global recommendations on physical activity for health. Available online: https://www.who.int/dietphysicalactivity/publications/9789241599979/en/ (accessed on 16 June 2020).
- Rosique-Esteban, N.; Babio, N.; Díaz-López, A.; Romaguera, D.; Alfredo Martínez, J.; Sanchez, V.M.; Schröder, H.; Estruch, R.; Vidal, J.; Buil-Cosiales, P.; et al. Leisure-time physical activity at moderate and high intensity is associated with parameters of body composition, muscle strength and sarcopenia in aged adults with obesity and metabolic syndrome from the PREDIMED-Plus study. Clin. Nutr. 2018, 38, 1324–1331. [Google Scholar] [CrossRef]
- Gianoudis, J.; Bailey, C.A.; Daly, R.M. Associations between sedentary behaviour and body composition, muscle function and sarcopenia in community-dwelling older adults. Osteoporos. Int. 2015, 26, 571–579. [Google Scholar] [CrossRef]
- Vásquez, E.; Batsis, J.; Germain, C. Impact of Obesity and Physical Activity on Functional Outcomes in the Elderly Data From NHANES 2005–2010. J. Aging 2014, 26, 1032–1046. [Google Scholar]
- WHO. Recomendaciones Mundiales sobre Actividad Física para la Salud. Available online: https://www.who.int/dietphysicalactivity/publications/9789241599979/es/ (accessed on 15 June 2020).
- Motl, R.W.; McAuley, E. Physical activity, disability, and quality of life in older adults. Phys. Med. Rehabil. Clin. N. Am. 2010, 21, 299–308. [Google Scholar] [CrossRef]
- Sherrington, C.; Whitney, J.C.; Lord, S.R.; Herbert, R.D.; Cumming, R.G.; Close, J.C.T. Effective exercise for the prevention of falls: A systematic review and meta-analysis. J. Am. Geriatr. Soc. 2008, 56, 2234–2243. [Google Scholar] [CrossRef]
- Wannamethee, S.G.; Shaper, A.G.; Walker, M. Changes in physical activity, mortality, and incidence of coronary heart disease in older men. Lancet 1998, 351, 1603–1608. [Google Scholar] [CrossRef]
- Vogel, T.; Brechat, P.H.; Leprêtre, P.M.; Kaltenbach, G.; Berthel, M.; Lonsdorfer, J. Health benefits of physical activity in older patients: A review. Int. J. Clin. Pract. 2009, 63, 303–320. [Google Scholar] [CrossRef]
- Enright, P.L.; McBurnie, M.A.; Bittner, V.; Tracy, R.P.; McNamara, R.; Arnold, A.; Newman, A.B. The 6-min Walk Test*. Chest 2003, 123, 387–398. [Google Scholar] [CrossRef] [PubMed]
- Maidan, I.; Nieuwhof, F.; Bernad-Elazari, H.; Reelick, M.F.; Bloem, B.R.; Giladi, N.; Deutsch, J.E.; Hausdorff, J.M.; Claassen, J.A.H.; Mirelman, A. The Role of the Frontal Lobe in Complex Walking among Patients with Parkinson’s Disease and Healthy Older Adults: An fNIRS Study. Neurorehabil. Neural. Repair 2016, 30, 963–971. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kikkert, L.H.J.; Vuillerme, N.; Van Campen, J.P.; Hortobágyi, T.; Lamoth, C.J. Walking ability to predict future cognitive decline in old adults: A scoping review. Ageing Res. Rev. 2016, 27, 1–14. [Google Scholar] [CrossRef]
- Graham, J.E.; Ostir, G.V.; Fisher, S.R.; Ottenbacher, K.J. Assessing walking speed in clinical research: A systematic review. J. Eval. Clin. Pract. 2008, 14, 552–562. [Google Scholar] [CrossRef]
- Latorre-Román, P.A.; Laredo-Aguilera, J.A.; García-Pinillos, F.; Soto-Hermoso, V.M.; Carmona-Torres, J.M. Physical activity, weight and functional limitations in elderly Spanish people: The National Health Survey (2009-2014). Eur. J. Public Health 2018, 28, 778–783. [Google Scholar] [CrossRef]
- Pirker, W.; Katzenschlager, R. Gait disorders in adults and the elderly: A clinical guide. Wien. Klin. Wochenschr. 2017, 129, 81–95. [Google Scholar] [CrossRef] [Green Version]
- Rubio Castañeda, F.J.; Tomás Aznar, C.; Muro Baquero, C. Medición de la actividad física en personas mayores de 65 años mediante el ipaq-e: Validez de contenido, fiabilidad y factores asociados. Rev. Esp. Salud Publica 2017, 91, e1–e12. [Google Scholar]
- Mantilla Toloza, S.C.; Gómez-Conesa, A. El Cuestionario Internacional de Actividad Física. Un instrumento adecuado en el seguimiento de la actividad física poblacional. Rev. Iberoam. Fisioter. y Kinesiol. 2007. [Google Scholar] [CrossRef]
- Ministerio de Sanidad Servicios Sociales e Igualdad. Instituto Nacional de Estadística European Health Survey in Spain EHSS 2009; Ministerio de Sanidad, Servicios Sociales e Igualdad: Madrid, Spain, 2010.
- Ministerio de Sanidad Servicios Sociales e Igualdad. Instituto Nacional de Estadística National Health Survey in Spain NHSS 2017; Ministerio de Sanidad, Servicios Sociales e Igualdad: Madrid, Spain, 2018.
- Ministerio de Sanidad Servicios Sociales e Igualdad. Instituto Nacional de Estadística European Health Survey in Spain EHSS 2014; Ministerio de Sanidad, Servicios Sociales e Igualdad: Madrid, Spain, 2015.
- WHO. Diet, nutrition and the prevention of chronic diseases. Available online: https://www.who.int/dietphysicalactivity/publications/trs916/en/ (accessed on 15 June 2020).
- Harvey, J.A.; Chastin, S.F.M.; Skelton, D.A. How sedentary are older people? A systematic review of the amount of sedentary behavior. J. Aging Phys. Act. 2015, 23, 471–487. [Google Scholar] [CrossRef]
- Mielgo-Ayuso, J.; Aparicio-Ugarriza, R.; Castillo, A.; Ruiz, E.; Ávila, J.M.; Aranceta-Batrina, J.; Gil, Á.; Ortega, R.M.; Serra-Majem, L.; Varela-Moreiras, G.; et al. Physical activity patterns of the spanish population are mostly determined by sex and age: Findings in the ANIBES study. PLoS One 2016. [Google Scholar] [CrossRef] [Green Version]
- Palacios-Cẽa, D.; Alonso-Blanco, C.; Jiménez-Garcia, R.; Hernández-Barrera, V.; Carrasco-Garrido, P.; Pilẽo-Martinez, E.; Fernández-De-Las-Pẽas, C. Time trends in leisure time physical activity and physical fitness in elderly people: 20 year follow-up of the Spanish population national health survey (1987–2006). BMC Public Health 2011. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sun, F.; Norman, I.J.; While, A.E. Physical activity in older people: A systematic review. BMC Public Health 2013, 13, 449. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Vestergaard, S.; Patel, K.V.; Bandinelli, S.; Ferrucci, L.; Guralnik, J.M. Characteristics of 400-m walk test performance and subsequent mortality in older adults. Rejuvenation Res. 2009, 12, 177–184. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ryan, A.; Murphy, C.; Boland, F.; Galvin, R.; Smith, S.M. What is the impact of physical activity and physical function on the development of multimorbidity in older adults over time? A population-based cohort study. Journals Gerontol.Ser. A Biol. Sci. Med. Sci. 2018. [Google Scholar] [CrossRef]
- Palladino, R.; Pennino, F.; Finbarr, M.; Millett, C.; Triassi, M. Multimorbidity and health outcomes in older adults in ten European health systems, 2006–2015. Health Aff. 2019. [Google Scholar] [CrossRef]
- Visser, M. Obesity, sarcopenia and their functional consequences in old age. Proc. Nutr. Soc. 2011, 70, 114–118. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Clark, B.C.; Manini, T.M. Sarcopenia ≠ dynapenia. J. Gerontol. A. Biol. Sci. Med. Sci. 2008, 63, 829–834. [Google Scholar] [CrossRef]
- Ogden, C.L.; Carroll, M.D.; Kit, B.K.; Flegal, K. M Prevalence of childhood and adult obesity in the United States, 2011–2012. JAMA 2014, 311, 806–814. [Google Scholar] [CrossRef] [Green Version]
- Bannerman, E.; Miller, M.D.; Daniels, L.A.; Cobiac, L.; Giles, L.C.; Whitehead, C.; Andrews, G.R.; Crotty, M. Anthropometric indices predict physical function and mobility in older Australians: The Australian Longitudinal Study of Ageing. Public Health Nutr. 2002, 5, 655–662. [Google Scholar] [CrossRef] [Green Version]
- Koster, A.; Penninx, B.W.J.H.; Newman, A.B.; Visser, M.; Van Gool, C.H.; Harris, T.B.; Van Eijk, J.T.M.; Kempen, G.I.J.M.; Brach, J.S.; Simonsick, E.M.; et al. Lifestyle factors and incident mobility limitation in obese and non-obese older adults. Obesity (Silver Spring) 2007, 15, 3122–3132. [Google Scholar] [CrossRef] [Green Version]
- Dhalwani, N.N.; O’Donovan, G.; Zaccardi, F.; Hamer, M.; Yates, T.; Davies, M.; Khunti, K. Long terms trends of multimorbidity and association with physical activity in older English population. Int. J. Behav. Nutr. Phys. Act. 2016, 13, 8. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jindai, K.; Nielson, C.M.; Vorderstrasse, B.A.; Quinones, A.R. Multimorbidity and Functional Limitations Among Adults 65 or Older, NHANES 2005-2012. Prev. Chronic Dis. 2016, 13, E151. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wassink-Vossen, S.; Collard, R.M.; Oude Voshaar, R.C.; Comijs, H.C.; De Vocht, H.M.; Naarding, P. Physical (in)activity and depression in older people. J. Affect. Disord. 2014. [Google Scholar] [CrossRef] [PubMed]
| Characteristics | 2009 | 2017 | p-Value | 2009 | 2017 | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n | All | n | All | n | Male | n | Female | n | Male | n | Female | ||
| Age (years) | 6026 | 75.61 (7.11) | 7023 | 76.01 (7.57) | 0.002 | 2330 | 74.83 (6.87) | 3696 | 76.11 (7.21) | 2850 | 74.85 (7.07) | 4173 | 76.81 (7.79) *** |
| Body mass (kg) | 5110 | 71.61 (12.43) | 6371 | 72.13 (13.06) | 0.031 | 2103 | 77.03 (11.70) | 3007 | 67.81 (11.49) | 2717 | 78.49 (11.89) *** | 3654 | 67.39 (11.82) |
| Body height (cm) | 5110 | 162.02 (8.49) | 6371 | 162.71 (8.42) | <0.001 | 2103 | 168.36 (6.92) | 3007 | 157.67 (6.47) | 2717 | 169.23 (6.54) *** | 3654 | 157.86 (6.51) |
| BMI (kg/m2) | 5110 | 27.25 (4.27) | 6371 | 27.21 (4.39) | 0.662 | 2103 | 27.17 (3.73) | 3007 | 27.31 (4.61) | 2717 | 27.39 (3.83) | 3654 | 27.08 (4.76) * |
| To walk (h/week) ≠ | 2133 | 7.11 (17.12) | 1372 | 1.28 (1.00) | <0.001 | 958 | 7.88 (5.99) | 1175 | 6.49 (22.41) | 626 | 1.43 (1.10) *** | 746 | 1.15 (0.90) *** |
| Moderate PA (h/week) ≠ | 2588 | 3.75 (6.67) | 405 | 1.32 (1.11) | <0.001 | 1101 | 2.94 (5.70) | 1487 | 4.36 (7.25) | 184 | 1.52 (1.34) ** | 221 | 1.14 (0.84) *** |
| Moderate PA (days/week) ǂ | 2600 | 2.16 (2.96) | 1704 | 0.94 (1.96) | <0.001 | 1108 | 1.91 (2.84) | 1492 | 2.35 (3.04) | 778 | 1.10 (2.19) *** | 926 | 0.82 (1.72) *** |
| Self-perceived health status (1–5) ǂ | 6026 | 2.86 (0.96) | 7023 | 2.70 (0.92) | <0.001 | 2330 | 2.68 (0.91) | 3696 | 2.97 (0.97) | 2850 | 2.56 (0.87) *** | 4173 | 2.79 (0.93) *** |
| Characteristics | 2009 | 2017 | 2009 | 2017 | |||
|---|---|---|---|---|---|---|---|
| All | All | Male | Female | Male | Female | ||
| Disease or chronic/long-lasting health problem (≥6 month) n (%) | Yes | 5028 (83.4) | 6493 (92.5) * | 1848 (79.3) | 3180 (86.0) | 2585 (90.7) * | 3908 (93.6) * |
| Difficulty walking 500 m without assistance n (%) | Severe difficulty | 490 (8.1) | 786 (11.2) * | 136 (5.8) | 354 (9.6) | 231 (8.1) * | 555 (13.3) * |
| Difficulty going up or down 12 stairs n (%) | Severe difficulty | 626 (10.4) | 1041 (14.8) * | 177 (7.6) | 449 (12.1) | 278 (9.8) * | 763 (18.3) * |
| Number of diseases; mean (SD) | 3.27 (2.55) | 5.06 (3.46) *** | 2.54 (2.14) | 3.73 (2.68) | 4.29 (3.01) *** | 5.58 (3.64) *** | |
| Characteristics | 2009 | 2017 | 2009 | 2017 | 2009 | 2017 | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 65–74 Years | 65–74 Years | 75–84 Years | 75–84 Years | ≥85 Years | ≥85 Years | |||||||
| Male n = 1206 | Female n = 1642 | Male n = 1549 | Female n = 1834 | Male n = 890 | Female n = 1537 | Male n = 979 | Female n = 1564 | Male n = 232 | Female n = 519 | Male n = 322 | Female n = 775 | |
| Age (year) mean (SD) | 69.37 (2.97) | 69.57 (3.01) | 69.41 (2.77) | 69.46 (2.83) | 78.78 (2.72) | 78.95 (2.77) | 79.13 (2.92) ** | 79.60 (2.80) *** | 88.09 (3.03) | 88.35 (3.21) | 87.99 (2.90) | 88.55 (3.31) |
| BMI (kg/m2) mean (SD) | 27.50 (3.71) | 27.53 (4.61) | 27.77 (4.00) | 27.22 (4.83) * | 26.98 (3.71) | 27.44 (4.60) | 27.18 (3.55) | 27.26 (4.66) | 25.96 (3.66) | 26.05 (4.47) | 26.04 (3.41) | 26.29 (4.75) |
| Disease or chronic/long-lasting health problems (≥6month) Yes (%) | 915 (75.7) | 1356 (82.7) | 1367 (88.3) *** | 1664 (90.7) *** | 737 (82.8) | 1361 (88.5) | 917 (93.7) *** | 1497 (95.7) *** | 196 (84.5) | 463 (89.2) | 301 (93.5) ** | 747 (96.4) *** |
| Number of diseases; mean (SD) | 2.26 (1.96) | 3.61 (2.75) | 3.87 (2.91) *** | 4.95 (3.54) *** | 2.74 (2.18) | 3.83 (2.64) | 4.69 (3.01) *** | 6.16 (3.71) *** | 3.20 (2.57) | 3.80 (2.54) | 5.09 (3.17) *** | 5.59 (3.48) *** |
| Self-perceived health status (1–5) ǂ mean (SD) | 2.54 (0.87) | 2.84 (0.97) | 2.41 (0.82) *** | 2.60 (0.89) *** | 2.78 (0.92) | 3.05 (0.97) | 2.73 (0.88) | 2.92 (0.92) *** | 3.01 (0.97) | 3.12 (0.97) | 2.82 (0.92) * | 2.97 (0.96) ** |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Latorre-Román, P.Á.; Carmona-Torres, J.M.; Cobo-Cuenca, A.I.; Laredo-Aguilera, J.A. Physical Activity, Ability to Walk, Weight Status, and Multimorbidity Levels in Older Spanish People: The National Health Survey (2009–2017). Int. J. Environ. Res. Public Health 2020, 17, 4333. https://doi.org/10.3390/ijerph17124333
Latorre-Román PÁ, Carmona-Torres JM, Cobo-Cuenca AI, Laredo-Aguilera JA. Physical Activity, Ability to Walk, Weight Status, and Multimorbidity Levels in Older Spanish People: The National Health Survey (2009–2017). International Journal of Environmental Research and Public Health. 2020; 17(12):4333. https://doi.org/10.3390/ijerph17124333
Chicago/Turabian StyleLatorre-Román, Pedro Ángel, Juan Manuel Carmona-Torres, Ana Isabel Cobo-Cuenca, and José Alberto Laredo-Aguilera. 2020. "Physical Activity, Ability to Walk, Weight Status, and Multimorbidity Levels in Older Spanish People: The National Health Survey (2009–2017)" International Journal of Environmental Research and Public Health 17, no. 12: 4333. https://doi.org/10.3390/ijerph17124333







