Smartphone-Based Health Program for Improving Physical Activity and Tackling Obesity for Young Adults: A Systematic Review and Meta-Analysis
Abstract
1. Introduction
2. Methods
2.1. Search Strategy
2.2. Inclusion Criteria
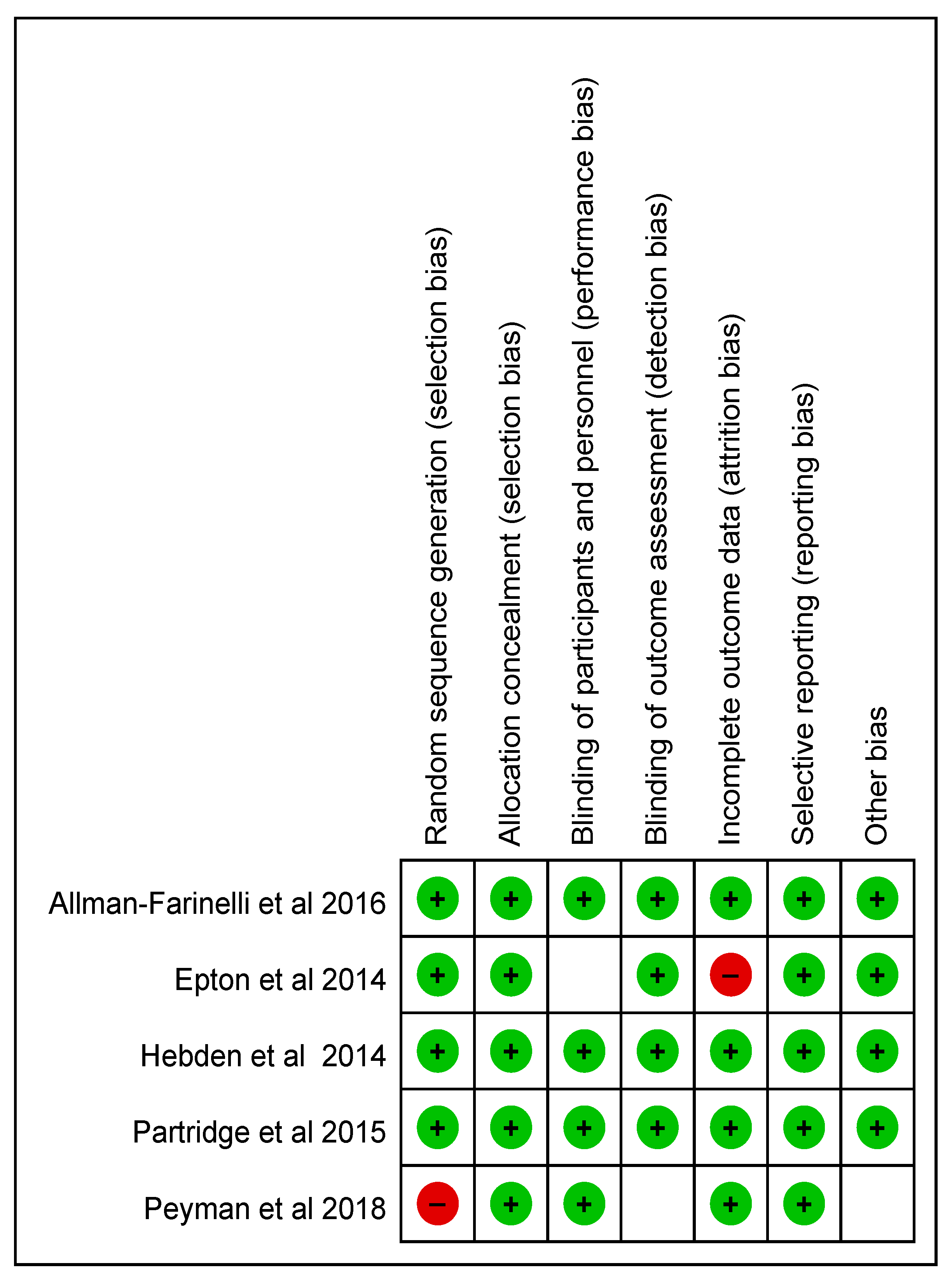
2.3. Risk of Bias Appraisal
2.4. Data Extraction and Synthesis
2.5. Statistical Analysis
3. Results
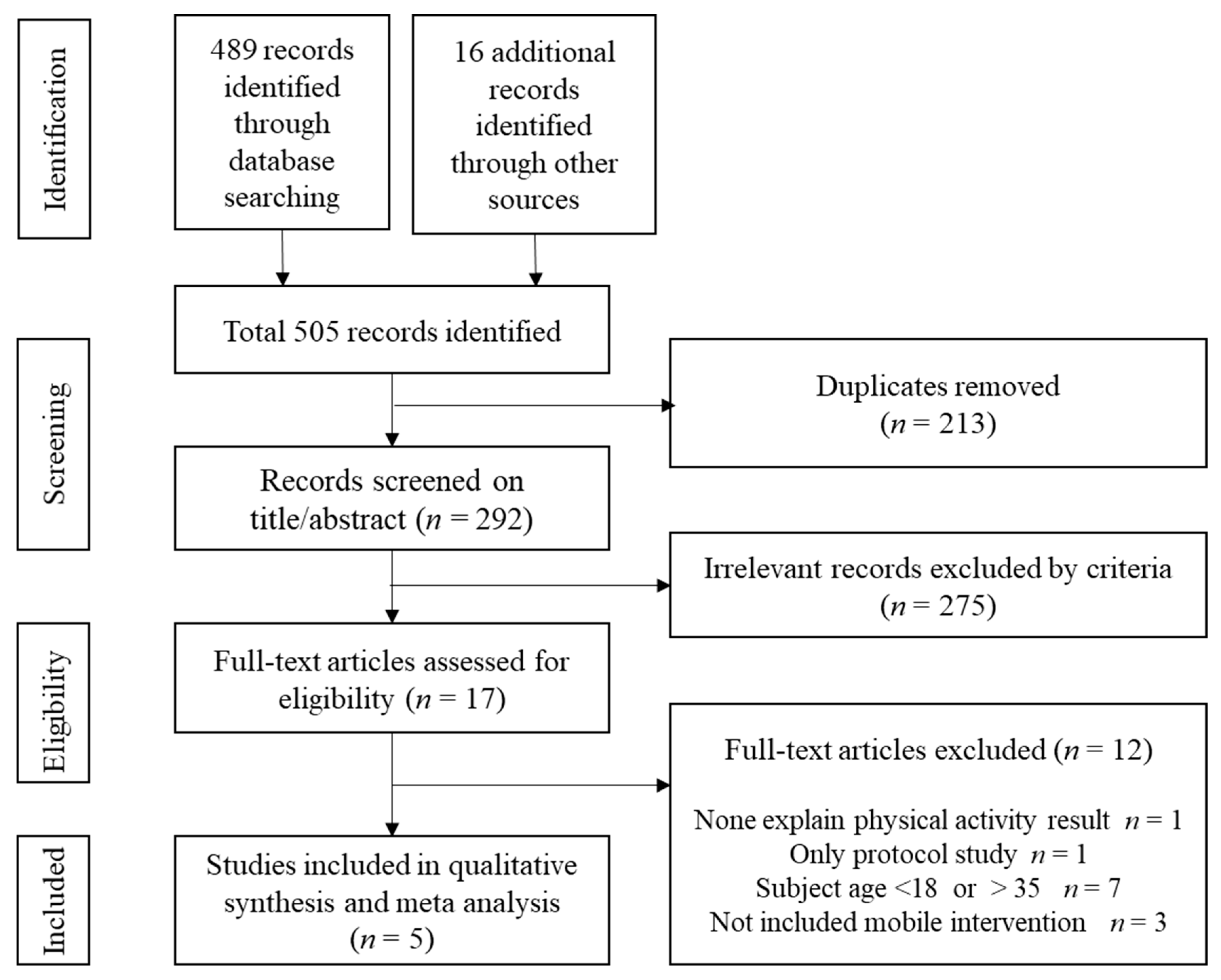
3.1. Search Outcomes
3.2. Characteristics of Included Studies
3.3. Data Extraction from Systematic Review
3.3.1. Participants
3.3.2. Program Contents Provided to Intervention and Control Groups
3.3.3. Outcomes
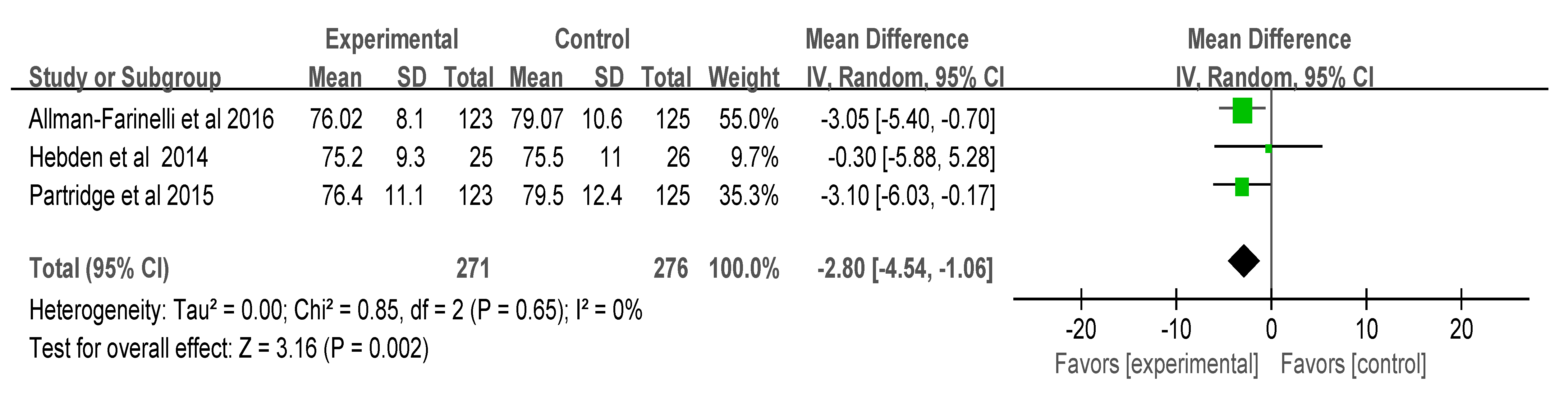
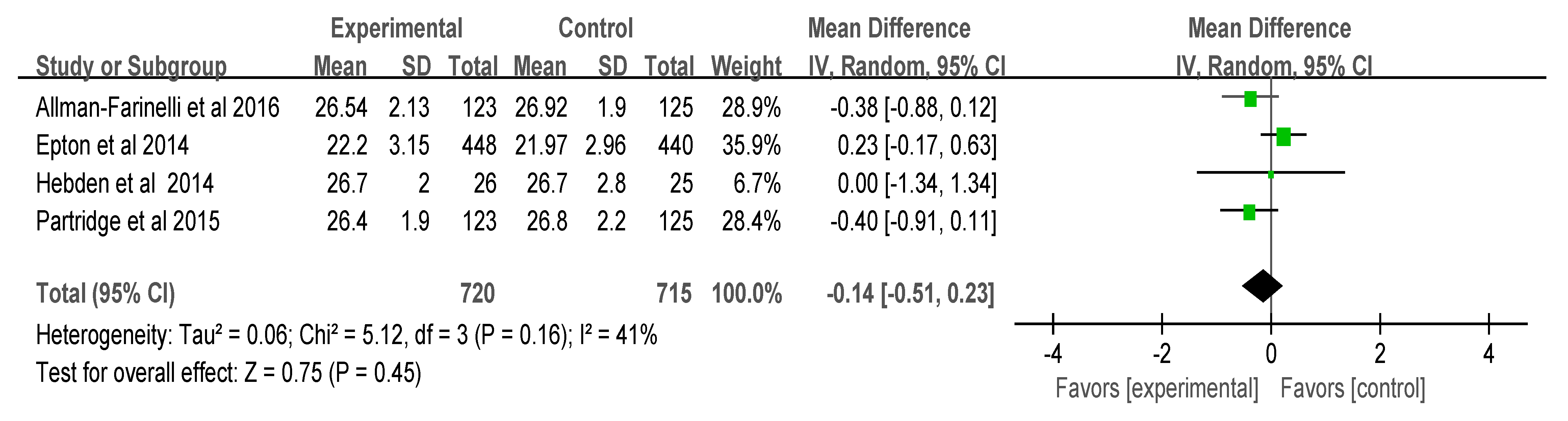
3.4. Meta-Analysis of the Results
4. Discussion
Limitations of This Study
5. Conclusions
Author Contributions
Acknowledgments
Conflicts of Interest
References
- Hagströmer, M.; Troiano, R.P.; Sjöström, M.; Berrigan, D. Levels and patterns of objectively assessed physical activity: A comparison between Sweden and the United States. Am. J. Epidemiol. 2010, 171, 1055–1106. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Global Recommendations on Physical Activity for Health. Available online: https://www.who.int/dietphysicalactivity/publications/9789241599979/en/ (accessed on 20 April 2019).
- Zhang, D.; Liu, X.; Liu, Y.; Sun, X.; Wang, B.; Ren, Y.; Zhao, Y.; Zhou, J.; Han, C.; Yin, L.; et al. Leisure-time physical activity and incident metabolic syndrome: A systematic review and dose-response meta-analysis of cohort studies. Metabolism 2017, 75, 36–44. [Google Scholar] [CrossRef] [PubMed]
- Harari, G.M.; Müller, S.R.; Mishra, V.; Wang, R.; Campbell, A.T.; Rentfrow, P.J.; Gosling, S.D. An evaluation of students’ interest in and compliance with self-tracking methods: Recommendations for incentives based on three smartphone sensing studies. Soc. Psychol. Personal. Sci. 2017, 8, 479–492. [Google Scholar] [CrossRef]
- Bort-Roig, J.; Gilson, N.D.; Puig-Ribera, A.; Contreras, R.S.; Trost, S.G. Measuring and influencing physical activity with smartphone technology: A systematic review. Sports Med. 2014, 44, 671–686. [Google Scholar] [CrossRef] [PubMed]
- Lewis, B.A.; Napolitano, M.A.; Buman, M.P.; Williams, D.M.; Nigg, C.R. Future directions in physical activity intervention research: Expanding our focus to sedentary behaviors, technology, and dissemination. J. Behav. Med. 2017, 40, 112–126. [Google Scholar] [CrossRef] [PubMed]
- Schumann, A.; Nigg, C.R.; Rossi, J.S.; Jordan, P.J.; Norman, G.J.; Garber, C.E.; Riebe, D.; Benisovich, S.V. Construct validity of the stages of change of exercise adoption for different intensities of physical activity in four samples of differing age groups. Am. J. Health Promot. 2002, 16, 280–287. [Google Scholar] [CrossRef]
- Katz, D.L.; O’Connell, M.; Yeh, M.C.; Nawaz, H.; Njike, V.; Anderson, L.; Cory, S.; Dietz, W. Public health strategies for preventing and controlling overweight and obesity in school and worksite settings: A report on recommendations of the Task Force on Community Preventive Services. Morb. Mortal. Wkly. Rep. Recomm. Rep. 2005, 54, 1–12. [Google Scholar]
- Anderson, L.M.; Quinn, T.A.; Glanz, K.; Ramirez, G.; Kahwati, L.C.; Johnson, D.B.; Buchanan, L.R.; Archer, W.R.; Chattopadhyay, S.; Kalra, G.P.; et al. The effectiveness of worksite nutrition and physical activity interventions for controlling employee overweight and obesity: A systematic review. Am. J. Prev. Med. 2009, 37, 340–357. [Google Scholar] [CrossRef]
- Fedele, D.A.; Cushing, C.C.; Fritz, A.; Amaro, C.M.; Ortega, A. Mobile health interventions for improving health outcomes in youth: A meta-analysis. JAMA Pediatr. 2017, 171, 461–469. [Google Scholar] [CrossRef]
- Kim, Y.-J. Exploratory study on acceptance intention of mobile devices and applications for healthcare services. J. Korea Contents Assoc. 2012, 12, 369–379. [Google Scholar] [CrossRef]
- Hannan, A.L.; Harders, M.P.; Hing, W.; Climstein, M.; Coombes, J.S.; Furness, J. Impact of wearable physical activity monitoring devices with exercise prescription or advice in the maintenance phase of cardiac rehabilitation: Systematic review and meta-analysis. BMC Sports Sci. Med. Rehabil. 2019, 11, 14. [Google Scholar] [CrossRef] [PubMed]
- Jong, S.; Cuca, Y.; Thompson, L.M. Meta-analysis of mobile phone reminders on HIV patients’ retention to care. J. Mob. Technol. Med. 2017, 6, 5–18. [Google Scholar] [CrossRef] [PubMed]
- Bailey, D.P.; Hewson, D.J.; Champion, R.B.; Sayegh, S. Sitting time and risk of cardiovascular disease and diabetes: A systematic review and meta-analysis. Am. J. Prev. Med. 2019, 57, 408–416. [Google Scholar] [CrossRef] [PubMed]
- Fanning, J.; Mullen, S.P.; McAuley, E. Increasing physical activity with mobile devices: A meta-analysis. J. Med. Internet Res. 2012, 14, e161. [Google Scholar] [CrossRef]
- Liberati, A.; Altman, D.G.; Tetzlaff, J.; Mulrow, C.; Gøtzsche, P.C.; Ioannidis, J.P.; Clarke, M.; Devereaux, P.J.; Kleijnen, J.; Moher, D. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: Explanation and elaboration. PLoS Med. 2009, 6, e1000100. [Google Scholar] [CrossRef]
- Higgins, J.P.; Altman, D.G.; Gøtzsche, P.C.; Jüni, P.; Moher, D.; Oxman, A.D.; Savović, J.; Schulz, K.F.; Weeks, L.; Sterne, J.A. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ 2011, 343, d5928. [Google Scholar] [CrossRef]
- Altman, D.G.; Bland, J.M. How to obtain the confidence interval from a P value. BMJ 2011, 343. [Google Scholar] [CrossRef]
- Hebden, L.; Cook, A.; Van Der Ploeg, H.P.; King, L.; Bauman, A.; Allman-Farinelli, M. A mobile health intervention for weight management among young adults: A pilot randomised controlled trial. J. Hum. Nutr. Diet. 2014, 27, 322–332. [Google Scholar] [CrossRef]
- Allman-Farinelli, M.; Partridge, S.R.; McGeechan, K.; Balestracci, K.; Hebden, L.; Wong, A.; Phongsavan, P.; Denney-Wilson, E.; Harris, M.F.; Bauman, A. A mobile health lifestyle program for prevention of weight gain in young adults (TXT2BFiT): Nine-month outcomes of a randomized controlled trial. JMIR Mhealth Uhealth 2016, 4, e78. [Google Scholar] [CrossRef]
- Epton, T.; Norman, P.; Dadzie, A.S.; Harris, P.R.; Webb, T.L.; Sheeran, P.; Naughton, D. A theory-based online health behaviour intervention for new university students (U@ Uni): Results from a randomised controlled trial. BMC Public Health 2014, 14, 563. [Google Scholar] [CrossRef]
- Peyman, N.; Rezai-Rad, M.; Tehrani, H.; Gholian-Aval, M.; Vahedian-Shahroodi, M.; Miri, H.H. Digital Media-based Health Intervention on the promotion of Women’s physical activity: A quasi-experimental study. BMC Public Health 2018, 18, 134. [Google Scholar] [CrossRef] [PubMed]
- Partridge, S.R.; McGeechan, K.; Hebden, L.; Balestracci, K.; Wong, A.T.; Denney-Wilson, E.; Harris, M.F.; Phongsavan, P.; Bauman, A.; Allman-Farinelli, M. Effectiveness of a mHealth lifestyle program with telephone support (TXT2BFiT) to prevent unhealthy weight gain in young adults: Randomized controlled trial. JMIR Mhealth Uhealth 2015, 3, e66. [Google Scholar] [CrossRef] [PubMed]
- Prochaska, J.O.; Diclemente, C.C. Stages and Processes of Self-Change of Smoking-toward an Integrative Model of Change. J. Consult. Clin. Psychol. 1983, 51, 390–395. [Google Scholar] [CrossRef] [PubMed]
- Ajzen, I. From intentions to actions: A theory of planned behavior. In Action Control; Springer: Berlin\Heidelberg, Germany, 1985; pp. 11–39. [Google Scholar]
- Deeks, J.J.; Higgins, J.P.T.; Altman, D.G.; on behalf of the Cochrane Statistical Methods Group. Analysing data and undertaking meta-analyses. In Cochrane Handbook for Systematic Reviews of Interventions; Higgins, J.P.T., Thomas, J., Chandler, J., Cumpston, M., Li, T., Page, M.J., Welch, V.A., Eds.; Cochrane: London, UK, 2019; Available online: www.training.cochrane.org/handbook (accessed on 20 May 2019).
- Direito, A.; Carraça, E.; Rawstorn, J.C.; Whittaker, R.; Maddison, R. mHealth technologies to influence physical activity and sedentary behaviors: Behavior change techniques, systematic review and meta-analysis of randomized controlled trials. Ann. Behav. Med. 2016, 51, 226–239. [Google Scholar] [CrossRef]
- Carter, D.D.; Robinson, K.; Forbes, J.; Hayes, S. Experience of mobile health in promoting physical activity: A qualitative systematic review and meta-ethnography. PLoS ONE 2018, 13, e0208759. [Google Scholar] [CrossRef]
- Stuckey, M.I.; Carter, S.W.; Knight, E. The role of smartphones in encouraging physical activity in adults. Int. J. Gen. Med. 2017, 10, 293–303. [Google Scholar] [CrossRef]
- Booth, M. Assessment of physical activity: An International perspective. Res. Q. Exer. Sport 2000, 71, 114–120. [Google Scholar] [CrossRef]
- Moy, K.; McFarlane, K.; Scragg, R.; Robinson, S. Validation of MOH-Short and SPARC-long Physical Activity Questionnaires; Sport and Recreation New Zealand (SPARC): Wellington, NZ, USA, 2003; pp. 1–142. [Google Scholar]
- Allman-Farinelli, M.A. Nutrition Promotion to prevent obesity in young adults. Healthcare 2015, 3, 809–821. [Google Scholar] [CrossRef]
- Flores Mateo, G.; Granado-Font, E.; Ferré-Grau, C.; Montaña-Carreras, X. Mobile phone apps to promote weight loss and increase physical activity: A systematic review and meta-analysis. J. Med. Internet Res. 2015, 17, e253. [Google Scholar] [CrossRef]
- Pagoto, S.; Schneider, K.L.; Jojic, M.; DeBiasse, M.A.; Mann, D.M. Evidence-based strategies in weight-loss mobile apps. Am. J. Prev. Med. 2013, 45, 576–582. [Google Scholar] [CrossRef]
- Kim, J.Y.; Wineinger, N.E.; Taitel, M.; Radin, M.; Akinbosoye, O.; Jiang, J.; Nikzad, N.; Orr, G.; Topol, E.; Steinhubl, S. Self-monitoring utilization patterns among individuals in an incentivized program for healthy behaviors. J. Med. Internet Res. 2016, 18, e292. [Google Scholar] [CrossRef] [PubMed]

| First Author (Published Year) | Study Design | Participants | Sample Size (I, C); Mean Age (Years) | Experimental Condition | Control Intervention | Follow Up | Measured Outcomes (Significant Outcomes) | ||
|---|---|---|---|---|---|---|---|---|---|
| Program Context | Application | Session/Duration | |||||||
| Allman-Farinelli et al. (2016) | Two-arm, parallel, RCT | Overweight over 18–35 year olds with a BMI ≥ 23 kg/m2. | 248 (I = 123, C = 125); 28.1, 27.2 | 12 weeks multicomponent diet program and 60 min physical activity; 5 coaching calls with motivational interviewing, personalized text messages, nutrition booklet with physical activity guidelines through web and apps. | Study website and mobile phone app | 12 weeks + 2 booster session at 5 months and 8 months | 12 weeks, minimal intervention with 4 text messages, 2-page handout based on the dietary guidelines and physical activity guidelines | 9 months | Weight (kg), BMI, physical activity (MET-minutes), and diet behaviors (intake of fruits, vegetables, SSBs, and take-out meals) |
| Hebden et al. (2014) | Two-arm, parallel, RCT | University students and staff | 51 (I = 26, C = 25); 22.6, 23.1 | Printed diet booklet with instructions. Text messages and email; had access to smartphone applications and Internet forums. | Mobile phone app | 12 weeks | Printed diet booklet with instructions | 13 weeks | Physical activity (IPAQ), BMI, usual weekly intake of SSB and energy-dense takeaway meals, and daily intake of fruit and vegetables |
| Epton et al. (2014) | Two arm, RCT | University students | 1107 (I = 549, C = 558); 18.7, 19.0 | Theory-based persuasive messages were developed to encourage regular exercise and fruit and vegetable intake, and to discourage binge drinking and smoking. Includes a mixture of text and video links to other relevant material. | Smartphone app | 6 months | none | 6 months | Smoking rates, physical activity, alcohol or fruit and vegetable consumption. Biochemical measures: A hair sample was taken to assess alcohol consumption, cigarette smoking, and recreational drug use. |
| Partridge et al. (2015) | Two-arm, parallel, RCT | Medicare locals; 18 to 35 year olds with a BMI of 23.0 to 24.9 kg/m2 | 241 (I = 110, C = 104); 28.1, 27.2 | 8 text messages and 1 email weekly, 5 personalized coaching calls, a diet booklet, and access to resources and mobile phone apps on a website. >TXT2BFiT | Mobile phone apps on a website | 12 weeks | 4 text messages and printed dietary and physical activity guidelines | 12 weeks | Self-reported weight and dietary intake of vegetables, sugary soft drinks, energy-dense takeout meals and physical activity (MET-minutes). |
| Peyman et al. (2018) | Quasi | Women visitors in health centers; older than 18 years and overweight. | 360 (I = 180, C = 180); 31.9, 33.4. | Educational website related to physical activity including film, video, video clips, educational material, CD, self-monitoring program, text messages daily | Web-based media, mobile phone. | 2 months | None | 6 months | IPAQ, mean score of knowledge, attitude, level of physical activity, MET-minutes/week, BMI. |
| First Authors (Published Year) | Study Design | Health Behavior Change Theory | Measurement of PA | Tool | Analysis |
|---|---|---|---|---|---|
| Allman-Farinelli et al. (2016) | Two-arm, parallel, RCT | Transtheoretical model | IPAQ (MET-minutes) | Questionnaire | Change in frequency (days) and minutes |
| Hebden et al. (2014) | Two-arm, parallel, RCT | Transtheoretical model | IPAQ (MET-minutes), daily step counts | Questionnaire, actigraph accelerometer | MVPA, light PA, total PA (minutes per week, MET-minutes /week), sitting time, sedentary time. Vigorous (>5738 counts per minute), moderate (1952–5737 counts per minute), light (101–1951 counts per minute) and sedentary (≤100 counts per minute) activities |
| Epton et al. (2014) | Two-arm, RCT | Theory of Planned Behaviors, self-efficacy | IPAQ-SF | Questionnaire in the past 7 days | Total MET and sitting mean hours |
| Partridge et al. (2015) | Two-arm, parallel, RCT | Transtheoretical model | IPAQ (MET-minutes) | Vigorous PA (MET-minutes per week, days per week), walking, moderate PA, total PA | |
| Peyman et al. (2018) | Quasi | None | IPAQ | Questionnaire | Total MET-minutes/week. |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kim, H.-N.; Seo, K. Smartphone-Based Health Program for Improving Physical Activity and Tackling Obesity for Young Adults: A Systematic Review and Meta-Analysis. Int. J. Environ. Res. Public Health 2020, 17, 15. https://doi.org/10.3390/ijerph17010015
Kim H-N, Seo K. Smartphone-Based Health Program for Improving Physical Activity and Tackling Obesity for Young Adults: A Systematic Review and Meta-Analysis. International Journal of Environmental Research and Public Health. 2020; 17(1):15. https://doi.org/10.3390/ijerph17010015
Chicago/Turabian StyleKim, Han-Na, and Kyoungsan Seo. 2020. "Smartphone-Based Health Program for Improving Physical Activity and Tackling Obesity for Young Adults: A Systematic Review and Meta-Analysis" International Journal of Environmental Research and Public Health 17, no. 1: 15. https://doi.org/10.3390/ijerph17010015
APA StyleKim, H.-N., & Seo, K. (2020). Smartphone-Based Health Program for Improving Physical Activity and Tackling Obesity for Young Adults: A Systematic Review and Meta-Analysis. International Journal of Environmental Research and Public Health, 17(1), 15. https://doi.org/10.3390/ijerph17010015





