A Multiple Streams Approach to Understanding the Issues and Challenges of Lyme Disease Management in Canada’s Maritime Provinces
Abstract
1. Introduction
1.1. Current Scholarship Surrounding Lyme Disease
1.1.1. The Academic Scholarship
Expansion of Ticks in Canada
Diagnosis
General Physician Knowledge
Treatment
1.1.2. The Grey Scholarship
Media Sources
Government Documents
2. Materials and Methods
2.1. Terminology
2.2. Survey Development and Administration
2.3. Participant Identification
2.4. Response Rates
3. Results and Discussion
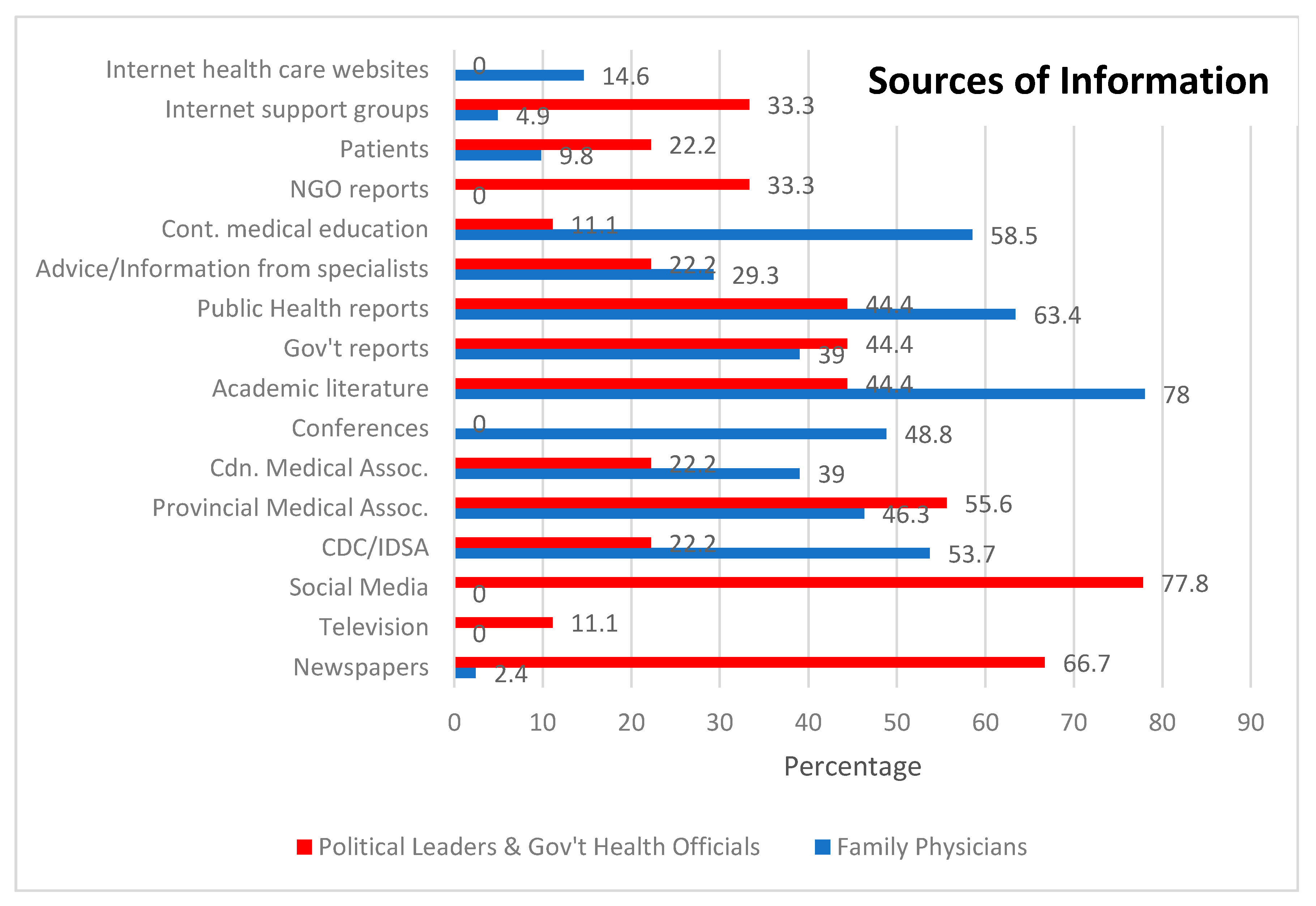
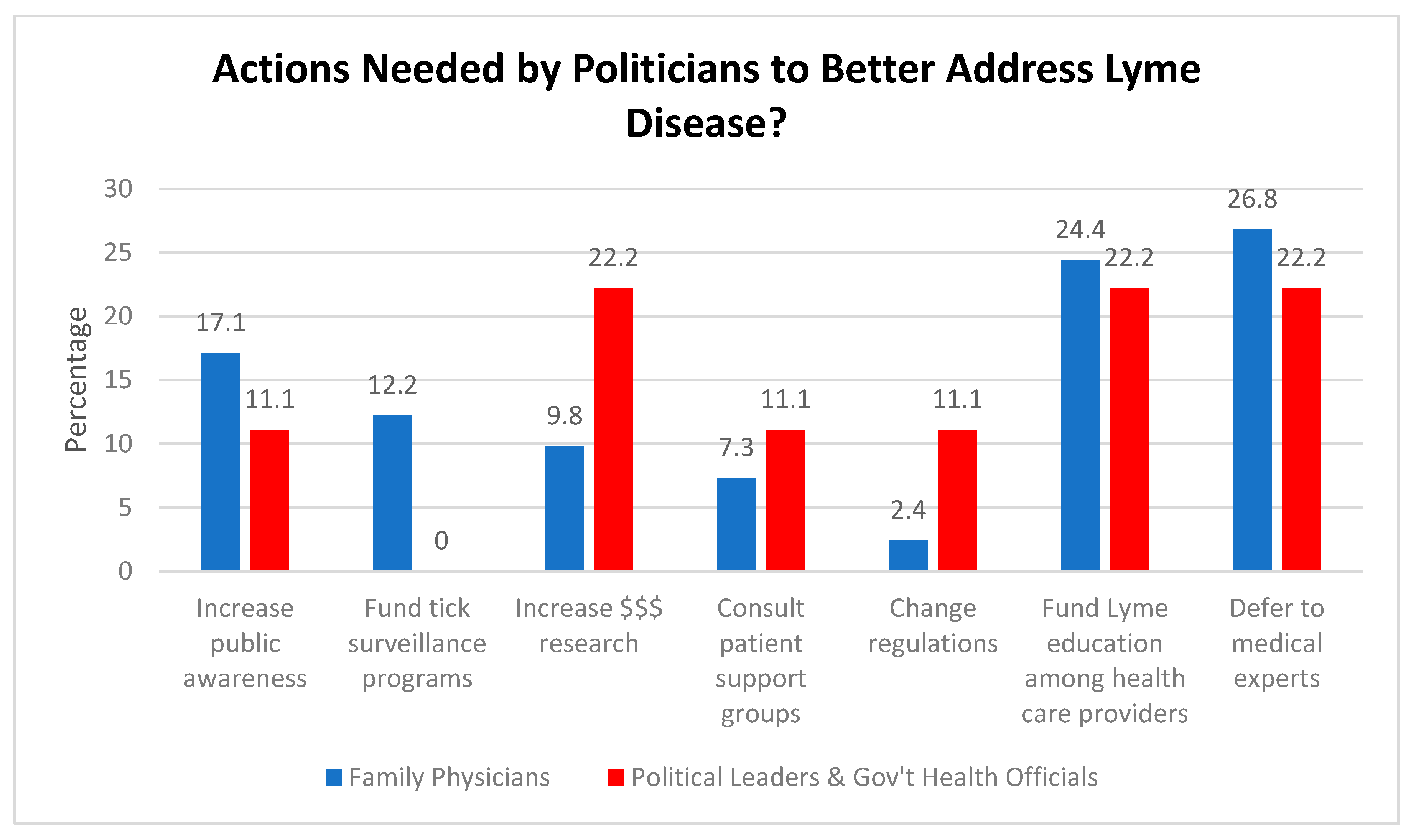
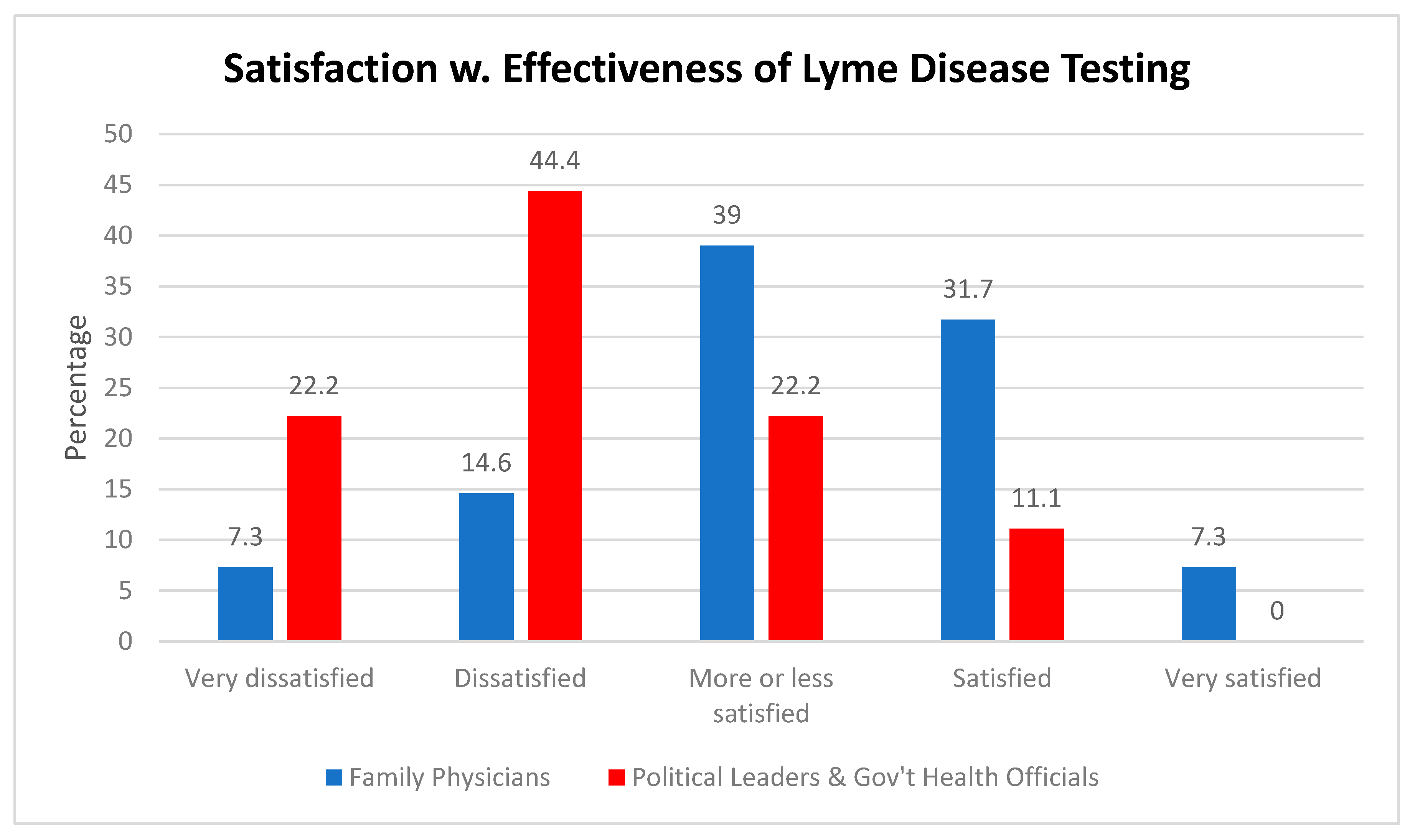
3.1. Key Points from the Surveys
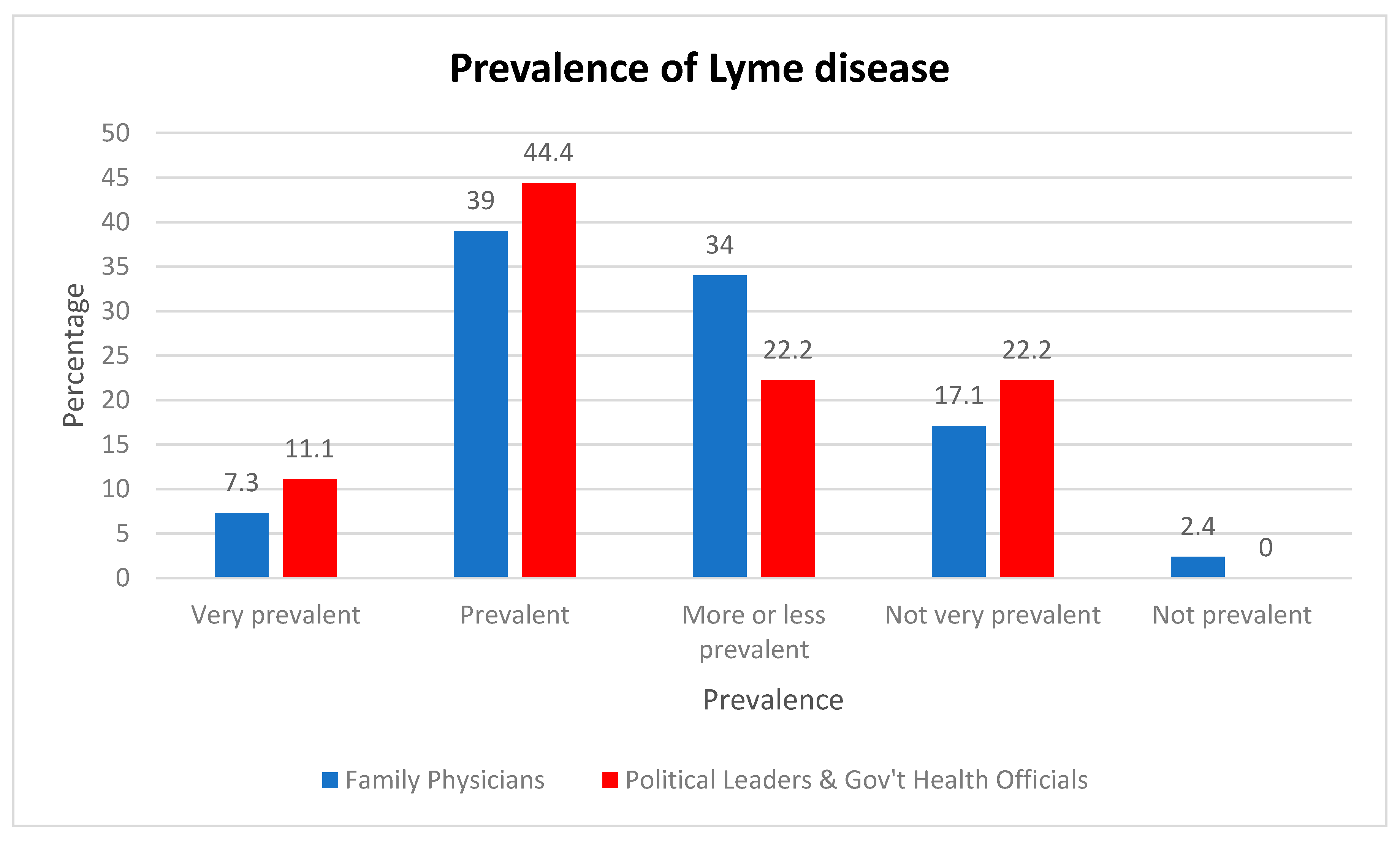
3.1.1. Prevalence of Lyme Disease
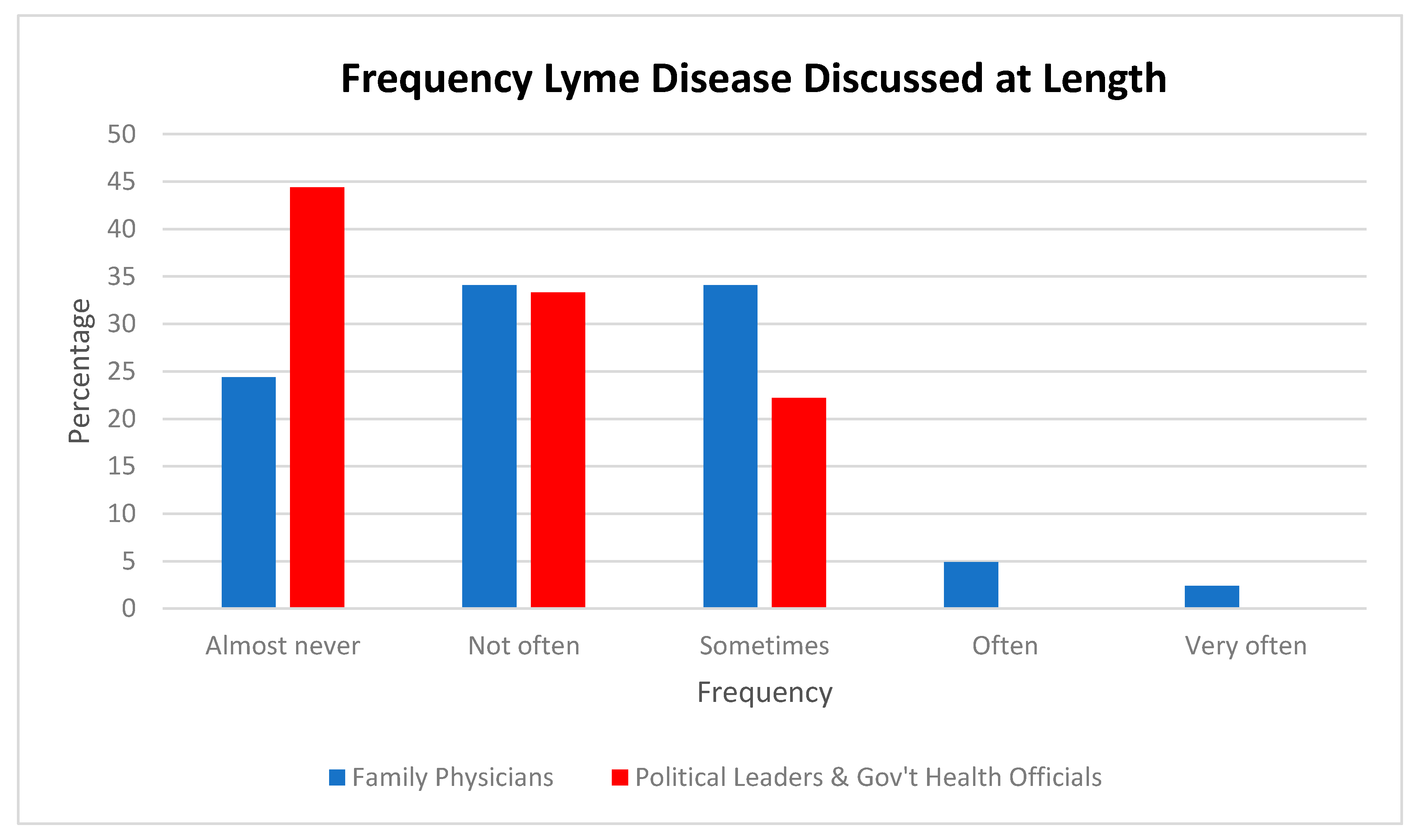
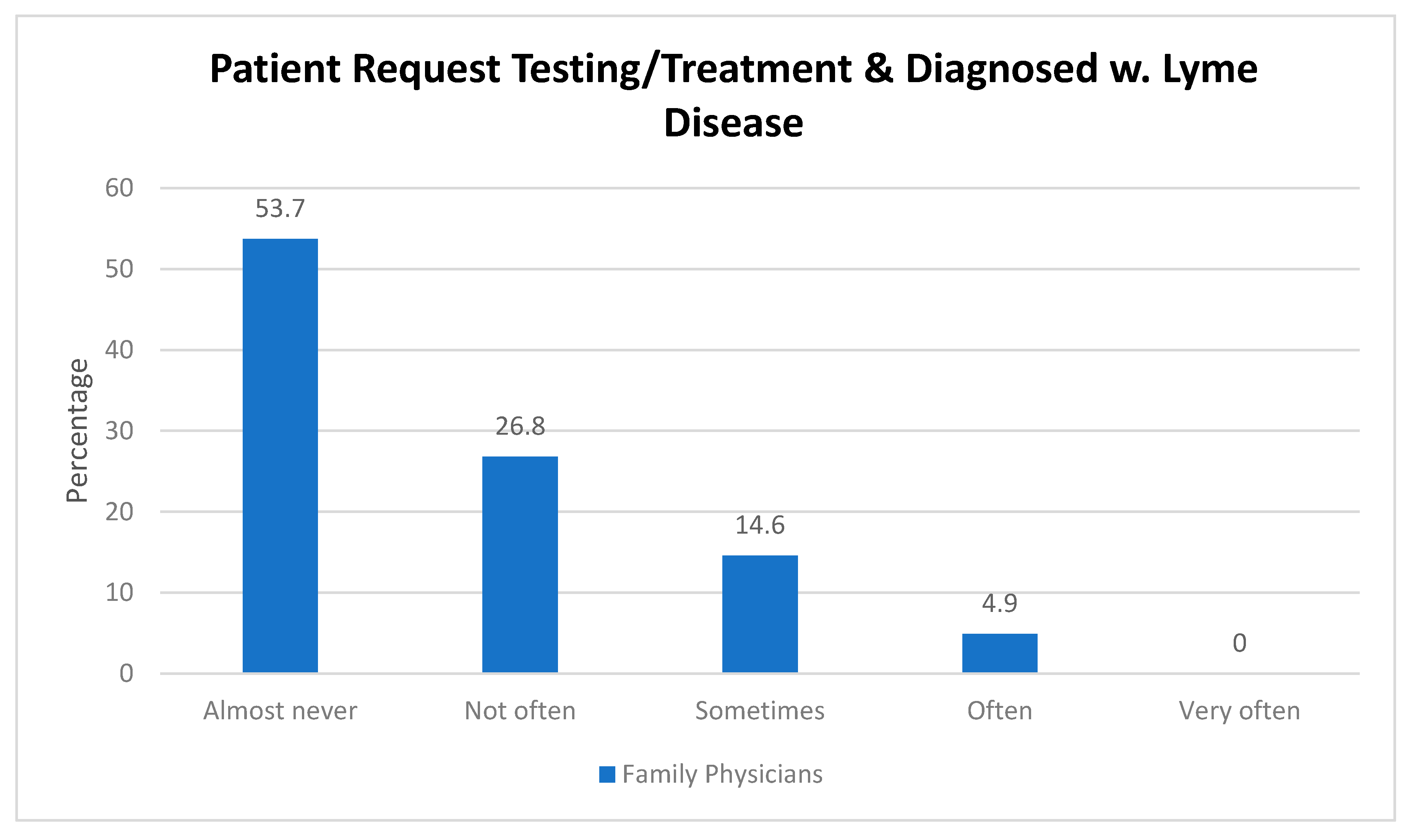
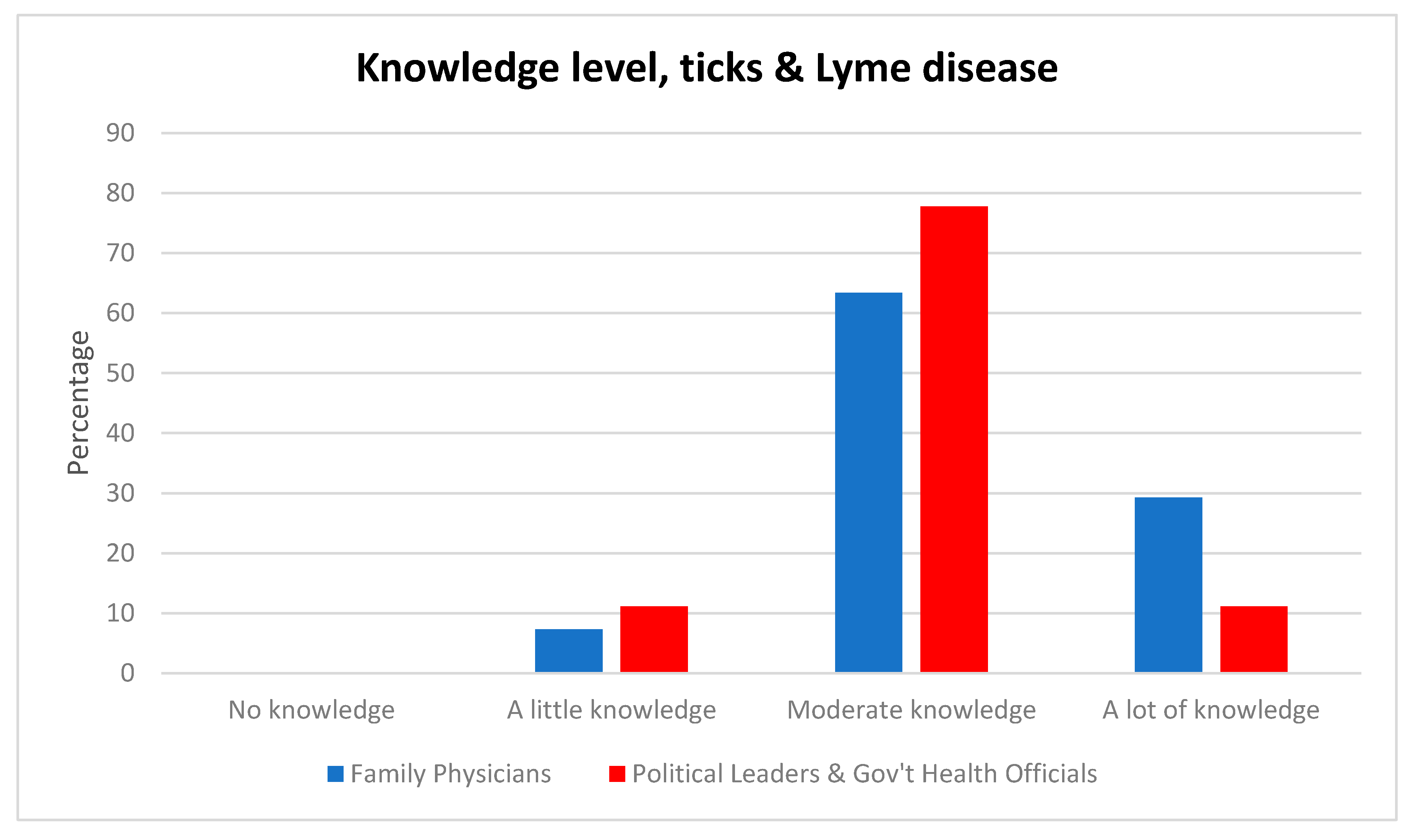
3.1.2. Knowledge of Lyme Disease
3.1.3. Government Actions
3.2. Challenges Identified
3.3. The Politics of Lyme Disease
4. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Appendix A


References
- Ogden, N.L.; Lindsay, R.; Morshed, M.; Sockett, P.N.; Artsob, H. The emergence of Lyme disease in Canada. CMAJ 2009, 180, 1221–1224. [Google Scholar] [CrossRef]
- Russell, N. P.E.I. Woman Finds Lyme Disease Diagnosis South of the Border. Available online: https://www.cbc.ca/news/canada/prince-edward-island/pei-lyme-disease-savannah-1.5048459 (accessed on 11 March 2019).
- N.S. Man Angry After Lyme Disease Medications Seized at Border. Available online: https://www.ctvnews.ca/canada/n-s-man-angry-after-lyme-disease-medications-seized-at-border-1.3472905 (accessed on 10 August 2018).
- Gregson, D.; Evans, G.; Patrick, D.; Bowie, W. Lyme disease: How reliable are serologic results. CMAJ 2015, 187, 1193–1194. [Google Scholar] [CrossRef]
- Leighton, P.A.; Koffi, J.K.; Pelcat, Y.; Lindsay, L.R.; Ogden, N.H. Predicting the speed of tick invasion: An empirical model of range expansion for the Lyme disease vector Ixodes scapularis in Canada. J. App. Ecol. 2012, 49, 457–464. [Google Scholar] [CrossRef]
- Centers for Disease Control and Prevention. How Many People Get Lyme Disease? Available online: https://www.cdc.gov/lyme/stats/humancases.html (accessed on 18 March 2019).
- Centers for Disease Control and Prevention. Lyme Disease Maps. Available online: https://www.cdc.gov/lyme/stats/maps.html (accessed on 21 May 2018).
- Gasmi, S.; Ogden, N.H.; Lindsay, L.R.; Burns, S.; Fleming, S.; Badcock, J.; Hanan, S.; Gaulin, C.; Leblanc, M.A.; Russell, C.; et al. Surveillance for Lyme disease in Canada: 2009–2015. Can. Commun. Dis. Rep. 2017, 43, 194–199. [Google Scholar] [CrossRef]
- Andany, N.; Cardew, S.; Bunce, P.E. A 35-year-old man with a positive Lyme test result from a private laboratory. CMAJ 2015, 187, 1222–1224. [Google Scholar] [CrossRef]
- Boudreau, C.R.; Lloyd, V.K.; Gould, O.N. Motivations and experiences of canadians seeking treatment for Lyme disease outside of the conventional Canadian health-care system. J. Pat. Exp. 2017, 5, 120–126. [Google Scholar] [CrossRef] [PubMed]
- Ogden, N.; Arsenault, J.; Hatchette, T.F.; Mechai, S.; Lindsay, L.R. Antibody responses to Borrelia burgdorferi detected by western blot vary geographically in Canada. PLoS ONE 2017, 12, e0171731. [Google Scholar] [CrossRef]
- Waddell, L.; Greig, J.; Mascarenhas, M.; Harding, S.; Lindsay, R. The accuracy of diagnostic tests for lyme disease in humans, a systematic review and meta-analysis of North American research. PLoS ONE 2016, 11, e0168613. [Google Scholar] [CrossRef] [PubMed]
- Lloyd, V.K.; Hawkins, R.G. Under-detection of Lyme disease in Canada. Healthcare 2018, 6, 125. [Google Scholar] [CrossRef]
- Eggertson, L. Advice varies for suspected Lyme disease. CMAJ 2014, 186, 899–900. [Google Scholar] [CrossRef]
- Auwaerter, P.G.; Bakken, J.S.; Dattwyler, R.J.; Dumler, J.S.; Halperin, J.J.; McSweegan, E.; Nadelman, R.B.; O’Connell, S.; Sood, S.K.; Weinstein, A.; et al. Scientific evidence and best patient care practices should guide the ethics of Lyme disease activism. J. Med. Ethics 2011, 37, 68–73. [Google Scholar] [CrossRef]
- Lloyd, V.; (Mount Allison University, Sackville, New Brunswick, Canada). Personal communication, 2018.
- Centers for Disease Control and Prevention Treatment. Available online: https://www.cdc.gov/lyme/treatment/index.html (accessed on 21 May 2018).
- Sanchez, E.; Vannier, E.; Wormser, G.P.; Hu, L.T. Diagnosis, treatment, and prevention of Lyme disease, human granulocytic anaplasmosis, and babesiosis a review. JAMA 2016, 315, 1767–1777. [Google Scholar] [CrossRef]
- Auwaerter, P.G. Point: Antibiotic therapy is not the answer for patients with persisting symptoms attributable to Lyme disease. Clin. Infect. Dis. 2007, 45, 143–148. [Google Scholar] [CrossRef]
- Radolf, J. Posttreatment chronic Lyme disease: What it is not. J. Infect. Dis. 2005, 192, 948–949. [Google Scholar] [CrossRef]
- Donta, S.T. Tetracycline therapy for chronic Lyme disease. Clin. Infect. Dis. 1997, 25, s52–s56. [Google Scholar] [CrossRef]
- Stricker, R.B. Counterpoint: Long-term antibiotic therapy improves persistent symptoms associated with Lyme disease. Clin. Infect. Dis. 2007, 45, 149–157. [Google Scholar] [CrossRef]
- Kowalski, T.J.; Tata, S.; Berth, W.; Mathiason, M.A.; Agger, W.A. Antibiotic treatment duration and long-term outcomes of patients with early Lyme disease from a Lyme disease–hyperendemic area. Clin. Infect. Dis. 2010, 50, 512–520. [Google Scholar] [CrossRef]
- Basul, S.; Garg, S. Antibiotic prescribing behavior among physicians: Ethical challenges in resource-poor settings. J. Med. Ethics Hist. Med. 2018, 11, 5–9. [Google Scholar]
- Shen, A.K.; Mead, P.S.; Beard, C.B. The Lyme disease vaccine—A public health perspective. Clin. Infect. Dis. 2011, 52, 5247–5252. [Google Scholar] [CrossRef]
- Kaaijk, P.; Luytjes, W. Vaccination against Lyme disease: Are we ready for it? Hum. Vacc. Imm. 2016, 12, 757–762. [Google Scholar] [CrossRef]
- Yaqub, O.; Castle-Clarke, S.; Sevdalis, N.; Chataway, J. Attitudes to vaccination: A critical review. Soc. Sci. Med. 2014, 112, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Poland, G.A.; Jacobson, R.M. Understanding those who do not understand: A brief review of the anti-vaccine movement. Vaccine 2001, 19, 2440–2445. [Google Scholar] [CrossRef]
- Dubé, E.; Vivion, M.; MacDonald, N.E. Vaccine hesitancy, vaccine refusal and the anti-vaccine movement: Influence, impact and implications. Exp. Rev. Vacc. 2015, 14, 99–117. [Google Scholar] [CrossRef]
- Canada. Public Health Canada. Lyme Disease in Canada—A Federal Framework. Available online: https://www.canada.ca/en/public-health/services/publications/diseases-conditions/lyme-disease-canada-federal-framework.html (accessed on 20 August 2018).
- Lieske, D.J.; Lloyd, V.K. Combining public participatory surveillance and occupancy modelling to predict the distributional response of Ixodes scapularis to climate change. Ticks Tick-borne Dis. 2018, 9, 695–706. [Google Scholar] [CrossRef] [PubMed]
- Silva, S. Reported Cases of Lyme Disease in Nova Scotia Expected to Reach New High. Available online: https://globalnews.ca/news/4194376/lyme-disease-nova-scotia/ (accessed on 19 January 2019).
- Rankin, A. ‘We Have a Problem, a Great Problem’; Public health failing to address Lyme disease crisis, says author. The Chronicle Herald, 4 June 2018, A3. ProQuest document ID: 2049910569.
- Ciolfe, T. Lyme disease uptick. Maclean’s 2018, 131, 17. [Google Scholar]
- Tunney, J. High-Risk Areas for Lyme Disease Expand to Include Moncton. Available online: https://www.cbc.ca/news/canada/new-brunswick/lyme-disease-high-risk-areas-1.4302257 (accessed on 3 March 2019).
- Gill, J. Ticks That Carry Lyme Disease on the Move in New Brunswick. Available online: https://www.cbc.ca/news/canada/new-brunswick/lyme-disease-york-county-1.4722036 (accessed on 3 March 2019).
- Russell, N. P.E.I. Tick Study Points to Risk of Lyme Disease on the Island. Available online: http://www.cbc.ca/news/canada/prince-edward-island/pei-tick-study-results-1.4673332 (accessed on 3 March 2019).
- Lyme Disease Increases in Canada as Climate, Land Use Change. Available online: http://www.cbc.ca/news/health/lyme-disease-climate-change-1.3586065 (accessed on 4 March 2019).
- Young, L. More Ticks Means an Increase of Lyme Disease Across Canada—Thanks to Climate Change. Available online: https://globalnews.ca/news/3472203/more-ticks-means-an-increase-of-lyme-disease-across-canada-thanks-to-climate-change/ (accessed on 4 March 2019).
- Ehman, K. Couple Forced to Travel to BC for Lyme Disease Diagnosis. Available online: http://www.peicanada.com/eastern_graphic/article_39c55d3a-1678-11e8-b1f0-b3feca65a3b3.html (accessed on 4 March 2019).
- Ubelacker, S. Lyme Disease Upticks in Canada; Infection Insects That Carry Disease Spreading in Canada, As Is Controversy over Disease. Available online: https://search-proquest-com.libproxy.mta.ca/docview/423310201?accountid=12599 (accessed on 21 August 2018).
- Kingston, A. How the New Impatient Patient Is Disrupting Medicine. Available online: https://www.macleans.ca/society/health/how-the-new-impatient-patient-is-disrupting-medicine/ (accessed on 31 August 2018).
- New Brunswick. Office of the Chief Medical Officer. New Brunswick Lyme Disease Strategy 2017. Available online: https://www2.gnb.ca/content/dam/gnb/Departments/h-s/pdf/en/CDC/LymeDiseaseStrategy.pdf (accessed on 1 August 2018).
- Nova Scotia. Department of Health and Wellness. Notifiable Disease in Nova Scotia 2016 Surveillance Report. Available online: https://novascotia.ca/dhw/populationhealth/documents/Annual-Notifiable-Disease-Surveillance-Report-2016.pdf (accessed on 1 August 2018).
- Nova Scotia. Department of Health and Wellness. Zoonotic Diseases Technical Working Group. Tick Borne Diseases Response Plan. Available online: https://novascotia.ca/dhw/cdpc/documents/Tick-Borne-Disease-Response-Plan.pdf (accessed on 14 August 2018).
- German, G. Prince Edward Island Lyme Disease Algorithm June 2014. Available online: http://www.gov.pe.ca/photos/original/hpei_lymediseas.pdf?_ga=1.197449967. 1534297227.1475780350 (accessed on 17 August 2018).
- Nova Scotia. Department of Health and Wellness. Infectious Disease Expert Group. Statement for Managing Lyme Disease in Nova Scotia. Available online: https://novascotia.ca/dhw/cdpc/documents/statement_for_managing_LD.pdf (accessed on 19 August 2018).
- Rankin, A. Strang Issues Statement on Lyme Disease Twitter Post. Available online: https://www.thechronicleherald.ca/news/local/strang-issues-statement-on-lyme-disease-twitter-post-280301/ (accessed on 1 February 2019).
- Rankin, A. Nova Scotia’s Top Doctor Takes Heat over Retweet Dismissing Chronic Lyme Disease. Available online: https://www.thechronicleherald.ca/news/local/provinces-top-doctor-takes-heat-over-tweet-dismissing-chronic-lyme-disease-279636/ (accessed on 28 April 2019).
- Statistics Canada. 2016 Census. Available online: https://www12.statcan.gc.ca/census-recensement/2016/dp-pd/index-eng.cfm (accessed on 9 July 2018).
- Statistics Canada. Census Profile—2016 Census. Prince Edward Island. Available online: https://www12.statcan.gc.ca/census-recensement/2016/dp-pd/prof/details/Page.cfm?Lang=E&Geo1=PR&Code1=11&Geo2=&Code2=&Data=Count&SearchText=Prince%20Edward%20Island&Search%20Type=Begins&SearchPR=01&B1=All&GeoLevel=PR&GeoCode=11 (accessed on 18 March 2019).
- Levesque, M. Bringing Patients In: Patient Engagement Options for New Brunswick Health Care; Voices in Harmony Project: Moncton, NB, Canada, 2013; p. 85.
- Abelson, J.; Forest, P.-G.; Eyles, J.; Smith, P.; Martin, E.; Gauvin, F.-P. Obtaining public input for health-systems decision-making: Past experiences and future prospects. Cdn. Pub. Admin. 2012, 45, 70–97. [Google Scholar] [CrossRef]
- Patrick, K.; Kebbe, M.; Aubin, D. A home for patient-oriented research. CMAJ 2018, 190, E607. [Google Scholar] [CrossRef]
- Rich, P. Patients seeking more involvement at medical meetings. CMAJ 2018, 190, E602. [Google Scholar] [CrossRef]
- Arnstein, S. A ladder of citizen participation. J. Am. Plan. Assoc. 1969, 35, 216–224. [Google Scholar] [CrossRef]
- Abelson, J.; Forest, P.G.; Eyles, J.; Casebeer, A.; Mackean, G.; Gauvin, F.P.; Kouri, D.; Martin, E.; Pennock, M.; Smith, P. Will it make a difference if I show up and share? A citizens’ perspective on improving public involvement processes for health system decision-making. J. Health Ser. Res. Pol. 2004, 9, 205–212. [Google Scholar] [CrossRef]
- Kingdon, J. Agendas, Alternatives and Public Policies; Little, Brown & Company: Boston, MA, USA, 1984. [Google Scholar]
- Zahariadis, N. The multiple streams framework: structure, limitations, prospects. In Theories of the Policy Process, 2nd ed.; Sabatier, P.A., Ed.; Westview Press: Boulder, CO, USA, 2007; pp. 65–92. [Google Scholar]
- Pelley, L. Lyme Disease on the Rise in Canada, but Doctors Still Confused About Diagnosis. Available online: https://www.cbc.ca/news/canada/toronto/lyme-disease-canada-1.4262478 (accessed on 1 August 2018).
- Mulholland, A. Is It Time to Bring Back the Lyme Disease Vaccine? Available online: https://www.ctvnews.ca/health/is-it-time-to-bring-back-the-lyme-disease-vaccine-1.4059767 (accessed on 4 January 2019).
- Luché-Thayer, J.; Perrone, C.; Meseko, C. Obstruction to treatment meeting international standards for Lyme and relapsing fever Borreliosis patients. Int. J. Law Pol. Sci. 2018, 12, 847–859. [Google Scholar]
- Committee on Standards for Developing Trustworthy Clinical Practice Guidelines. Clinical Practice Guidelines We Can Trust. Available online: http://data.care-statement.org/wp-content/uploads/2016/12/IOMGuidelines-2013-1.pdf (accessed on 24 February 2019).
| Province | No. Identified | No. with Fax # | No. Faxed | No. Failed After 2 Tries | Net No. |
|---|---|---|---|---|---|
| New Brunswick | |||||
| Health Region 1 (Moncton) | 283 | 196 | 100 | 10 | 90 |
| Health Region 2 (Saint John, Southwest NB) | 199 | 110 | 80 | 3 | 77 |
| Health Region 6 (Bathurst) | 91 | 58 | 58 | 0 | 58 |
| Health Region 4 (Edmundston) | 69 | 44 | 44 | 0 | 44 |
| NB Totals | 642 | 408 | 282 | 13 | 269 |
| Nova Scotia | |||||
| Halifax, Dartmouth, Bedford | 313 | 226 | 92 | 3 | 89 |
| Yarmouth, Shelburne, Liverpool | 28 | 19 | 19 | 0 | 19 |
| Pictou, Trenton, New Glasgow, Antigonish | 36 | 17 | 17 | 0 | 17 |
| NS Totals | 377 | 262 | 128 | 3 | 125 |
| Prince Edward Island | 102 | 102 | 52 | 0 | 52 |
| PEI Totals | 102 | 102 | 52 | 0 | 52 |
| Total | 1121 | 772 | 462 | 16 | 446 |
| New Brunswick | Nova Scotia | Prince Edward Island (PEI) | Total | |
|---|---|---|---|---|
| Provincial Politicians (MLAs) | 49 | 51 | 27 | 127 |
| Government Health Officials | 14 | 6 | 5 | 25 |
| Total | 63 | 57 | 32 | 152 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Levesque, M.; Klohn, M. A Multiple Streams Approach to Understanding the Issues and Challenges of Lyme Disease Management in Canada’s Maritime Provinces. Int. J. Environ. Res. Public Health 2019, 16, 1531. https://doi.org/10.3390/ijerph16091531
Levesque M, Klohn M. A Multiple Streams Approach to Understanding the Issues and Challenges of Lyme Disease Management in Canada’s Maritime Provinces. International Journal of Environmental Research and Public Health. 2019; 16(9):1531. https://doi.org/10.3390/ijerph16091531
Chicago/Turabian StyleLevesque, Mario, and Matthew Klohn. 2019. "A Multiple Streams Approach to Understanding the Issues and Challenges of Lyme Disease Management in Canada’s Maritime Provinces" International Journal of Environmental Research and Public Health 16, no. 9: 1531. https://doi.org/10.3390/ijerph16091531
APA StyleLevesque, M., & Klohn, M. (2019). A Multiple Streams Approach to Understanding the Issues and Challenges of Lyme Disease Management in Canada’s Maritime Provinces. International Journal of Environmental Research and Public Health, 16(9), 1531. https://doi.org/10.3390/ijerph16091531




