The Relationship between Socioeconomic Status, Mental Health, and Need for Long-Term Services and Supports among the Chinese Elderly in Shandong Province—A Cross-Sectional Study
Abstract
1. Background
2. Methods
2.1. Study Location and its Population Aging Conditions
2.2. Data Collection and Research Participants
2.3. Measurements
2.4. Statistical Analysis
2.5. Ethical Considerations
3. Results
3.1. Sample Characteristics
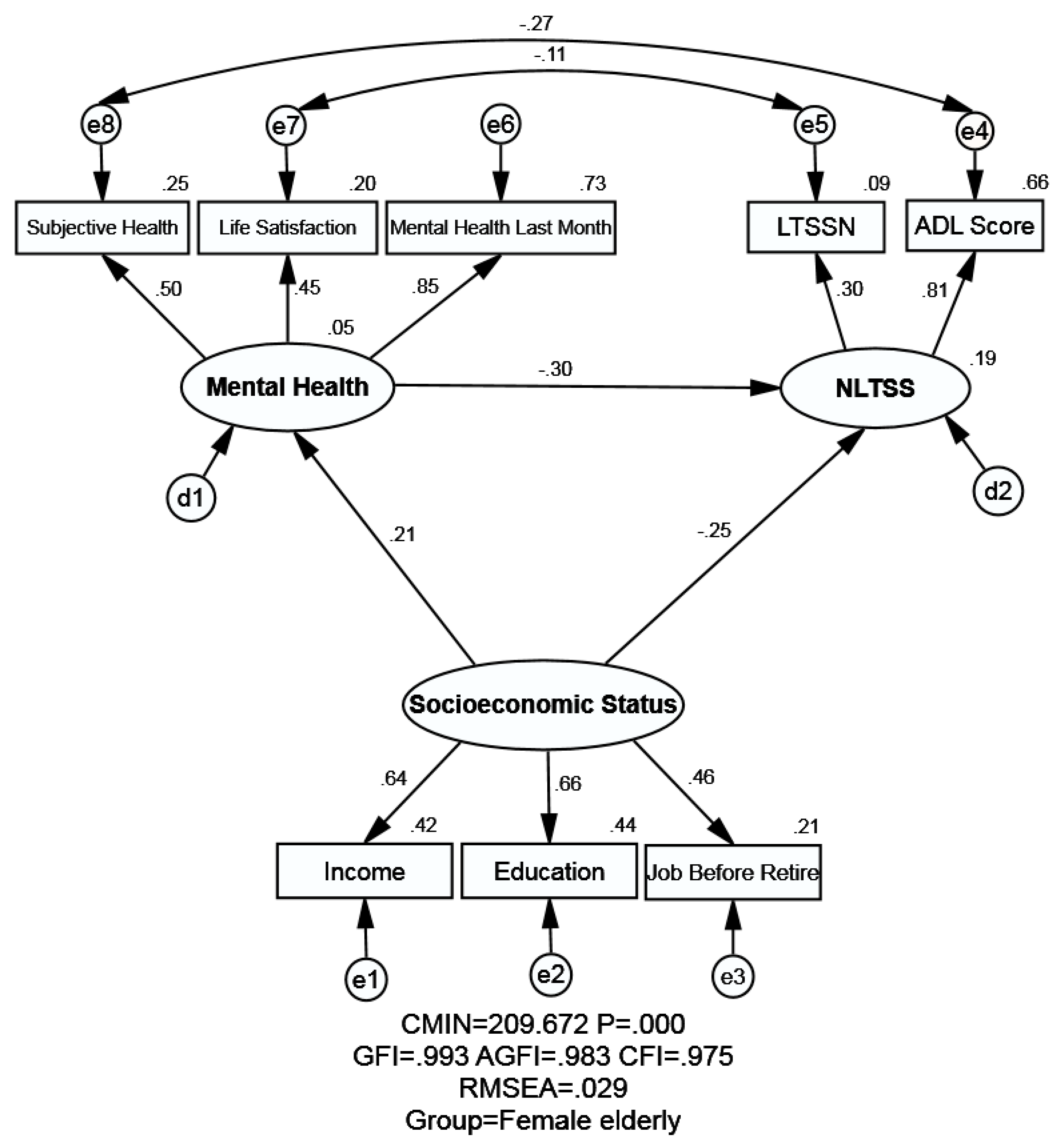
3.2. The Structural Model
3.2.1. Measurement Invariance Across Gender
3.2.2. Model Fitness Indices
3.3. Relationship between SES, Mental Health and NLTSS Assessed with SEM
3.3.1. Association between SES and NLTSS
3.3.2. Association between Mental Health and NLTSS
3.3.3. Association between SES and Mental Health
4. Discussion
4.1. Principal Findings and Comparison with Other Studies
4.1.1. NLTSS of the Participants
4.1.2. SES and NLTSS
4.1.3. Mental Health and NLTSS
4.1.4. SES and Mental Health
4.1.5. SES, Health and NLTSS
4.2. Implications
4.3. Limitations
4.4. Future Research
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Abbreviations
| SES | socioeconomic status |
| NLTSS | need for long-term services and support |
| LTCI | long-term care insurance |
| SEM | structural equation modeling |
| GDP | gross domestic product |
| PSUs | primary sampling units |
| SSUs | secondary sampling units |
| ADL | activities of daily living |
| IADL | instrumental activities of daily living |
| PSMS | physical self-maintenance scale |
| SPSS | statistical package for social science |
| LTSSN | long-term services and support needs |
| GFI | goodness of fit index |
| AGFI | adjusted goodness of fit index |
| CFI | comparative fit index |
| RMSEA | root mean square error of approximation |
| UEBMI | urban employee basic medical insurance |
| URBMI | urban resident basic medical insurance |
| NRCMS | new rural cooperative medical System |
Appendix A. Brief Introduction to SEM
Appendix B. Model Fitness Index of SEM
Appendix C. Measurement Invariance across Groups in SEM
References
- United Nations. World Family Planning 2017 Highlights; United Nations Publications: New York, NY, USA, 2017. [Google Scholar]
- United Nations. World Population Prospects 2017 REVISION Volume I: Comprehensive Tables; United Nations Publications: New York, NY, USA, 2017. [Google Scholar]
- The State Council of The People’s Republic of China. 241 Million Old Adults in China and Equals 17.3% of the Whole Population. Available online: http://www.gov.cn/xinwen/2018-02/26/content_5268992.htm (accessed on 8 July 2018).
- United Nations. World Population Prospects The 2017 Revision Key Findings and Advance Tables; United Nations Publications: New York, NY, USA, 2017. [Google Scholar]
- Choi, H.; Burgard, S.; Elo, I.T.; Heisler, M. Are older adults living in more equal counties healthier than older adults living in more unequal counties? A propensity score matching approach. Soc. Sci. Med. (1982) 2015, 141, 82–90. [Google Scholar] [CrossRef] [PubMed]
- Lim, S.; Chan, P.Y.; Walters, S.; Culp, G.; Huynh, M.; Gould, L.H. Impact of residential displacement on healthcare access and mental health among original residents of gentrifying neighborhoods in New York City. PLoS ONE 2017, 12, e0190139. [Google Scholar] [CrossRef] [PubMed]
- Hassanzadeh, J.; Asadi-Lari, M.; Baghbanian, A.; Ghaem, H.; Kassani, A.; Rezaianzadeh, A. Association between social capital, health-related quality of life, and mental health: A structural-equation modeling approach. Croat. Med. J. 2016, 57, 58–65. [Google Scholar] [CrossRef] [PubMed]
- Honjo, K.; Kawakami, N.; Tsuchiya, M.; Sakurai, K. Association of subjective and objective socioeconomic status with subjective mental health and mental disorders among Japanese men and women. Int. J. Behav. Med. 2014, 21, 421–429. [Google Scholar] [CrossRef] [PubMed]
- Kong, F.L.; Hoshi, T.; Ai, B.; Shi, Z.M.; Nakayama, N.; Wang, S.; Yang, S.W. Association between socioeconomic status (SES), mental health and need for long-term care (NLTC)-A Longitudinal Study among the Japanese Elderly. Arch. Gerontol. Geriatr. 2014, 59, 372–381. [Google Scholar] [CrossRef]
- Tani, Y.; Fujiwara, T.; Kondo, N.; Noma, H.; Sasaki, Y.; Kondo, K. Childhood Socioeconomic Status and Onset of Depression among Japanese Older Adults: The JAGES Prospective Cohort Study. Am. J. Geriatr. Psychiatry Off. J. Am. Assoc. Geriatr. Psychiatry 2016, 24, 717–726. [Google Scholar] [CrossRef] [PubMed]
- Nonnemaker, J.M.; Allen, J.A.; Davis, K.C.; Kamyab, K.; Duke, J.C.; Farrelly, M.C. The influence of antismoking television advertisements on cessation by race/ethnicity, socioeconomic status, and mental health status. PLoS ONE 2014, 9, e102943. [Google Scholar] [CrossRef] [PubMed]
- Donisi, V.; Tedeschi, F.; Percudani, M.; Fiorillo, A.; Confalonieri, L.; De Rosa, C.; Salazzari, D.; Tansella, M.; Thornicroft, G.; Amaddeo, F. Prediction of community mental health service utilization by individual and ecological level socio-economic factors. Psychiatry Res. 2013, 209, 691–698. [Google Scholar] [CrossRef] [PubMed]
- Ju, Y.J.; Park, E.C.; Han, K.T.; Choi, J.W.; Kim, J.L.; Cho, K.H.; Park, S. Low socioeconomic status and suicidal ideation among elderly individuals. Int. Psychogeriatr. 2016, 28, 2055–2066. [Google Scholar] [CrossRef] [PubMed]
- Berkman, C.S.; Gurland, B.J. The relationship among income, other socioeconomic indicators, and functional level in older persons. J. Aging Health 1998, 10, 81–98. [Google Scholar] [CrossRef]
- Schmidt, A.E. Analysing the importance of older people’s resources for the use of home care in a cash-for-care scheme: Evidence from Vienna. Health Soc. Care Community 2017, 25, 514–526. [Google Scholar] [CrossRef] [PubMed]
- Martikainen, P.; Moustgaard, H.; Murphy, M.; Einio, E.K.; Koskinen, S.; Martelin, T.; Noro, A. Gender, living arrangements, and social circumstances as determinants of entry into and exit from long-term institutional care at older ages: A 6-year follow-up study of older Finns. Gerontology 2009, 49, 34–45. [Google Scholar] [CrossRef] [PubMed]
- Paraponaris, A.; Davin, B.; Verger, P. Formal and informal care for disabled elderly living in the community: An appraisal of French care composition and costs. Eur. J. Health Econ. Hepac Health Econ. Prev. Care 2012, 13, 327–336. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.C.; Chung, M.H.; Lai, K.L.; Chou, C.C.; Kao, S. Preferences of the elderly and their primary family caregivers in the arrangement of long-term care. J. Formos. Med Assoc. 2004, 103, 533–539. [Google Scholar] [PubMed]
- Tennstedt, S.; Chang, B.H. The relative contribution of ethnicity versus socioeconomic status in explaining differences in disability and receipt of informal care. J. Gerontol. Ser. Bpsychol. Sci. Soc. Sci. 1998, 53, S61–S70. [Google Scholar] [CrossRef]
- Miller, B.; McFall, S.; Campbell, R.T. Changes in sources of community long-term care among African American and white frail older persons. J. Gerontol. 1994, 49, S14–S24. [Google Scholar] [CrossRef] [PubMed]
- Hall, P.A.; Husein, N.; Vincent, C. Mental Health Needs of Patients Living with Diabetes in the Long-Term Care Context: A Comment on Sears and Schmidt. Can. J. Diabetes 2016, 40, 490–491. [Google Scholar] [CrossRef]
- Luber, M.P.; Meyers, B.S.; Williams-Russo, P.G.; Hollenberg, J.P.; DiDomenico, T.N.; Charlson, M.E.; Alexopoulos, G.S. Depression and Service Utilization in Elderly Primary Care Patients. Am. J. Geriatr. Psychiatry 2001, 9, 169–176. [Google Scholar] [CrossRef]
- Snowdon, J. Mental health service delivery in long-term care homes. Int. Psychogeriatr. 2010, 22, 1063–1071. [Google Scholar] [CrossRef]
- Ito, K.; Inagaki, H.; Okamura, T.; Shimokado, K.; Awata, S. Factors associated with mental health well-being of urban community-dwelling elders in Japan: Comparison between subjects with and without long-term care insurance certification. Nihon Ronen Igakkai Zasshi. Jpn. J. Geriatr. 2012, 49, 82–89. [Google Scholar] [CrossRef]
- Hutchison, S.L.; Terhorst, L.; Murtaugh, S.; Gross, S.; Kogan, J.N.; Shaffer, S.L. Effectiveness of a Staff Promoted Wellness Program to Improve Health in Residents of a Mental Health Long-Term Care Facility. Issues Ment. Health Nurs. 2016, 37, 257–264. [Google Scholar] [CrossRef] [PubMed]
- De Rooij, A.H.; Luijkx, K.G.; Declercq, A.G.; Emmerink, P.M.; Schols, J.M. Professional caregivers’ mental health problems and burnout in small-scale and traditional long term care settings for elderly people with dementia in the Netherlands and Belgium. J. Am. Med Dir. Assoc. 2012, 13, 486.e7–11. [Google Scholar] [CrossRef]
- Shandong Provincial Office of Local Chronicles. The General Information about Shandong Province. Available online: http://www.sdsqw.cn/overview/2016gk/2017/1116/38480.html (accessed on 7 June 2018).
- Shandong Provincial Bureau of Statistics. Statistical Bulletin of Shandong Provincial National Economic and Social Development. Available online: http://www.shandong.gov.cn/art/2018/3/1/art_2531_11001.html (accessed on 8 September 2018).
- Andrew, M.K. Brocklehurst’s Textbook of Geriatric Medicine and Gerontology, 7th ed.; W.B. Saunders: Philadelphia, PA, USA, 2010; p. 198. [Google Scholar]
- Winters-Miner, L.A.; Bolding, P.S.; Hilbe, J.M.; Goldstein, M.; Hill, T.; Nisbet, R.; Walton, N.; Miner, G.D. Practical Predictive Analytics and Decisioning Systems for Medicine; Academic Press: Cambridge, MA, USA, 2015; pp. 176–204. [Google Scholar]
- Cutler, D.M.; Lleras-Muney, A.; Vogl, T. Socioeconomic Status and Health: Dimensions and Mechanisms; National Bureau of Economic Research: Cambridge, MA, USA, 2008. [Google Scholar]
- Ross, C.E.; Wu, C.-L. The links between education and health. Am. Sociol. Rev. 1995, 60, 719–745. [Google Scholar] [CrossRef]
- Lantz, P.M.; House, J.S.; Lepkowski, J.M.; Williams, D.R.; Mero, R.P.; Chen, J. Socioeconomic factors, health behaviors, and mortality. J. Am. Med Assoc. 1998, 279, 1703–1708. [Google Scholar] [CrossRef]
- Wilkinson, R.G. Income distribution and mortality: A ‘natural’experiment. Soc. Health Illn. 1990, 12, 391–412. [Google Scholar] [CrossRef]
- Laszlo, K.D.; Pikhart, H.; Kopp, M.S.; Bobak, M.; Pajak, A.; Malyutina, S.; Salavecz, G.; Marmot, M. Job insecurity and health: A study of 16 European countries. Soc. Sci. Med. (1982) 2010, 70, 867–874. [Google Scholar] [CrossRef] [PubMed]
- Moulin, J.J.; Labbe, E.; Sass, C.; Gerbaud, L. Job insecurity, unemployment and health: Results from the health examination centers of the French General Health Insurance. Rev. Epidemiol. Sante Publique 2009, 57, 141–149. [Google Scholar] [CrossRef] [PubMed]
- D’Souza, R.M.; Strazdins, L.; Lim, L.L.Y.; Broom, D.H.; Rodgers, B. Work and health in a contemporary society: Demands, control, and insecurity. J. Epidemiol. Community Health 2003, 57, 849. [Google Scholar] [CrossRef]
- Coenen, P.; Huysmans, M.A.; Holtermann, A.; Krause, N.; van Mechelen, W.; Straker, L.M.; van der Beek, A.J. Do highly physically active workers die early? A systematic review with meta-analysis of data from 193 696 participants. Br. J. Sports Med. 2018, 52, 1320. [Google Scholar] [CrossRef]
- World Health Organization. Mental health: Strengthening our response. Available online: http://www.who.int/news-room/fact-sheets/detail/mental-health-strengthening-our-response (accessed on 25 April 2018).
- Lawton, M.P.; Brody, E.M. Assessment of older people: Self-maintaining and instrumental activities of daily living. Gerontology 1969, 9 Pt 1, 179–186. [Google Scholar] [CrossRef]
- Hoile, V.; Thang, P.; Lindholm, L. Elderly care in daily living in rural Vietnam: Need and its socioeconomic determinants. BMC Geriatr. 2011, 11, 81. [Google Scholar]
- McKevitt, C.; Fudge, N.; Redfern, J.; Sheldenkar, A.; Crichton, S.; Rudd, A.R.; Forster, A.; Young, J.; Nazareth, I.; Silver, L.E.; et al. Self-reported long-term needs after stroke. Stroke 2011, 42, 1398–1403. [Google Scholar] [CrossRef] [PubMed]
- Laporte, A.; Croxford, R.; Coyte, P.C. Can a publicly funded home care system successfully allocate service based on perceived need rather than socioeconomic status? A Canadian experience. Health Soc. Care Community 2007, 15, 108–119. [Google Scholar] [CrossRef] [PubMed]
- Kim, N.H.; Hoyek, G.E.; Chau, D. Long-term care of the aging population with intellectual and developmental disabilities. Clin. Geriatr. Med. 2011, 27, 291–300. [Google Scholar] [CrossRef] [PubMed]
- Reid, K.A.; Smiley, E.; Cooper, S.A. Prevalence and associations of anxiety disorders in adults with intellectual disabilities. J. Intellect. Disabil. Res. 2011, 55, 172–181. [Google Scholar] [CrossRef] [PubMed]
- Wolfe, C.D.; Crichton, S.L.; Heuschmann, P.U.; McKevitt, C.J.; Toschke, A.M.; Grieve, A.P.; Rudd, A.G. Estimates of outcomes up to ten years after stroke: Analysis from the prospective South London Stroke Register. PLoS Med. 2011, 8, e1001033. [Google Scholar] [CrossRef] [PubMed]
- Samuelsson, G.; Sundstrom, G.; Dehlin, O.; Hagberg, B. Formal support, mental disorders and personal characteristics: A 25-year follow-up study of a total cohort of older people. Health Soc. Care Community 2003, 11, 95–102. [Google Scholar] [CrossRef]
- Gong, F.; Xu, J.; Takeuchi, D.T. Beyond conventional socioeconomic status: Examining subjective and objective social status with self-reported health among Asian immigrants. J. Behav. Med. 2012, 35, 407–419. [Google Scholar] [CrossRef]
- Sani, F.; Magrin, M.E.; Scrignaro, M.; McCollum, R. In-group identification mediates the effects of subjective in-group status on mental health. Br. J. Soc. Psychol. 2010, 49 Pt 4, 883–893. [Google Scholar] [CrossRef]
- Mavrinac, G.V.; Sersic, D.M.; Mujkic, A. Cardiovascular and behavioral risk factors in relation to self-assessed health status. Coll. Antropol. 2009, 33 (Suppl. 1), 99–106. [Google Scholar]
- Honjo, K.; Kawakami, N.; Takeshima, T.; Tachimori, H.; Ono, Y.; Uda, H.; Hata, Y.; Nakane, Y.; Nakane, H.; Iwata, N.; et al. Social class inequalities in self-rated health and their gender and age group differences in Japan. J. Epidemiol. 2006, 16, 223–232. [Google Scholar] [CrossRef] [PubMed]
- Daniels, N.; Kennedy, B.; Kawachi, I. Health and inequality, or, why justice is good for our health. In Public Health, Ethics, and Equity; Anand, S., Peter, F., Sen, A., Eds.; Oxford University Press: Oxford, UK, 2004; pp. 63–91. [Google Scholar]
- Fiorillo, D.; Sabatini, F. Quality and quantity: The role of social interactions in self-reported individual health. Soc. Sci. Med. (1982) 2011, 73, 1644–1652. [Google Scholar] [CrossRef]
- Erreygers, G. A dual atkinson measure of socioeconomic inequality of health. Health Econ. 2012, 22, 466–479. [Google Scholar] [CrossRef]
- Marmot, M.; Wilkinson, R. Social Determinants of Health; Oxford University Press: New York, NY, USA, 1999. [Google Scholar]
- Kawachi, I.; Kennedy, B.P. Health and social cohesion: Why care about income inequality? BMJ (Clin. Res. Ed.) 1997, 314, 1037–1040. [Google Scholar] [CrossRef]
- Kagamimori, S.; Gaina, A.; Nasermoaddeli, A. Socioeconomic status and health in the Japanese population. Soc. Sci. Med. (1982) 2009, 68, 2152–2160. [Google Scholar] [CrossRef] [PubMed]
- Jensen, R.T. Socioeconomic status, nutrition, and health among the elderly. In Perspectives on the Economics of Aging; University of Chicago Press: Chicago, IL, USA, 2004; pp. 313–332. [Google Scholar]
- International Monetary Fund. World Economic Outlook Database. 2017. Available online: https://www.imf.org/external/pubs/ft/weo/2017/02/weodata/download.aspx (accessed on 12 September 2018).
- Feldstein, M. Social security pension reform in China. In Urbanization and Social Welfare in China; Routledge: Abingdon, UK, 2018; pp. 25–36. [Google Scholar]
- Li, C.; Yu, X.; Butler, J.R.G.; Yiengprugsawan, V.; Yu, M. Moving towards universal health insurance in China: Performance, issues and lessons from Thailand. Soc. Sci. Med. 2011, 73, 359–366. [Google Scholar] [CrossRef] [PubMed]
- Wang, H. A dilemma of Chinese healthcare reform: How to re-define government roles? China Econ. Rev. 2009, 20, 598–604. [Google Scholar] [CrossRef]
- Phelan, E.A.; Anderson, L.A.; LaCroix, A.Z.; Larson, E.B. Older adults’ views of “successful aging”—How do they compare with researchers’ definitions? J. Am. Geriatr. Soc. 2004, 52, 211–216. [Google Scholar] [CrossRef]
- Bråne, G.; Karlsson, I.; Kihlgren, M.; Norberg, A. Integrity-promoting care of demented nursing home patients: Psychological and biochemical changes. Int. J. Geriatr. Psychiatry 1989, 4, 165–172. [Google Scholar] [CrossRef]
- Schilling, O. Development of life satisfaction in old age: Another view on the “paradox”. Soc. Indic. Res. 2006, 75, 241–271. [Google Scholar] [CrossRef]
- Chiang, H.H.; Chien, L.H.; Lin, J.S.; Yeh, Y.H.; Lee, T.S. Modeling psychological well-being and family relationships among retired older people in Taiwan. Int. J. Ment. Health Nurs. 2013, 22, 93–101. [Google Scholar] [CrossRef] [PubMed]
- Ullman, J.B.; Bentler, P.M. Structural equation modeling. Handb. Psychol. 2012. [Google Scholar] [CrossRef]
- Lomax, R.G.; Schumacker, R.E. A Beginner’s Guide to Structural Equation Modeling; Lawrence Erlbaum Associates, Inc.: Mahwah, NJ, USA, 2004. [Google Scholar]
- Bentler, P.M.; Bonett, D.G. Significance tests and goodness of fit in the analysis of covariance structures. Psychol. Bull. 1980, 88, 588–606. [Google Scholar] [CrossRef]
- Jöreskog, K.G.; Andersen, E.B.; Laake, P.; Cox, D.; Schweder, T. Analysis of Covariance Structures [with Discussion and Reply]. Scand. J. Stat. 1981, 8, 65–92. [Google Scholar]
- Fan, X.T.; Thompson, B.; Wang, L. Effects of sample size, estimation methods, and model specification on structural equation modeling fit indexes. Struct. Equ. Model. A Multidiscip. J. 1999, 6, 56–83. [Google Scholar] [CrossRef]
- Rong, T. Amos and Research Method, 2nd ed.; Chongqing University Press: Chongqing, China, 2010. [Google Scholar]
- Kline, R.B. Principles and Practice of Structural Equation Modeling, 4th ed.; The Guilford Press: New York, NY, USA, 2016. [Google Scholar]
- Cheung, G.W.; Rensvold, R.B. Evaluating Goodness-of-Fit Indexes for Testing Measurement Invariance. Struct. Equ. Model. A Multidiscip. J. 2002, 9, 233–255. [Google Scholar] [CrossRef]
- Chen, F.F. Sensitivity of goodness of fit indexes to lack of measurement invariance. Struct. Equ. Model. 2007, 14, 464–504. [Google Scholar] [CrossRef]

| Variables | Definition | Measurements | Options |
|---|---|---|---|
| Socioeconomic Status | A broad concept that compositely assess an individual’s economic and sociological position in relation to others. | Education | (1) Illiteracy |
| (2) Graduate from Elementary School | |||
| (3) Graduate from Junior Middle School | |||
| (4) Graduate from Senior Middle School and above | |||
| Annual income | (1) less than 2200 RMB (USD = 326) | ||
| (2) from 2201 to 3300 RMB (USD = 489) | |||
| (3) from 3301 to 6200 RMB (USD = 919) | |||
| (4) from 6201 to 21,400 RMB (USD = 3170) | |||
| (5) more than 21,400 RMB (USD = 3170) | |||
| Job before retire | (1) Professionals/technical | ||
| (2) Leaders of government/public institution | |||
| (3) Clerks or staff | |||
| (4) Businessman/commercial servants | |||
| (5) Farming/forestry/fishing industry | |||
| (6) Transportation industry/manual workers | |||
| (7) Privately/individually owned business | |||
| (8) Other jobs. | |||
| Mental Health | A state of well-being in which every individual realizes his or her own potential, can cope with the normal stresses of life, can work productively and fruitfully, and is able to make a contribution to her or his community. | How do you feel about your health status (subjective health)? | (1) Very bad |
| (2) Fairly bad | |||
| (3) Moderately | |||
| (4) Fairly good | |||
| (5) Very good | |||
| How about your mental health status last month (mental health last month)? | (1) Very bad | ||
| (2) Bad | |||
| (3) Moderately | |||
| (4) Good | |||
| (5) Very good | |||
| Are you satisfied with your life (life satisfaction)? | (1) Very Dissatisfied | ||
| (2) Fairly dissatisfied | |||
| (3) Moderately | |||
| (4) Fairly satisfied | |||
| (5) Very satisfied | |||
| Need for long-term services and supports | The subjectively assessment of need for long-term services and supports by the elderly, which include both home and community-based services, as well as long-term care facilities. | long-term services and supports needs | (1) Not needed |
| (2) Needed | |||
| ADL Score | (1) 14 | ||
| (2) 15 | |||
| (3) 16 | |||
| (4) 17 | |||
| (5) 18–27 | |||
| (6) ≥28 |
| Variable | LTSSN | χ2 Test | |||||
|---|---|---|---|---|---|---|---|
| No Need (n = 6768) | Need (n = 302) | Total (n = 7070) | |||||
| n | % | n | % | n | % | ||
| Gender | |||||||
| Male | 2722 | 95.6% | 124 | 4.4% | 2846 | 100.0% | 0.085 p = 0.771 |
| Female | 4046 | 95.8% | 178 | 4.2% | 4224 | 100.0% | |
| Age | |||||||
| 60–64 | 1520 | 96.4% | 57 | 3.6% | 1577 | 100.0% | 31.767 p < 0.001 |
| 65–69 | 2060 | 96.8% | 69 | 3.2% | 2129 | 100.0% | |
| 70–74 | 1711 | 96.1% | 69 | 3.9% | 1780 | 100.0% | |
| >75 | 1477 | 93.2% | 107 | 6.8% | 1584 | 100.0% | |
| Variable | Gender | χ2 Test | |||||
|---|---|---|---|---|---|---|---|
| Male (n = 2846) | Female (n = 4224) | Total (n = 7070) | |||||
| n | % | n | % | n | % | ||
| Education (graduation from) | |||||||
| Illiteracy | 491 | 21.6% | 1779 | 78.4% | 2270 | 100.0% | 561.142 p < 0.001 |
| Elementary School | 1294 | 44.3% | 1630 | 55.7% | 2924 | 100.0% | |
| Junior Middle School | 718 | 54.6% | 597 | 45.4% | 1315 | 100.0% | |
| Senior Middle School and above | 343 | 61.1% | 218 | 38.9% | 561 | 100.0% | |
| Income (RMB per year) | |||||||
| 0–2200 | 505 | 30.0% | 1180 | 70.0% | 1685 | 100.0% | 117.736 p < 0.001 |
| 2201–3300 | 439 | 38.1% | 714 | 61.9% | 1153 | 100.0% | |
| 3301–6200 | 607 | 43.2% | 797 | 56.8% | 1404 | 100.0% | |
| 6201–21,400 | 652 | 46.1% | 762 | 53.9% | 1414 | 100.0% | |
| >21,400 | 643 | 45.5% | 771 | 54.5% | 1414 | 100.0% | |
| Job Before Retire | |||||||
| Professionals/technical | 243 | 55.0% | 199 | 45.0% | 442 | 100.0% | 121.792 p < 0.001 |
| Leaders of government/public institution | 111 | 61.7% | 69 | 38.3% | 180 | 100.0% | |
| Clerks or staff | 87 | 53.0% | 77 | 47.0% | 164 | 100.0% | |
| Businessman/commercial servants | 28 | 24.1% | 88 | 75.9% | 116 | 100.0% | |
| Farming/ forestry/fishing | 2107 | 38.5% | 3372 | 61.5% | 5479 | 100.0% | |
| Transportation industry/manual workers | 174 | 45.4% | 209 | 54.6% | 383 | 100.0% | |
| Privately/individually-owned business | 14 | 43.8% | 18 | 56.3% | 32 | 100.0% | |
| Other jobs | 82 | 29.9% | 192 | 70.1% | 274 | 100.0% | |
| Variable | Gender | χ2 Test | |||||
|---|---|---|---|---|---|---|---|
| Male (n = 2846) | Female (n = 4224) | Total (n = 7070) | |||||
| n | % | n | % | n | % | ||
| Subjective Health | |||||||
| Very bad | 55 | 43.3% | 72 | 56.7% | 127 | 100.0% | 23.336 p < 0.001 |
| Fairly bad | 434 | 37.1% | 735 | 62.9% | 1169 | 100.0% | |
| Moderately | 747 | 37.5% | 1245 | 62.5% | 1992 | 100.0% | |
| Fairly good | 1098 | 41.6% | 1541 | 58.4% | 2639 | 100.0% | |
| Very good | 512 | 44.8% | 631 | 55.2% | 1143 | 100.0% | |
| Life Satisfaction | |||||||
| Very Dissatisfied | 33 | 37.9% | 54 | 62.1% | 87 | 100.0% | 5.400 p = 0.249 |
| Fairly dissatisfied | 35 | 39.8% | 53 | 60.2% | 88 | 100.0% | |
| Moderately | 47 | 34.8% | 88 | 65.2% | 135 | 100.0% | |
| Fairly satisfied | 1103 | 39.1% | 1719 | 60.9% | 2822 | 100.0% | |
| Very satisfied | 1628 | 41.3% | 2310 | 58.7% | 3938 | 100.0% | |
| Mental Health Last Month | |||||||
| Very bad | 18 | 46.2% | 21 | 53.8% | 39 | 100.0% | 25.614 p < 0.001 |
| Bad | 107 | 37.2% | 181 | 62.8% | 288 | 100.0% | |
| Moderately | 418 | 35.1% | 774 | 64.9% | 1192 | 100.0% | |
| Good | 1347 | 40.1% | 2014 | 59.9% | 3361 | 100.0% | |
| Very good | 956 | 43.7% | 1234 | 56.3% | 2190 | 100.0% | |
| LTSSN | |||||||
| Not needed | 2722 | 40.2% | 4046 | 59.8% | 6768 | 100.0% | 0.085 p = 0.771 |
| Needed | 124 | 41.1% | 178 | 58.9% | 302 | 100.0% | |
| ADL Score | |||||||
| 14 | 2274 | 41.6% | 3193 | 58.4% | 5467 | 100.0% | 25.090 p < 0.001 |
| 15 | 171 | 35.5% | 311 | 64.5% | 482 | 100.0% | |
| 16 | 67 | 30.2% | 155 | 69.8% | 222 | 100.0% | |
| 17 | 70 | 34.1% | 135 | 65.9% | 205 | 100.0% | |
| 18–27 | 191 | 36.4% | 334 | 63.6% | 525 | 100.0% | |
| ≥28 | 73 | 43.2% | 96 | 56.8% | 169 | 100.0% | |
| Model | χ2 | df | χ2/df | GFI | AGFI | CFI | RMSEA | ΔCFI | ΔRMSEA |
|---|---|---|---|---|---|---|---|---|---|
| M1 | 209.672 *** | 30 | 6.989 | 0.993 | 0.983 | 0.975 | 0.029 | --- | --- |
| M2 | 209.672 *** | 30 | 6.989 | 0.993 | 0.983 | 0.975 | 0.029 | 0 | 0 |
| M3 | 209.672 *** | 30 | 6.989 | 0.993 | 0.983 | 0.975 | 0.029 | 0 | 0 |
| M4 | 275.631 *** | 35 | 7.875 | 0.991 | 0.980 | 0.966 | 0.031 | 0.009 | 0.002 |
| M5 | 290.786 *** | 38 | 7.652 | 0.990 | 0.981 | 0.965 | 0.031 | 0.001 | 0 |
| Variable | Direct | Indirect | Total | |||
|---|---|---|---|---|---|---|
| Male | Female | Male | Female | Male | Female | |
| Socioeconomic Status→NLTSS | −0.117 *** | −0.252 *** | −0.113 *** | −0.064 *** | −0.230 *** | −0.316 *** |
| Mental Health→NLTSS | −0.400 *** | −0.300 *** | - | - | −0.400 *** | −0.300 *** |
| Socioeconomic Status→Mental Health | 0.281 *** | 0.214 *** | - | - | 0.281 *** | 0.214 *** |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kong, F.; Xu, L.; Kong, M.; Li, S.; Zhou, C.; Li, J.; Sun, L.; Qin, W. The Relationship between Socioeconomic Status, Mental Health, and Need for Long-Term Services and Supports among the Chinese Elderly in Shandong Province—A Cross-Sectional Study. Int. J. Environ. Res. Public Health 2019, 16, 526. https://doi.org/10.3390/ijerph16040526
Kong F, Xu L, Kong M, Li S, Zhou C, Li J, Sun L, Qin W. The Relationship between Socioeconomic Status, Mental Health, and Need for Long-Term Services and Supports among the Chinese Elderly in Shandong Province—A Cross-Sectional Study. International Journal of Environmental Research and Public Health. 2019; 16(4):526. https://doi.org/10.3390/ijerph16040526
Chicago/Turabian StyleKong, Fanlei, Lingzhong Xu, Mei Kong, Shixue Li, Chengchao Zhou, Jiajia Li, Long Sun, and Wenzhe Qin. 2019. "The Relationship between Socioeconomic Status, Mental Health, and Need for Long-Term Services and Supports among the Chinese Elderly in Shandong Province—A Cross-Sectional Study" International Journal of Environmental Research and Public Health 16, no. 4: 526. https://doi.org/10.3390/ijerph16040526
APA StyleKong, F., Xu, L., Kong, M., Li, S., Zhou, C., Li, J., Sun, L., & Qin, W. (2019). The Relationship between Socioeconomic Status, Mental Health, and Need for Long-Term Services and Supports among the Chinese Elderly in Shandong Province—A Cross-Sectional Study. International Journal of Environmental Research and Public Health, 16(4), 526. https://doi.org/10.3390/ijerph16040526






