Characterizing the Spatial Determinants and Prevention of Malaria in Kenya
Abstract
1. Introduction
2. Data and Methods
2.1. Data Sources
2.1.1. Kenyan Demographic and Health Surveys (DHS)
2.1.2. Kenya Malaria Indicator Survey
2.1.3. Data Availability
2.2. Methods
3. Results
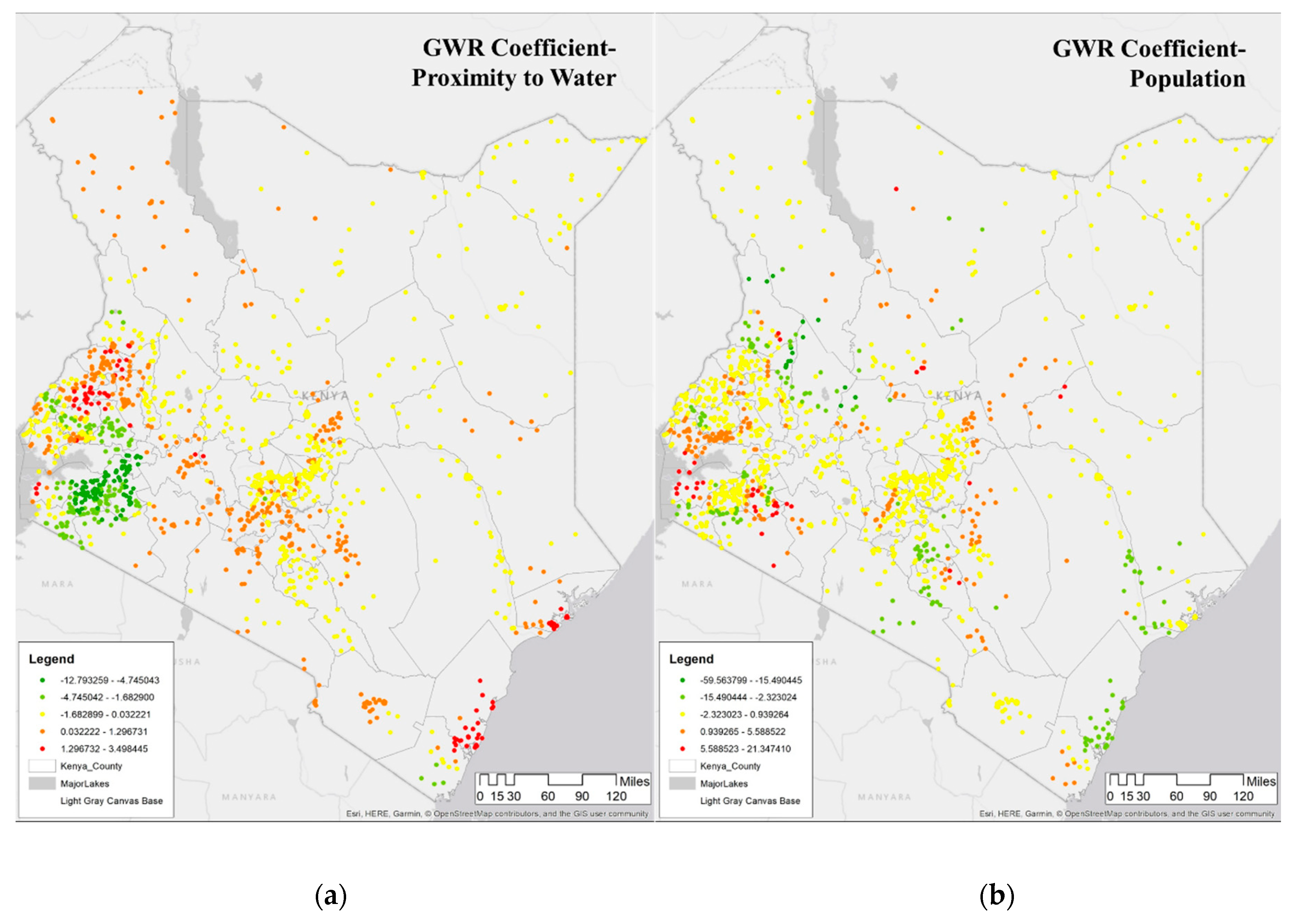
3.1. Examining Local Spatial Autocorrelation of Malaria
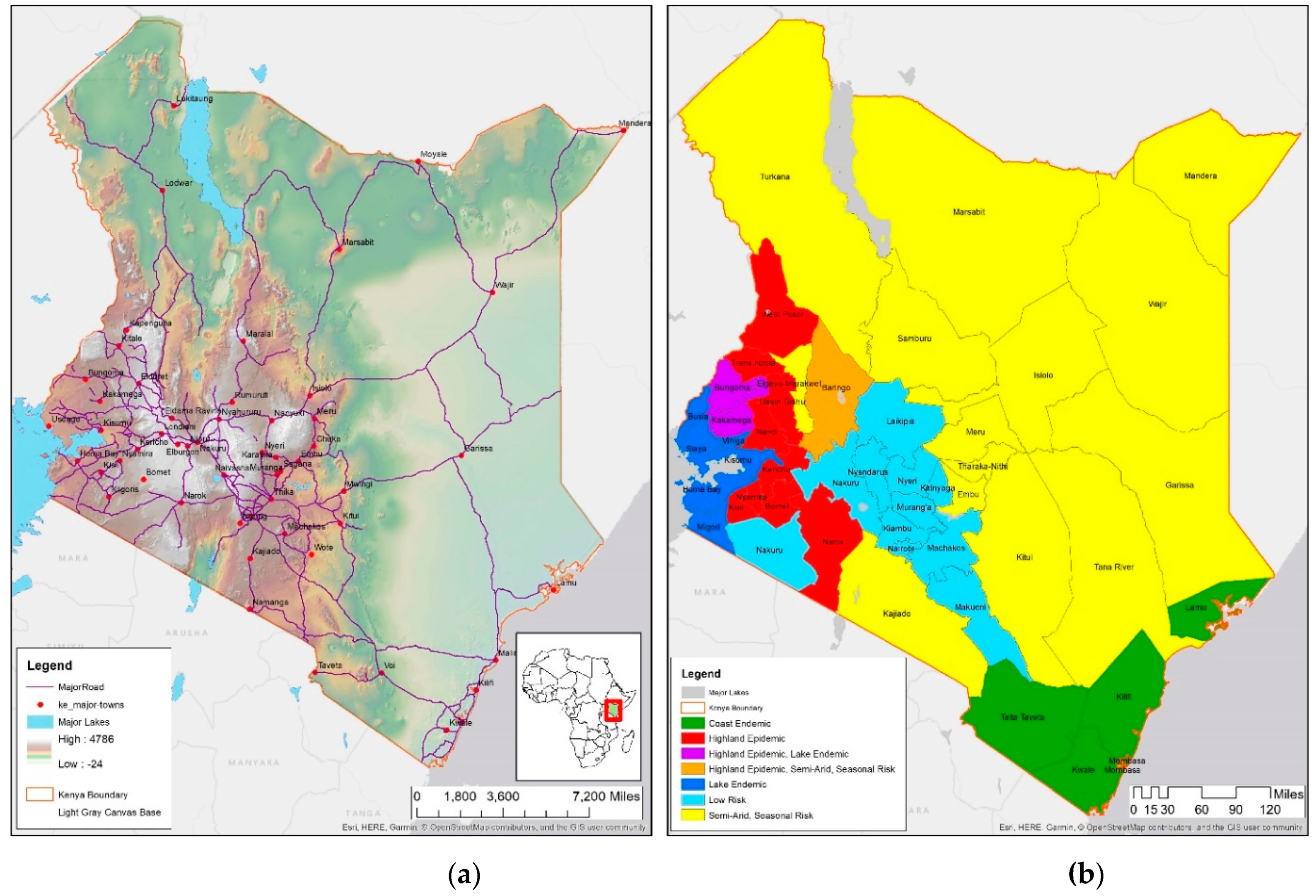
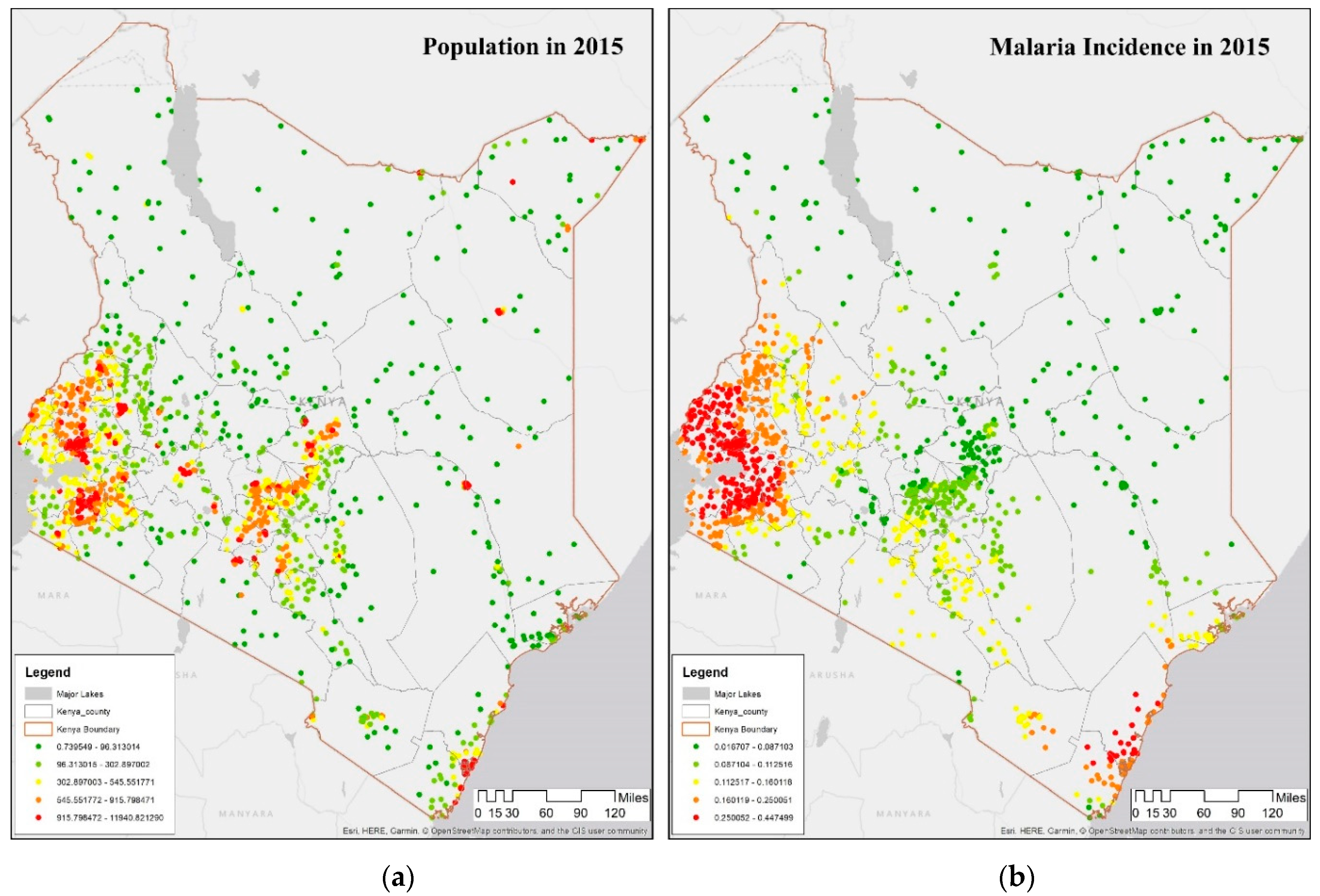
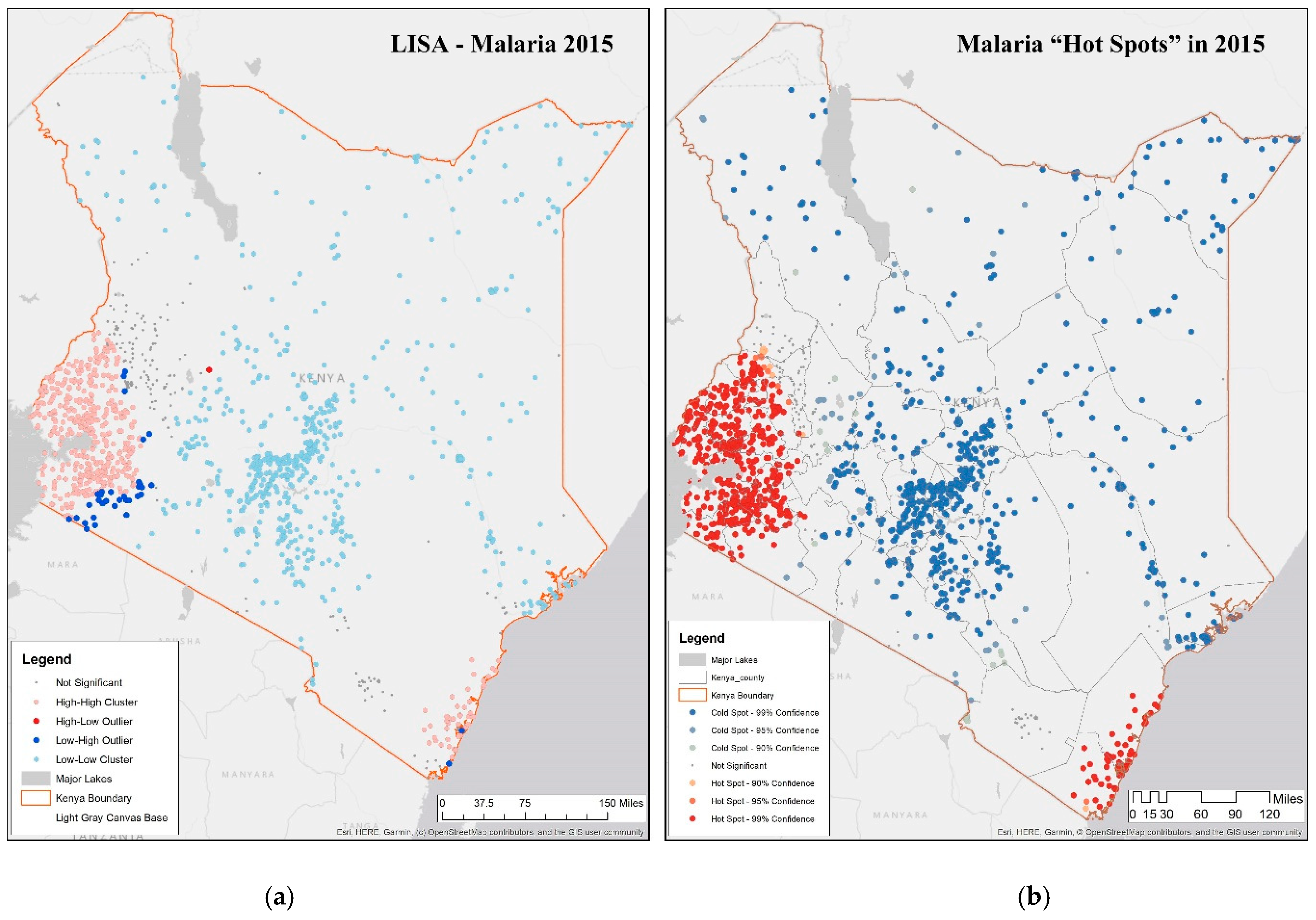
- A cluster with high values of malaria incidence rate per 1000 (high-high or hot spot) in all years of observation show that the Lake Victoria region is a noticeable hot spot; both rainfall and proximity to water are significantly higher than other regions of the country. A second smaller hot spot cluster is around Mombasa, on the east coast; these two hot spots appear across all four years with minor differences along the boundary regions, where there are some outliers. These two regions in 2015 coincide with DHS malaria zones called the coastal endemic and lake endemic regions, as shown in Figure 1b.
- A cluster with low values of malaria incidence rate per 1000 (low-low or cold spot) indicating low or no disease, located in the northern part of the country as well as around Nairobi; these regions are in the DHS semi-arid and seasonal risk areas. The only difference across the four periods is the appearance of some outliers on the outer edges of Lake Victoria endemic region indicating a “boundary” effect as locations at the boundary of 2 zones flip from being insignificant to some level of significance in some time-periods.
- An outlier of high value of malaria incidence rate per 1000 surrounded by a low value (high-low), is found in Baringo, which is in the highland epidemic region, with semi-arid, seasonal risk; this outlier is visible in 2015, as shown in Figure 3a. Such locations need scrutiny since people may be unprepared while at risk.
- An outlier of low value of malaria incidence rate per 1000 surrounded by a high value (low-high), is prevalent in Nakuru, lying in a low risk area neighboring Lake endemic malaria zone in the southwest. This pattern persists through all the time-periods.
- Non-significant values encompass all areas in which there were no significant associations, and are found in Trans Nzoia and Uasin Gishu, classified as being in the highland epidemic [49].
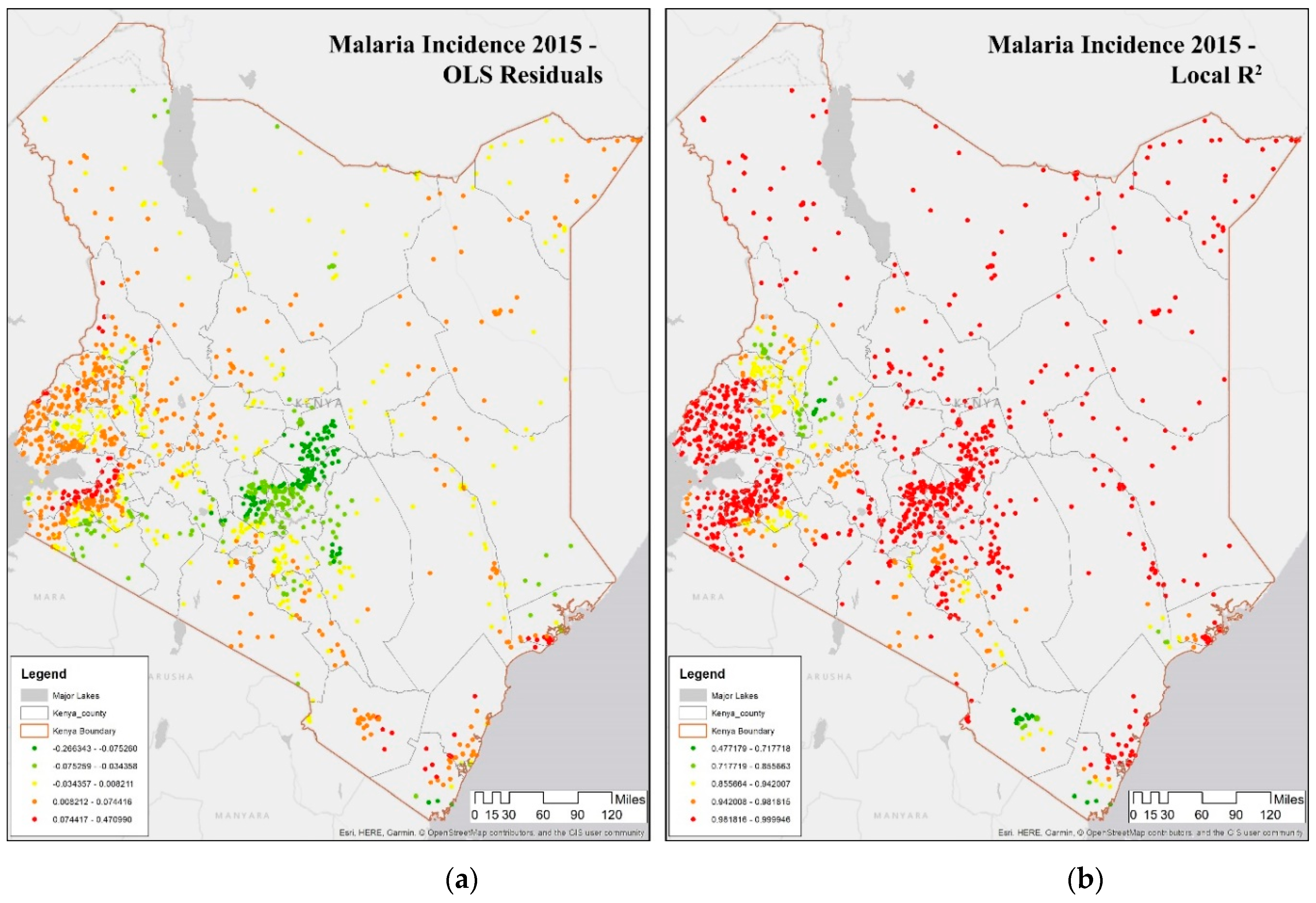
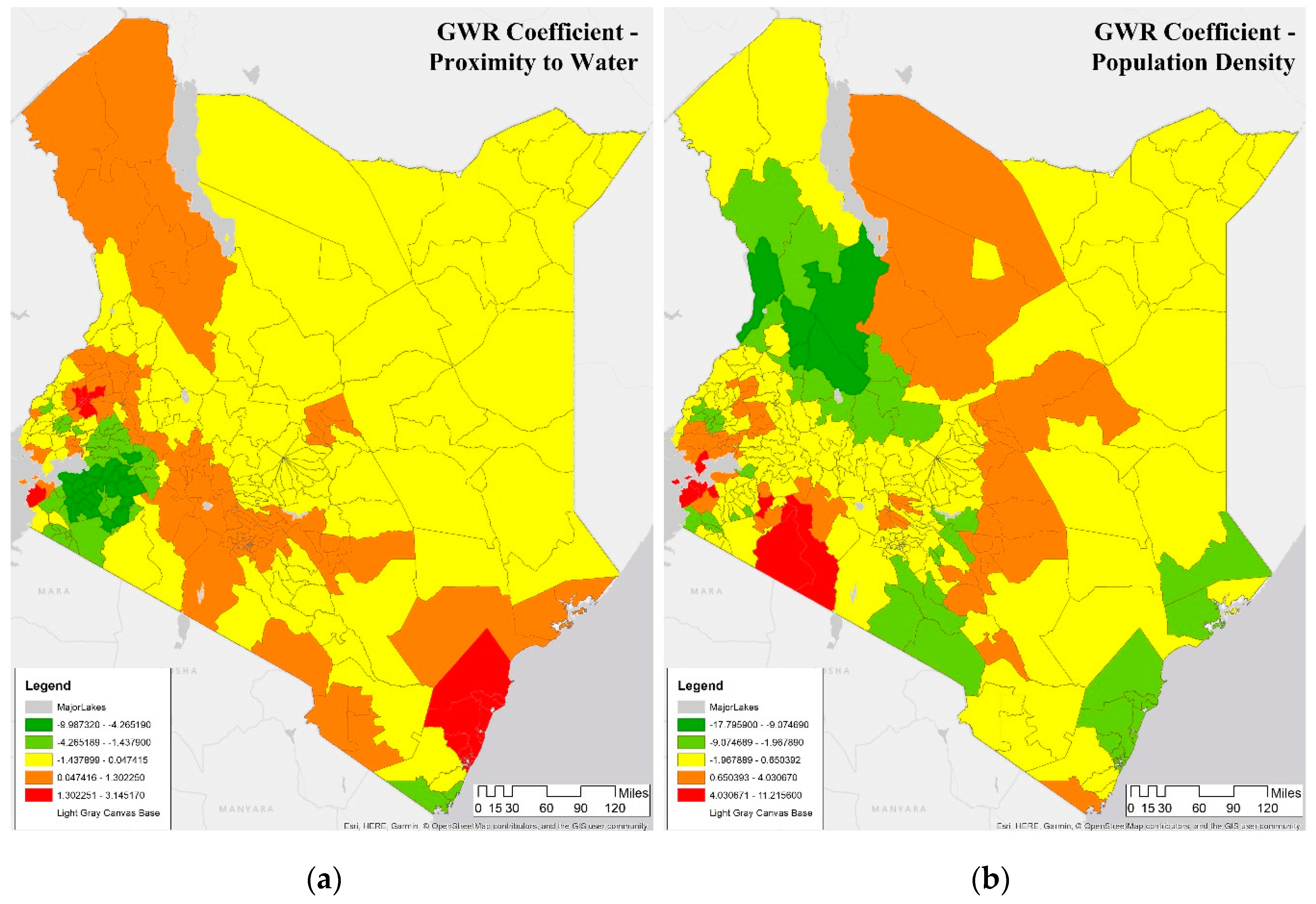
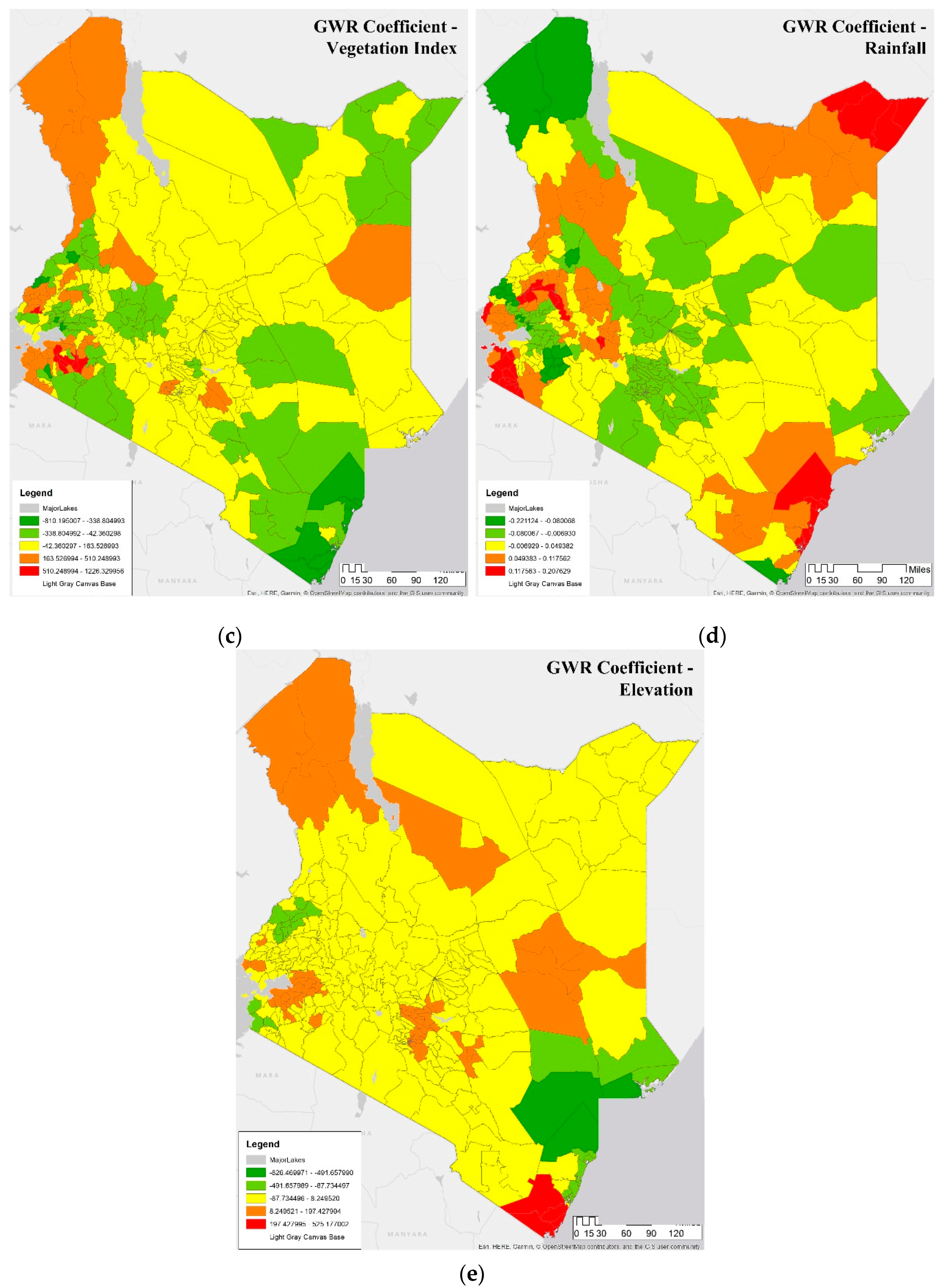
3.2. Spatial Determinants of Malaria
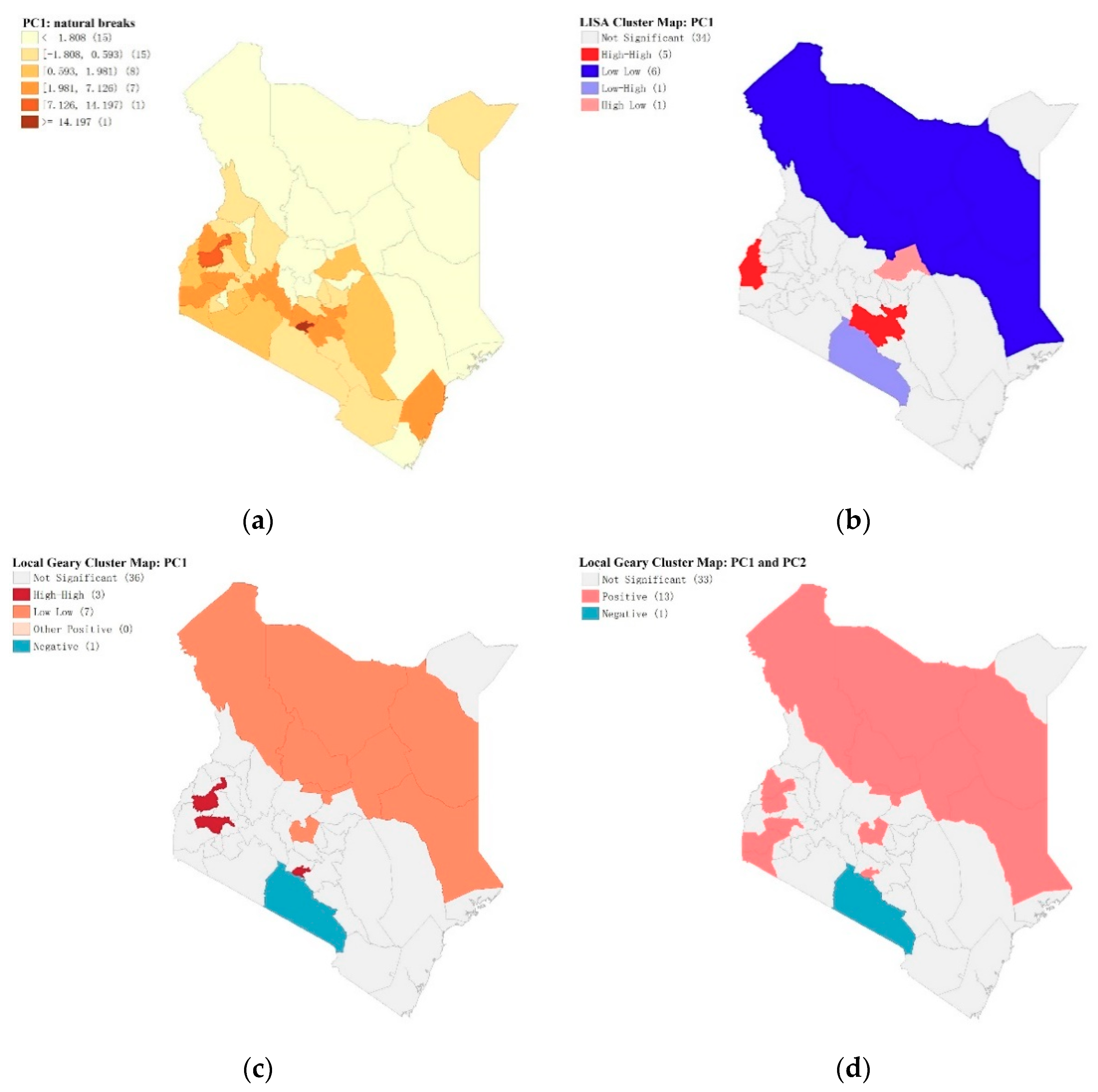
3.3. Spatial Analysis of Social, Demographics, Housing, and Behavior Characteristics of the Vulnerable Population
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- World Health Organization. World Malaria Report; World Health Organization: Geneva, Switzerland, 2018. [Google Scholar]
- Autino, B.; Noris, A.; Russo, R.; Castelli, F. Epidemiology of malaria in endemic areas. Mediterr. J. Hematol. Infect. Dis. 2012, 4, e2012060. [Google Scholar] [CrossRef] [PubMed]
- Tangpukdee, N.; Duangdee, C.; Wilairatana, P.; Krudsood, S. Malaria diagnosis: A brief review. Korean J. Parasitol. 2009, 47, 93. [Google Scholar] [CrossRef] [PubMed]
- UN DESA. Sustainable Development Goal 3: Ensuring Health Lives and Promote Well-Being for All at All Ages. 2015. Available online: https://sustainabledevelopment.un.org/sdg3 (accessed on 15 September 2019).
- Breman, J.G.; Egan, A.; Keusch, G.T. The intolerable burden of malaria: A new look at the numbers. Am. J. Trop. Med. Hyg. 2001, 64 (Suppl. 1–2), iv–vii. [Google Scholar] [CrossRef] [PubMed]
- Shretta, R.; Avanceña, A.L.; Hatefi, A. The economics of malaria control and elimination: A systematic review. Malar. J. 2016, 15, 593. [Google Scholar] [CrossRef]
- National Malaria Control Programme (NMCP); Kenya National Bureau of Statistics (KNBS); ICF International. Kenya Malaria Indicator Survey; NMCP, KNBS, ICF International: Nairobi, Kenya; Rockville, MD, USA, 2015. [Google Scholar]
- USAID. President’s Malaria Initiative, Kenya: Malaria Operational Plan FY 2018; USAID: Washington, DC, USA, 2018. [Google Scholar]
- Amboko, B.I.; Ayieko, P.; Ogero, M.; Julius, T.; Irimu, G.; English, M. Malaria investigation and treatment of children admitted to county hospitals in western Kenya. Malar. J. 2016, 15, 506. [Google Scholar] [CrossRef] [PubMed]
- Sultana, M.; Sheikh, N.; Mahumud, R.A.; Jahir, T.; Islam, Z.; Sarker, A.R. Prevalence and associated determinants of malaria parasites among Kenyan children. Trop. Med. Health 2017, 45, 25. [Google Scholar] [CrossRef] [PubMed]
- Kimani-Murage, E.W.; Fotso, J.C.; Egondi, T.; Abuya, B.; Elungata, P.; Ziraba, A.K.; Madise, N. Trends in childhood mortality in Kenya: The urban advantage has seemingly been wiped out. Health Place 2014, 29, 95–103. [Google Scholar] [CrossRef]
- Bashir, I.M.; Nyakoe, N.; van der Sande, M. Targeting remaining pockets of malaria transmission in Kenya to hasten progress towards national elimination goals: An assessment of prevalence and risk factors in children from the Lake endemic region. Malar. J. 2019, 18, 233. [Google Scholar] [CrossRef]
- Njuguna, P.; Maitland, K.; Nyaguara, A.; Mwanga, D.; Mogeni, P.; Mturi, N.; Lowe, B. Observational study: 27 years of severe malaria surveillance in Kilifi, Kenya. BMC Med. 2019, 17, 124. [Google Scholar] [CrossRef]
- Peprah, S.; Tenge, C.; Genga, I.O.; Mumia, M.; Were, P.A.; Kuremu, R.T.; Legason, I.D. A Cross-Sectional Population Study of Geographic, Age-Specific, and Household Risk Factors for Asymptomatic Plasmodium falciparum Malaria Infection in Western Kenya. Am. J. Trop. Med. Hyg. 2019, 100, 54–65. [Google Scholar] [CrossRef]
- Amek, N.O.; Van Eijk, A.; Lindblade, K.A.; Hamel, M.; Bayoh, N.; Gimnig, J.; Vounatsou, P. Infant and child mortality in relation to malaria transmission in KEMRI/CDC HDSS, Western Kenya: Validation of verbal autopsy. Malar. J. 2018, 17, 37. [Google Scholar] [CrossRef] [PubMed]
- Lee, E.H.; Olsen, C.H.; Koehlmoos, T.; Masuoka, P.; Stewart, A.; Bennett, J.W.; Mancuso, J. A cross-sectional study of malaria endemicity and health system readiness to deliver services in Kenya, Namibia and Senegal. Health Policy Plan. 2017, 32 (Suppl. 3), iii75–iii87. [Google Scholar] [CrossRef] [PubMed]
- Ondiba, I.M.; Oyieke, F.A.; Ong’amo, G.O.; Olumula, M.M.; Nyamongo, I.K.; Estambale, B.B. Malaria vector abundance is associated with house structures in Baringo County, Kenya. PLoS ONE 2018, 13, e0198970. [Google Scholar] [CrossRef] [PubMed]
- Sicuri, E.; Vieta, A.; Lindner, L.; Constenla, D.; Sauboin, C. The economic costs of malaria in children in three sub-Saharan countries: Ghana, Tanzania and Kenya. Malar. J. 2013, 12, 307. [Google Scholar] [CrossRef] [PubMed]
- Stuckey, E.M.; Stevenson, J.; Galactionova, K.; Baidjoe, A.Y.; Bousema, T.; Odongo, W.; Chitnis, N. Modeling the cost effectiveness of malaria control interventions in the highlands of western Kenya. PLoS ONE 2014, 9, e107700. [Google Scholar] [CrossRef]
- Were, V.; Buff, A.M.; Desai, M.; Kariuki, S.; Samuels, A.M.; Phillips-Howard, P.; Niessen, L.W. Trends in malaria prevalence and health related socioeconomic inequality in rural western Kenya: Results from repeated household malaria cross-sectional surveys from 2006 to 2013. BMJ Open 2019, 9, e033883. [Google Scholar] [CrossRef]
- Essendi, W.M.; Vardo-Zalik, A.M.; Lo, E.; Machani, M.G.; Zhou, G.; Githeko, A.K.; Afrane, Y.A. Epidemiological risk factors for clinical malaria infection in the highlands of Western Kenya. Malar. J. 2019, 18, 211. [Google Scholar] [CrossRef]
- Stuckey, E.M.; Stevenson, J.C.; Cooke, M.K.; Owaga, C.; Marube, E.; Oando, G.; Chitnis, N. Simulation of malaria epidemiology and control in the highlands of western Kenya. Malar. J. 2012, 11, 357. [Google Scholar] [CrossRef]
- Berk, J.; Adhvaryu, A. The impact of a novel franchise clinic network on access to medicines and vaccinations in Kenya: a cross-sectional study. BMJ Open 2012, 2, e000589. [Google Scholar] [CrossRef]
- Kisia, J.; Nelima, F.; Otieno, D.O.; Kiilu, K.; Emmanuel, W.; Sohani, S.; Akhwale, W. Factors associated with utilization of community health workers in improving access to malaria treatment among children in Kenya. Malar. J. 2012, 11, 248. [Google Scholar] [CrossRef]
- Hill, J.; Dellicour, S.; Bruce, J.; Ouma, P.; Smedley, J.; Otieno, P.; ter Kuile, F.O. Effectiveness of antenatal clinics to deliver intermittent preventive treatment and insecticide treated nets for the control of malaria in pregnancy in Kenya. PLoS ONE 2013, 8, e64913. [Google Scholar] [CrossRef] [PubMed]
- Siekmans, K.; Sohani, S.; Kisia, J.; Kiilu, K.; Wamalwa, E.; Nelima, F.; Ngindu, A. Community case management of malaria: A pro-poor intervention in rural Kenya. Int. Health 2013, 5, 196–204. [Google Scholar] [CrossRef] [PubMed]
- Ochomo, E.; Chahilu, M.; Cook, J.; Kinyari, T.; Bayoh, N.M.; West, P.; Mathenge, E. Insecticide-treated nets and protection against insecticide-resistant malaria vectors in western Kenya. Emerg. Infect. Dis. 2017, 23, 758. [Google Scholar] [CrossRef] [PubMed]
- Kibe, L.W.; Habluetzel, A.; Gachigi, J.K.; Kamau, A.W.; Mbogo, C.M. Exploring communities’ and health workers’ perceptions of indicators and drivers of malaria decline in Malindi, Kenya. Malar. World J. 2019, 8, 21. [Google Scholar]
- Matsushita, N.; Kim, Y.; Ng, C.F.S.; Moriyama, M.; Igarashi, T.; Yamamoto, K.; Otieno, W.; Minakawa, N.; Hashizume, M. Differences of Rainfall–Malaria Associations in Lowland and Highland in Western Kenya. Int. J. Environ. Res. Public Health 2019, 16, 19. [Google Scholar] [CrossRef]
- Le, P.V.V.; Kumar, P.; Ruiz, M.O.; Mbogo, C.; Muturi, E.J. Predicting the Direct and Indirect Impacts of Climate Change on Malaria in Coastal Kenya. PLoS ONE 2019, 14, e0211258. [Google Scholar] [CrossRef]
- Ministry of Health. Kenya Health Policy 2014–2030; Ministry of Health: Nairobi, Kenya, 2014. [Google Scholar]
- Carter, R.; Mendis, K.N.; Roberts, D. Spatial targeting of interventions against malaria. Bull. World Health Organ. 2000, 78, 1401–1411. [Google Scholar]
- Bousema, T.; Griffin, J.T.; Sauerwein, R.W.; Smith, D.L.; Churcher, T.S.; Takken, W.; Gosling, R. Hitting hotspots: Spatial targeting of malaria for control and elimination. PLoS Med. 2012, 9, e1001165. [Google Scholar] [CrossRef]
- Kakmeni, M.M.; Guimapi, R.Y.A.; Ndjomatchoua, F.T.; Pedro, S.A.; Mutunga, J.; Tonnang, H.E.Z. Spatial Panorama of Malaria Prevalence in Africa under Climate Change and Interventions Scenarios. Int. J. Health Geogr. 2018, 17, 2. [Google Scholar] [CrossRef]
- Macharia, P.M.; Giorgi, E.; Noor, A.M.; Waqo, E.; Kiptui, R.; Okiro, E.A.; Snow, R.W. Spatio-temporal Analysis of Plasmodium Falciparum Prevalence to Understand the Past and Chart the Future of Malaria Control in Kenya. Malar. J. 2018, 17, 340. [Google Scholar] [CrossRef]
- Walker, M.; Winskill, P.; Basanez, M.-G.; Mwangangi, J.M.; Mbogo, C.; Beier, J.C.; Midega, J.T. Temporal and Micro-Spatial Heterogeneity in the Distribution of Anopheles Vectors of Malaria along the Kenyan Coast. Parasites Vectors 2013, 6, 311. Available online: http://www.parasitesandvectors.com/content/6/1/311 (accessed on 14 November 2019). [CrossRef] [PubMed]
- Nmor, J.C.; Sunahara, T.; Goto, K.; Futami, K.; Sonye, G.; Akweywa, P.; Dida, G.; Minakawa, N. Topographic Models for Predictin Malaria Vector Breeding Habitatat: Potential tools for Vector Control Managers. Parasites Vectors 2013, 6, 14. Available online: http://www.parasitesandvectors.com/content/6/1/14 (accessed on 14 November 2019). [CrossRef] [PubMed]
- Amek, N.; Bayoh, N.; Hamel, M.; Lindblade, K.A.; Gimnig, J.; Laserson, K.F.; Slutsker, L.; Smith, T.; Vounatsou, P. Spatio-temporal Modelling of Sparse Geostatistical Malaria Sprorozite Rate Data using a Zero Inflated Binomial Model. Spat. Spatio-temporal Epidemiol. 2011, 2, 283–290. [Google Scholar] [CrossRef] [PubMed]
- Khagayi, S.; Amek, N.; Bigogo, G.; Odhiambo, F.; Vounatsou, P. Bayesian Spatio-temporal Modelling of Mortality in Relation to Malaria Incidence in Western Kenya. PLoS ONE 2017, 12, e0180516. [Google Scholar] [CrossRef]
- Bisanzio, D.; Mutuku, F.; LaBeaud, A.D.; Mungai, P.L.; Muinde, J.; Busaidy, H.; Mutoko, D.; King, C.H.; Kitron, U. Use if Prospective Hospital Surveillance Data to Define Spatiotemporal Heaterogeneity of Malaria Risk in Coastal Kenya. Malar. J. 2015, 14, 482. [Google Scholar] [CrossRef]
- Amek, N.; Bayoh, N.; Hamel, M.; Lindblade, K.A.; Gimnig, J.E.; Odhiambo, F.; Laserson, K.F.; Slutsker, L.; Smith, T.; Vounatsou, P. Spatial and Temporal Dynamics of Malaria Transmission in Rural Western Kenya. Parasites Vectors 2012, 5, 86. Available online: http://www.parasitesandvectors.com/content/5/1/86 (accessed on 14 November 2019). [CrossRef]
- Njuki, K. Land-Use Policy and Environmental Conservation in Kenya. East Afr. Agric. For. J. 1996, 62, 287–293. [Google Scholar] [CrossRef]
- Braile, L.W.; Keller, G.R.; Wendlandt, R.F.; Morgan, P.; Khan, M.A. The East African rift system. In Developments in Geotectonics; Elsevier: Amsterdam, The Netherlands, 2006. [Google Scholar]
- Mala, A.O.; Irungu, L.W.; Shililu, J.I.; Muturi, E.J.; Mbogo, C.M.; Njagi, J.K.; Githure, J.I. Plasmodium falciparum transmission and aridity: A Kenyan experience from the dry lands of Baringo and its implications for Anopheles arabiensis control. Malar. J. 2011, 10, 121. [Google Scholar] [CrossRef]
- Laurent, B.S.; Cooke, M.; Krishnankutty, S.M.; Asih, P.; Mueller, J.D.; Kahindi, S.; Cox, J. Molecular characterization reveals diverse and unknown malaria vectors in the Western Kenyan highlands. Am. J. Trop. Med. Hyg. 2016, 94, 327–335. [Google Scholar] [CrossRef]
- Ogola, E.O.; Chepkorir, E.; Sang, R.; Tchouassi, D.P. A previously unreported potential malaria vector in a dry ecology of Kenya. Parasites Vectors 2019, 12, 80. [Google Scholar] [CrossRef]
- Turkington, T.; Timbal, B.; Rahmat, R. The impact of global warming on sea surface temperature based El Niño–Southern Oscillation monitoring indices. Int. J. Climatol. 2019, 39, 1092–1103. [Google Scholar] [CrossRef]
- McGregor, G.; Ebi, K. El Niño southern oscillation (ENSO) and health: An overview for climate and health researchers. Atmosphere 2018, 9, 282. [Google Scholar] [CrossRef]
- US President’s Malaria Initiative Kenya. Available online: https://www.pmi.gov/docs/default-source/default-document-library/malaria-operational-plans/fy-2018/fy-2018-kenya-malaria-operational-plan.pdf (accessed on 15 September 2019).
- The Demographic and Health Surveys. Available online: https://dhsprogram.com/ (accessed on 15 September 2019).
- Burgert, C.R.; Colston, J.; Roy, T.; Zachary, B. Geographic Displacement Procedure and Georeferenced Data Release Policy for the Demographic and Health Surveys; DHS Program; ICF International: Calverton, MD, USA, 2013. [Google Scholar]
- Mayala, B.; Fish, T.D.; Eitelberg, D.; Dontamsetti, T. The DHS Program Geospatial Covariate Datasets Manual, 2nd ed.; ICF: Rockville, MD, USA, 2018. [Google Scholar]
- Tatem, A.J. WorldPop, open data for spatial demography. Sci. Data 2017, 4, 170004. [Google Scholar] [CrossRef] [PubMed]
- Climate Hazards Group. Climate Hazards Group InfraRed Precipitation with Station Data 2.0. Available online: http://chg.geog.ucsb.edu/data/chirps/index.html (accessed on 15 September 2019).
- Wessel, P.; Smith, W. A Global Self-Consistent, Hierarchical, High-Resolution Geography Database Version 2.3.7. Available online: http://www.soest.hawaii.edu/pwessel/gshhg/ (accessed on 15 September 2019).
- The Demographic and Health Surveys for Kenya. Available online: https://dhsprogram.com/data/dataset/Kenya_MIS_2015.cfm?flag=0 (accessed on 15 September 2019).
- Agresti, A. Categorical Data Analysis; John Wiley & Sons: New York, NY, USA, 2013. [Google Scholar]
- Anselin, L. Local Indicators of Spatial Association—LISA. Geogr. Anal. 1995, 27, 93–115. [Google Scholar] [CrossRef]
- Getis, A.; Ord, J.K. The Analysis of Spatial Association by Use of Distance Statistics. Geogr. Anal. 1992, 24, 189–206. [Google Scholar] [CrossRef]
- Ord, J.K.; Getis, A. Local spatial autocorrelation statistics: Distributional issues and an application. Geogr. Anal. 1995, 27, 286–306. [Google Scholar] [CrossRef]
- Generate Spatial Weights Matrix. Available online: http://desktop.arcgis.com/en/arcmap/10.3/tools/spatial-statistics-toolbox/generate-spatial-weights-matrix.htm (accessed on 15 October 2019).
- Anselin, L. Spatial Econometrics: Methods and Models (Vol. 4); Springer Science & Business Media: New York, NY, USA, 2013. [Google Scholar]
- Bivand, R.; Yu, D.; Nakaya, T.; Garcia-Lopez, M. Spgwr: Geographically Weighted Regression. R Package Version 0.6-31. R. Found. Stat. Comput. Available online: https://CRAN.R-project.org/package=spgwr (accessed on 3 September 2017).
- Bivand, R.S.; Pebesma, E.J.; Gomez-Rubio, V. Applied Spatial Data Analysis with R, 2nd ed.; Springer: New York, NY, USA, 2013. [Google Scholar]
- Brunsdon, C.; Fotheringham, S.; Charlton, M. Geographically weighted regression. J. R. Stat. Soc. Ser. D (Stat.) 1998, 47, 431–443. [Google Scholar] [CrossRef]
- Lu, B.; Brunsdon, C.; Charlton, M.; Harris, P. Geographically weighted regression with parameter-specific distance metrics. Int. J. Geogr. Inf. Sci. 2017, 31, 982–998. [Google Scholar] [CrossRef]
- Geoda. Available online: https://geodacenter.github.io/workbook/7a_clusters_1/lab7a.html (accessed on 15 October 2019).
- Anselin, L. A local indicator of multivariate spatial association: Extending Geary’s C. Geogr. Anal. 2019, 51, 133–150. [Google Scholar] [CrossRef]
- Mohamed MO, S.; Neukermans, G.; Kairo, J.G.; Dahdouh-Guebas, F.; Koedam, N. Mangrove forests in a peri-urban setting: The case of Mombasa (Kenya). Wetl. Ecol. Manag. 2009, 17, 243–255. [Google Scholar] [CrossRef]
- Alsop, Z. Malaria returns to Kenya’s highlands as temperatures rise. Lancet 2007, 370, 925–926. [Google Scholar] [CrossRef]
- Wandiga, S.O.; Opondo, M.; Olago, D.; Githeko, A.; Githui, F.; Marshall, M.; Yanda, P.Z. Vulnerability to epidemic malaria in the highlands of Lake Victoria basin: The role of climate change/variability, hydrology and socio-economic factors. Clim. Chang. 2010, 99, 473–497. [Google Scholar] [CrossRef]
- Chretien, J.P.; Anyamba, A.; Small, J.; Britch, S.; Sanchez, J.L.; Halbach, A.C.; Linthicum, K.J. Global climate anomalies and potential infectious disease risks: 2014–2015. PLoS Curr. 2015, 7. [Google Scholar] [CrossRef] [PubMed]
- Ndenga, B.A.; Simbauni, J.A.; Mbugi, J.P.; Githeko, A.K.; Fillinger, U. Productivity of malaria vectors from different habitat types in the western Kenya highlands. PLoS ONE 2011, 6, e19473. [Google Scholar] [CrossRef]
- Minakawa, N.; Dida, G.O.; Sonye, G.O.; Futami, K.; Njenga, S.M. Malaria vectors in Lake Victoria and adjacent habitats in western Kenya. PLoS ONE 2012, 7, e32725. [Google Scholar] [CrossRef]
- Achoki, T.; Miller-Petrie, M.K.; Glenn, S.D.; Kalra, N.; Lesego, A.; Gathecha, G.K.; Barsosio, H.C. Health disparities across the counties of Kenya and implications for policy makers, 1990–2016: A systematic analysis for the Global Burden of Disease Study 2016. Lancet Glob. Health 2019, 7, e81–e95. [Google Scholar] [CrossRef]
| Variables | Variable Loadings in 2015 | |
|---|---|---|
| PC1 | PC2 | |
| # of Mosquito Bed nets | 0.279199 | 0.0778586 |
| # Of Children Under 5 Slept under Net Last Night | 0.278166 | −0.175717 |
| # Of Children Slept under Net Last Night | 0.237191 | −0.337577 |
| # Of Children under 5 Had Fever | 0.253837 | −0.337189 |
| # Children under 5 Received Treatment | 0.257043 | −0.302508 |
| # Of Children under 5 | 0.274868 | −0.207184 |
| # Of Household Members | 0.294541 | −0.012094 |
| # Of Women | 0.286635 | 0.194498 |
| # Of Children | 0.258989 | −0.327962 |
| # Of Pregnant Women | 0.266416 | 0.15378 |
| Has Mosquito Bed Net for Sleeping | 0.285655 | 0.191331 |
| Given Away a Mosquito Net | 0.247505 | 0.291434 |
| Type of Place of Residence | 0.236617 | 0.476703 |
| Imp. of Having Children Sleep under a Tr. Net | 0.276666 | 0.288097 |
| Importance of components: | ||
| Standard deviation | 3.274989 | 1.255193 |
| Proportion of Variance | 0.766111 | 0.112536 |
| Cumulative Proportion | 0.766111 | 0.878647 |
| Values | 2000 | 2005 | 2010 | 2015 |
|---|---|---|---|---|
| Moran’s I | 0.666407 | 0.585607 | 0.642730 | 0.698402 |
| Expected Index: | 0.000732 | 0.000775 | 0.000775 | 0.000775 |
| Variance: | 0.000077 | 0.000085 | 0.000085 | 0.000086 |
| z-score: | 75.796087 | 63.427044 | 69.677760 | 75.567593 |
| p-value: | <0.001 | <0.001 | <0.001 | <0.001 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gopal, S.; Ma, Y.; Xin, C.; Pitts, J.; Were, L. Characterizing the Spatial Determinants and Prevention of Malaria in Kenya. Int. J. Environ. Res. Public Health 2019, 16, 5078. https://doi.org/10.3390/ijerph16245078
Gopal S, Ma Y, Xin C, Pitts J, Were L. Characterizing the Spatial Determinants and Prevention of Malaria in Kenya. International Journal of Environmental Research and Public Health. 2019; 16(24):5078. https://doi.org/10.3390/ijerph16245078
Chicago/Turabian StyleGopal, Sucharita, Yaxiong Ma, Chen Xin, Joshua Pitts, and Lawrence Were. 2019. "Characterizing the Spatial Determinants and Prevention of Malaria in Kenya" International Journal of Environmental Research and Public Health 16, no. 24: 5078. https://doi.org/10.3390/ijerph16245078
APA StyleGopal, S., Ma, Y., Xin, C., Pitts, J., & Were, L. (2019). Characterizing the Spatial Determinants and Prevention of Malaria in Kenya. International Journal of Environmental Research and Public Health, 16(24), 5078. https://doi.org/10.3390/ijerph16245078





