Designing Supportive Soundscapes for Nursing Home Residents with Dementia
Abstract
1. Introduction
2. State of the Art
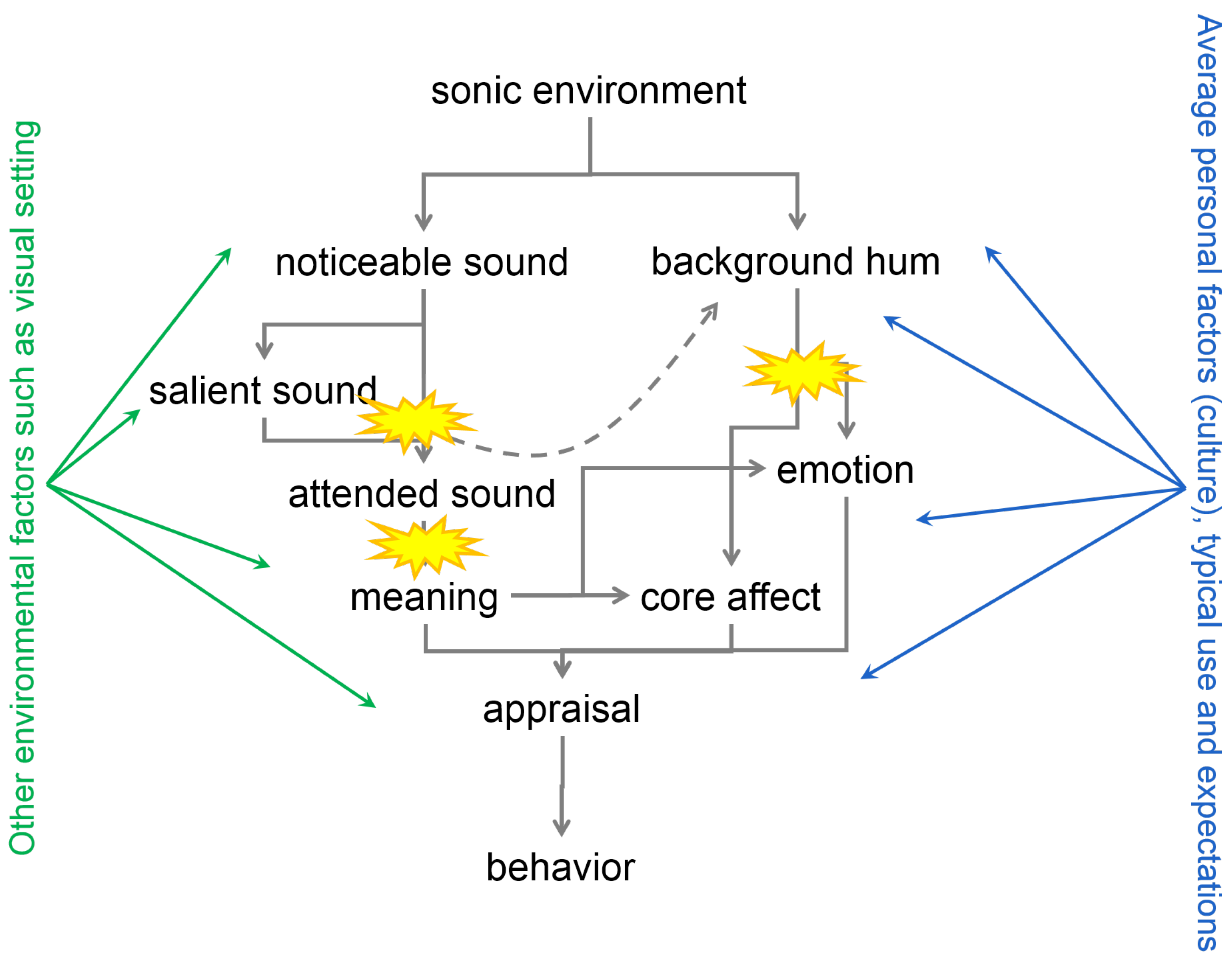
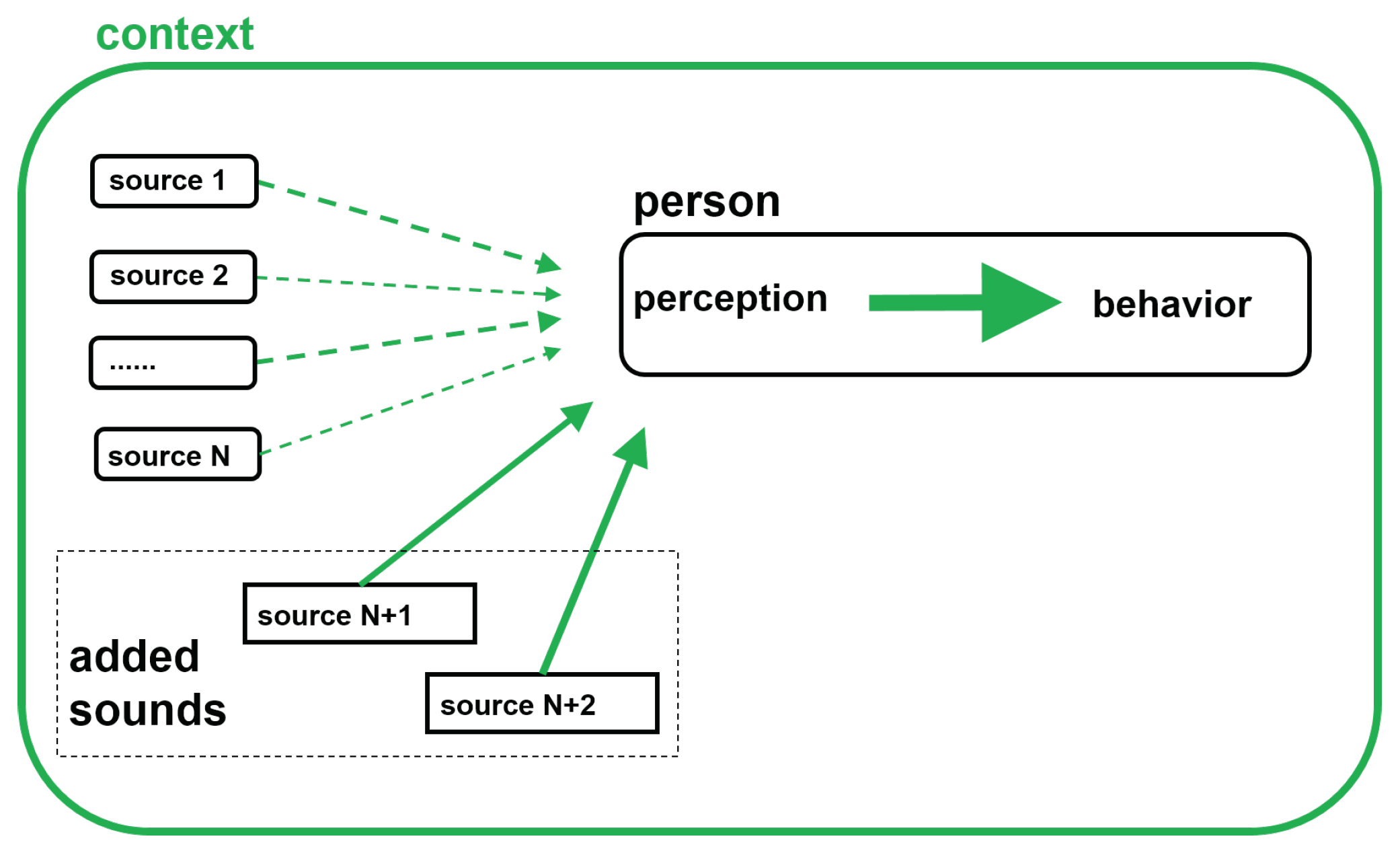
2.1. Perception: From Sonic Environment (Acoustic Scene) to Soundscape
2.2. Perceived Safety Theory
2.3. Effects of Subliminal and Attended Sound on Behavior
2.4. Changing Auditory Processing and Cognition with Age
2.5. Deviant Auditory Processing and Resulting Behavior in Dementia
- Impaired perception of sound features: this may manifest as cortical deafness or relatively selective ‘word deafness’ or auditory agnosia, more commonly described with progressive non fluent aphasia.
- Impaired recognition of sounds: due to erosion of semantic memory deficits of nonverbal sound recognition (auditory associative agnosia) like the recognition of environmental sounds are present in patients with semantic dementia, while for some individuals recognition of melodies preserves.
- Impaired perception of auditory scenes and objects: in this case difficulty following conversations and other sounds against background noise are reported, this may result in avoiding social interactions and a general dislike of complex auditory environments.
- Auditory hallucinations: Tinnitus as an elementary auditory hallucination is commonly reported by patients with semantic dementia. Muffled sounds or voices as hallucinations are often reported by patients with Lewy body dementia, as well as other musical hallucinations (comprising persistent familiar, basal tunes).
- Abnormal auditory behaviors: In this case, deviant emotional or hedonic behavioral responses to sound are observed in patients with dementia (due to impaired recognition of musical and nonverbal vocal emotions). Sound aversion is present in many patients of fronto-temporal dementia. On the other hand, abnormal craving for music (musicophilia) is associated with semantic dementia, these patients may show increased sensitivity to sound (hyperacusis).
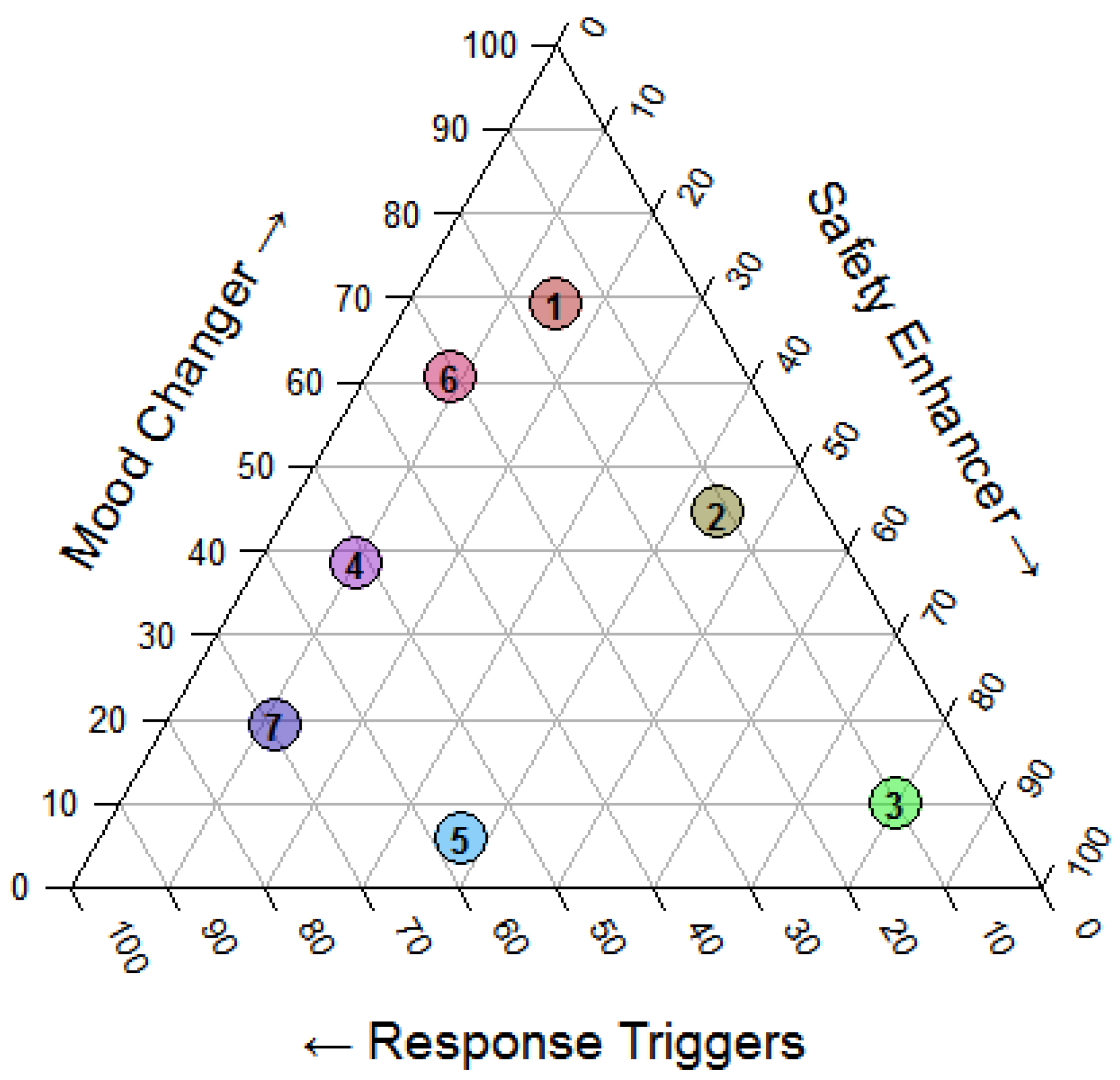
3. Soundscape Design Framework
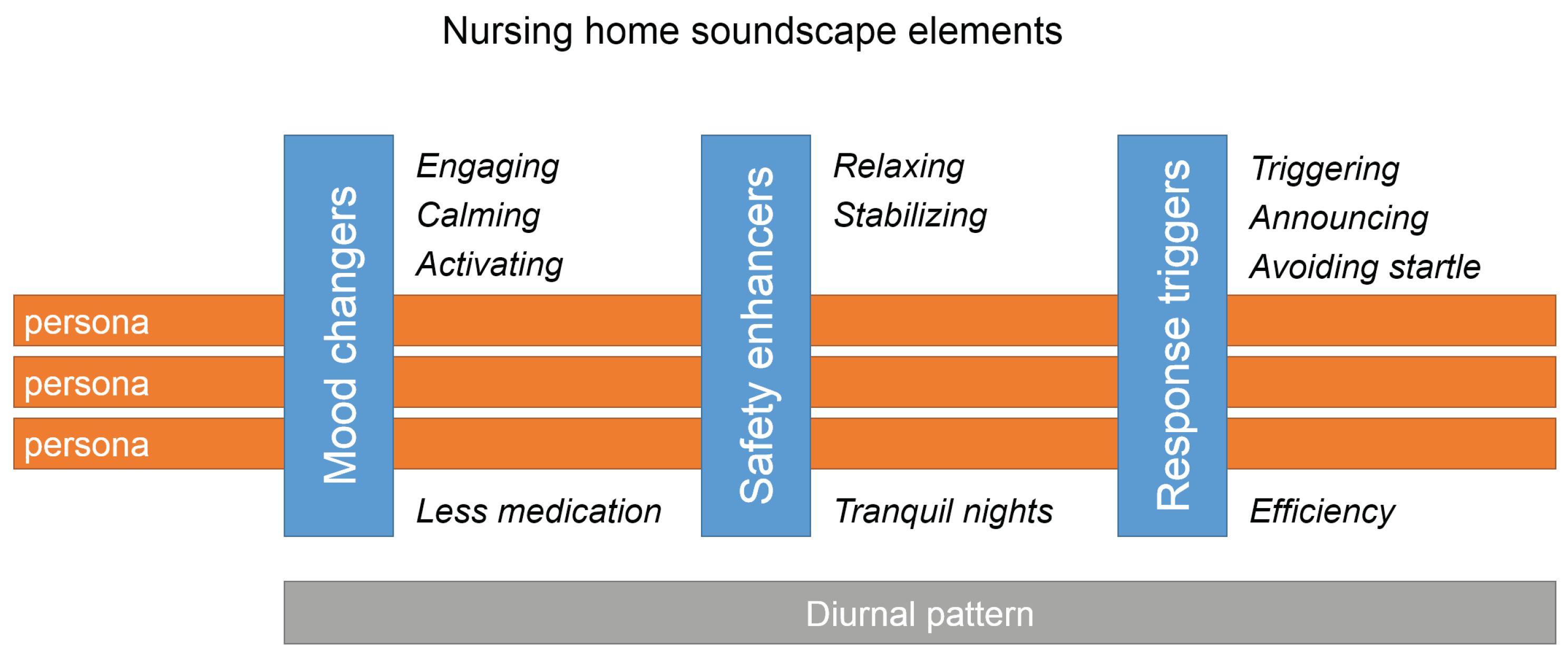
3.1. Designing for Effects
3.1.1. Mood Changers
3.1.2. Safety Enhancers
3.1.3. Response Triggers
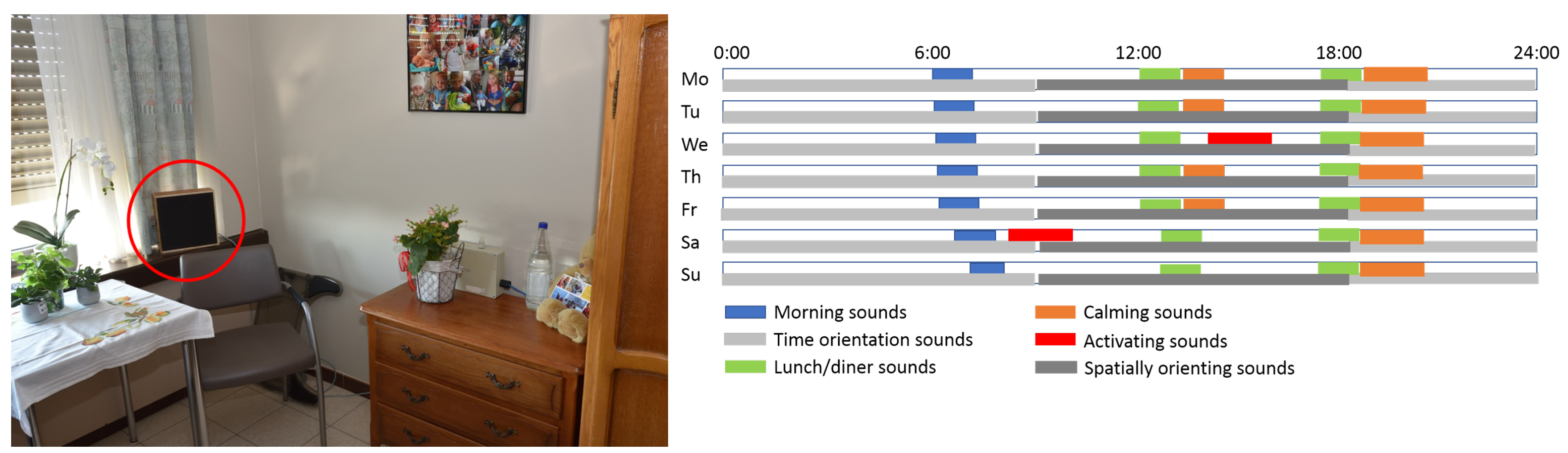
3.2. Soundscape Composition
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- World Health Organization. Dementia: A Public Health Priority; World Health Organization: Geneva, Switzerland, 2012. [Google Scholar]
- Prince, M.; Bryce, R.; Albanese, E.; Wimo, A.; Ribeiro, W.; Ferri, C.P. The global prevalence of dementia: A systematic review and metaanalysis. Alzheimer’s Dement. 2013, 9, 63–75. [Google Scholar] [CrossRef] [PubMed]
- Ferri, C.P.; Prince, M.; Brayne, C.; Brodaty, H.; Fratiglioni, L.; Ganguli, M.; Hall, K.; Hasegawa, K.; Hendrie, H.; Huang, Y.; et al. Global prevalence of dementia: A Delphi consensus study. Lancet 2005, 366, 2112–2117. [Google Scholar] [CrossRef]
- Livingston, G.; Sommerlad, A.; Orgeta, V.; Costafreda, S.G.; Huntley, J.; Ames, D.; Ballard, C.; Banerjee, S.; Burns, A.; Cohen-Mansfield, J.; et al. Dementia prevention, intervention, and care. Lancet 2017, 390, 2673–2734. [Google Scholar] [CrossRef]
- Dijkstra, K.; Pieterse, M.; Pruyn, A. Physical environmental stimuli that turn healthcare facilities into healing environments through psychologically mediated effects: Systematic review. J. Adv. Nurs. 2006, 56, 166–181. [Google Scholar] [CrossRef]
- ISO. Acoustics—Soundscape—Part 1: Definition and Conceptual Framework; Technical Report; ISO: Geneva, Switzerland, 2014. [Google Scholar]
- Graham, M.E. Re-socialising sound: Investigating sound, selfhood and intersubjectivity among people living with dementia in long-term care. Sound Stud. 2018, 5, 175–190. [Google Scholar] [CrossRef]
- Van den Bosch, K.A. Safe and Sound: Soundscape research in special needs care. Gron. Univ. Gron. 2015, 13, 61–68. [Google Scholar] [CrossRef]
- Van den Bosch, K.A.; Andringa, T.C.; Başkent, D.; Vlaskamp, C. The Role of Sound in Residential Facilities for People With Profound Intellectual and Multiple Disabilities. J. Policy Pract. Intellect. Disabil. 2016, 13, 61–68. [Google Scholar] [CrossRef]
- Aletta, F.; Botteldooren, D.; Thomas, P.; Vander Mynsbrugge, T.; De Vriendt, P.; Van de Velde, D.; Devos, P. Monitoring Sound Levels and Soundscape Quality in the Living Rooms of Nursing Homes: A Case Study in Flanders (Belgium). Appl. Sci. 2017, 7, 874. [Google Scholar] [CrossRef]
- Aletta, F.; Vander Mynsbrugge, T.; Van de Velde, D.; De Vriendt, P.; Thomas, P.; Filipan, K.; Botteldooren, D.; Devos, P. Awareness of ‘sound’ in nursing homes: A large-scale soundscape survey in Flanders (Belgium). Build. Acoust. 2018, 25, 43–59. [Google Scholar] [CrossRef]
- Kayser, C.; Petkov, C.I.; Lippert, M.; Logothetis, N.K. Mechanisms for Allocating Auditory Attention: An Auditory Saliency Map. Curr. Biol. 2005, 15, 1943–1947. [Google Scholar] [CrossRef]
- Oldoni, D.; Coensel, B.D.; Boes, M.; Rademaker, M.; Baets, B.D.; Renterghem, T.V.; Botteldooren, D. A computational model of auditory attention for use in soundscape research. J. Acoust. Soc. Am. 2013, 134, 852–861. [Google Scholar] [CrossRef] [PubMed]
- Kaya, E.M.; Elhilali, M. Modelling auditory attention. Philos. Trans. R. Soc. B Biol. Sci. 2017, 372, 20160101. [Google Scholar] [CrossRef] [PubMed]
- Talsma, D.; Senkowski, D.; Soto-Faraco, S.; Woldorff, M.G. The multifaceted interplay between attention and multisensory integration. Trends Cogn. Sci. 2010, 14, 400–410. [Google Scholar] [CrossRef] [PubMed]
- Raimbault, M.; Dubois, D. Urban soundscapes: Experiences and knowledge. Cities 2005, 22, 339–350. [Google Scholar] [CrossRef]
- Västfjäll, D. Emotion induction through music: A review of the musical mood induction procedure. Music. Sci. 2001, 5, 173–211. [Google Scholar] [CrossRef]
- Botteldooren, D.; Coensel, B.D.; Muer, T.D. The temporal structure of urban soundscapes. J. Sound Vib. 2006, 292, 105–123. [Google Scholar] [CrossRef]
- Västfjäll, D. Emotional Reactions to Sounds without Meaning. Psychology 2012, 3, 606–609. [Google Scholar] [CrossRef]
- Pearce, M.T.; Wiggins, G.A. Auditory Expectation: The Information Dynamics of Music Perception and Cognition. Top. Cogn. Sci. 2012, 4, 625–652. [Google Scholar] [CrossRef]
- Filipan, K.; Boes, M.; Coensel, B.D.; Domitrovic, H.; Botteldooren, D. Identifying and recognizing noticeable sounds from physical measurements and their effect on soundscape. In Proceedings of the 10th European Congress and Exposition on Noise Control Engineering Euronoise 2015, Maastricht, The Netherlands, 31 May–3 June 2015. [Google Scholar]
- Maslow, A.H. A theory of human motivation. Psychol. Rev. 1943, 50, 370–396. [Google Scholar] [CrossRef]
- Brosschot, J.F.; Verkuil, B.; Thayer, J.F. Exposed to events that never happen: Generalized unsafety, the default stress response, and prolonged autonomic activity. Neurosci. Biobehav. Rev. 2017, 74, 287–296. [Google Scholar] [CrossRef]
- Brosschot, J.; Verkuil, B.; Thayer, J. Generalized Unsafety Theory of Stress: Unsafe Environments and Conditions, and the Default Stress Response. Int. J. Environ. Res. Public Health 2018, 15, 464. [Google Scholar] [CrossRef] [PubMed]
- Schäfer, T.; Huron, D.; Shanahan, D.; Sedlmeier, P. The sounds of safety: Stress and danger in music perception. Front. Psychol. 2015, 6. [Google Scholar] [CrossRef] [PubMed]
- Iyendo, T.O. Exploring the effect of sound and music on health in hospital settings: A narrative review. Int. J. Nurs. Stud. 2016, 63, 82–100. [Google Scholar] [CrossRef] [PubMed]
- Iyendo, T.O. Sound as a supportive design intervention for improving health care experience in the clinical ecosystem: A qualitative study. Complement. Ther. Clin. Pract. 2017, 29, 58–96. [Google Scholar] [CrossRef] [PubMed]
- Sloboda, J.A.; ONeill, S.A.; Ivaldi, A. Functions of Music in Everyday Life: An Exploratory Study Using the Experience Sampling Method. Music. Sci. 2001, 5, 9–32. [Google Scholar] [CrossRef]
- Salamon, J.; Jacoby, C.; Bello, J.P. A Dataset and Taxonomy for Urban Sound Research. In Proceedings of the ACM International Conference on Multimedia, MM 14, Orlando, FL, USA, 3–7 November 2014. [Google Scholar] [CrossRef]
- Lindborg, P. A taxonomy of sound sources in restaurants. Appl. Acoust. 2016, 110, 297–310. [Google Scholar] [CrossRef]
- Alvarsson, J.J.; Wiens, S.; Nilsson, M.E. Stress Recovery during Exposure to Nature Sound and Environmental Noise. Int. J. Environ. Res. Public Health 2010, 7, 1036. [Google Scholar] [CrossRef]
- Benfield Jacob, A.; Derrick, T.B.; Peter, N.; Joshua, S. Natural Sound Facilitates Mood Recovery. Ecopsychology 2014, 6, 183–188. [Google Scholar] [CrossRef]
- Kaplan, S. The restorative benefits of nature: Toward an integrative framework. J. Environ. Psychol. 1995, 15, 169–182. [Google Scholar] [CrossRef]
- Mackrill, J.; Jennings, P.; Cain, R. Exploring positive hospital ward soundscape interventions. Appl. Ergon. 2014, 45, 1454–1460. [Google Scholar] [CrossRef]
- Mackrill, J.; Cain, R.; Jennings, P. Experiencing the hospital ward soundscape: Towards a model. J. Environ. Psychol. 2013, 36, 1–8. [Google Scholar] [CrossRef]
- Ratcliffe, E.; Gatersleben, B.; Sowden, P.T. Bird sounds and their contributions to perceived attention restoration and stress recovery. J. Environ. Psychol. 2013, 36, 221–228. [Google Scholar] [CrossRef]
- Ratcliffe, E.; Gatersleben, B.; Sowden, P.T. Associations with bird sounds: How do they relate to perceived restorative potential? J. Environ. Psychol. 2016, 47, 136–144. [Google Scholar] [CrossRef]
- Axelsson, Ö.; Nilsson, M.E.; Berglund, B. A principal components model of soundscape perception. J. Acoust. Soc. Am. 2010, 128, 2836–2846. [Google Scholar] [CrossRef] [PubMed]
- Gates, G.A.; Mills, J.H. Presbycusis. Lancet 2005, 366, 1111–1120. [Google Scholar] [CrossRef]
- Stothart, G.; Kazanina, N. Auditory perception in the aging brain: The role of inhibition and facilitation in early processing. Neurobiol. Aging 2016, 47, 23–34. [Google Scholar] [CrossRef] [PubMed]
- Martin, J.S.; Jerger, J.F. Some effects of aging on central auditory processing. J. Rehabil. Res. Dev. 2005, 42, 25–44. [Google Scholar] [CrossRef]
- Pichora-Fuller, M.K.; Singh, G. Effects of age on auditory and cognitive processing: Implications for hearing aid fitting and audiologic rehabilitation. Trends Amplif. 2006, 10, 29–59. [Google Scholar] [CrossRef]
- Howarth, A.; Shone, G.R. Ageing and the auditory system. Postgrad. Med. J. 2006, 82, 166–171. [Google Scholar] [CrossRef]
- Ross, B.; Fujioka, T.; Tremblay, K.L.; Picton, T.W. Aging in Binaural Hearing Begins in Mid-Life: Evidence from Cortical Auditory-Evoked Responses to Changes in Interaural Phase. J. Neurosci. 2007, 27, 11172–11178. [Google Scholar] [CrossRef]
- Bronkhorst, A.W.; Houtgast, T. Auditory distance perception in rooms. Nature 1999, 397, 517–520. [Google Scholar] [CrossRef] [PubMed]
- Kolarik, A.J.; Moore, B.C.J.; Zahorik, P.; Cirstea, S.; Pardhan, S. Auditory distance perception in humans: A review of cues, development, neuronal bases, and effects of sensory loss. Atten. Percept. Psychophys. 2016, 78, 373–395. [Google Scholar] [CrossRef]
- Ahveninen, J.; Huang, S.; Nummenmaa, A.; Belliveau, J.W.; Hung, A.Y.; Jääskeläinen, I.P.; Rauschecker, J.P.; Rossi, S.; Tiitinen, H.; Raij, T. Evidence for distinct human auditory cortex regions for sound location versus identity processing. Nat. Commun. 2013, 4, 2585. [Google Scholar] [CrossRef] [PubMed]
- Fortunato, S.; Forli, F.; Guglielmi, V.; De Corso, E.; Paludetti, G.; Berrettini, S.; Fetoni, A.R. A review of new insights on the association between hearing loss and cognitive decline in ageing. Acta Otorhinolaryngol. Ital. 2016, 36, 155–166. [Google Scholar] [PubMed]
- Wallhagen, M.I.; Strawbridge, W.J.; Shema, S.J.; Kurata, J.; Kaplan, G.A. Comparative Impact of Hearing and Vision Impairment On Subsequent Functioning. J. Am. Geriatr. Soc. 2001, 49, 1086–1092. [Google Scholar] [CrossRef]
- Meister, H.; Rählmann, S.; Walger, M.; Margolf-Hackl, S.; Kießling, J. Hearing aid fitting in older persons with hearing impairment: The influence of cognitive function, age, and hearing loss on hearing aid benefit. Clin. Interv. Aging 2015, 10, 435. [Google Scholar] [CrossRef]
- Hardy, C.J.D.; Marshall, C.R.; Golden, H.L.; Clark, C.N.; Mummery, C.J.; Griffiths, T.D.; Bamiou, D.E.; Warren, J.D. Hearing and dementia. J. Neurol. 2016, 263, 2339–2354. [Google Scholar] [CrossRef]
- Goll, J.C.; Kim, L.G.; Hailstone, J.C.; Lehmann, M.; Buckley, A.; Crutch, S.J.; Warren, J.D. Auditory object cognition in dementia. Neuropsychologia 2011, 49, 2755–2765. [Google Scholar] [CrossRef]
- Goll, J.C.; Kim, L.G.; Ridgway, G.R.; Hailstone, J.C.; Lehmann, M.; Buckley, A.H.; Crutch, S.J.; Warren, J.D. Impairments of auditory scene analysis in Alzheimer’s disease. Brain J. Neurol. 2012, 135, 190–200. [Google Scholar] [CrossRef]
- Fletcher, P.D.; Nicholas, J.M.; Downey, L.E.; Golden, H.L.; Clark, C.N.; Pires, C.; Agustus, J.L.; Mummery, C.J.; Schott, J.M.; Rohrer, J.D.; et al. A physiological signature of sound meaning in dementia. Cortex 2016, 77, 13–23. [Google Scholar] [CrossRef]
- Vander Mynsbrugge, T.; Van de Velde, D.; Aletta, F.; Botteldooren, D.; Devos, P.; De Vriendt, P. A model of soundscape for people with dementia living in nursing homes. In Proceedings of the WFOT Congress 2018, Cape Town, South Africa, 21–25 May 2018. [Google Scholar]
- De Vriendt, P.; Vander Mynsbrugge, T.; Aletta, F.; Botteldooren, D.; Devos, P.; Van de Velde, D. Developing a method for soundscape design for people with dementia living in nursing homes: Validation of four persona. Int. Psychogeriatr. 2019, 31, 58. [Google Scholar]
- Russell, J.A. A circumplex model of affect. J. Personal. Soc. Psychol. 1980, 39, 1161–1178. [Google Scholar] [CrossRef]
- Posner, J.; Russell, J.A.; Peterson, B.S. The circumplex model of affect: An integrative approach to affective neuroscience, cognitive development, and psychopathology. Dev. Psychopathol. 2005, 17. [Google Scholar] [CrossRef] [PubMed]
- Putkinen, V.; Makkonen, T.; Eerola, T. Music-induced positive mood broadens the scope of auditory attention. Soc. Cogn. Affect. Neurosci. 2017, 12, 1159–1168. [Google Scholar] [CrossRef]
- Peng, J.; Zeng, Y.; Zhao, L.; Zeng, J. An investigation of acoustical environments in the elderly care facilities. Appl. Acoust. 2018, 137, 45–50. [Google Scholar] [CrossRef]
- Brown, J.; Fawzi, W.; Shah, A.; Joyce, M.; Holt, G.; McCarthy, C.; Stevenson, C.; Marange, R.; Shakes, J.; Solomon-Ayeh, K. Low stimulus environments: Reducing noise levels in continuing care. BMJ Qual. Improv. Rep. 2016, 5, u207447-w4214. [Google Scholar] [CrossRef]
- Jerlehag, C.; Lee, P.J.; Park, S.H.; Jones, T.; Carroll, N. Acoustic environments of patient room in a typical geriatric ward. Appl. Acoust. 2018, 133, 186–193. [Google Scholar] [CrossRef]
- Riche, Y.; Mackay, W. PeerCare: Supporting Awareness of Rhythms and Routines for Better Aging in Place. Comput. Supported Coop. Work 2010, 19, 73–104. [Google Scholar] [CrossRef]
- Devos, P.; Aletta, F.; Thomas, P.; Filipan, K.; Petrovic, M.; Botteldooren, D.; Vander Mynsbrugge, T.; Van de Velde, D.; De Vriendt, P. Soundscape Design for Management of Behavioral Disorders: A Pilot Study among Nursing Home Residents with Dementia. In Proceedings of the Internoise 2018 Conference, Chicago, IL, USA, 26–29 August 2018. [Google Scholar]
- Thomas, P.; Aletta, F.; Vander Mynsbrugge, T.; Filipan, K.; Dijckmans, A.; De Geetere, L.; Botteldooren, D.; Petrovic, M.; De Vriendt, P.; Van de Velde, D.; et al. Evaluation and improvement of the acoustic comfort in nursing homes: A case study in Flanders, Belgium. In Proceedings of the 11th European Congress and Exposition on Noise Control Engineering (Euronoise 2018), Crete, Greece, 27–31 May 2018; pp. 405–412. [Google Scholar]
- Thomas, P.; Aletta, F.; Filipan, K.; Mynsbrugge, T.V.; Geetere, L.D.; Dijckmans, A.; Botteldooren, D.; Petrovic, M.; de Velde, D.V.; Vriendt, P.D.; et al. Noise environments in nursing homes: An overview of the literature and a case study in Flanders with quantitative and qualitative methods. Appl. Acoust. 2020, 159, 107103. [Google Scholar] [CrossRef]
- Brinker, J.K. Rumination and reminiscence in older adults: Implications for clinical practice. Eur. J. Ageing 2013, 10, 223–227. [Google Scholar] [CrossRef]
- Sayin, E.; Krishna, A.; Ardelet, C.; Briand Decré, G.; Goudey, A. “Sound and safe”: The effect of ambient sound on the perceived safety of public spaces. Int. J. Res. Mark. 2015, 32, 343–353. [Google Scholar] [CrossRef]
- Andringa, T.C.; Lanser, J.J.L. How pleasant sounds promote and annoying sounds impede health: A cognitive approach. Int. J. Environ. Res. Public Health 2013, 10, 1439–1461. [Google Scholar] [CrossRef] [PubMed]
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Devos, P.; Aletta, F.; Thomas, P.; Petrovic, M.; Vander Mynsbrugge, T.; Van de Velde, D.; De Vriendt, P.; Botteldooren, D. Designing Supportive Soundscapes for Nursing Home Residents with Dementia. Int. J. Environ. Res. Public Health 2019, 16, 4904. https://doi.org/10.3390/ijerph16244904
Devos P, Aletta F, Thomas P, Petrovic M, Vander Mynsbrugge T, Van de Velde D, De Vriendt P, Botteldooren D. Designing Supportive Soundscapes for Nursing Home Residents with Dementia. International Journal of Environmental Research and Public Health. 2019; 16(24):4904. https://doi.org/10.3390/ijerph16244904
Chicago/Turabian StyleDevos, Paul, Francesco Aletta, Pieter Thomas, Mirko Petrovic, Tara Vander Mynsbrugge, Dominique Van de Velde, Patricia De Vriendt, and Dick Botteldooren. 2019. "Designing Supportive Soundscapes for Nursing Home Residents with Dementia" International Journal of Environmental Research and Public Health 16, no. 24: 4904. https://doi.org/10.3390/ijerph16244904
APA StyleDevos, P., Aletta, F., Thomas, P., Petrovic, M., Vander Mynsbrugge, T., Van de Velde, D., De Vriendt, P., & Botteldooren, D. (2019). Designing Supportive Soundscapes for Nursing Home Residents with Dementia. International Journal of Environmental Research and Public Health, 16(24), 4904. https://doi.org/10.3390/ijerph16244904





