‘Not to Be Harsh but Try Less to Relate to ‘the Teens’ and You’ll Relate to Them More’: Co-Designing Obesity Prevention Text Messages with Adolescents
Abstract
1. Introduction
2. Materials and Methods
2.1. Design
2.2. Phase 1: Initial Development of Text Messages
2.3. Phase 2: User Acceptance Testing
2.4. Phase 3: Final Development and Platform Testing
3. Results
3.1. Phase 1: Initial Development of Text Messages
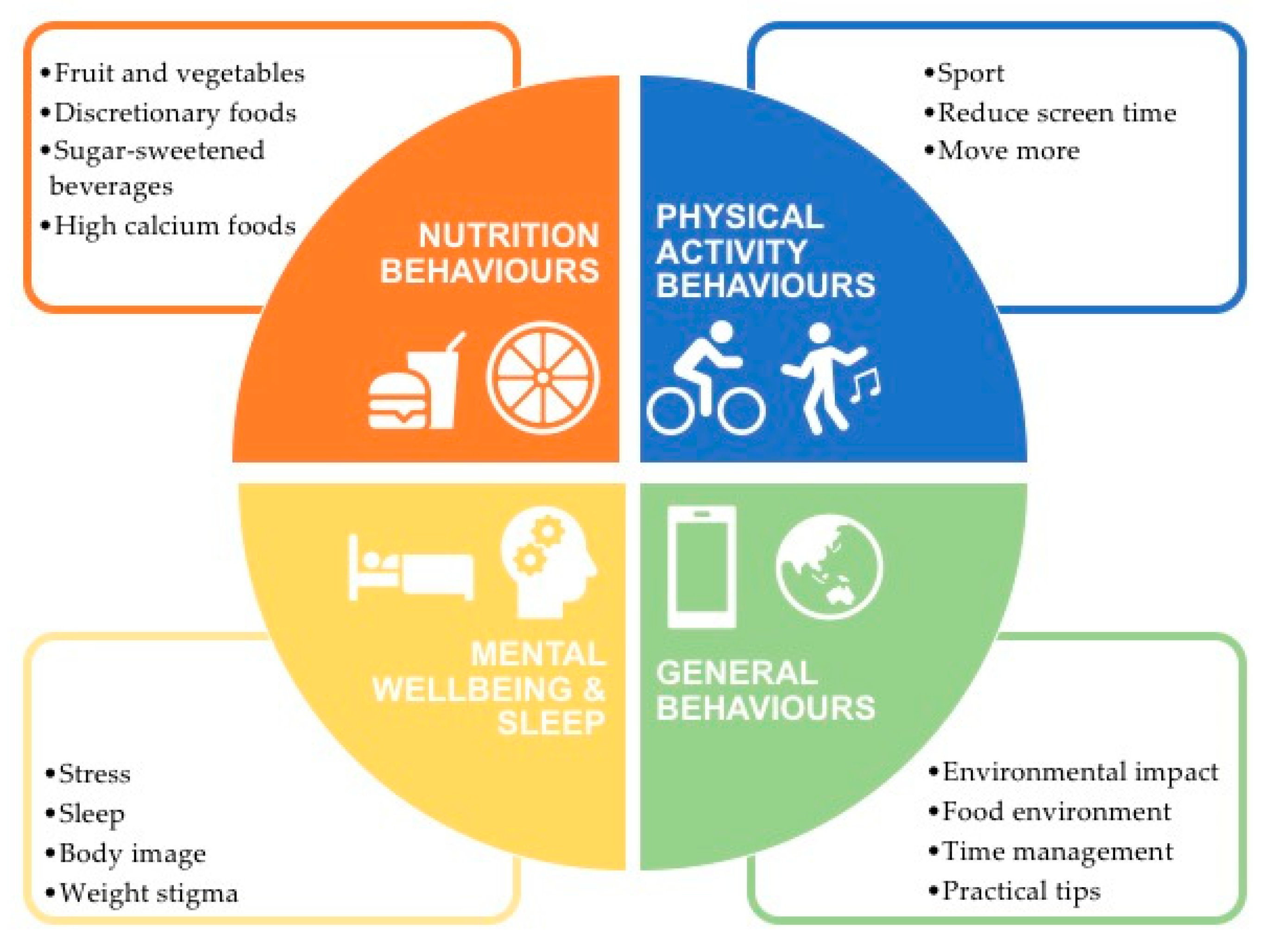
3.1.1. Key Behaviors Associated with Obesity in Adolescents
3.1.2. Previous Text Message Development Work with Adolescents
3.1.3. Effective Behavioral Change Techniques for Obesity Prevention in Adolescents
3.1.4. Workshop with Health and Research Professionals
3.1.5. Initial Text Messages Bank Drafting
3.2. Phase 2: User Acceptance Testing
3.2.1. Participant Demographics
3.2.2. Text Message Understanding and Usefulness Scores and Feedback
3.3. Phase 3: Final Development and Platform Testing
3.3.1. Final Text Message Bank
3.3.2. Platform Testing
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Abarca-Gómez, L.; Abdeen, Z.A.; Hamid, Z.A.; Abu-Rmeileh, N.M.; Acosta-Cazares, B.; Acuin, C.; Adams, R.J.; Aekplakorn, W.; Afsana, K.; Aguilar-Salinas, C.A.; et al. Worldwide trends in body-mass index, underweight, overweight, and obesity from 1975 to 2016: A pooled analysis of 2416 population-based measurement studies in 128.9 million children, adolescents, and adults. Lancet 2017, 390, 2627–2642. [Google Scholar] [CrossRef]
- Freedman, D.S.; Mei, Z.; Srinivasan, S.R.; Berenson, G.S.; Dietz, W.H. Cardiovascular risk factors and excess adiposity among overweight children and adolescents: The Bogalusa Heart Study. J. Pediatrics 2007, 150, 12–17. [Google Scholar] [CrossRef] [PubMed]
- Gordon-Larsen, P.; Adair, L.S.; Nelson, M.C.; Popkin, B.M. Five-year obesity incidence in the transition period between adolescence and adulthood: The National Longitudinal Study of Adolescent Health. Am. J. Clin. Nutr. 2004, 80, 569–575. [Google Scholar] [CrossRef] [PubMed]
- Patton, G.C.; Coffey, C.; Carlin, J.B.; Sawyer, S.M.; Williams, J.; Olsson, C.A.; Wake, M. Overweight and obesity between adolescence and young adulthood: A 10-year prospective cohort study. J. Adolesc. Health 2011, 48, 275–280. [Google Scholar] [CrossRef] [PubMed]
- Attard, S.M.; Herring, A.H.; Howard, A.G.; Gordon-Larsen, P. Longitudinal trajectories of BMI and cardiovascular disease risk: The national longitudinal study of adolescent health. Obesity 2013, 21, 2180–2188. [Google Scholar] [CrossRef]
- Lascar, N.; Brown, J.; Pattison, H.; Barnett, A.H.; Bailey, C.J.; Bellary, S. Type 2 diabetes in adolescents and young adults. Lancet Diabetes Endocrinol. 2018, 6, 69–80. [Google Scholar] [CrossRef]
- Sung, H.; Siegel, R.L.; Rosenberg, P.S.; Jemal, A. Emerging cancer trends among young adults in the USA: Analysis of a population-based cancer registry. Lancet Public Health 2019, 4, 137–147. [Google Scholar] [CrossRef]
- National Health and Medical Research Council. Clinical Practice Guidelines for the Management of Overweight and Obesity in Adults, Adolescents and Children in Australia; Health Do. Canberra: Melbourne, Australia, 2013.
- Brown, T.; Moore, T.H.M.; Hooper, L.; Gao, Y.; Zayegh, A.; Ijaz, S.; Elwenspoek, M.; Foxen, S.C.; Magee, L.; O’Malley, C.; et al. Interventions for preventing obesity in children. Cochrane Database Syst. Rev. 2019. [Google Scholar] [CrossRef]
- Skelton, J.A.; Beech, B.M. Attrition in paediatric weight management: A review of the literature and new directions. Obes. Rev. 2011, 12, 273–281. [Google Scholar] [CrossRef]
- Partridge, S.; Redfern, J. Strategies to Engage Adolescents in Digital Health Interventions for Obesity Prevention and Management. Healthcare 2018, 6, 70. [Google Scholar] [CrossRef]
- Kebbe, M.; Perez, A.; Buchholz, A.; McHugh, T.L.F.; Scott, S.D.; Richard, C.; Dyson, M.P.; Ball, G.D.C. End-user perspectives to inform policy and program decisions: A qualitative and quantitative content analysis of lifestyle treatment recommendations by adolescents with obesity. BMC Pediatrics 2019, 19, 418. [Google Scholar] [CrossRef] [PubMed]
- Raeside, R.; Partridge, S.R.; Singleton, A.; Redfern, J. Cardiovascular Disease Prevention in Adolescents: eHealth, Co-Creation, and Advocacy. Med. Sci. 2019, 7, 34. [Google Scholar] [CrossRef] [PubMed]
- Radovic, A.; McCarty, C.A.; Katzman, K.; Richardson, L.P. Adolescents’ Perspectives on Using Technology for Health: Qualitative Study. JMIR Pediatr. Parent 2018, 1. [Google Scholar] [CrossRef] [PubMed]
- Growth from Knowledge. Texting is Now Teens’ Favorite Way to Communicate with Friends. Available online: https://www.marketingcharts.com/demographics-and-audiences/teens-and-younger-105705 (accessed on 22 October 2019).
- Hall, A.K.; Cole-Lewis, H.; Bernhardt, J.M. Mobile text messaging for health: A systematic review of reviews. Annu. Rev. Public Health 2015, 36, 393–415. [Google Scholar] [CrossRef]
- Chow, C.K.; Redfern, J.; Hillis, G.S.; Thakkar, J.; Santo, K.; Hackett, M.L.; Jan, S.; Graves, N.; de Keizer, L.; Barry, T.; et al. Effect of Lifestyle-Focused Text Messaging on Risk Factor Modification in Patients With Coronary Heart Disease: A Randomized Clinical Trial. JAMA 2015, 314, 1255–1263. [Google Scholar] [CrossRef]
- Bobrow, K.; Farmer, A.J.; Springer, D.; Shanyinde, M.; Yu, L.M.; Brennan, T.; Rayner, B.; Namane, M.; Steyn, K.; Tarassenko, L.; et al. Mobile Phone Text Messages to Support Treatment Adherence in Adults with High Blood Pressure (SMS-Text Adherence Support [StAR]): A Single-Blind, Randomized Trial. Circulation 2016, 133, 592–600. [Google Scholar] [CrossRef]
- Siopis, G.; Chey, T.; Allman-Farinelli, M. A systematic review and meta-analysis of interventions for weight management using text messaging. J. Hum. Nutr. Diet. 2015, 28, 1–15. [Google Scholar] [CrossRef]
- Whittaker, R.; McRobbie, H.; Bullen, C.; Rodgers, A.; Gu, Y. Mobile phone-based interventions for smoking cessation. Cochrane Database Syst. Rev. 2016, 4. [Google Scholar] [CrossRef]
- Wickham, C.A.; Carbone, E.T. Who’s calling for weight loss? A systematic review of mobile phone weight loss programs for adolescents. Nutr. Rev. 2015, 73, 386–398. [Google Scholar] [CrossRef]
- Rose, T.; Barker, M.; Maria Jacob, C.; Morrison, L.; Lawrence, W.; Strommer, S.; Vogel, C.; Woods-Townsend, K.; Farrell, D.; Inskip, H.; et al. A Systematic Review of Digital Interventions for Improving the Diet and Physical Activity Behaviors of Adolescents. J. Adolesc. Health 2017, 61, 669–677. [Google Scholar] [CrossRef]
- Abraham, A.A.; Chow, W.C.; So, H.K.; Yip, B.H.; Li, A.M.; Kumta, S.M.; Woo, J.; Chan, S.M.; Lau, E.Y.; Nelson, E.A. Lifestyle intervention using an internet-based curriculum with cell phone reminders for obese Chinese teens: A randomized controlled study. PLoS ONE 2015, 10, e0125673. [Google Scholar] [CrossRef] [PubMed]
- Bagherniya, M.; Mostafavi Darani, F.; Sharma, M.; Maracy, M.R.; Allipour Birgani, R.; Ranjbar, G.; Taghipour, A.; Safraian, M.; Keshavarz, S.A. Assessment of the Efficacy of Physical Activity Level and Lifestyle Behavior Interventions Applying Social Cognitive Theory for Overweight and Obese Girl Adolescents. J. Res. Health Sci. 2018, 18, e00409. [Google Scholar] [PubMed]
- Chen, J.L.; Guedes, C.M.; Cooper, B.A.; Lung, A.E. Short-Term Efficacy of an Innovative Mobile Phone Technology-Based Intervention for Weight Management for Overweight and Obese Adolescents: Pilot Study. Interact. J. Med. Res. 2017, 6. [Google Scholar] [CrossRef] [PubMed]
- Jensen, C.D.; Duraccio, K.M.; Barnett, K.A.; Fortuna, C.; Woolford, S.J.; Giraud-Carrier, C.G. Feasibility, acceptability, and preliminary effectiveness of an adaptive text messaging intervention for adolescent weight control in primary care. Clin. Pract. Pediatric Psychol. 2019, 7, 57–67. [Google Scholar] [CrossRef]
- Love-Osborne, K.; Fortune, R.; Sheeder, J.; Federico, S.; Haemer, M.A. School-based health center-based treatment for obese adolescents: Feasibility and body mass index effects. Child. Obes. 2014, 10, 424–431. [Google Scholar] [CrossRef]
- Mameli, C.; Brunetti, D.; Colombo, V.; Bedogni, G.; Schneider, L.; Penagini, F.; Borsani, B.; Zuccotti, G.V. Combined use of a wristband and a smartphone to reduce body weight in obese children: Randomized controlled trial. Pediatric Obes. 2018, 13, 81–87. [Google Scholar] [CrossRef]
- Nguyen, B.; Shrewsbury, V.A.; O’Connor, J.; Steinbeck, K.S.; Lee, A.; Hill, A.J.; Shah, S.; Kohn, M.R.; Torvaldsen, S.; Baur, L.A. Twelve-month outcomes of the loozit randomized controlled trial: A community-based healthy lifestyle program for overweight and obese adolescents. Arch. Pediatrics Adolesc. Med. 2012, 166, 170–177. [Google Scholar] [CrossRef]
- Patrick, K.; Norman, G.J.; Davila, E.P.; Calfas, K.J.; Raab, F.; Gottschalk, M.; Sallis, J.F.; Godbole, S.; Covin, J.R. Outcomes of a 12-month technology-based intervention to promote weight loss in adolescents at risk for type 2 diabetes. J. Diabetes Sci. Technol. 2013, 7, 759–770. [Google Scholar] [CrossRef]
- Partridge, S.R.; Singleton, A.C.; Hyun, K.; Latham, Z.; Grunseit, A.; Steinbeck, K.; Chow, C.; Redfern, J. TEXT Message Behavioural Intervention for Teens on Eating, physical activity and Social wellbeing (TEXTBITES): A randomised controlled trial protocol. JMIR Res. Protoc. 2019. [Google Scholar] [CrossRef]
- Redfern, J.; Thiagalingam, A.; Jan, S.; Whittaker, R.; Hackett, M.L.; Mooney, J.; De Keizer, L.; Hillis, G.S.; Chow, C.K. Development of a set of mobile phone text messages designed for prevention of recurrent cardiovascular events. Eur. J. Prev. Cardiol. 2014, 21, 492–499. [Google Scholar] [CrossRef]
- Cargo, M.; Mercer, S.L. The value and challenges of participatory research: Strengthening its practice. Annu. Rev. Public Health 2008, 29, 325–350. [Google Scholar] [CrossRef] [PubMed]
- Flesch, R. A new readability yardstick. J. Appl. Psychol. 1948, 32, 221. [Google Scholar] [CrossRef] [PubMed]
- Australian Bureau of Statistics. 4364.0.55.001-National Health Survey: First Results, 2017–2018; Australian Bureau of Statistics: Canberra, Australia, 2017.
- Australian Bureau of Statistics. 4324.0.55.002-Microdata: Australian Health Survey: Nutrition and Physical Activity. Available online: http://bit.ly/2jkRRZO (accessed on 1 April 2017).
- Must, A.; Tybor, D.J. Physical activity and sedentary behavior: A review of longitudinal studies of weight and adiposity in youth. Int. J. Obes. 2005, 29, 84–96. [Google Scholar] [CrossRef] [PubMed]
- Nour, M.; Lutze, S.A.; Grech, A.; Allman-Farinelli, M. The Relationship between Vegetable Intake and Weight Outcomes: A Systematic Review of Cohort Studies. Nutrients 2018, 10, 1626. [Google Scholar] [CrossRef] [PubMed]
- Janssen, I.; Leblanc, A.G. Systematic review of the health benefits of physical activity and fitness in school-aged children and youth. Int. J. Behav. Nutr. Phys. Act. 2010, 7, 40. [Google Scholar] [CrossRef]
- Field, A.E.; Gillman, M.W.; Rosner, B.; Rockett, H.R.; Colditz, G.A. Association between fruit and vegetable intake and change in body mass index among a large sample of children and adolescents in the United States. Int. J. Obes. 2003, 27, 821–826. [Google Scholar] [CrossRef]
- Ledoux, T.A.; Hingle, M.D.; Baranowski, T. Relationship of fruit and vegetable intake with adiposity: A systematic review. Obes. Rev. 2011, 12, 143–150. [Google Scholar] [CrossRef]
- Wang, X.; Ouyang, Y.; Liu, J.; Zhu, M.; Zhao, G.; Bao, W.; Hu, F.B. Fruit and vegetable consumption and mortality from all causes, cardiovascular disease, and cancer: Systematic review and dose-response meta-analysis of prospective cohort studies. BMJ 2014, 349. [Google Scholar] [CrossRef]
- Bleich, S.N.; Vercammen, K.A. The negative impact of sugar-sweetened beverages on children’s health: An update of the literature. BMC Obes. 2018, 5, 6. [Google Scholar] [CrossRef]
- Braithwaite, I.; Stewart, A.W.; Hancox, R.J.; Beasley, R.; Murphy, R.; Mitchell, E.A. Fast-food consumption and body mass index in children and adolescents: An international cross-sectional study. BMJ Open 2014, 4. [Google Scholar] [CrossRef]
- Pereira, M.A.; Kartashov, A.I.; Ebbeling, C.B.; Van Horn, L.; Slattery, M.L.; Jacobs, D.R., Jr.; Ludwig, D.S. Fast-food habits, weight gain, and insulin resistance (the CARDIA study): 15-year prospective analysis. Lancet 2005, 365, 36–42. [Google Scholar] [CrossRef]
- World Health Organization. The Global Strategy for Women’s, Children’s, and Adolescents’ Health (2016–2030); World Health Organization: Geneva, Switzerland, 2015. [Google Scholar]
- Ebbeling, C.B.; Feldman, H.A.; Chomitz, V.R.; Antonelli, T.A.; Gortmaker, S.L.; Osganian, S.K.; Ludwig, D.S. A randomized trial of sugar-sweetened beverages and adolescent body weight. N. Engl. J. Med. 2012, 367, 1407–1416. [Google Scholar] [CrossRef] [PubMed]
- Fong, M.; Li, A.; Hill, A.J.; Cunich, M.; Skilton, M.R.; Madigan, C.D.; Caterson, I.D. Modelling the Association between Core and Discretionary Energy Intake in Adults with and without Obesity. Nutrients 2019, 11, 683. [Google Scholar] [CrossRef] [PubMed]
- Gohil, A.; Hannon, T.S. Poor Sleep and Obesity: Concurrent Epidemics in Adolescent Youth. Front. Endocrinol. 2018, 9, 364. [Google Scholar] [CrossRef]
- Conklin, A.I.; Guo, S.X.R.; Yao, C.A.; Tam, A.C.T.; Richardson, C.G. Stressful life events, gender and obesity: A prospective, population-based study of adolescents in British Columbia. Int. J. Pediatrics Adolesc. Med. 2019, 6, 41–46. [Google Scholar] [CrossRef]
- Roberts, R.E.; Duong, H.T. Does major depression affect risk for adolescent obesity? J. Affect. Disord. 2015, 186, 162–167. [Google Scholar] [CrossRef]
- Hunger, J.M.; Tomiyama, A.J. Weight Labeling and Disordered Eating Among Adolescent Girls: Longitudinal Evidence From the National Heart, Lung, and Blood Institute Growth and Health Study. J. Adolesc. Health 2018, 63, 360–362. [Google Scholar] [CrossRef]
- Brochu, P.M.; Pearl, R.L.; Simontacchi, L.A. Weight Stigma and Related Social Factors in Psychological Care. In Psychological Care in Severe Obesity: A Practical and Integrated Approach; Hawa, R., Sockalingam, S., Cassin, S., Eds.; Cambridge University Press: Cambridge, UK, 2018; pp. 42–60. [Google Scholar]
- Hingle, M.; Nichter, M.; Medeiros, M.; Grace, S. Texting for Health: The Use of Participatory Methods to Develop Healthy Lifestyle Messages for Teens. J. Nutr. Educ. Behav. 2013, 45, 12–19. [Google Scholar] [CrossRef]
- Smith, K.L.; Kerr, D.A.; Fenner, A.A.; Straker, L.M. Adolescents just do not know what they want: A qualitative study to describe obese adolescents’ experiences of text messaging to support behavior change maintenance post intervention. J. Med. Internet Res. 2014, 16. [Google Scholar] [CrossRef]
- Thompson, D.; Cantu, D.; Ramirez, B.; Cullen, K.W.; Baranowski, T.; Mendoza, J.; Anderson, B.; Jago, R.; Rodgers, W.; Liu, Y. Texting to Increase Adolescent Physical Activity: Feasibility Assessment. Am. J. Health Behav. 2016, 40, 472–483. [Google Scholar] [CrossRef]
- Wickham, C.A.; Carbone, E.T. “Just Say It Like It Is!” Use of a Community-Based Participatory Approach to Develop a Technology-Driven Food Literacy Program for Adolescents. Int. Q. Community Health Educ. 2018, 38, 83–97. [Google Scholar] [CrossRef] [PubMed]
- Woolford, S.J.; Barr, K.L.; Derry, H.A.; Jepson, C.M.; Clark, S.J.; Strecher, V.J.; Resnicow, K. OMG do not say LOL: Obese adolescents’ perspectives on the content of text messages to enhance weight loss efforts. Obesity 2011, 19, 2382–2387. [Google Scholar] [CrossRef] [PubMed]
- Martin, J.; Chater, A.; Lorencatto, F. Effective behaviour change techniques in the prevention and management of childhood obesity. Int. J. Obes. 2013, 37, 1287–1294. [Google Scholar] [CrossRef] [PubMed]
- Michie, S.; Ashford, S.; Sniehotta, F.F.; Dombrowski, S.U.; Bishop, A.; French, D.P. A refined taxonomy of behaviour change techniques to help people change their physical activity and healthy eating behaviours: The CALO-RE taxonomy. Psychol. Health 2011, 26, 1479–1498. [Google Scholar] [CrossRef] [PubMed]
- Greenhalgh, T.; Hinton, L.; Finlay, T.; Macfarlane, A.; Fahy, N.; Clyde, B.; Chant, A. Frameworks for supporting patient and public involvement in research: Systematic review and co-design pilot. Health Expect. 2019, 22, 785–801. [Google Scholar] [CrossRef] [PubMed]
- Rouf, A.; Allman-Farinelli, M. Messaging for Interventions Aiming to Improve Calcium Intake in Young Adults-A Mixed Methods Study. Nutrients 2018, 10, 1673. [Google Scholar] [CrossRef]
- Robinson, T.N. Save the World, Prevent Obesity: Piggybacking on Existing Social and Ideological Movements. Obesity 2010, 18, 17–22. [Google Scholar] [CrossRef]
- Skouteris, H.; Cox, R.; Huang, T.; Rutherford, L.; Edwards, S.; Cutter-Mackenzie, A. Promoting obesity prevention together with environmental sustainability. Health Promot. Int. 2013, 29, 454–462. [Google Scholar] [CrossRef][Green Version]
- Rubak, S.; Sandbaek, A.; Lauritzen, T.; Christensen, B. Motivational interviewing: A systematic review and meta-analysis. Br. J. Gen. Pract. 2005, 55, 305–312. [Google Scholar]
- Pearson, E.S. Goal setting as a health behavior change strategy in overweight and obese adults: A systematic literature review examining intervention components. Patient Educ. Couns. 2012, 87, 32–42. [Google Scholar] [CrossRef]
- Mihrshahi, S.; Gow, M.L.; Baur, L.A. Contemporary approaches to the prevention and management of paediatric obesity: An Australian focus. Med. J. Aust. 2018, 209, 267–274. [Google Scholar] [CrossRef] [PubMed]
| Author, Year, Country, Citation | Study Type, Focus, & Design | Participants | Key Findings Related to Text Message Preferences |
|---|---|---|---|
| Hingle et al. 2013, US, [54] | Type: Formative research & pilot study Focus: Nutrition and physical activity behaviors Design: Youth participatory approach with focus groups, discussions, & 8-week pilot study | N = 177 (aged 12–18 years)
|
|
| Smith et al. 2014, Australia, [55] | Type: Qualitative study Focus: Nutrition and physical activity behaviors for weight management Design: Focus groups with adolescents who had participated in an 8-week intervention and maintenance phase with text message support | N = 12 (aged 12–16 years) |
|
| Thompson et al. 2016, US, [56] | Type: Feasibility study Focus: Physical activity behaviors Design: Four-group (40 per group) randomized design & post-intervention research with a subset of participants examined program reactions | N = 160 (aged 14–17 years)
|
|
| Wickham and Carbone, 2018, US, [57] | Type: Formative research Focus: Food literacy Design: Community based participatory research approach with a Kid Council | N = 4 (aged 13–16 years)
|
|
| Woolford et al. 2011, US, [58] | Type: Formative research Focus: Weight loss Design: Focus groups | N = 24 (aged 11–19 years) |
|
| Characteristic | Participants | |
|---|---|---|
| Adolescents | n = 25 | |
| Age (years ± SD) | 15 ± 2 | |
| Gender identity | Female | 15 |
| Male | 10 | |
| Language spoken at home | English-speaking a | 21 |
| Current high school student | Yes | 25 |
| Current school year | Years 7–8 | 6 |
| Years 9–10 | 13 | |
| Years 11–12 | 10 | |
| SES quintile | 0–60 (lowest) b | 8 |
| 61–80 | 5 | |
| 81–100 (highest) | 11 | |
| Professionals | n = 15 | |
| Age (years ± SD) | 36 ± 11 | |
| Gender identity | Female | 12 |
| Male | 3 | |
| Area of expertise | Physical activity | 1 |
| Nutrition and diet | 4 | |
| Adolescent medicine | 2 | |
| Medicine | 2 | |
| Public health | 6 | |
| Prevention | 2 | |
| Behavior change | 4 | |
| Psychology | 1 | |
| High school teacher | 2 |
| Original Text Message | Reasons for Rating | Rational for Rating | Amended or New Message |
|---|---|---|---|
| Corn isn’t just a tasty snack, it’s multi-purpose! It can be used to make fireworks, glue, paint & plastic. But let’s face it, popcorn is one of the best uses, check out some recipe ideas here: tinyurl.com/airpopcorn | Practical and fun | Scored 15/15 for both usefulness and understanding by both adolescents and professionals Adolescent reviewer: “Perfect.” Professional review: “This is a fun one!” | No revision |
| Producing a fast-food burger can create up to 3.5 kg of carbon emissions! Skip the processing, help save the planet & make your own: tinyurl.com/tanburger | Focused on environmental sustainability | Scored >12/15 for both usefulness and understanding by both adolescents and professionals Professional reviewer: “I really like this one.” | No revision |
| Need a dose of some happy hormones? Stretching can release endorphins, reduce your stress, make you feel great, and you can do it anywhere, even while watching TV or YouTube. Check it out: tinyurl.com/stretchyout | Benefits other than physical health | Scored 15/15 for both usefulness and understanding by both adolescents and professionals Professional reviewer: “I like this message! The second half could flow a bit better.” Revision: Modification to sentence structure | Need a dose of some happy hormones? Stretching can release endorphins, reduce your stress and make you feel great. The best part? You can do it anywhere, even while watching TV or YouTube. Check it out: tinyurl.com/stretchyout |
| Want to get your homework or study done in record time? Do power bursts! Put your phone on do not disturb and power it out for 25 min. Take a 5 min break (yep, you can check your phone) and repeat until it’s done! | Succinct and straightforward | Scored 15/15 for both usefulness and understanding by both adolescents and professionals Adolescent reviewer: “Good info!!” Professional reviewer: "I like this one, very straightforward. Maybe right at the end say, ’your work’ instead of ’it’s’." | Want to get your homework or study done in record time? Do power bursts! Put your phone on do not disturb and power it out for 25 min. Take a 5 min break (yep, you can check your phone) and repeat until your work is done! |
| Learning to cook now is the best time because, by the time you move out of home, you’ll be a whiz! It will save you money, keep you energized, as well as impress your friends & maybe someone special-a triple win! vegpower.org.uk/recipes/ | Age-appropriate | Scored >12/15 for both usefulness and understanding by both adolescents and professionals This message was rated more appropriate for older adolescents, 17–18 years of age and an alternate text message was included for younger adolescents, 13–16 years of age. Revision: Included an age-appropriate message for younger adolescents. | Learning to cook now is the best time because it can help you understand different cultures and flavors! Check out some cool recipes here-vegpower.org.uk/recipes/ |
| 33% of all the world’s food gets wasted! Isn’t that crazy?! :O #FightFoodWaste & check out what you can do: tinyurl.com/fightfoodwa | Remove youth jargon, abbreviations, or unnecessary emojis | Scored >12/15 for both usefulness and understanding by both adolescents and professionals Professional reviewer: “Using hashtags in a text message won’t lead anywhere as they would in social media and could result in just being confusing. Instead, maybe direct the person to use the hashtag to display their actions to affect food waste.” Adolescent reviewer: “No emoticons, do you need the hashtag?" and “Yeah, I [don’t know] what that emoji means. Not to be harsh but try less to relate to ’the teens’, and you’ll relate to them more” Revision: Removed hashtag and emoji. | 33% of all the world’s food gets wasted! Isn’t that crazy?! Fight food waste & check out what you can do to help: tinyurl.com/fightfoodwa |
| An egg, the most-liked photo on Instagram! No yolks, it was eggcellent. For a soft-boiled egg, cook for 5 min & hard-boiled eggs, cook for 8 min. Delicious on a wholemeal cracker or toast. For more tips check out this clip: tinyurl.com/eggboil | Limiting puns and jokes | Scored >12/15 for both usefulness and understanding by both adolescents and professionals Adolescent reviewer: “Too many puns?” Professional reviewer: “I’d stick to only using one pun in the message instead of 2.” Revision: removed pun ‘eggcellent.’ | An egg is the most-liked photo on Instagram! No yolks! For a soft-boiled egg, cook for 5 min & hard-boiled eggs, cook for 8 min. Delicious on a wholemeal cracker or toast. For more tips check out this clip: tinyurl.com/eggboil |
| Ever pulled an all-nighter to study for an exam? If yes, don’t worry, you’re not alone! But lack of sleep will decrease your performance the next day. You’ll study better & retain more knowledge when you study consistently in small bite-sized chunks. Plan a study schedule for your next big exam! | More practical advice and links | Scored >12/15 for both usefulness and understanding by both adolescents and professionals Adolescent reviewer: "Maybe put a link to a weekly planner page to help with organisation" Revision: included link to an online study schedule | Ever pulled an all-nighter to study for an exam? If yes, don’t worry, you’re not alone! You’ll study better & retain more knowledge when you sleep well & study consistently in small bite-sized chunks. Plan a study schedule for your next big exam, try this template: tinyurl.com/y4ymrej2 |
| Instead of binging on your fav TV show to avoid a finishing a big assessment, reward yourself with one episode after completing small chunks | Advice that is different from ‘norm’ of being an adolescent | Scored >12/15 for understanding by both adolescents and professionals and conflicting reviewer scores and feedback with adolescents rating 11/15 and professionals 15/15 for usefulness. Adolescent reviewer: “The nature of tv shows is that you feel compelled to binge them. watching one can end up being a whole series." Professional reviewer: “Excellent message, really important.” | Excluded |
| On a ‘kite’ study schedule & can’t find time for physical activity? Why not fly a kite! Kite flying is a professional sport in Thailand & it requires mental skills too like concentration | Perceived as ‘trying too hard.’ | Scored <12/15 for both usefulness and understanding by both adolescents and professionals Adolescent reviewers: “I don’t know what a kite study schedule is, and I don’t believe that kite flying is teenagers preferred pastime” and “Not relevant, a bit weird.” | Excluded |
| Our brains weigh about 1.5 kg & are 70% water! The other 30% is made up of fat & protein with a little sugar & a little salt. Similar to pancakes, but more useful for thinking & far less delicious than pancakes. Speaking of pancakes: tinyurl.com/pancaketip | Long and wordy | Scored <12/15 for both usefulness and understanding by both adolescents and professionals Adolescent reviewer: “Slightly unclear.” | Excluded |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Partridge, S.R.; Raeside, R.; Latham, Z.; Singleton, A.C.; Hyun, K.; Grunseit, A.; Steinbeck, K.; Redfern, J. ‘Not to Be Harsh but Try Less to Relate to ‘the Teens’ and You’ll Relate to Them More’: Co-Designing Obesity Prevention Text Messages with Adolescents. Int. J. Environ. Res. Public Health 2019, 16, 4887. https://doi.org/10.3390/ijerph16244887
Partridge SR, Raeside R, Latham Z, Singleton AC, Hyun K, Grunseit A, Steinbeck K, Redfern J. ‘Not to Be Harsh but Try Less to Relate to ‘the Teens’ and You’ll Relate to Them More’: Co-Designing Obesity Prevention Text Messages with Adolescents. International Journal of Environmental Research and Public Health. 2019; 16(24):4887. https://doi.org/10.3390/ijerph16244887
Chicago/Turabian StylePartridge, Stephanie R., Rebecca Raeside, Zoe Latham, Anna C. Singleton, Karice Hyun, Alicia Grunseit, Katharine Steinbeck, and Julie Redfern. 2019. "‘Not to Be Harsh but Try Less to Relate to ‘the Teens’ and You’ll Relate to Them More’: Co-Designing Obesity Prevention Text Messages with Adolescents" International Journal of Environmental Research and Public Health 16, no. 24: 4887. https://doi.org/10.3390/ijerph16244887
APA StylePartridge, S. R., Raeside, R., Latham, Z., Singleton, A. C., Hyun, K., Grunseit, A., Steinbeck, K., & Redfern, J. (2019). ‘Not to Be Harsh but Try Less to Relate to ‘the Teens’ and You’ll Relate to Them More’: Co-Designing Obesity Prevention Text Messages with Adolescents. International Journal of Environmental Research and Public Health, 16(24), 4887. https://doi.org/10.3390/ijerph16244887





