The Effectiveness of Tobacco Dependence Education in Health Professional Students’ Practice: A Systematic Review and Meta-Analysis of Randomized Controlled Trials
Abstract
:1. Introduction
Review Question
2. Materials and Methods
2.1. Criteria for Inclusion
2.1.1. Inclusion Criteria: Participants
2.1.2. Inclusion Criteria: Intervention
2.1.3. Inclusion Criteria: Comparator
2.1.4. Inclusion Criteria: Outcomes
2.1.5. Inclusion Criteria: Study Types
2.2. Search Strategy
2.3. Study Selection
2.4. Methodological Quality
2.5. Data Extraction
2.6. Data Synthesis
3. Results
3.1. Meta-Analysis Study Characteristics
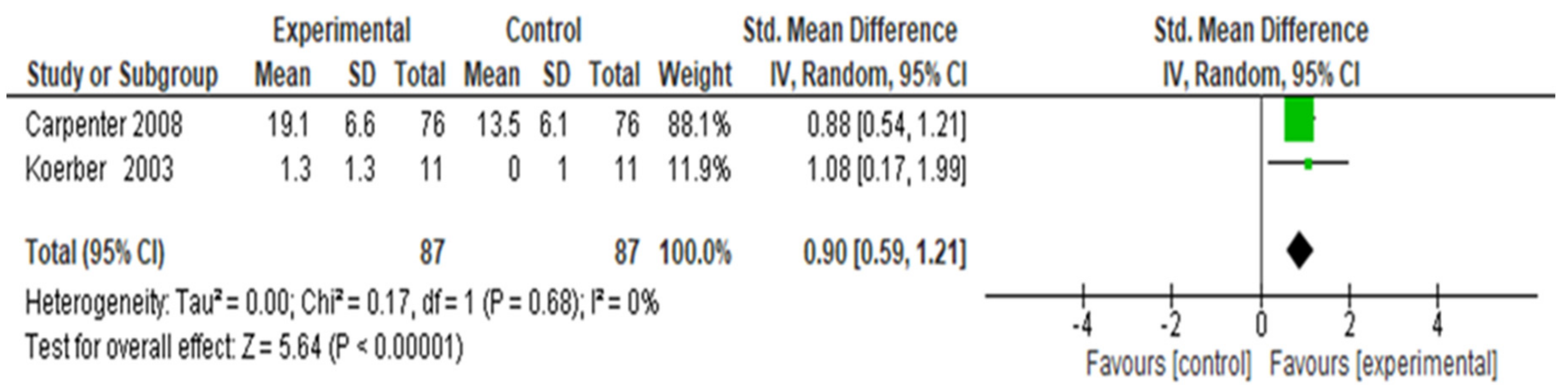
3.2. Student Tobacco Cessation Counseling Skills
3.3. Student Self-Efficacy Outcomes
3.4. Patient Smoking Cessation Outcomes
4. Discussion
5. Conclusions
- Comparative studies of the 5As, Trans-theoretical Model of Change, Self-Efficacy theory and Motivational Interviewing approaches in appropriately powered and carefully monitored RCTs to assess which approach produces the best results for trainees and patients. Currently, educators use a combination of these approaches.
- Identify the ideal length of instruction time to optimise outcomes. Currently, it ranges from 8 to 12 hours.
- Identify the best combination of lectures, videotaping and role play with peers and trained professionals to optimise outcomes.
- Observe and train preceptors to ensure that they provide optimum feedback and monitor improvements in trainee competence.
- Observe trainees to ensure they conduct the interventions correctly and completely according to the manual.
- Measure the counselling skills of trainees and identify those who need more training and provide it.
- Have trainees observe trained professionals, observe how the trainees implement new skills they observed and discuss how well they implemented them.
- Ask preceptors to provide feedback on the patient-centredness and quality of the patient–trainee relationship and how to improve it.
- Maintain good contact with the clients to avoid attrition by the 6- or 12-month follow ups.
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Bilano, V.; Gilmour, S.; Moffiet, T.; D’Espaignet, E.T.; Stevens, A.; Commar, A.; Tuyl, F.; Hudson, I.; Shibuya, K. Global trends and projections for tobacco use, 1990–2025: An analysis of smoking indicators from the WHO Comprehensive Information Systems for Tobacco Control. Lancet 2015, 385, 966–976. [Google Scholar] [CrossRef]
- Mathers, C.; Loncar, D. Projections of global mortality and burden of disease from 2002 to 2030. PLoS Med. 2006, 3, e442. [Google Scholar] [CrossRef] [PubMed]
- Ezzati, M.; Lopez, A.D. Estimates of global mortality attributable to smoking in 2000. Lancet 2003, 362, 847–852. [Google Scholar] [CrossRef]
- World Health Organization and the Secretariat of the WHO Framework Convention on Tobacco Control. The Economic and Health Benefits of Tobacco Taxation [Online]; WHO: Geneva, Switzerland, 2015; Available online: https://apps.who.int/iris/bitstream/handle/10665/179423/WHO_NMH_PND_15.6_eng.pdf?sequence=1 (accessed on 29 September 2019).
- Ellison, L.F.; Morrison, H.I.; De Groh, M.; Villeneuve, P.J. Health consequences of smoking among Canadian smokers: An update. Chronic Dis. Can. 1999, 20, 36–39. [Google Scholar] [PubMed]
- Makomaski Illing, E.M.; Kaiserman, M.J. Mortality attributable to tobacco use in Canada and its regions, 1994 and 1996. Chronic Dis. Can. 1999, 20, 111–117. [Google Scholar] [PubMed]
- Shafey, O.; Eriksen, M.; Ross., H.; Mackay, J. The Tobacco Atlas, 3rd ed.; American Cancer Society: Atlanta, GA, USA, 2009. [Google Scholar]
- Canadian Cancer Society. Why Tobacco Control Is Important. 2019. Available online: http://www.cancer.ca/en/get-involved/take-action/what-we-are-doing/tobacco-control/?region=mb (accessed on 29 September 2019).
- Heart and Stroke Foundation of Canada. Smoking and Tobacco. 2018. Available online: http://www.heartandstroke.ca/heart/risk-and-prevention/lifestyle-risk-factors/smoking-and-tobacco (accessed on 29 September 2019).
- Canadian Lung Association. Smoking and Tobacco. Updated 10 December 2016. Available online: https://www.lung.ca/lung-health/smoking-and-tobacco (accessed on 29 September 2019).
- Xia, J.; Wang, L.; Ma, Z.; Zhong, L.; Wang, Y.; Gao, Y.; He, L.; Su, X. Cigarette smoking and chronic kidney disease in the general population: A systematic review and meta-analysis of prospective cohort studies. Nephrol. Dial. Transplant. 2017, 32, 475–487. [Google Scholar] [CrossRef]
- Van Osch, F.H.M.; Jochems, S.H.J.; Van Schooten, F.-J.; Bryan, R.T.; Zeegers, M.P. Quantified relations between exposure to tobacco smoking and bladder cancer risk: A meta-analysis of 89 observational studies. Int. J. Epidemiol. 2016, 45, 857–870. [Google Scholar] [CrossRef]
- Zhang, P.; Wang, R.; Li, Z.; Wang, Y.; Gao, C.; Lv, X.; Song, W.; Li, B. The risk of smoking on multiple sclerosis: A meta-analysis based on 20,626 cases from case-control and cohort studies. PeerJ 2016, 4, e1797. [Google Scholar] [CrossRef]
- Bluman, L.G.; Mosca, L.; Newman, N.; Simon, D.G. Preoperative smoking habits and postoperative pulmonary complications. Chest 1998, 113, 883–889. [Google Scholar] [CrossRef]
- Akrawi, W.; Benumof, J.L. A pathophysiological basis for informed preoperative smoking cessation counseling. J. Cardiothorac. Vasc. Anesth. 1997, 11, 629–640. [Google Scholar] [CrossRef]
- Moller, A.M.; Villebro, N.; Pedersen, T.; Tonnesen, H. Effect of preoperative smoking intervention on postoperative complications: A randomised clinical trial. Lancet 2002, 359, 113–117. [Google Scholar] [CrossRef]
- Kwiatkowski, T.C.; Hanley, E.N.; Ramp, W.K. Cigarette smoking and its orthopedic consequences. Am. J. Orthop. 1996, 25, 590–597. [Google Scholar] [PubMed]
- Haverstock, B.D.; Mandracchia, V.J. Cigarette smoking and bone healing: Implications in foot and ankle surgery. J. Foot Ankle Surg. 1998, 37, 69–74. [Google Scholar] [CrossRef]
- Krueger, J.K.; Rohrich, R.J. Clearing the smoke: The scientific rationale for tobacco abstention with plastic surgery. Plast. Reconstr. Surg. 2001, 108, 1063–1073. [Google Scholar] [CrossRef] [PubMed]
- Myrha, W.; Davis, M.; Mueller, B.A.; Hickok, D. Maternal smoking and the risk of polyhydramnios. Am. J. Public Health 1992, 82, 176–179. [Google Scholar] [CrossRef]
- Wainwright, R.L. Change in observed birth weight associated with change in maternal cigarette smoking. Am. J. Epidemiol. 1983, 117, 668–675. [Google Scholar] [CrossRef]
- Silins, J.; Semenciw, R.M.; Morrison, H.I.; Lindsay, J.; Sherman, G.J.; Mao, Y.; Wigle, D.T. Risk factors for perinatal mortality in Canada. Can. Med. Assoc. J. 1985, 133, 1214–1219. [Google Scholar]
- Edwards, D.; Freeman, T.; Roche, A.M. Dentists’ and dental hygienists’ role in smoking cessation: An examination and comparison of current practice and barriers to service provision. Health Promot. J. Aust. 2006, 17, 145–151. [Google Scholar] [CrossRef]
- Simansalam, S.; Shamsudin, S.H.; Mohamed, M.H.N. Malaysian pharmacy students’ intention to provide smoking cessation counseling. Curr. Pharm. Teach. Learn. 2017, 9, 918–924. [Google Scholar] [CrossRef]
- Canadian Nurses Association. The Role of Health Professionals in Tobacco Cessation [Online]. 2011. Available online: https://www.cna-aiic.ca/-/media/cna/page-content/pdf-en/jps_tobacco_cessation_2011_e.pdf (accessed on 29 September 2019).
- Schultz, A.S.H.; Tremblay, M.; Quinlan, B.; Brewster, J.; Hyndman, K.; Compton, S.; Fisher, K.; Brown, J. Canadian Health Professionals, Health Organizations, and Tobacco Control; Final Report; The University of Manitoba: Winnipeg, MB, Canada, 2008. [Google Scholar]
- World Health Organization. Policy Recommendations for Smoking Cessation and Treatment of Tobacco Dependence. June 2003. Available online: https://www.who.int/tobacco/publications/smoking_cessation/recommendations/en/ (accessed on 29 September 2019).
- Muramoto, M.L.; Lando, H. Faculty development in tobacco cessation: Training health professionals and promoting tobacco control in developing countries. Drug Alcohol Rev. 2009, 28, 498–506. [Google Scholar] [CrossRef] [Green Version]
- World Health Organization. WHO Framework Convention on Tobacco Control. 2005. Available online: http://www.who.int/fctc/text_download/en/ (accessed on 29 September 2019).
- Fiore, M.C.; Jaén, C.R.; Baker, T.B.; Bailey, W.C.; Benowitz, N.L.; Curry, S.J.; Dorfman, S.F.; Froelicher, E.S.; Goldstein, M.G.; Healton, C.G.; et al. Treating Tobacco Use and Dependence, 2008 Update; U.S. Department of Health and Human Services, Public Health Service: Rockville, MD, USA, 2008. [Google Scholar]
- Carson, K.V.; Verbiest, M.E.A.; Crone, M.R.; Brinn, M.P.; Esterman, A.J.; Assendelft, W.J.J.; Smith, B.J. Training health professionals in smoking cessation. Cochrane Database Syst. Rev. 2012. [Google Scholar] [CrossRef] [PubMed]
- Sheffer, C.E.; Barone, C.P.; Anders, M.E. Training health care providers in the treatment of tobacco use and dependence: Pre- and post-training results. J. Eval. Clin. Pract. 2009, 15, 607–613. [Google Scholar] [CrossRef] [PubMed]
- Gorin, S.S.; Heck, J.E. Meta-analysis of the efficacy of tobacco counseling by health care providers. Cancer Epidemiol. Biomark. Prev. 2004, 13, 2012–2022. [Google Scholar]
- Hopkins, D.P.; Husten, C.G.; Fielding, J.E.; Rosenquist, J.N.; Westphal, L.L. Evidence reviews and recommendations on interventions to reduce tobacco use and exposure to environmental tobacco smoke. Am. J. Prev. Med. 2001, 20, 67–87. [Google Scholar] [CrossRef]
- Taylor, M.C.; Dingle, J.L. Prevention of tobacco-caused disease. In The Canadian Guide to Clinical Preventive Health Care; Canadian Task Force on the Periodic Health Examination, Ed.; Canada Communication Group Publishing: Ottawa, ON, Canada, 1994; pp. 500–511. [Google Scholar]
- Canadian Nurses Association. Working with Canadians Affected by Tobacco: Guidelines for Registered Nurses; University of British Columbia: Vancouver, BC, Canada, 1997. [Google Scholar]
- Hyndman, K. An Evaluation of a Dissemination Intervention to Enhance Registered Nurses’ Use of Clinical Practice Guidelines on Tobacco Reduction. Master’s Thesis, University of British Columbia, Vancouver, BC, Canada, 2005. [Google Scholar]
- Cooke, M.; Mattick, R.P.; Campbell, E. The influence of individual and organizational factors on the reported smoking intervention practices of staff in 20 antenatal clinics. Drug Alcohol Rev. 1998, 17, 175–185. [Google Scholar] [CrossRef]
- Cooke, M.; Mattick, R.P.; Barclay, L. Predictors of brief smoking intervention in a midwifery setting. Addiction 1996, 91, 1715–1725. [Google Scholar] [CrossRef]
- Clasper, P.; White, M. Smoking cessation interventions in pregnancy: Practice and views of midwives, GPs and obstetricians. Health Educ. J. 1995, 54, 150–162. [Google Scholar] [CrossRef]
- Walsh, R.A.; Redman, S.; Brinsmead, M.W.; Arnold, B. Smoking cessation in pregnancy: A survey of the medical and nursing directors of public antenatal clinics in Australia. Aust. N. Z. J. Obstet. Gynaecol. 1995, 35, 144–150. [Google Scholar] [CrossRef]
- Zapka, J.G.; Pbert, L.; Stoddard, A.M.; Ockene, J.K.; Goins, K.V.; Bonollo, D. Smoking cessation counseling with pregnant and postpartum women: A survey of community health center providers. Am. J. Public Health 2000, 90, 78–84. [Google Scholar] [CrossRef]
- Canadian Lung Association. Making Quit Happen: Canada’s Challenges to Smoking Cessation. Updated 17 January 2018. Available online: https://www.lung.ca/news/advocacy-tools/our-publications (accessed on 29 September 2019).
- Schultz, A.S.H.; Johnson, J.L.; Bottorff, J.L. Registered nurses’ perspectives on tobacco reduction: Views from western Canada. Can. J. Nurs. Res. 2006, 38, 192–211. [Google Scholar]
- Fiore, M.C.; Bailey, W.C.; Cohen, S.J.; Dorfman, S.F.; Goldstein, M.G.; Gritz, E.R.; Heyman, R.B.; Jaén, C.R.; Kotte, T.E.; Lando, H.A.; et al. Treating Tobacco Use and Dependence: Clinical Practice Guideline; Department of Health and Human Services, Public Health Service: Rockville, MD, USA, 2000. [Google Scholar]
- Fiore, M.C. US public health service clinical practice guideline: treating tobacco use and dependence. Respir. Care 2000, 45, 1200–1262. [Google Scholar] [PubMed]
- Sarna, L.; Bialous, S.A.; Rice, V.H.; Wewers, M.E. Promoting tobacco dependence treatment in nursing education. Drug Alcohol Rev. 2009, 28, 507–516. [Google Scholar] [CrossRef] [PubMed]
- Williams, D.M. Preparing pharmacy students and pharmacists to provide tobacco cessation counselling. Drug Alcohol Rev. 2009, 28, 533–540. [Google Scholar] [CrossRef] [PubMed]
- Registered Nurses’ Association of Ontario. Integrating Smoking Cessation into Daily Practice: Nursing Best Practice Guideline; Registered Nurses’ Association of Ontario: Toronto, ON, Canada, 2007. [Google Scholar]
- Halperin, A.C.; Thompson, L.A.; Hymer, J.C.; Peterson, A.K.; Thompson, B. A case-based clinician training program for treating tobacco use in college students. Public Health Rep. 2006, 121, 557–562. [Google Scholar] [CrossRef] [PubMed]
- Richmond, R. The process of introducing a tobacco curriculum in medical school. Respirology 2004, 9, 165–172. [Google Scholar] [CrossRef] [PubMed]
- Pederson, L.L.; Blumenthal, D.S.; Dever, A.; McGrady, G. A web-based smoking cessation and prevention curriculum for medical students: Why, how, what, and what next. Drug Alcohol Rev. 2006, 25, 39–47. [Google Scholar] [CrossRef] [PubMed]
- Brown, R.L.; Pfeifer, J.M.; Gjerde, C.L.; Seibert, C.S.; Haq, C.L. Teaching patient-centered tobacco intervention to first-year medical students. J. Gen. Intern. Med. 2004, 19, 534–539. [Google Scholar] [CrossRef] [Green Version]
- Humair, J.P.; Cornuz, J. A new curriculum using active learning methods and standardized patients to train residents in smoking cessation. J. Gen. Intern. Med. 2003, 18, 1023–1027. [Google Scholar] [CrossRef] [Green Version]
- Corelli, R.L.; Kroon, L.A.; Chung, E.P.; Sakamoto, L.M.; Gundersen, B.; Fenlon, C.M.; Hudmon, K.S. Statewide evaluation of a tobacco cessation curriculum for pharmacy students. Prev. Med. 2005, 40, 888–895. [Google Scholar] [CrossRef]
- Hudmon, K.S.; Kroon, L.A.; Corelli, R.L.; Saunders, K.C.; Spitz, M.R.; Bates, T.R.; Liang, D. Training future pharmacists at a minority educational institution: Evaluation of the Rx for Change tobacco cessation training program. Cancer Epidemiol. Biomark. Prev. 2004, 13, 477–481. [Google Scholar]
- Hudmon, K.S.; Corelli, R.L.; Chung, E.; Gundersen, B.; Kroon, L.A.; Sakamoto, L.M.; Hemberger, K.K.; Fenlon, C.; Prokhorov, A.V. Development and implementation of a tobacco cessation training program for students in the health professions. J. Cancer Educ. 2003, 18, 142–149. [Google Scholar] [CrossRef] [PubMed]
- Kelley, F.J.; Heath, J.; Crowell, N. Using the Rx for Change tobacco curriculum in advanced practice nursing education. Crit. Care Nurs. Clin. N. Am. 2006, 18, 131–138. [Google Scholar] [CrossRef] [PubMed]
- Wewers, M.C.; Kidd, K.; Armbruster, D.; Sarna, L. Tobacco dependence curricula in U.S. baccalaureate and graduate nursing education. Nurs. Outlook 2004, 52, 95–101. [Google Scholar] [CrossRef] [PubMed]
- Richmond, R.; Zwar, N.; Taylor, R.; Hunnisett, J.; Hyslop, F. Teaching about tobacco in medical schools: A worldwide study. Drug Alcohol Rev. 2009, 28, 484–497. [Google Scholar] [CrossRef]
- Ling Leong, S.; Lewis, P.R.; Curry, W.J.; Gingrich, D.L. Tobacco world: Evaluation of a tobacco cessation training program for third-year medical students. Acad. Med. 2008, 83, S25–S28. [Google Scholar] [CrossRef]
- Heath, J.; Andrews, J.; Thomas, S.A.; Kelley, F.J.; Friedman, E. Tobacco dependence curricula in acute care nurse practitioner education. Am. J. Crit. Care 2002, 11, 27–33. [Google Scholar]
- Campbell, H.S.; Sletten, M.; Petty, T. Patient perceptions of tobacco cessation services in dental offices. J. Am. Dent. Assoc. 1999, 130, 219–226. [Google Scholar] [CrossRef]
- Ellerbeck, E.F.; Choi, W.S.; McCarter, K.; Jolicoeur, D.G.; Greiner, A.; Ahluwalia, J.S. Impact of patient characteristics on physician’s smoking cessation strategies. Prev. Med. 2003, 36, 464–470. [Google Scholar] [CrossRef]
- Ossip-Klein, D.J.; McIntosh, S.; Utman, C.; Burton, K.; Spada, J.; Guido, J. Smokers ages 50+: Who gets physician advice to quit? Prev. Med. 2000, 31, 364–369. [Google Scholar] [CrossRef]
- Ratner, P.A.; Johnson, J.L.; Richardson, C.G.; Bottorff, J.L.; Moffat, B.; Mackay, M.; Fofonff, D.; Kingsbury, K.; Miller, C.; Budz, B. Efficacy of smoking-cessation intervention for elective-surgical patients. Res. Nurs. Health 2004, 27, 148–161. [Google Scholar] [CrossRef]
- Rikard-Bell, G.; Donnelly, N.; Ward, J. Preventive dentistry: What do Australian patients endorse and recall of smoking cessation advice by their dentists? Br. Dent. J. 2003, 194, 159–164. [Google Scholar] [CrossRef] [PubMed]
- Slama, K.J.; Redman, S.; Cockburn, J.; Sanson-Fisher, R.W. Community views about the role of general practitioners in disease prevention. Fam. Pract. 1989, 6, 203–209. [Google Scholar] [CrossRef] [PubMed]
- Stanford, J.B.; Solberg, L.I. Rural patients’ interests in preventive medical care. J. Am. Board Fam. Pract. 1991, 4, 11–18. [Google Scholar]
- Wallace, P.G.; Haines, A.P. General practitioner and health promotion: What patients think. Br. Med. J. 1984, 289, 533–536. [Google Scholar] [CrossRef] [PubMed]
- Hyndman, K.; Thomas, R.; Patterson, S.; Compton, S.; Schira, R.; Godfrey, C.; Bradley, J.; Chachula, K. Effectiveness of tobacco intervention education in health professional students’ practice: A systematic review protocol. JBI Database Syst. Rev. Implement. Rep. 2016, 14, 78–90. [Google Scholar] [CrossRef] [PubMed]
- The Joanna Briggs Institute. Joanna Briggs Institute Reviewer’s Manual [Online]; Joanna Briggs Institute: Adelaide, Australia, 2014; Available online: http://joannabriggs.org/assets/-docs/sumari/reviewersmanual-2014.pdf (accessed on 24 April 2019).
- Higgins, J.P.T.; Green, S. (Eds.) Cochrane Handbook for Systematic Reviews of Interventions [Online], Version 5.1.0; The Cochrane Collaboration. 2011. Available online: https://web.archive.org/web/20190907014421/http://handbook-5-1.cochrane.org/ (accessed on 7 September 2019).
- Review Manager (RevMan) [Computer Program]; Version 5.3; The Cochrane Collaboration: Copenhagen, Denmark, 2014; Available online: https://web.archive.org/web/20190914183308/https://community.cochrane.org/help/tools-and-software/revman-5 (accessed on 14 September 2019).
- Allen, B.; Pederson, L.L.; Leonard, E.H. Effectiveness of physicians-in-training counseling for smoking cessation in African Americans. J. Natl. Med. Assoc. 1998, 90, 597–604. [Google Scholar] [PubMed]
- Cannick, G.F.; Horowitz, A.M.; Garr, D.R.; Reed, S.G.; Neville, B.W.; Day, T.A.; Woolson, R.F.; Lackland, D.T. Use of the OSCE to evaluate brief communication skills training for dental students. J. Dent. Educ. 2007, 71, 1203–1209. [Google Scholar]
- Carpenter, K.M.; Cohn, L.G.; Glynn, L.H.; Stoner, S.A. Brief interventions for tobacco users: Using the Internet to train healthcare providers. Int. Electron. J. Health Educ. 2008, 11, 1–12. [Google Scholar]
- Cornuz, J.; Humair, J.-P.; Seematter, L.; Stoianov, R.; van Melle, G.; Stalder, H.; Pécoud, A. Efficacy of resident training in smoking cessation: A randomized, controlled trial of a program based on application of behavioral theory and practice with standardized patients. Ann. Intern. Med. 2002, 136, 429–437. [Google Scholar] [CrossRef]
- Hebert, J.R.; Kristeller, J.; Ockene, J.K.; Landon, J.; Luippold, R.; Goldberg, R.J.; Kalan, K. Patient characteristics and the effect of three physician-delivered smoking interventions. Prev. Med. 1992, 21, 557–573. [Google Scholar] [CrossRef]
- Koerber, A.; Crawford, J.; O’Connell, K. The effects of teaching dental students brief motivational interviewing for smoking-cessation counseling: A pilot study. J. Dent. Educ. 2003, 67, 439–447. [Google Scholar] [PubMed]
- Ockene, J.K.; Kristeller, J.; Goldberg, R.; Amick, T.L.; Pekow, P.S.; Hosmer, D.; Quirk, M.; Kalan, K. Increasing the efficacy of physician-delivered smoking interventions. J. Gen. Intern. Med. 1991, 6, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Ockene, J.K.; Hayes, R.B.; Churchill, L.C.; Crawford, S.L.; Jolicoeur, D.G.; Murray, D.M.; Shoben, A.B.; David, S.P.; Ferguson, K.J.; Huggett, K.N.; et al. Teaching medical students to help patients quit smoking: Outcomes of a 10-school randomized controlled trial. J. Gen. Intern. Med. 2016, 31, 172–181. [Google Scholar] [CrossRef] [PubMed]
- Rapp, K.; Büchele, G.; Jähnke, A.G.; Weiland, S.K. A cluster-randomized trial on smoking cessation in German student nurses. Prev. Med. 2006, 42, 443–448. [Google Scholar] [CrossRef]
- Steinemann, S.; Roytman, T.; Chang, J.; Holzman, J.; Hishinuma, E.; Nagoshi, M.; Tam, E.; Murakami, S.; Wong, J. Impact of education on smoking cessation counseling by surgical residents. Am. J. Surg. 2005, 189, 44–46. [Google Scholar] [CrossRef]
- Strecher, V.J.; O’Malley, M.S.; Villagra, V.G.; Campbell, E.E.; Gonzalez, J.J.; Irons, T.C.; Kenney, R.D.; Turner, R.C.; Rogers, C.S.; Lyles, M.F.; et al. Can residents be trained to counsel patients about quitting smoking? J. Gen. Intern. Med. 1991, 6, 9–17. [Google Scholar] [CrossRef]
- Adkins, J.R. The Effects of Standardized Patient Training on Dental Hygiene Students’ Confidence in Delivering Tobacco Cessation Counseling. Master’s Thesis, University of North Carolina, Chapel Hill, NC, USA, 2009. [Google Scholar]
- Brame, J.L.; Martin, R.; Tavoc, T.; Stein, M.; Curran, A.E. A randomized controlled trial of the effect of standardized patient scenarios on dental hygiene students’ confidence in providing tobacco dependence counseling. J. Dent. Hyg. 2012, 86, 282–291. [Google Scholar]
- Borenstein, M.; Hedges, L.V.; Higgins, J.P.T.; Rothstein, H.R. Introduction to Meta-Analysis; John Wiley & Sons: Chichester, UK, 2009. [Google Scholar]
- Tufaranu, C.; Munn, Z.; Stephenson, M.; Aromataris, E. Fixed or random effects meta-analysis? Common methodological issues in systematic reviews of effectiveness. Int. J. Evid.-Based Healthc. 2015, 13, 196–207. [Google Scholar] [CrossRef] [Green Version]
- Tufanaru, C.; Munn, Z.; Aromataris, E.; Campbell, J.; Hopp, L. Systematic reviews of effectiveness. In Joanna Briggs Institute Reviewer’s Manual [Online]; Chapter 3; Aromataris, E., Munn, Z., Eds.; The Joanna Briggs Institute: Adelaide, Australia, 2017; Available online: https://reviewersmanual.joannabriggs.org (accessed on 29 September 2019).
- Carpenter, K.M.; Watson, J.M.; Raffety, B.; Chabal, C. Teaching brief interventions for smoking cessation via an interactive computer-based tutorial. J. Health Psychol. 2003, 8, 149–160. [Google Scholar] [CrossRef]
- Coultas, D.B.; Klecan, D.A.; Whitten, R.M.; Obenshain, S.S.; Rubin, R.H.; Wiese, W.H.; Wilson, B.E.; Woodall, G.W.; Stidley, C.A. Training medical students in smoking-cessation counseling. Acad. Med. 1994, 69, S48–S50. [Google Scholar] [CrossRef]
- Garg, A.; Butz, A.M.; Dworkin, P.H.; Lewis, R.A.; Thompson, R.E.; Serwint, J.R. Improving the management of family psychosocial problems at low-income children’s well-child care visits: The WE CARE project. Pediatrics 2007, 120, 547–558. [Google Scholar] [CrossRef] [PubMed]
- Hymowitz, N.; Schwab, J.V.; Haddock, C.K.; Pyle, S.A.; Schwab, L.M. The pediatric residency training on tobacco project: Four-year resident outcome findings. Prev. Med. 2007, 45, 481–490. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mounsey, A.L.; Bovbjerg, V.; White, L.; Gazewood, J. Do students develop better motivational interviewing skills through role-play with standardised patients or with student colleagues? Med. Educ. 2006, 40, 775–780. [Google Scholar] [CrossRef] [PubMed]
- Papadakis, M.A.; Croughan-Minihane, M.; Fromm, L.J.; Wilkie, H.A.; Ernster, V.L. A comparison of two methods to teach smoking-cessation techniques to medical students. Acad. Med. 1997, 72, 725–727. [Google Scholar] [CrossRef]
- Prochaska, J.J.; Gali, K.; Miller, B.; Hauer, K.E. Medical students’ attention to multiple risk behaviors: A standardized patient examination. J. Gen. Intern. Med. 2012, 27, 700–707. [Google Scholar] [CrossRef]
- Roche, A.M.; Eccleston, P.; Sanson-Fisher, R. Teaching smoking cessation skills to senior medical students: A block-randomized controlled trial of four different approaches. Prev. Med. 1996, 25, 251–258. [Google Scholar] [CrossRef]
- Seim, H.C.; Verhoye, J.R. Comparison of training techniques using a patient-centred approach to smoking cessation. Med. Educ. 1995, 29, 139–143. [Google Scholar] [CrossRef]
- Sejr, H.S.; Osler, M. Do smoking and health education influence student nurses’ knowledge, attitudes, and professional behavior? Prev. Med. 2002, 34, 260–265. [Google Scholar] [CrossRef]
- Stolz, D.; Langewitz, W.; Meyer, A.; Pierer, K.; Tschudi, P.; S’ng, C.T.; Strobel, W.; Perruchoud, A.P.; Fagerström, K.; Tamm, M. Enhanced didactic methods of smoking cessation training for medical students-a randomized study. Nicotine Tob. Res. 2012, 14, 224–228. [Google Scholar] [CrossRef]
- Roche, A.M.; Eccleston, P.; Jordan, D. Smoking-related knowledge and attitudes of senior Australian medical students. Tob. Control 1996, 5, 271–279. [Google Scholar] [CrossRef]
- Royce, J.M.; Gorin, S.S.; Edelman, B.; Rendino-Perrone, R.; Orlandi, M.A. Student nurses and smoking cessation. Prog. Clin. Biol. Res. 1990, 339, 49–71. [Google Scholar] [PubMed]
- Strayer, S.M.; Pelletier, S.L.; Martindale, J.R.; Rais, S.; Powell, J.; Schorling, J.B. A PDA-based counseling tool for improving medical student smoking cessation counseling. Fam. Med. 2010, 42, 350–357. [Google Scholar] [PubMed]
- Ward, J.; Sanson-Fisher., R. Does a 3-day workshop for family medicine trainees improve preventive care? A randomized control trial. Prev. Med. 1996, 25, 741–747. [Google Scholar] [CrossRef] [PubMed]
- Schünemann, H.; Brożek, J.; Guyatt, G.; Oxman, A. (Eds.) GRADE Handbook for Grading Quality of Evidence and Strength of Recommendations [Online]; The GRADE Working Group; 2013; Available online: https://gdt.gradepro.org/app/handbook/handbook.html (accessed on 29 September 2019).
- Evidence Prime, Inc. GRADEpro Guideline Development Tool [Online]; McMaster University: Hamilton, ON, Canada, 2015; Available online: https://gradepro.org/cite/ (accessed on 29 September 2019).
- World Health Organization. Tobacco. Available online: https://www.who.int/en/news-room/fact-sheets/detail/tobacco (accessed on 29 September 2019).
- WHO Framework Convention on Tobacco Control. Guidelines for Implementation of Article 14. Demand Reduction Measures Concerning Tobacco Dependence and Cessation. Available online: https://www.who.int/fctc/treaty_instruments/adopted/Guidelines_Article_14_English.pdf (accessed on 29 September 2019).
- World Health Organization. Offer Help to Quit Tobacco Use. Available online: https://www.who.int/tobacco/mpower/publications/en_tfi_mpower_brochure_o.pdf?ua=1 (accessed on 29 September 2019).
- Leone, F.T.; Evers-Casey, S.; Veloski, J.; Patkar, A.A.; Kanzleiter, L. Short-, intermediate-, and long-term outcomes of Pennsylvania’s continuum of tobacco education pilot project. Nicotine Tob. Res. 2009, 11, 387–393. [Google Scholar] [CrossRef] [PubMed]
- Geller, A.C.; Brooks, D.R.; Powers, C.A.; Brooks, K.R.; Rigotti, N.A.; Bognar, B.; McIntosh, S.; Zapka, J. Tobacco cessation and prevention practices reported by second and fourth year students at US medical schools. J. Gen. Intern. Med. 2008, 23, 1071–1076. [Google Scholar] [CrossRef]
- Geller, A.C.; Prout, M.N.; Miller, D.R.; Siegel, B.; Sun, T.; Ockene, J.; Koh, H.K. Evaluation of a cancer prevention and detection curriculum for medical students. Prev. Med. 2002, 35, 78–86. [Google Scholar] [CrossRef]
- Kosowicz, L.Y.; Pfeiffer, C.A.; Vargas, M. Long-term retention of smoking cessation counseling skills learned in the first year of medical school. J. Gen. Intern. Med. 2007, 22, 1161–1165. [Google Scholar] [CrossRef]
- Spangler, J.G.; George, G.; Foley, K.L.; Crandall, S.J. Tobacco intervention training: Current efforts and gaps in US medical schools. JAMA 2002, 288, 1102–1109. [Google Scholar] [CrossRef]
- Hayes, R.B.; Geller, A.C.; Crawford, S.L.; Jolicoeur, D.G.; Churchill, L.C.; Okuyemi, K.S.; David, S.P.; Adams, M.; Waugh, J.; Allen, S.E.; et al. Medical school curriculum characteristics associated with intentions and frequency of tobacco dependence treatment among 3rd year U.S. medical students. Prev. Med. 2015, 72, 56–63. [Google Scholar] [CrossRef] [Green Version]
- Cornuz, J.; Zellweger, J.; Mounoud, C.; Decrey, H.; Pecoud, A.; Burnand, B. Smoking cessation counseling by residents in an outpatient clinic. Prev. Med. 1997, 26, 292–296. [Google Scholar] [CrossRef]
- Collins, R.L.; D’Angelo, S.; Stearns, S.D.; Campbell, L.R. Training pediatric residents to provide smoking cessation counseling to parents. Sci. World J. 2005, 5, 410–419. [Google Scholar] [CrossRef] [PubMed]
- Secker-Walker, R.H.; Solomon, L.J.; Flynn, B.S.; LePage, S.S.; Crammond, J.E.; Worden, J.K.; Mead, P.B. Training obstetric and family practice residents to give smoking cessation advice during prenatal care. Am. J. Obstet. Gynecol. 1992, 166, 1356–1363. [Google Scholar] [CrossRef]
- Mitchell, J.; Brown, J.B.; Smith, C. Interprofessional education: A nurse practitioner impacts family medicine residents’ smoking cessation counseling experiences. J. Interprofessional Care 2009, 23, 401–409. [Google Scholar] [CrossRef] [PubMed]
- Geller, A.C.; Hayes, R.B.; Leone, F.; Churchill, L.C.; Leung, K.; Reed, G.; Jolicoeur, D.; Okuliar, C.; Adams, M.; Murray, D.; et al. Tobacco dependence treatment teaching by medical school clerkship preceptors: Survey responses from more than 1000 US medical students. Prev. Med. 2013, 57, 81–86. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Butler, K.M.; Rayens, M.K.; Zhang, M.; Maggio, L.G.; Riker, C. Tobacco dependence treatment education for baccalaureate nursing students. J. Nurs. Educ. 2009, 48, 249–254. [Google Scholar] [CrossRef] [PubMed]
- Chan, S.S.; So, W.K.; Wong, D.C.; Lam, T.H. Building an integrated model of tobacco control education in the nursing curriculum: Findings of a students’ survey. J. Nurs. Educ. 2008, 47, 223–226. [Google Scholar] [CrossRef] [PubMed]
- Lenz, B.K. Beliefs, knowledge, and self-efficacy of nursing students regarding tobacco cessation. Am. J. Prev. Med. 2008, 35, S494–S500. [Google Scholar] [CrossRef]
- Davies, B.L.; Matte-Lewis, L.; O’Connor, A.M.; Dulberg, C.S.; Drake, E.R. Evaluation of the “Time to Quit” self-help smoking cessation program. Can. J. Public Health 1992, 83, 19–23. [Google Scholar]
- Shishani, K.; Stevens, K.; Dotson, J.; Riebe, C. Improving nursing students’ knowledge using online education and simulation to help smokers quit. Nurse Educ. Today 2013, 33, 210–213. [Google Scholar] [CrossRef]
- Sohn, M.; Ahn, Y.; Park, H.; Lee, M. Simulation-based smoking cessation intervention education for undergraduate nursing students. Nurse Educ. Today 2012, 32, 868–872. [Google Scholar] [CrossRef]
- Hudmon, K.S.; Bardel, K.; Kroon, L.A.; Fenlon, C.M.; Corelli, R.L. Tobacco education in U.S. schools of pharmacy. Nicotine Tob. Res. 2005, 7, 225–232. [Google Scholar] [CrossRef] [PubMed]
- Kristina, S.A.; Thavorncharoensap, M.; Pongcharoensuk, P.; Montakantikul, P.; Suansanae, T.; Prabandari, Y.S. Effectiveness of tobacco education for pharmacy students in Indonesia. Asian Pac. J. Cancer Prev. 2014, 15, 10783–10786. [Google Scholar] [CrossRef] [PubMed]
- Gordon, J.S.; Severson, H.H.; Seely, J.R.; Christiansen, S. Development and evaluation of an interactive tobacco cessation CD-ROM educational program for dental students. J. Dent. Educ. 2004, 68, 361–369. [Google Scholar] [PubMed]
- Singleton, J.A.; Carrico, R.M.; Myers, J.A.; Scott, D.A.; Wilson, R.W.; Worth, C.T. Tobacco cessation treatment education for dental students using standardized patients. J. Dent. Educ. 2014, 78, 895–905. [Google Scholar] [PubMed]
- Romito, L.; Schrader, S.; Zahl, D. Using experiential learning and OSCEs to teach and assess tobacco dependence education with first-year dental students. J. Dent. Educ. 2014, 78, 703–713. [Google Scholar]
- Romito, L.; Budyn, C.; Oklak, M.A.; Gotlib, J.; Eckert, G.J. Tobacco use and health risks in two dental clinic populations: Implementation and evaluation of a brief targeted intervention. Gen. Dent. 2012, 60, e326–e334. [Google Scholar]
- Ehizele, A.O.; Azodo, C.C.; Ezeja, E.B.; Ehigiator, O. Nigerian dental students’ compliance with the 4As approach to tobacco cessation. J. Prev. Med. Hyg. 2011, 52, 12–16. [Google Scholar]
- Walsh, S.E.; Singleton, J.A.; Worth, C.T.; Krugler, J.; Moore, R.; Wesley, G.C.; Mitchell, C.K. Tobacco cessation counseling training with standardized patients. J. Dent. Educ. 2007, 71, 1171–1178. [Google Scholar]
- Boyd, L.D.; Fun, K.; Madden, T.E. Initiating tobacco curricula in dental hygiene education. Subst. Abus. 2006, 27, 53–60. [Google Scholar] [CrossRef]
- Evans, M.W.; Hawk, C.; Boyd, J. Smoking cessation for chiropractic interns: A theory-driven intervention. J. Am. Chiropr. Assoc. 2006, 43, 13–19. [Google Scholar]
- Evans, M.W.; Hawk, C.; Strasser, S.M. An educational campaign to increase chiropractic intern advising roles on patient smoking cessation. Chiropr. Osteopat. 2006, 14, 1–9. [Google Scholar]
- Hawk, C.; Kaeser, M.A.; Beavers, D.V. Feasibility of using a standardized patient encounter for training chiropractic students in tobacco cessation counseling. J. Chiropr. Educ. 2013, 27, 135–140. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pignataro, R.M.; Gurka, M.; Jones, D.L.; Kershner, R.E.; Ohtake, P.J.; Stauber, W.; Swisher, A.K. Educating physical therapist students in tobacco cessation counseling: Feasibility and preliminary outcomes. J. Phys. Ther. Educ. 2015, 29, 68–79. [Google Scholar] [CrossRef] [PubMed]
- Price, J.H.; Mohamed, I.; Jeffrey, J.D. Tobacco intervention training in American College of Nurse-Midwives accredited education programs. J. Midwifery Women’s Health 2008, 53, 68–74. [Google Scholar] [CrossRef]
- Spafford, M.M.; Iley, M.D.; Schultz, A.S.H.; Kennedy, R.D. Tobacco dependence education in Optometry: A Canadian pilot study assessing practices and opportunities. Optom. Educ. 2010, 36, 38–44. [Google Scholar]
- Coan, L.L.; Christen, A.; Romito, L. Evolution of a tobacco cessation curriculum for dental hygiene students at Indiana University School of Dentistry. J. Dent. Educ. 2007, 71, 776–784. [Google Scholar]
- Schmelz, A.N.; Nixon, B.; McDaniel, A.; Hudmon, K.S.; Zillich, A.J. Evaluation of an online tobacco cessation course for health professions students. Am. J. Pharm. Educ. 2010, 74, 1–9. [Google Scholar] [CrossRef]
- Zwar, N.; Richmond, R.; Davidson, D.; Hasan, I. Postgraduate education for doctors in smoking cessation. Drug Alcohol Rev. 2009, 28, 466–473. [Google Scholar] [CrossRef]
- Lewis, F.M. Perspectives on Models of Interpersonal Health Behavior. In Health Behavior and Health Education: Theory, Research, and Practice, 3rd ed.; Glanz, K., Rimer, B.K., Lewis, F.M., Eds.; Jossey-Bass: San Francisco, CA, USA, 2002; pp. 265–273. [Google Scholar]
- Gould, G.S.; Twyman, L.; Stevenson, L.; Gribbin, G.R.; Bonevski, B.; Palazzi, K.; Zeev, Y.B. What components of smoking cessation care during pregnancy are implemented by health providers? A systematic review and meta-analysis. Br. Med. J. Open 2019, 9, e026037. [Google Scholar] [CrossRef] [Green Version]
- Geller, A.C.; Brooks, D.R.; Woodring, B.; Oppenheimer, S.; McCabe, M.; Rogers, J.; Timm, A.; Resnick, E.A.; Winicko, J.P. Smoking cessation counseling for parents during child hospitalization: A national survey of pediatric nurses. Public Health Nurs. 2011, 28, 475–484. [Google Scholar] [CrossRef]
- Vijayaraghavan, M.; Yuan, P.; Gregorich, S.; Lum, P.; Appelle, N.; Napoles, A.M.; Kalkhoran, S.; Satterfield, J. Disparities in receipt of 5As for smoking cessation in diverse primary care and HIV clinics. Prev. Med. Rep. 2017, 6, 80–87. [Google Scholar] [CrossRef] [PubMed]
- Baltaci, D.; Aydin, L.Y.; Alasan, F.; Deler, M.H.; Karacam, M.S.; Turker, Y.; Gur, M.; Sariguzel, F. Evaluation of smoking cessation practice by physicians for hospitalized patients in a tertiary hospital. J. Pak. Med. Assoc. 2016, 66, 1547–1553. [Google Scholar] [PubMed]
- Katz, D.A.; Vander Weg, M.W.; Holman, J.; Nugent, A.; Baker, L.; Johnson, S.; Hillis, S.L.; Titler, M. The Emergency Department Action in Smoking Cessation (EDASC) Trial: Impact on delivery of smoking cessation counseling. Acad. Emerg. Med. 2012, 19, 409–420. [Google Scholar] [CrossRef] [PubMed]
- Ye, L.; Goldie, C.; Sharma, T.; John, S.; Bamford, M.; Smith, P.M.; Selby, P.; Schultz, A.S.H. Tobacco-nicotine education and training for health-care professional students and practitioners: A systematic review. Nicotine Tob. Res. 2018, 20, 531–542. [Google Scholar] [CrossRef]
- Bandura, A. Social Foundations of Thought and Action: A Social Cognitive Theory; Prentice-Hall: Englewood Cliffs, NJ, USA, 1986. [Google Scholar]
- Bandura, A. Self-Efficacy: The Exercise of Control; W.H. Freeman and Company: New York, NY, USA, 1997. [Google Scholar]
- Bandura, A. Social Learning Theory; Prentice-Hall: Englewood Cliffs, NJ, USA, 1977. [Google Scholar]
- O’Leary, A. Self-efficacy and health. Behav. Res. Ther. 1985, 23, 437–451. [Google Scholar] [CrossRef]
- Baranowski, T.; Perry, C.L.; Parcel, G.S. How Individuals, Environments, and Health Behavior Interact. In Health Behavior and Health Education: Theory, Research, and Practice, 3rd ed.; Glanz, K., Rimer, B.K., Lewis, F.M., Eds.; Jossey-Bass: San Francisco, CA, USA, 2002; pp. 165–184. [Google Scholar]
- Prochaska, J.O.; DiClemente, C.C. Stages and processes of self-change of smoking: Toward an integrative model of change. J. Consult. Clin. Psychol. 1983, 51, 390–395. [Google Scholar] [CrossRef]
- Prochaska, J.O.; DiClemente, C.C.; Norcross, J.C. In search of how people change: Applications to addictive behaviors. Am. Psychol. 1992, 47, 1102–1114. [Google Scholar] [CrossRef]
- Miller, W.R.; Rollnick, S. Motivational Interviewing: Preparing People for Change; The Guilford Press: New York, NY, USA, 1991. [Google Scholar]
- Miller, W.R.; Rollnick, S. Motivational Interviewing: Preparing People for Change, 2nd ed.; The Guilford Press: New York, NY, USA, 2002. [Google Scholar]
- Green, L.; Kreuter, M. Health Promotion Planning: An Educational and Ecological Approach, 4th ed.; McGraw-Hill: Boston, MA, USA, 2005. [Google Scholar]
- Di Sessa, A.A.; Minstrell, J. Cultivating Conceptual Change with Benchmark Lessons. In Thinking Practices; Greeno, J.G., Ed.; Lawrence Erlbaum Associates: Mahwah, NJ, USA, 1998; pp. 220–243. [Google Scholar]







| Health Professional Programs | Post-Graduate Medical Programs |
|---|---|
| Chiropractic Therapy; Dental Hygiene; Dental Therapy; Dentistry; Medicine; Midwifery; Naturopathic Medicine; Nursing (Registered Nurses, Registered Psychiatric Nurses, Advanced Practice Nurses/Nurse Practitioners; Licensed Practical Nurses); Occupational Therapy; Optometry; Pharmacy; Physical Therapy; Psychology; Respiratory Therapy; Social Work; and Speech Language Therapy | Anesthesia; Cardiac Surgery; Cardiology; Community Medicine; Critical Care Medicine; Dermatology; Endocrinology and Metabolism; Emergency Medicine; Family Medicine; General Medicine; Medical Oncology; Nephrology; Neurology; Obstetrics/Gynecology; Ophthalmology; Orthopedic Surgery; Otolaryngology; Pediatrics; Plastic Surgery; Psychiatry; Radiation Oncology; Respiratory Medicine; Surgery; and Vascular Surgery |
| Systematic Review Databases | Published Studies Databases | Grey Literature |
|---|---|---|
| JBI Database of Systematic Reviews and Implementation Reports; the Cochrane Library of Systematic Reviews (including the Tobacco Addiction Group Reviews); the Campbell Collaboration Library. The National Health Centre Reviews and Dissemination databases [Database of Systematic Reviews; Health Technology Assessment; Economic Evaluation Database]; Health Technology Assessment International; Evidence of Policy and Practice Information; Physiotherapy Evidence Database; Occupational Therapy Systematic Evaluation of Evidence; PROSPERO; PubMed; CINAHL and Epistemonikos from July 2015 | Allied and Complementary Medicine; CINAHL; PubMed; EMBASE; Scopus; SocIndex; PsychInfo; Academic Search Premier; Education Resources Information Center; Education Search Complete; Health Source-Nursing/Academic Edition; Translating Research into Practice; Google Scholar; Web of Science; and Natural Standard | Theses Canada Portal; ProQuest Dissertations and Theses; CADTH; Directory of Grey Literature via New York Academy of Medicine website; websites of the Canadian Council of Tobacco Control (until March 30, 2012); Canadian Centre on Substance Abuse; Health Canada; and Canadian Public Health Association |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hyndman, K.; Thomas, R.E.; Schira, H.R.; Bradley, J.; Chachula, K.; Patterson, S.K.; Compton, S.M. The Effectiveness of Tobacco Dependence Education in Health Professional Students’ Practice: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Int. J. Environ. Res. Public Health 2019, 16, 4158. https://doi.org/10.3390/ijerph16214158
Hyndman K, Thomas RE, Schira HR, Bradley J, Chachula K, Patterson SK, Compton SM. The Effectiveness of Tobacco Dependence Education in Health Professional Students’ Practice: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. International Journal of Environmental Research and Public Health. 2019; 16(21):4158. https://doi.org/10.3390/ijerph16214158
Chicago/Turabian StyleHyndman, Kathryn, Roger E. Thomas, H. Rainer Schira, Jenifer Bradley, Kathryn Chachula, Steven K. Patterson, and Sharon M. Compton. 2019. "The Effectiveness of Tobacco Dependence Education in Health Professional Students’ Practice: A Systematic Review and Meta-Analysis of Randomized Controlled Trials" International Journal of Environmental Research and Public Health 16, no. 21: 4158. https://doi.org/10.3390/ijerph16214158
APA StyleHyndman, K., Thomas, R. E., Schira, H. R., Bradley, J., Chachula, K., Patterson, S. K., & Compton, S. M. (2019). The Effectiveness of Tobacco Dependence Education in Health Professional Students’ Practice: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. International Journal of Environmental Research and Public Health, 16(21), 4158. https://doi.org/10.3390/ijerph16214158






