Geodemographic Area Classification and Association with Mortality: An Ecological Study of Small Areas of Cyprus
Abstract
1. Introduction
2. Materials and Methods
2.1. Data
2.2. Statistical Methods
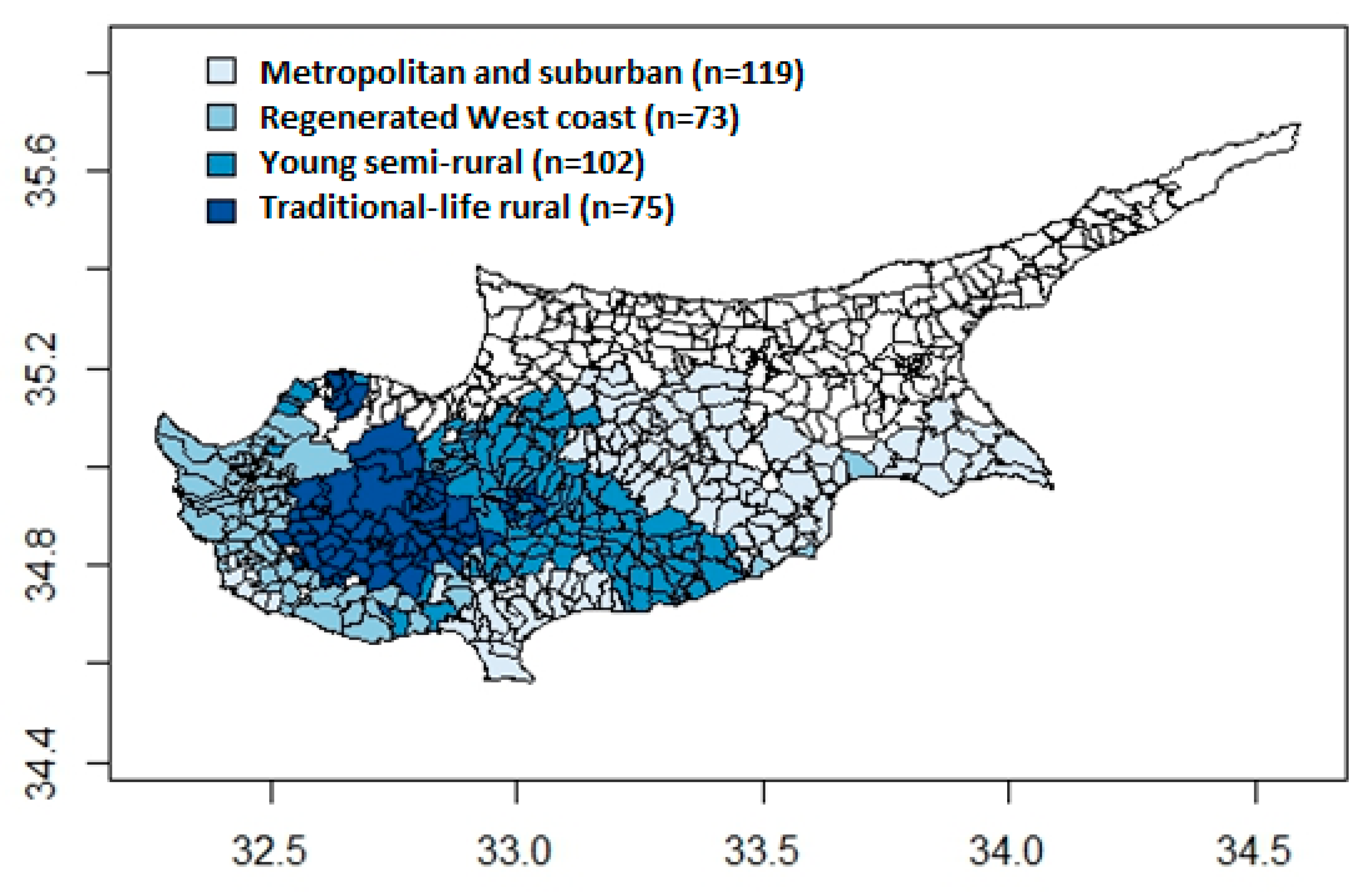
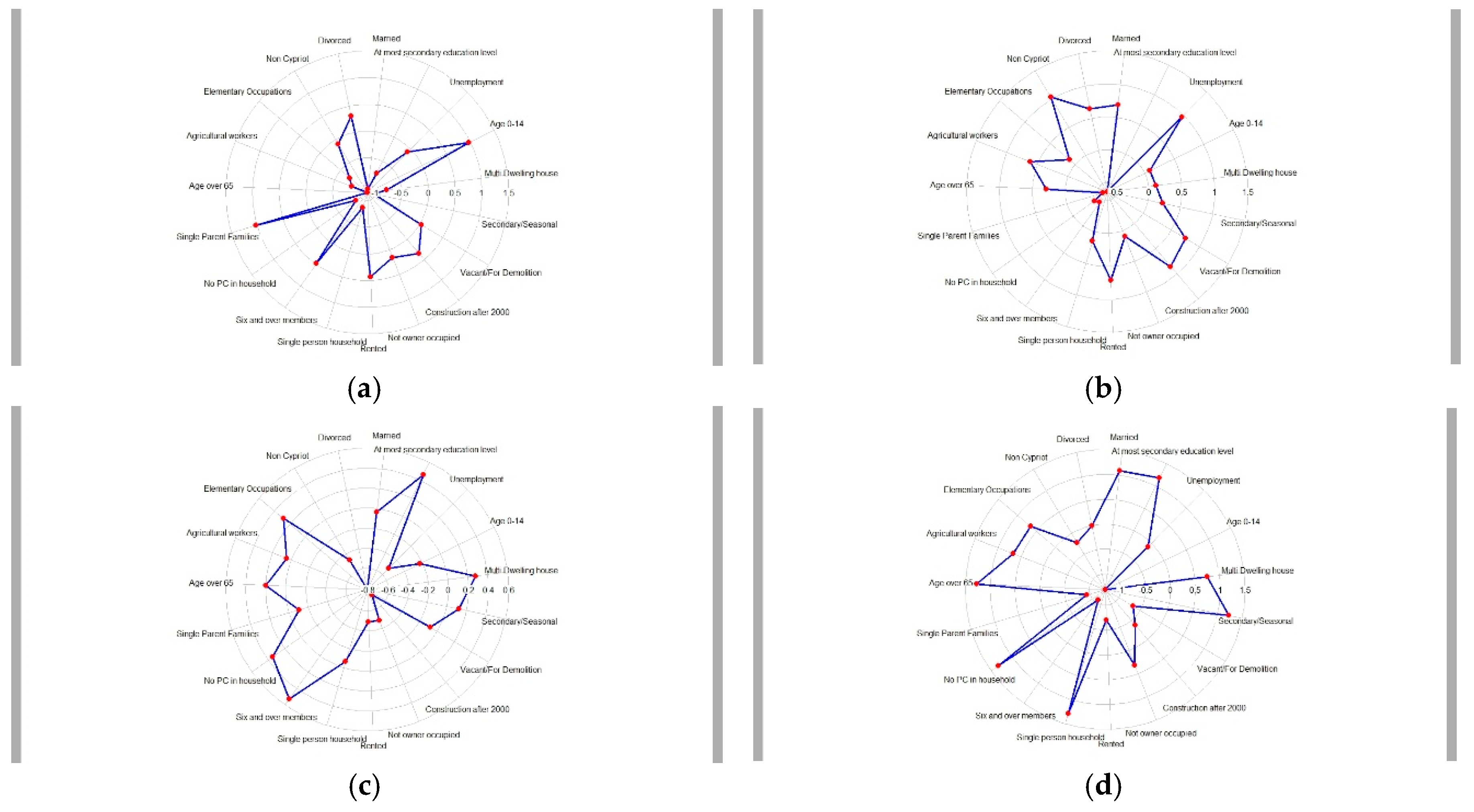
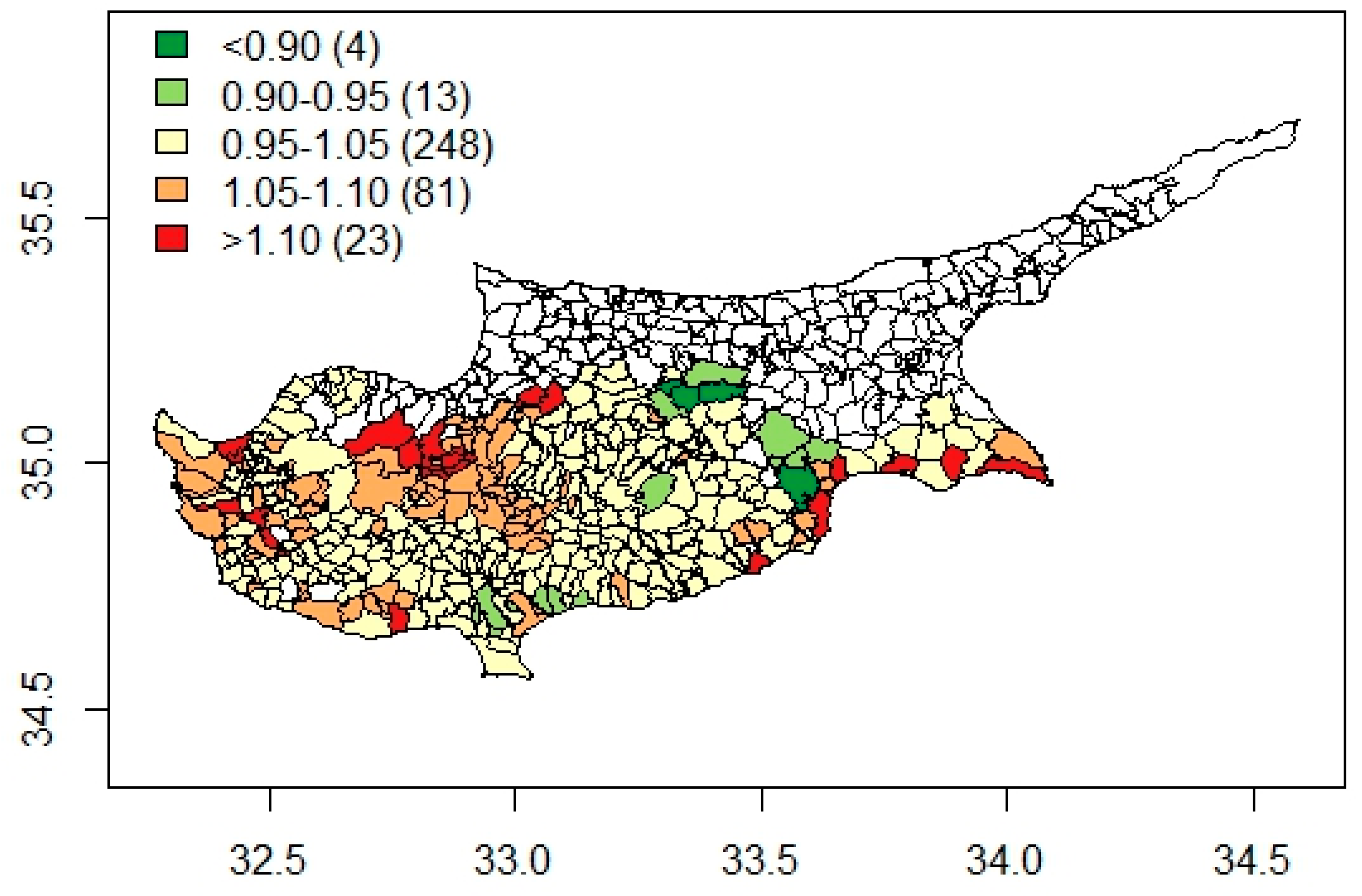
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Curtis, S.; Rees Jones, I. Is There a Place for Geography in the Analysis of Health Inequality? Sociol. Health Illn. 1998, 20, 645–672. [Google Scholar] [CrossRef]
- Ellaway, A.; Benzeval, M.; Green, M.; Leyland, A.; MacIntyre, S. “Getting sicker quicker”: Does living in a more deprived neighbourhood mean your health deteriorates faster? Health Place 2012, 18, 132–137. [Google Scholar] [CrossRef] [PubMed]
- Diez Roux, A. V Investigating Neighborhood and Area Effects on Health. Am. J. Public Health 2001, 91, 1783–1789. [Google Scholar] [CrossRef] [PubMed]
- Mackenbach, J.P. Health Inequalities: Europe in Profile; UK Presidency of the EU: London, UK, 2006. [Google Scholar]
- Marmot, M.; Wilkinson, R. Social Determinants of Health; Oxford University Press: Oxford, UK, 2005; ISBN 9780198565895. [Google Scholar]
- Braveman, P.A.; Egerter, S.A.; Woolf, S.H.; Marks, J.S. When Do We Know Enough to Recommend Action on the Social Determinants of Health? Am. J. Prev. Med. 2011, 40, S58–S66. [Google Scholar] [CrossRef] [PubMed]
- Meijer, M.; Röhl, J.; Bloomfield, K.; Grittner, U. Do neighborhoods affect individual mortality? A systematic review and meta-analysis of multilevel studies. Soc. Sci. Med. 2012, 74, 1204–1212. [Google Scholar] [CrossRef] [PubMed]
- Diez Roux, A.V.; Mair, C. Neighborhoods and health. Ann. N. Y. Acad. Sci. 2010, 1186, 125–145. [Google Scholar] [CrossRef] [PubMed]
- Havard, S.; Deguen, S.; Bodin, J.; Louis, K.; Laurent, O.; Bard, D. A small-area index of socioeconomic deprivation to capture health inequalities in France. Soc. Sci. Med. 2008, 67, 2007–2016. [Google Scholar] [CrossRef] [PubMed]
- Pampalon, R.; Hamel, D.; Gamache, P.; Raymond, G. A deprivation index for health planning in Canada. Chronic Dis. Can. 2009, 29, 178–191. [Google Scholar] [PubMed]
- Juhász, A.; Nagy, C.; Páldy, A.; Beale, L. Development of a Deprivation Index and its relation to premature mortality due to diseases of the circulatory system in Hungary, 1998–2004. Soc. Sci. Med. 2010, 70, 1342–1349. [Google Scholar] [CrossRef]
- Panczak, R.; Galobardes, B.; Voorpostel, M.; Spoerri, A.; Zwahlen, M.; Egger, M. A Swiss neighbourhood index of socioeconomic position: Development and association with mortality. J. Epidemiol. Community Health 2012, 66, 1129–1136. [Google Scholar] [CrossRef]
- Lalloué, B.; Monnez, J.-M.; Padilla, C.; Kihal, W.; Le Meur, N.; Zmirou-Navier, D.; Deguen, S. A statistical procedure to create a neighborhood socioeconomic index for health inequalities analysis. Int. J. Equity Health 2013, 12, 21. [Google Scholar] [CrossRef] [PubMed]
- Meijer, M.; Engholm, G.; Gritter, U.; Bloomfield, K. A socioeconomic deprivation index for small areas in Denmark. Scand. J. Public Health 2013, 41, 560–569. [Google Scholar] [CrossRef] [PubMed]
- Allik, M.; Brown, D.; Dundas, R.; Leyland, A.H. Developing a new small-area measure of deprivation using 2001 and 2011 census data from Scotland. Health Place 2016, 39, 122–130. [Google Scholar] [CrossRef] [PubMed]
- Lamnisos, D.; Lambrianidou, G.; Lavranos, G.; Middleton, N. A small-area validation of deprivation using 2011 census data from Cyprus. Eur. J. Public Health 2017, 27, 431. [Google Scholar] [CrossRef][Green Version]
- Lamnisos, D.; Lambrianidou, G.; Middleton, N. Small-area socioeconomic deprivation indices in Cyprus: Development and association with premature mortality. BMC Public Health 2019, 19, 627. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.S.; Chuang, Y.C. Neighborhood effects on an individual’s health using neighborhood measurements developed by factor analysis and cluster analysis. J. Urban Health 2009, 86, 5–18. [Google Scholar] [CrossRef] [PubMed]
- Rapkin, B.D.; Luke, D.A. Cluster analysis in community research: Epistemology and practice. Am. J. Community Psychol. 1993, 21, 247–277. [Google Scholar] [CrossRef]
- Drukker, M.; Kaplan, C.; van Os, J. Residential instability in socioeconomically deprived neighbourhoods, good or bad? Health Place 2005, 11, 121–129. [Google Scholar] [CrossRef]
- Aungkulanon, S.; Tangcharoensathien, V.; Shibuya, K.; Bundhamcharoen, K.; Chongsuvivatwong, V. Area-level socioeconomic deprivation and mortality differentials in Thailand: Results from principal component analysis and cluster analysis. Int. J. Equity Health 2017, 16, 1–12. [Google Scholar] [CrossRef]
- Debenham, J.; Clarke, G.; Stillwell, J. Extending geodemographic classification: A new regional prototype. Environ. Plan. A 2003, 35, 1025–1050. [Google Scholar] [CrossRef]
- Nnoaham, K.E.; Frater, A.; Roderick, P.; Moon, G.; Halloran, S. Do geodemographic typologies explain variations in uptake in colorectal cancer screening? An assessment using routine screening data in the south of England. J. Public Health 2010, 32, 572–581. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Vickers, D.; Rees, P. Creating the UK National Statistics 2001 output area classification. J. R. Stat. Soc. Ser. A Stat. Soc. 2007, 170, 379–403. [Google Scholar] [CrossRef]
- Gale, C.G.; Singleton, A.D.; Bates, A.G.; Longley, P.A. Creating the 2011 area classification for output areas (2011 OAC). J. Spat. Inf. Sci. 2016, 12, 1–27. [Google Scholar] [CrossRef]
- Openshaw, S.; Blake, M. Geodemographic segmentation systems for screening health data. J. Epidemiol. Community Health 1995, 49 (Suppl. 2), S34–S38. [Google Scholar] [CrossRef]
- Shelton, N.J.; Birkin, M.H.; Dorling, D. Where not to live: A geo-demographic classification of mortality for England and Wales, 1981–2000. Health Place 2006, 12, 557–569. [Google Scholar] [CrossRef] [PubMed]
- Lawlor, D.; Harvey, D.; Dews, H. Investigation of the association between excess winter mortality and socio-economic deprivation. J. Public Health 2000, 22, 176–181. [Google Scholar] [CrossRef]
- Odoi, A.; Wray, R.; Emo, M.; Birch, S.; Hutchison, B.; Eyles, J.; Abernathy, T. Inequalities in neighbourhood socioeconomic characteristics: potential evidence-base for neighbourhood health planning. Int. J. Health Geogr. 2005, 15, 1–15. [Google Scholar]
- Sheringham, J.; Sowden, S.; Stafford, M.; Simms, I.; Raine, R. Monitoring inequalities in the National Chlamydia Screening Programme in England: Added value of ACORN, a commercial geodemographic classification tool. Sex. Health 2009, 6, 57–62. [Google Scholar] [CrossRef]
- Petersen, J.; Gibin, M.; Longley, P.; Mateos, P.; Atkinson, P.; Ashby, D. Geodemographics as a tool for targeting neighbourhoods in public health campaigns. J. Geogr. Syst. 2011, 13, 173–192. [Google Scholar] [CrossRef]
- Muggli, E.E.; McCloskey, D.; Halliday, J.L. Health behaviour modelling for prenatal diagnosis in Australia: A geodemographic framework for health service utilisation and policy development. BMC Health Serv. Res. 2006, 6, 109. [Google Scholar] [CrossRef][Green Version]
- Besag, J.; York, J.; Mollie, A. Bayesian image restoration, with two applications in spatial statistics. Ann. Inst. Stat. Math. 1991, 43, 1–20. [Google Scholar] [CrossRef]
- Gareth, J.; Witten, D.; Hastie, T.; Tibshiranin, R. An Introduction to Statistical Learning: With Applications in R; Springer: Berlin, Germany, 2013; ISBN 9781461471370. [Google Scholar]
- Everitt, B.S.; Landau, S.; Leese, M.; Stahl, D. Cluster Analysis; Wiley Series in Probability and Statistics; John Wiley & Sons, Ltd.: Chichester, UK, 2011; ISBN 9780470977811. [Google Scholar]
- R Core Team. R: A Language and Environment for Statistical Computing; R Foundation for Statistical Computing: Vienna, Austria, 2016. [Google Scholar]
- Lunn, D.; Spiegelhalter, D.; Thomas, A.; Best, N. The BUGS project: Evolution, critique and future directions. Stat. Med. 2009, 28, 3049–3067. [Google Scholar] [CrossRef] [PubMed]
- Lee, D. CARBayes: An R Package for Bayesian Spatial Modeling with Conditional Autoregressive Priors. J. Stat. Softw. 2013, 55, 1–24. [Google Scholar] [CrossRef]
- Ingram, D.; Franco, S. 2013 NCHS Urban—Rural Classification Scheme for Counties. Natl. Cent. Health Stat. Vital Health Stat. 2014, 2, 1–73. [Google Scholar]
- Fukuda, Y.; Nakamura, K.; Takano, T. Higher mortality in areas of lower socioeconomic position measured by a single index of deprivation in Japan. Public Health 2007, 121, 163–173. [Google Scholar] [CrossRef] [PubMed]
- Deloitte. Cyprus Real Estate Market Outlook Real Estate Advisory Services; Deloitte: Nicosia, Cyprus, 2016. [Google Scholar]
- Riva, M.; Curtis, S.; Gauvin, L.; Fagg, J. Unravelling the extent of inequalities in health across urban and rural areas: Evidence from a national sample in England. Soc. Sci. Med. 2009, 68, 654–663. [Google Scholar] [CrossRef] [PubMed]
- Eberhardt, M.S.; Pamuk, E.R. The importance of place of residence: Examining health in rural and nonrural areas. Am. J. Public Health 2004, 94, 1682–1686. [Google Scholar] [CrossRef] [PubMed]
- Gartner, A.; Farewell, D.; Dunstan, F.; Gordon, E. Differences in mortality between rural and urban areas in England and Wales, 2002–04. Health Stat. Q. 2008, 39, 6–13. [Google Scholar]
- Hart, L.G.; Larson, E.H.; Lishner, D.M. Rural definitions for health policy and research. Am. J. Public Health 2005, 95, 1149–1155. [Google Scholar] [CrossRef] [PubMed]
- Lim, A.; Asher, M.I.; Ellwood, E.; Ellwood, P.; Exeter, D.J. How are “urban” and “rural” defined in publications regarding asthma and related diseases? Allergol. Immunopathol. 2014, 42, 157–161. [Google Scholar] [CrossRef]
- Ghosn, W.; Kassié, D.; Jougla, E.; Salem, G.; Rey, G.; Rican, S. Trends in geographic mortality inequalities and their association with population changes in France, 1975–2006. Eur. J. Public Health 2013, 23, 834–840. [Google Scholar] [CrossRef] [PubMed]
- Riva, M.; Curtis, S.; Norman, P. Residential mobility within England and urban–rural inequalities in mortality. Soc. Sci. Med. 2011, 73, 1698–1706. [Google Scholar] [CrossRef] [PubMed]
- Theodorou, M.; Charalambous, C.; Petrou, C.; Cylus, J. Health Systems in Transition; European Observatory on Health Systems and Policies: Brussels, Belgium, 2012; Volume 14. [Google Scholar]
- Petrou, P.; Vandoros, S. Healthcare reforms in Cyprus 2013–2017: Does the crisis mark the end of the healthcare sector as we know it? Health Policy 2017, 122, 75–80. [Google Scholar] [CrossRef] [PubMed]
- Syed, S.T.; Gerber, B.S.; Sharp, L.K. Traveling towards disease: Transportation barriers to health care access. J. Community Health 2013, 38, 976–993. [Google Scholar] [CrossRef] [PubMed]
- Tyrovolas, S.; Tountas, Y.; Polychronopoulos, E.; Panagiotakos, D. A classification and regression tree analysis for the evaluation of the role of nutritional services on cardiovascular disease risk status of older people living in Greek islands and Cyprus. Int. J. Food Sci. Nutr. 2012, 63, 522–529. [Google Scholar] [CrossRef]
- Befort, C.A.; Niaman, N.; Perri, M.G. Prevalence of obesity among adults from rural and urban areas of the United States: Findings from NHANES (2005–2008). J. Rural Health 2012, 28, 392–397. [Google Scholar] [CrossRef]
- Robertson, M.C.; Song, J.; Taylor, W.C.; Durand, C.P.; Basen-Engquist, K.M. Urban-Rural Differences in Aerobic Physical Activity, Muscle Strengthening Exercise, and Screen-Time Sedentary Behavior. J. Rural Health 2018, 34, 401–410. [Google Scholar] [CrossRef]
- Heraclιdes, A.; Kolokotroni, O.; Charalambous, A. Socio-demographic determinants of obesity in a cross-sectional study of adults in Cyprus. Eur. J. Public Health 2015, 25. [Google Scholar] [CrossRef]
- Middleton, N.; Ellina, P.; Zannoupas, G.; Lamnisos, D.; Kouta, C. Socio-economic inequality in health: individual-and area-level measures of socio-economic position. In Socio-Economic Environment and Human Psychology: Social, Ecological, and Cultural Perspectives; Üskül, A., Oishi, S., Eds.; Oxford University Press: Oxford, UK, 2018. [Google Scholar]
- Singleton, A.; Pavlis, M.; Longley, P.A. The stability of geodemographic cluster assignments over an intercensal period. J. Geogr. Syst. 2016, 18, 97–123. [Google Scholar] [CrossRef]
- Openshaw, S. The Modifiable Areal Unit Problem, Concepts and Techniques in Modern Geography Series; Geo Books: Norwich, UK, 1983. [Google Scholar]
- Mitchell, R.; Dorling, D.; Shaw, M.; Joseph Rowntree Foundation. Inequalities in Life and Death: What if Britain Were More Equal? Policy Press: Bristol, UK, 2000; ISBN 1861342349. [Google Scholar]
| Indicator | Definition |
|---|---|
| Demographic | |
| Age 0–14 | Population aged 0–14 years, as a proportion of the total population |
| Age over 65 | Population aged over 65, as a proportion of the total population |
| Non-Cypriot population | Population identifying as non-Cypriot, as a proportion of the total population |
| Retired population | Retired population, as a proportion of the total population |
| Household Composition | |
| Married population | Married persons, as a proportion of the total population |
| Divorced population | Divorced persons, as a proportion of the total population |
| Single-person households | Households with a single person, as a proportion of total households in conventional dwelling |
| Single-parent households | Households with a single parent, as a proportion of total households in conventional dwelling |
| Six and over members | Households with six and over members, as a proportion of total households |
| Housing features | |
| Multi dwelling house | Multi dwelling houses, as a proportion of total conventional dwellings |
| Secondary/Seasonal | Secondary/seasonal living quarters, as a proportion of total living quarters |
| Vacant/For demolition | Vacant/for demolition living quarters, as a proportion of total living quarters |
| Construction after 2000 | Conventional dwellings constructed after 2000, as a proportion of total conventional dwellings |
| Socio-Economic Status | |
| Not owner-occupied | Not owner-occupied households, as a proportion of households in conventional dwelling |
| Privately renting | Rented households, as a proportion of households in conventional dwelling |
| Educational attainment | Persons with at most lower secondary education, as a proportion of total population over 15 years of age |
| No PC in household | Households without access to a personal computer, as a proportion of total households |
| Occupational Structure | |
| Unemployment | Unemployed economically active persons, as a proportion of total economically active population |
| Agricultural workers | Persons in employment working in agriculture, as a proportion of total employed population |
| Elementary occupations | Persons in employment working in elementary occupations, as a proportion of total employed population |
| Cluster | Median, Mean of RR (95% Credible Interval) |
|---|---|
| Metropolitan and suburban areas | Ref |
| Regenerated west coast communities | 1.17, 1.16 (0.97, 1.39) |
| Young semi-rural communities | 1.36, 1.37 (1.13, 1.62) |
| Traditional-life rural communities | 1.44, 1.44 (1.06, 1.91) |
| Cluster | Median, Mean of RR (95% Credible Interval) |
|---|---|
| Metropolitan and suburban areas | Ref |
| Regenerated west coast communities | 0.93, 0.94 (0.84, 1.03) |
| Young semi-rural communities | 0.96, 0.95 (0.87, 1.05) |
| Traditional-life rural communities | 0.88, 0.89 (0.77, 0.99) |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lamnisos, D.; Middleton, N.; Kyprianou, N.; Talias, M.A. Geodemographic Area Classification and Association with Mortality: An Ecological Study of Small Areas of Cyprus. Int. J. Environ. Res. Public Health 2019, 16, 2927. https://doi.org/10.3390/ijerph16162927
Lamnisos D, Middleton N, Kyprianou N, Talias MA. Geodemographic Area Classification and Association with Mortality: An Ecological Study of Small Areas of Cyprus. International Journal of Environmental Research and Public Health. 2019; 16(16):2927. https://doi.org/10.3390/ijerph16162927
Chicago/Turabian StyleLamnisos, Demetris, Nicos Middleton, Nikoletta Kyprianou, and Michael A. Talias. 2019. "Geodemographic Area Classification and Association with Mortality: An Ecological Study of Small Areas of Cyprus" International Journal of Environmental Research and Public Health 16, no. 16: 2927. https://doi.org/10.3390/ijerph16162927
APA StyleLamnisos, D., Middleton, N., Kyprianou, N., & Talias, M. A. (2019). Geodemographic Area Classification and Association with Mortality: An Ecological Study of Small Areas of Cyprus. International Journal of Environmental Research and Public Health, 16(16), 2927. https://doi.org/10.3390/ijerph16162927







