Underlying Differences in Health Spending Within the World Health Organisation Europe Region—Comparing EU15, EU Post-2004, CIS, EU Candidate, and CARINFONET Countries
Abstract
1. Introduction
2. Materials and Methods
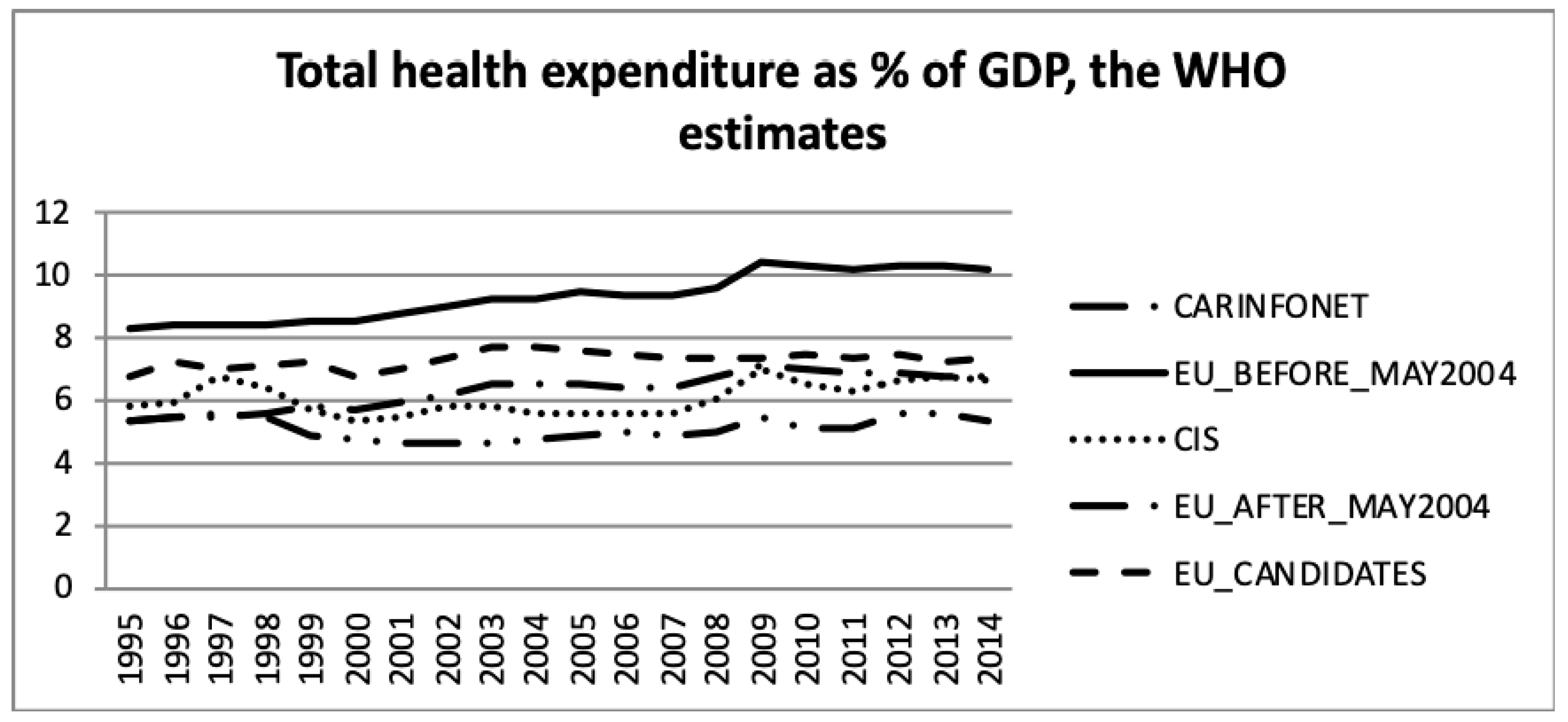
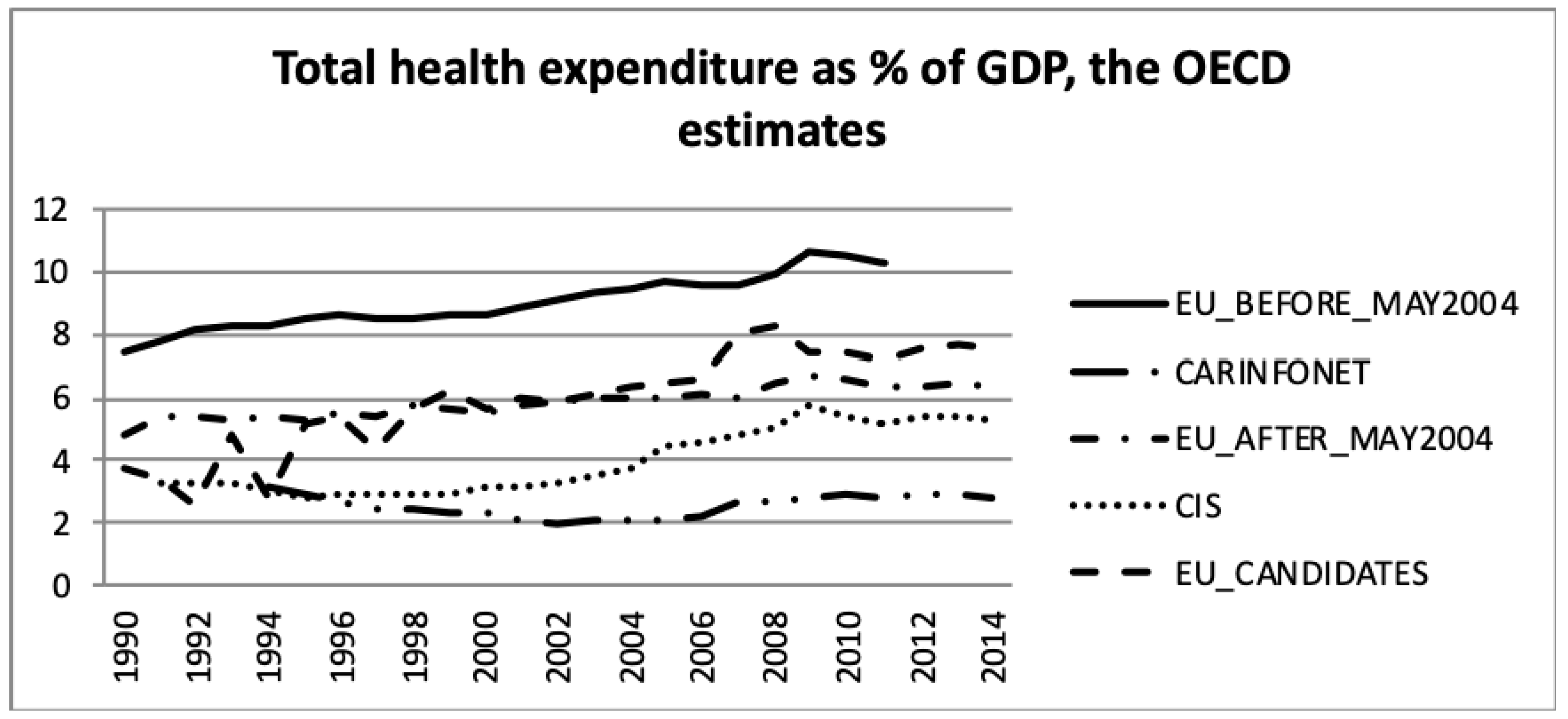
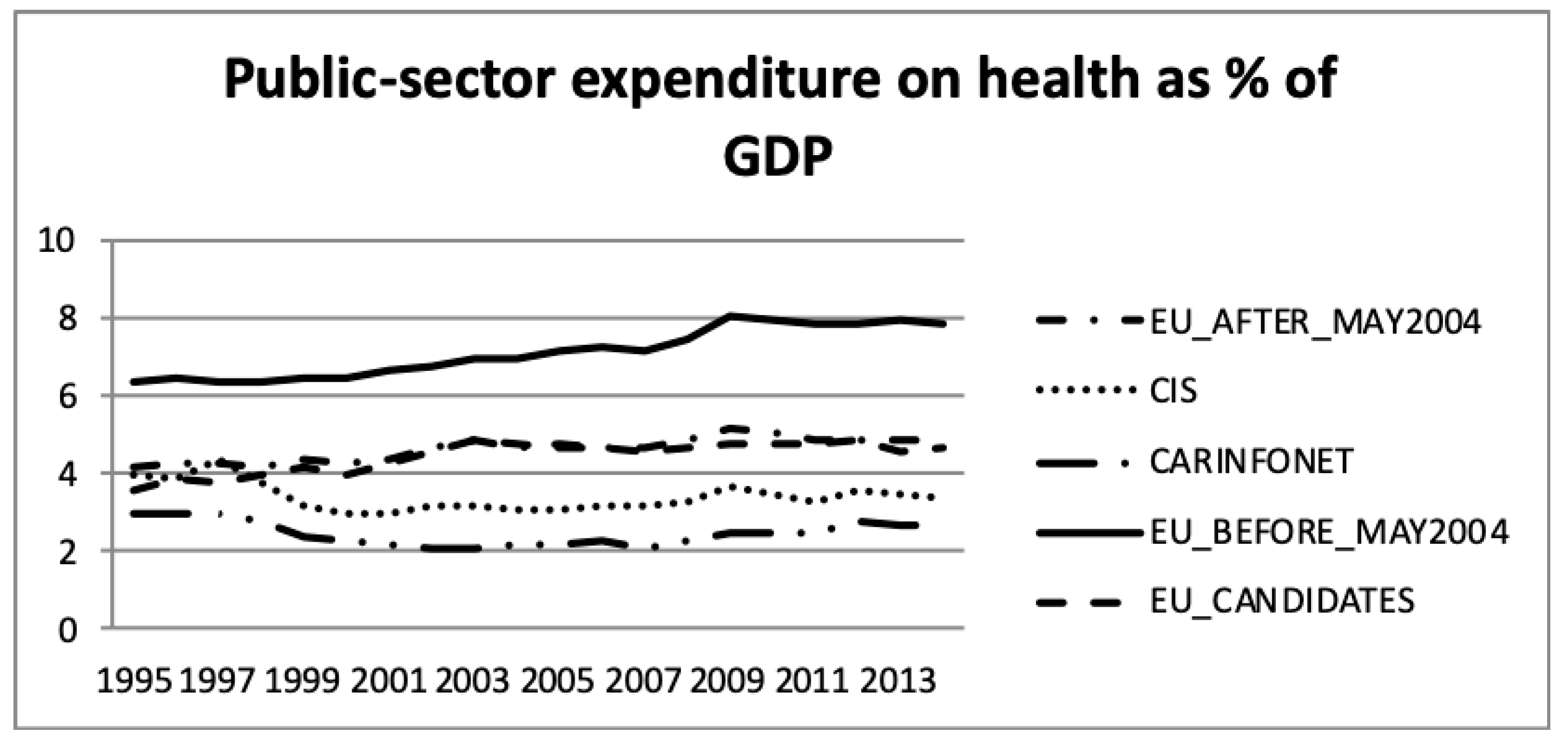
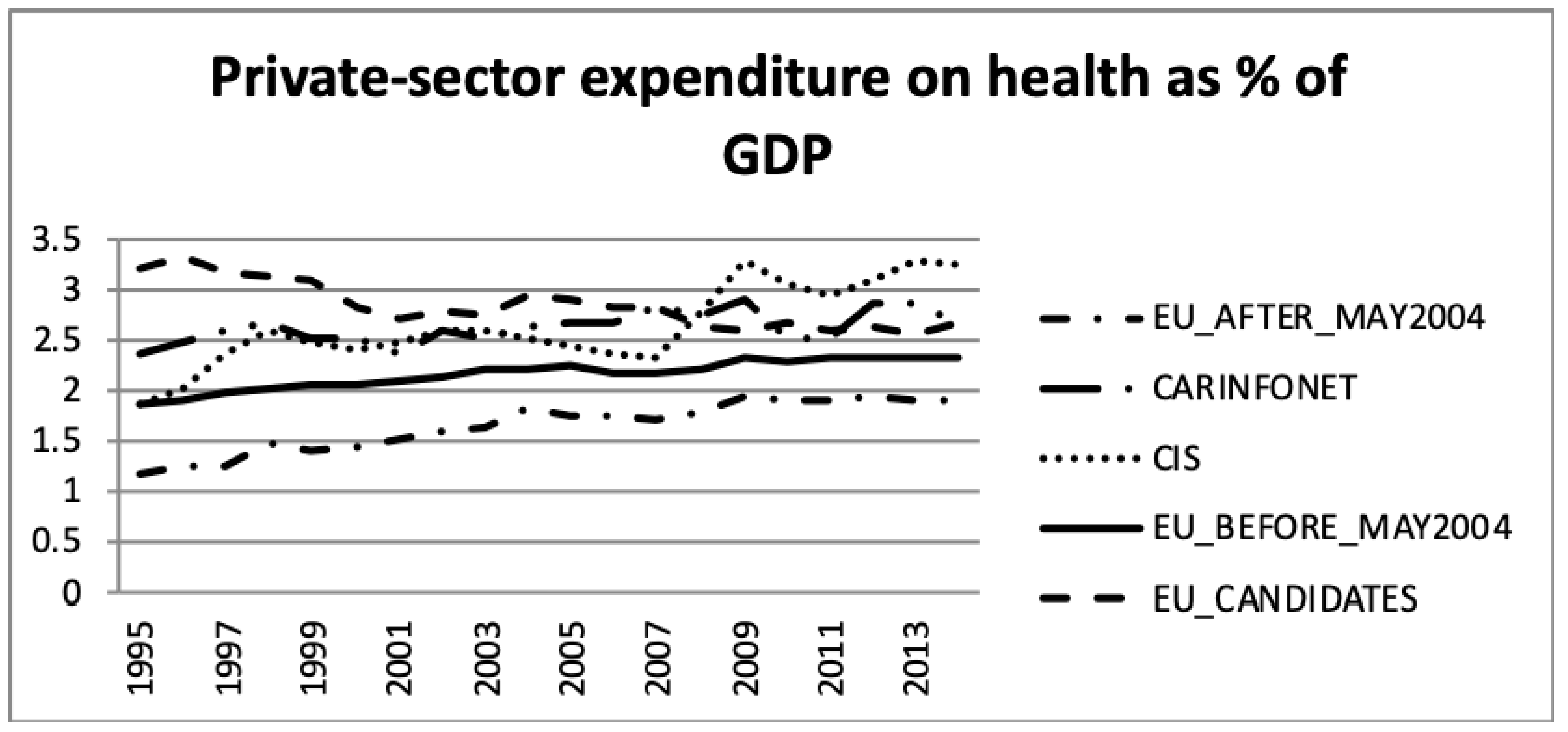
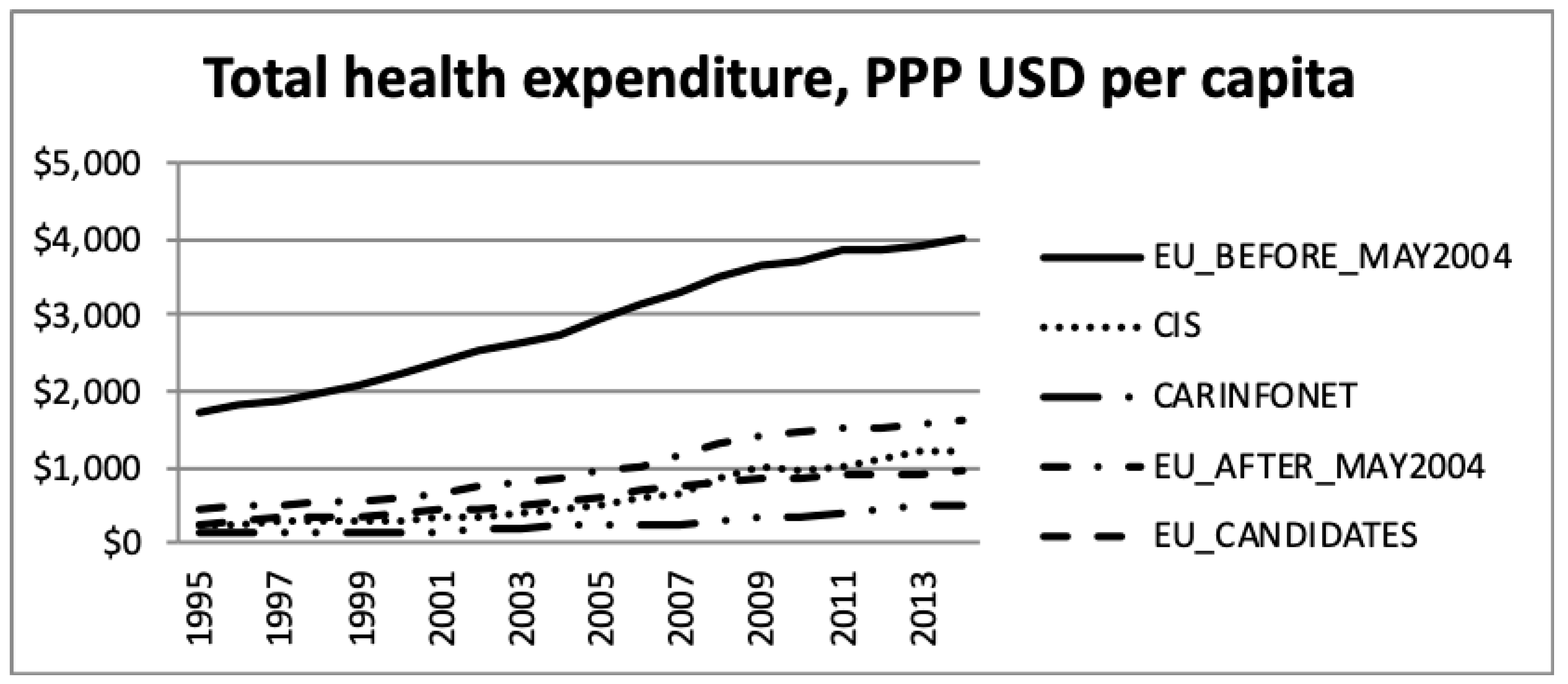
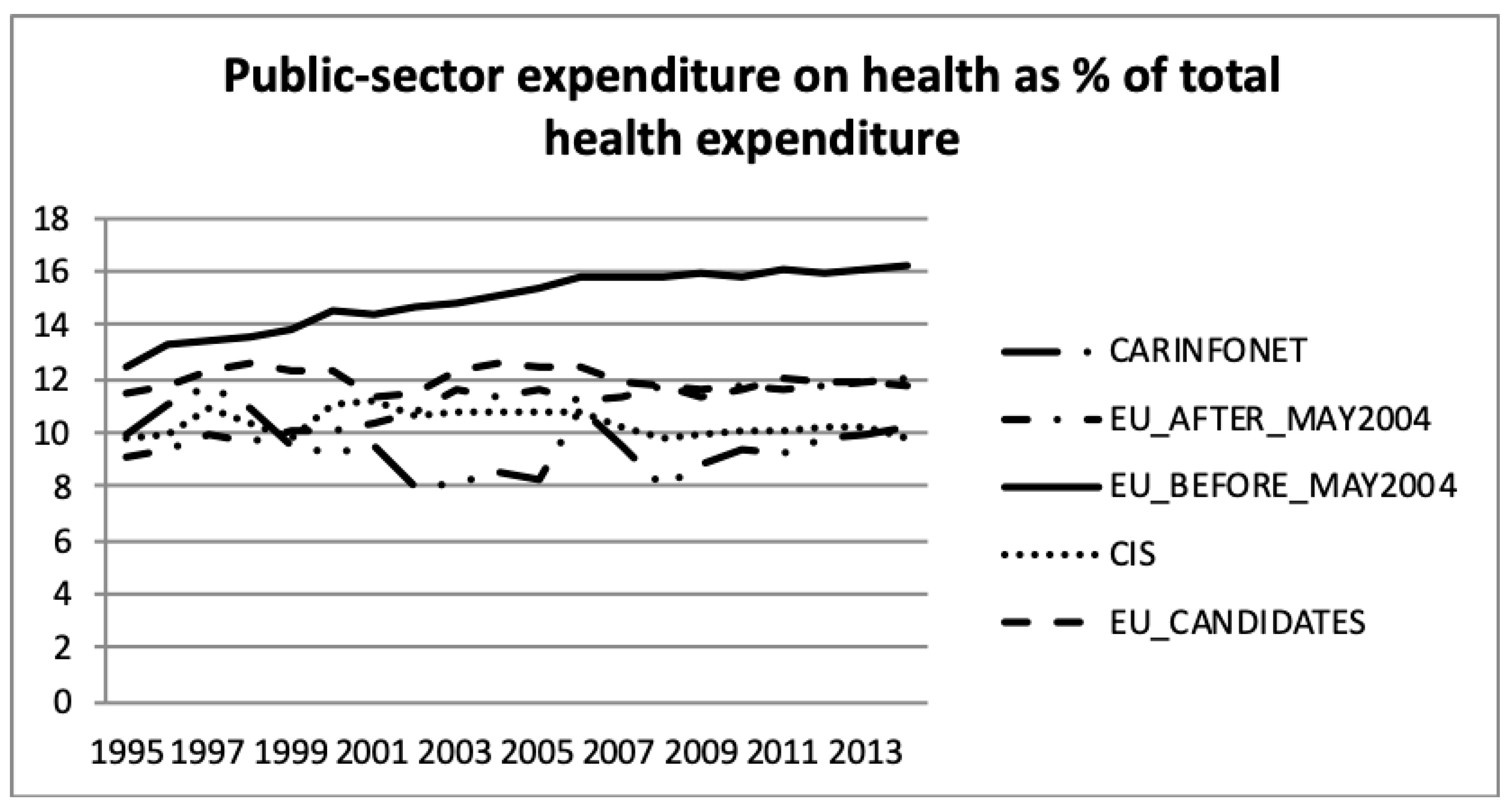
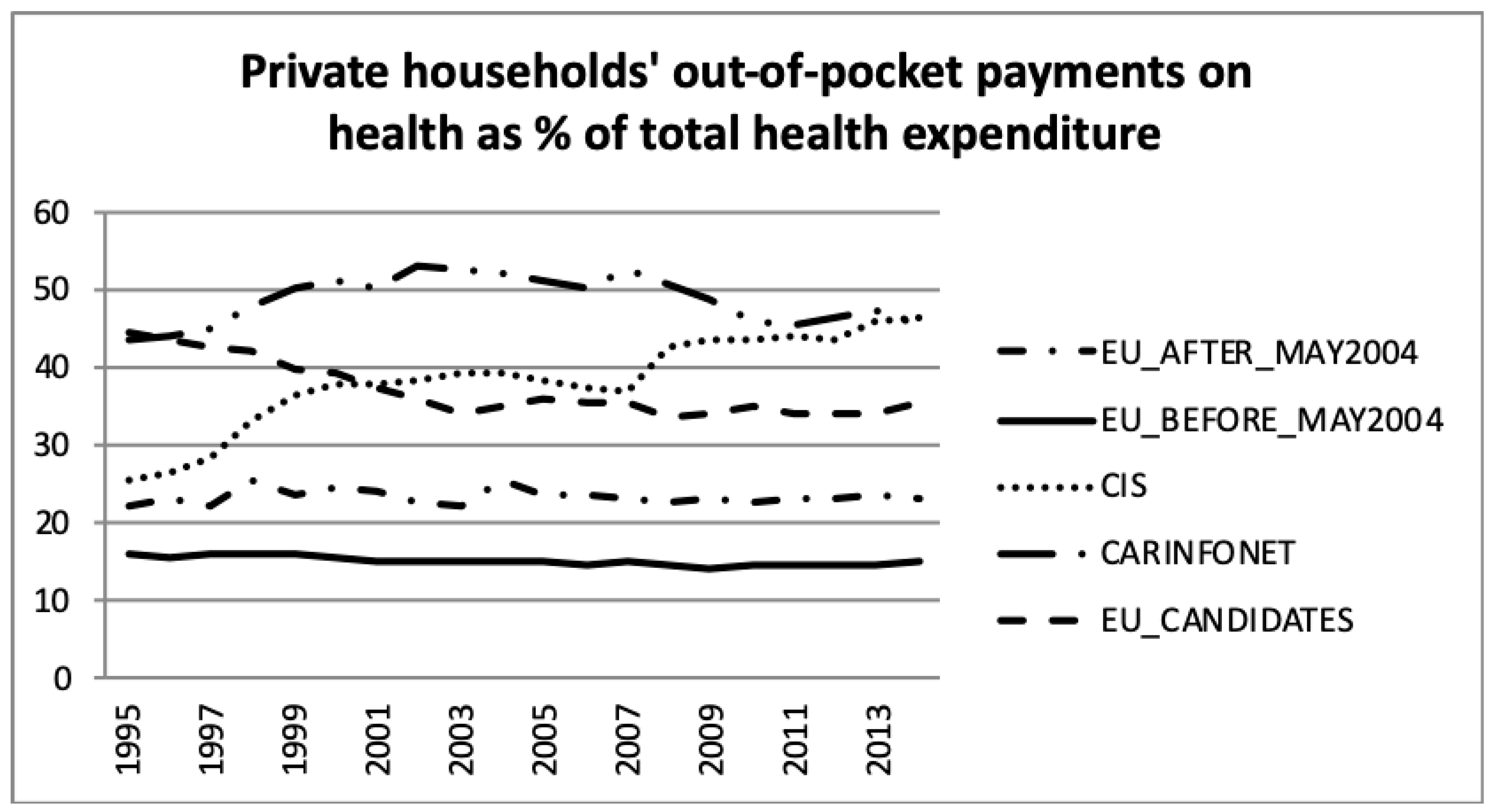
3. Results
4. Study Limitations
5. Discussion
6. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Kuznets, S.; Friedman, M. Incomes from Independent Professional Practice, 1929–1936. In Incomes from Independent Professional Practice; NBER: Berkshire, UK, 1939. [Google Scholar]
- Mushkin, S.J. Toward a definition of health economics. Public Health Rep. 1958, 73, 785–794. [Google Scholar] [CrossRef] [PubMed]
- Jakovljevic, M.B.; Ogura, S. Health economics at the crossroads of centuries—From the past to the future. Front. Public Health 2016, 4, 115. [Google Scholar] [CrossRef] [PubMed]
- Getzen, T.E. Medical care price indexes: Theory, construction & empirical analysis of the US series 1927–1990. Adv. Health Econ. Health Serv. Res. 1992, 13, 83–128. [Google Scholar] [PubMed]
- Smith, S.; Newhouse, J.P.; Freeland, M.S. Income, insurance, and technology: Why does health spending outpace economic growth? Health Aff. 2009, 28, 1276–1284. [Google Scholar] [CrossRef] [PubMed]
- Bärnighausen, T.; Sauerborn, R. One hundred and eighteen years of the German health insurance system: Are there any lessons for middle-and low-income countries? Soc. Sci. Med. 2002, 54, 1559–1587. [Google Scholar] [CrossRef]
- Grimes, S.S. The British National Health Service: State Intervention in the Medical Marketplace, 1911–1948; Routledge: London, UK, 2016. [Google Scholar]
- Kutzin, J.; Ibraimova, A.; Jakab, M.; O’Dougherty, S. Bismarck meets Beveridge on the Silk Road: Coordinating funding sources to create a universal health financing system in Kyrgyzstan. Bull. World Health Organ. 2009, 87, 549–554. [Google Scholar] [CrossRef]
- Jakovljevic, M.; Potapchik, E.; Popovich, L.; Barik, D.; Getzen, T.E. Evolving health expenditure landscape of the BRICS nations and projections to 2025. Health Econ. 2017, 26, 844–852. [Google Scholar] [CrossRef]
- Arsentyev, E.V.; Reshetnikov, V.A. To the biography of N.A. Semashko: The activities of the first Commissar of Health in 1920–1925. Soc. Hist. Med. 2018, 3, 183–192. [Google Scholar]
- Cutler, D.M.; McClellan, M. Is technological change in medicine worth it? Health Aff. 2001, 20, 11–29. [Google Scholar] [CrossRef]
- Ogura, S.; Jakovljevic, M.B. Health financing constrained by population aging—An opportunity to learn from Japanese experience. Serb. J. Exp. Clin. Res. 2014, 15, 175–181. [Google Scholar] [CrossRef]
- Jakovljevic, M.B.; Milovanovic, O. Growing burden of non-communicable diseases in the emerging health markets: The case of BRICS. Front. Public Health 2015, 3, 65. [Google Scholar] [CrossRef]
- Parente, S.T.; Feldman, R.; Christianson, J.B. Evaluation of the effect of a consumer-driven health plan on medical care expenditures and utilization. Health Serv. Res. 2004, 39, 1189–1210. [Google Scholar] [CrossRef] [PubMed]
- Footman, K.; Roberts, B.; Mills, A.; Richardson, E.; McKee, M. Public satisfaction as a measure of health system performance: A study of nine countries in the former Soviet Union. Health Policy 2013, 112, 62–69. [Google Scholar] [CrossRef] [PubMed]
- Bonilla-Chacin, M.E.; Murrugarra, E.; Temourov, M. Health care during transition and health systems reform: Evidence from the poorest CIS countries. Soc. Policy Adm. 2005, 39, 381–408. [Google Scholar] [CrossRef]
- Groenewegen, P.P.; Dourgnon, P.; Greß, S.; Jurgutis, A.; Willems, S. Strengthening weak primary care systems: Steps towards stronger primary care in selected Western and Eastern European countries. Health Policy 2013, 113, 170–179. [Google Scholar] [CrossRef] [PubMed]
- Mechanick, A. Пирамида Семашко [The Pyramid of Semashko]. Expert 2011, 30/31, 68–72. (In Russian) [Google Scholar]
- Ulumbekova, G.E. Здравоохранение России. Что надо делать: научное обоснование «Стратегии развития здравоохранения РФ до 2020 года» [Healthcare of Russia. What to do: The Scientific Rationale of the “Strategy for the development of healthcare in the Russian Federation until 2020”]. Mosc. Geotar-Media 2010, 1–96. (In Russian) [Google Scholar]
- Manerova, O.A.; Drygin, D.M.; Davydov, P.K. Актуальные Вопросы Подготовки Медицинских Кадров: к 140-Летию со Дня Рождения Н.А. Семашко [Topical Issues Concerning Medical Training: Devoted the 140th Anniversary of the Birth N.A. Semashko]. Available online: https://historymedjournal.com/volume/number_3/3-2014__Manerova_Dpigin_Davidov_aktual%20voprosi.pdf (accessed on 20 July 2014).
- Fleck, F. Rocky road from the Semashko to a new health model. World Health Organization. Bull. World Health Organ. 2013, 91, 320–321. [Google Scholar]
- Borisova, L.V. Health care systems as determinants of health outcomes in transition countries: Developing classification. Soc. Theory Health 2011, 9, 326–354. [Google Scholar] [CrossRef]
- Habibov, N.N.; Afandi, E.N. Self-rated health and social capital in transitional countries: Multilevel analysis of comparative surveys in Armenia, Azerbaijan, and Georgia. Soc. Sci. Med. 2011, 72, 1193–1204. [Google Scholar] [CrossRef] [PubMed]
- Borowitz, M.; Atun, R. The unfinished journey from Semashko to Bismarck: Health reform in Central Asia from 1991 to 2006. Central Asian Surv. 2006, 25, 419–440. [Google Scholar] [CrossRef]
- Jakovljevic, M.B.; Arsenijevic, J.; Pavlova, M.; Verhaeghe, N.; Laaser, U.; Groot, W. Within the triangle of healthcare legacies: Comparing the performance of South-Eastern European health systems. J. Med. Econ. 2017, 20, 483–492. [Google Scholar] [CrossRef] [PubMed]
- Rapkin, D.P.; Thompson, W.R.; Christopherson, J.A. Bipolarity and bipolarization in the Cold War era: Conceptualization, measurement, and validation. J. Confl. Resolut. 1979, 23, 261–295. [Google Scholar] [CrossRef]
- Farazmand, A. Public organizations in the age of accelerated globalization. Public Organ. Rev. 2001, 1, 5–11. [Google Scholar] [CrossRef]
- Cueto, M. The origins of primary health care and selective primary health care. Am. J. Public Health 2004, 94, 1864–1874. [Google Scholar] [CrossRef] [PubMed]
- Rowland, D.; Telyukov, A.V. Soviet health care from two perspectives. Health Aff. 1991, 10, 71–86. [Google Scholar] [CrossRef]
- Rhodes, M.; Van Apeldoorn, B. Capitalism versus capitalism in Western Europe. In Developments in West European Politics; Palgrave: London, UK, 1997; pp. 171–189. [Google Scholar]
- WHO Global Health Expenditure Database. Available online: http://apps.who.int/nha/database (accessed on 5 August 2019).
- OECD Reviews of Health Systems: A Series of Country Reports. Available online: https://www.oecd.org/els/health-systems/reviews-health-systems.htm (accessed on 5 August 2019).
- OECD. Improving Estimates of Spending on Administration. Available online: https://www.oecd.org/els/health-systems/Improving-Estimates-of-Spending-on-Administration.pdf (accessed on 5 August 2019).
- OECD. Classification of Health Care Financing Schemes (ICHA-HF). Available online: https://www.oecd-ilibrary.org/docserver/9789264270985-9-en.pdf?expires=1555511574&id=id&accname=guest&checksum=6D1A3B7F7058293A58BD2831DA3845B2 (accessed on 5 August 2019).
- OECD Health Statistics 2018. Available online: http://www.oecd.org/els/health-systems/health-data.htm (accessed on 5 August 2019).
- WHO. European Health for All Database (HFA-DB) Data Source. Available online: http://www.euro.who.int/en/data-and-evidence/databases/european-health-for-all-family-of-databases-hfa-db (accessed on 5 August 2019).
- WHO. European Health for All Database (HFA-DB). Available online: https://gateway.euro.who.int/en/datasets/european-health-for-all-database/ (accessed on 5 August 2019).
- Pedroni, P. Purchasing power parity tests in cointegrated panels. Rev. Econ. Stat. 2001, 83, 727–731. [Google Scholar] [CrossRef]
- Poullier, J.P.; Hernandez, P.; Kawabata, K.; Savedoff, D.W. National Health Accounts: Concepts, Data Sources and Methodology. Available online: https://books.google.rs/books?hl=en&lr=&id=Ut_xcxWHobYC&oi=fnd&pg=PA182&dq=41.39.%09Poullier,+J.P.%3B+Hernandez,+P.%3B+Kawabata,+K.%3B+Savedoff,+D.W.+National+health+accounts:+Concepts,+data+sources+and+methodology.+World+Health+Organ&ots=ji1I980VTv&sig=g_37Y2ci0WEdklTrfR4nK0sSAKk&redir_esc=y#v=onepage&q&f=false (accessed on 5 August 2019).
- Berman, P.A. National health accounts in developing countries: Appropriate methods and recent applications. Health Econ. 1997, 6, 11–30. [Google Scholar] [CrossRef]
- Bui, A.L.; Lavado, R.F.; Johnson, E.K.; Brooks, B.P.; Freeman, M.K.; Graves, C.M.; Haakenstad, A.; Shoemaker, B.; Hanlon, M.; Dieleman, J.L.; et al. National health accounts data from 1996 to 2010: A systematic review. Bull. World Health Organ. 2015, 93, 566–576. [Google Scholar] [CrossRef]
- WHO. WHO Methods and Data Sources for Global Burden of Disease Estimates 2000–2011; Department of Health Statistics and Information Systems: Geneva, Switzerland, 2013. [Google Scholar]
- Cowen, D.; Smith, N. After geopolitics? From the geopolitical social to geoeconomics. Antipode 2009, 41, 22–48. [Google Scholar] [CrossRef]
- Sparke, M. From geopolitics to geoeconomics: Transnational state effects in the borderlands. Geopolitics 1998, 3, 62–98. [Google Scholar] [CrossRef]
- Wigell, M.; Vihma, A. Geopolitics versus geoeconomics: The case of Russia’s geostrategy and its effects on the EU. Int. Aff. 2016, 92, 605–627. [Google Scholar] [CrossRef]
- Saltman, R.B.; Figueras, J.; Sakellarides, C. Critical Challenges for Health Care Reform in Europe; McGraw-Hill Education: Berkshire, UK, 1998. [Google Scholar]
- Krajewski-Siuda, K.; Romaniuk, P. Poland—An “experimental range” for health care system changes. Two reforms: Decentralization and centralization and their consequences. J. Public Health 2008, 16, 61–70. [Google Scholar] [CrossRef]
- Széles, G.; Vokó, Z.; Jenei, T.; Kardos, L.; Pocsai, Z.; Bajtay, A.; Papp, E.; Pásti, G.; Kósa, Z.; Molnár, I.; et al. A preliminary evaluation of a health monitoring programme in Hungary. Eur. J. Public Health 2005, 15, 26–32. [Google Scholar] [CrossRef]
- Bryndová, L.; Pavloková, K.; Roubal, T.; Rokosová, M.; Gaskins, M.; van Ginneken, E. Czech Republic. Health system review. Health Syst. Transit. (Eur. Obs. Health Syst. Policies) 2009, 11. [Google Scholar]
- Jakovljevic, M.B. Resource allocation strategies in Southeastern European Health Policy. Res. Alloc. Strategy. Southeast. Eur. Health Policy 2013, 14, 153–159. [Google Scholar] [CrossRef]
- Jakovljevic, M.; Vukovic, M.; Chen, C.C.; Antunovic, M.; Dragojevic-Simic, V.; Velickovic-Radovanovic, R.; Djendji, M.S.; Jankovic, N.; Rankovic, A.; Kovacevic, A.; et al. Do health reforms impact cost consciousness of Health care professionals? Results from a nation-wide survey in the Balkans. Balkan Med. J. 2016, 3, 8–17. [Google Scholar] [CrossRef]
- Baris, E.; Mollahaliloglu, S.; Aydin, S. Healthcare in Turkey: From laggard to leader. BMJ 2011, 342, c7456. [Google Scholar] [CrossRef] [PubMed]
- Akaeev, A.A.; Anufriev, I.E.; Popov, G.N. Технологическая модернизация- промышленности и инновационное развитие – ключ к экономическому возрождению России в XXI веке [Technological modernization of industry and innovative development is the key to the economic revival of Russia in the XXI century]. Инновации [Innovations] 2010, 15–28. (In Russian) [Google Scholar]
- Yegorychev, A.M.; Dubinin, S.N. Россия на пороге XXI века: инновационные тенденции и национальные приоритеты [Russia on the edge of the XXI century: Innovation trends and national priorities]. Ученые Записки Российского Государственного Социального Университета [Sci. Notes Rus. State Soc. Univ.] 2010, 10–15. (In Russian) [Google Scholar]
- Kotz, D.M. Lessons from economic transition in Russia and China. Political Econ. Contemp. Capital. Radic. Perspect. Econ. Theory Policy 2000, 210–217. [Google Scholar]
- Rancic, N.; Jakovljevic, M.B. Long term health spending alongside population aging in N-11 emerging nations. East Eur. Bus. Econ. J. 2016, 2, 2–26. [Google Scholar]
- Caliskan, Z. The relationship between pharmaceutical expenditure and life expectancy: Evidence from 21 OECD countries. Appl. Econ. Lett. 2009, 16, 1651–1655. [Google Scholar] [CrossRef]
- Mourre, G. What Explains the Differences in Income and Labour Utilisation and Drives Labour and Economic Growth in Europe? A GDP Accounting Perspective (No. 354). Directorate General Economic and Financial Affairs (DG ECFIN); European Commission: Brussels, Belgium, 2009. [Google Scholar]
- Kaitila, V. Convergence of Real GDP Per Capita in the EU15. How do the Accession Countries Fit in? (No. 025). 2004. Available online: https://ideas.repec.org/p/epr/enepwp/025.html (accessed on 21 August 2019).
- Kerem, K.; Puss, T.; Viies, M.; Maldre, R. Health and convergence of health care expenditure in EU. Int. Bus. Econ. Res. J. 2008, 7, 29–44. [Google Scholar] [CrossRef]
- Bech, M.; Christiansen, T.; Khoman, E.; Lauridsen, J.; Weale, M. Ageing and health care expenditure in EU-15. Eur. J. Health Econ. 2011, 12, 469–478. [Google Scholar] [CrossRef] [PubMed]
- Jakovljevic, M. The aging of Europe. The unexplored potential. Farmecon. Health Econ. Ther. Pathw. 2015, 16, 89–92. [Google Scholar] [CrossRef]
- Jakovljevic, M.B.; Netz, Y.; Buttigieg, S.C.; Asany, R.; Laaser, U.; Varjacic, M. Population aging and migration—History and UN forecasts in the EU-28 and its east and south near neighborhood—One century perspective 1950–2050. Glob. Health 2018, 14, 30. [Google Scholar] [CrossRef]
- Korotayev, A.; Arkhangelsky, V.; Bogevolnov, J.; Goldstone, J.; Khaltourina, G.A.; Malkov, A.; Novikov, A.; Riazantsev, S.; Rybalchenko, S.; Rybalchenko, S.; et al. Critical 10 Years. Demographic Policies of the Russian Federation: Successes and Challenges; “Delo” Publishing House (RANEPA): Moscow, Russia, April 2015; ISBN 978-57749-1068-7. [Google Scholar]
- Khasanova, R.R. Самосохранительное поведение населения как фактор продолжительности жизни [Self-preservation behavior of the population as a factor in life expectancy]. Здоровье населения и среда обитания [Public Health Habitat] 2013, 5, 43–46. (In Russian) [Google Scholar]
- Denisenko, M.; Varshavskaya, E. Продолжительность трудовой жизни в России [Working life expectancy in Russia]. HSE Econ. J. 2017, 21, 592–622. (In Russian) [Google Scholar]
- Belov, V.B.; Rogovina, A.G. Основные медико-демографические показатели здоровья населения России к 2013 г [The basic medical demographic indicators of population health of Russia up to 2013]. Проблемы социальной гигиены, здравоохранения и истории медицины [Probl. Soc. Hyg. Public Health Hist. Med.] 2014, 6, 18–22. (In Russian) [Google Scholar]
- Jakovljevic, M.B.; Laaser, U. Population aging from 1950 to 2010 in seventeen transitional countries in the wider region of South Eastern Europe. SEEJPH 2015, 3, 1–12. [Google Scholar]
- Jakovljevic, M.B. Starenje stanovništva i rast izdvajanja za zdravstvenu zaštitu [Aging of the population and growth of appropriations for health care]. Srpski Arhiv za Celokupno Lekarstvo 2017, 145, 534–539. (In Serbian) [Google Scholar] [CrossRef]
- Jakovljevic, M.; Vukovic, M.; Fontanesi, J. Life expectancy and health expenditure evolution in Eastern Europe—DiD and DEA analysis. Expert Rev. Pharm. Outcomes Res. 2016, 16, 537–546. [Google Scholar] [CrossRef]
- Morgan, D.; Astolfi, R. Financial impact of the GFC: Health care spending across the OECD. Health Econ. Policy Law 2015, 10, 7–19. [Google Scholar] [CrossRef] [PubMed]
- Rivlin, A.M.; Antos, J.R. Restoring Fiscal Sanity 2007: The Health Spending Challenge; Brookings Institution Press: Washington, DC, USA, 2007. [Google Scholar]
- Jakovljevic, M.; Souliotis, K. Pharmaceutical expenditure changes in Serbia and Greece during the global economic recession. South East. Eur. J. Public Health 2016, 5, 1–17. [Google Scholar]
- Sotiropoulos, D.A. The EU’s impact on the Greek welfare state: Europeanization on paper? J. Eur. Soc. Policy 2004, 14, 267–284. [Google Scholar] [CrossRef]
- Huidrom, R.; Kose, A.; Ohnsorge, F.L. How Important Are Spillovers from Major Emerging Markets? Policy Research Working Paper, no. WPS 8093; World Bank Group: Washington, DC, USA, 2017. [Google Scholar]
- Kose, A. Big Emerging Market Economies Versus the G7: Which Group Will Drive the Upswing in Global Growth? Available online: https://www.brookings.edu/blog/up-front/2017/07/14/big-emerging-market-economies-versus-the-g-7-which-group-will-drive-the-upswing-in-global-growth/ (accessed on 5 August 2019).


| EU15 | EU Post-2004 | CIS * | CARINFONET ** | EU Candidate Countries |
|---|---|---|---|---|
| Austria AUT | Bulgaria BGR | Armenia ARM | Kazakhstan KAZ | Albania ALB |
| Belgium BEL | Croatia HRV | Azerbaijan AZE | Kyrgyzstan KGZ | Montenegro MNE |
| Denmark DNK | Cyprus CYP | Belarus BLR | Tajikistan TJK | Serbia SRB |
| Finland FIN | Czech Republic CZE | Kazakhstan KAZ | Turkmenistan TKM | The former Yugoslav Republic of Macedonia MKD |
| France FRA | Estonia EST | Kyrgyzstan KGZ | Uzbekistan UZB | Turkey TUR |
| Germany DEU | Hungary HUN | Republic of Moldova MDA | Bosnia and Herzegovina BIH | |
| Greece GRC | Latvia LVA | Russian Federation RUS | ||
| Ireland IRL | Lithuania LTU | Tajikistan TJK | ||
| Italy ITA | Malta MLT | Turkmenistan TKM | ||
| Luxembourg LUX | Poland POL | Ukraine UKR | ||
| Netherlands NLD | Romania ROU | Uzbekistan UZB | ||
| Portugal PRT | Slovakia SVK | |||
| Spain ESP | Slovenia SVN | |||
| Sweden SWE | ||||
| United Kingdom GBR |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jakovljevic, M.; Fernandes, P.O.; Teixeira, J.P.; Rancic, N.; Timofeyev, Y.; Reshetnikov, V. Underlying Differences in Health Spending Within the World Health Organisation Europe Region—Comparing EU15, EU Post-2004, CIS, EU Candidate, and CARINFONET Countries. Int. J. Environ. Res. Public Health 2019, 16, 3043. https://doi.org/10.3390/ijerph16173043
Jakovljevic M, Fernandes PO, Teixeira JP, Rancic N, Timofeyev Y, Reshetnikov V. Underlying Differences in Health Spending Within the World Health Organisation Europe Region—Comparing EU15, EU Post-2004, CIS, EU Candidate, and CARINFONET Countries. International Journal of Environmental Research and Public Health. 2019; 16(17):3043. https://doi.org/10.3390/ijerph16173043
Chicago/Turabian StyleJakovljevic, Mihajlo, Paula Odete Fernandes, João Paulo Teixeira, Nemanja Rancic, Yuriy Timofeyev, and Vladimir Reshetnikov. 2019. "Underlying Differences in Health Spending Within the World Health Organisation Europe Region—Comparing EU15, EU Post-2004, CIS, EU Candidate, and CARINFONET Countries" International Journal of Environmental Research and Public Health 16, no. 17: 3043. https://doi.org/10.3390/ijerph16173043
APA StyleJakovljevic, M., Fernandes, P. O., Teixeira, J. P., Rancic, N., Timofeyev, Y., & Reshetnikov, V. (2019). Underlying Differences in Health Spending Within the World Health Organisation Europe Region—Comparing EU15, EU Post-2004, CIS, EU Candidate, and CARINFONET Countries. International Journal of Environmental Research and Public Health, 16(17), 3043. https://doi.org/10.3390/ijerph16173043








