An Exploratory Study on the Effects of Forest Therapy on Sleep Quality in Patients with Gastrointestinal Tract Cancers
Abstract
1. Introduction
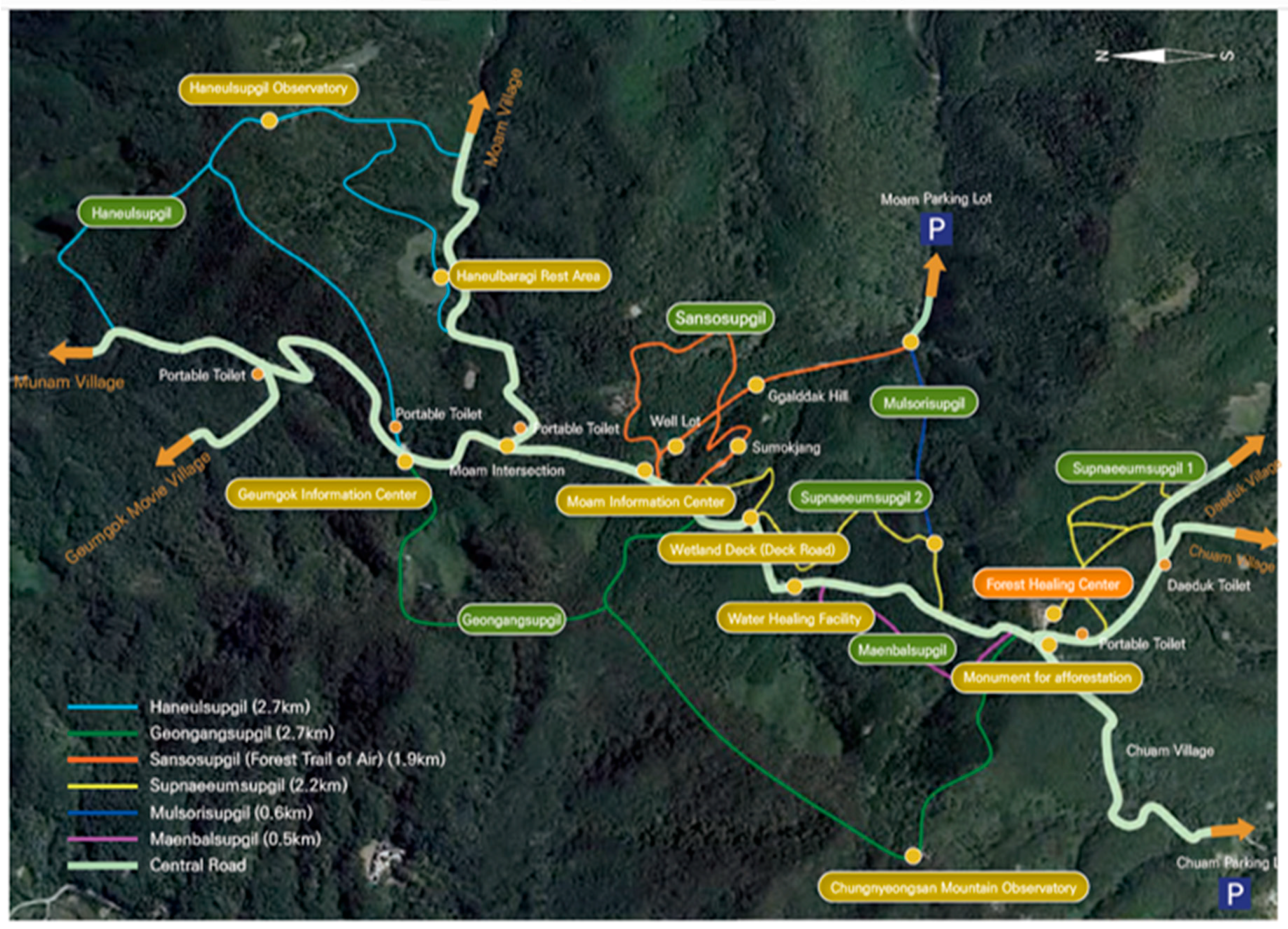
2. Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Hansen, M.M.; Jones, R.; Tocchini, K. Shinrin-Yoku (Forest Bathing) and Nature Therapy: A State-of-the-Art Review. Int. J. Environ. Res. Public. Health 2017, 14, 851. [Google Scholar] [CrossRef]
- Chun, M.H.; Chang, M.C.; Lee, S.J. The effects of forest therapy on depression and anxiety in patients with chronic stroke. Int. J. Neurosci. 2017, 127, 199–203. [Google Scholar] [CrossRef]
- Lee, I.; Choi, H.; Bang, K.S.; Kim, S.; Song, M.; Lee, B. Effects of Forest Therapy on Depressive Symptoms among Adults: A Systematic Review. Int. J. Environ. Res. Public Health 2017, 14, 321. [Google Scholar] [CrossRef]
- Ochiai, H.; Ikei, H.; Song, C.; Kobayashi, M.; Takamatsu, A.; Miura, T.; Kagawa, T.; Li, Q.; Kumeda, S.; Imai, M.; et al. Physiological and psychological effects of forest therapy on middle-aged males with high-normal blood pressure. Int. J. Environ. Res. Public Health 2015, 12, 2532–2542. [Google Scholar] [CrossRef]
- Bowler, D.E.; Buyung-Ali, L.M.; Knight, T.M.; Pullin, A.S. A systematic review of evidence for the added benefits to health of exposure to natural environments. BMC Public Health 2010, 10, 456. [Google Scholar] [CrossRef]
- Antonelli, M.; Barbieri, G.; Donelli, D. Effects of forest bathing (shinrin-yoku) on levels of cortisol as a stress biomarker: A systematic review and meta-analysis. Int. J. Biometeorol. 2019. [Google Scholar] [CrossRef]
- Saito, H.; Horiuchi, M.; Takayama, N.; Fujiwara, A. Effects of managed forest versus unmanaged forest on physiological restoration from a stress stimulus, and the relationship with individual traits. J. For. Res. 2019, 24, 77–85. [Google Scholar] [CrossRef]
- Vander Wal, G.S.; Lichstein, K.L.; Perkins, C.K. Correlation of Disturbed Sleep and Cancer Stress. Behav. Sleep Med. 2017, 15, 39–52. [Google Scholar] [CrossRef]
- Samuelsson, L.B.; Bovbjerg, D.H.; Roecklein, K.A.; Hall, M.H. Sleep and circadian disruption and incident breast cancer risk: An evidence-based and theoretical review. Neurosci. Biobehav. Rev. 2018, 84, 35–48. [Google Scholar] [CrossRef]
- Lin, C.L.; Liu, T.C.; Wang, Y.N.; Chung, C.H.; Chien, W.C. The Association Between Sleep Disorders and the Risk of Colorectal Cancer in Patients: A Population-based Nested Case-Control Study. In Vivo (Athens, Greece) 2019, 33, 573–579. [Google Scholar] [CrossRef]
- Trudel-Fitzgerald, C.; Zhou, E.S.; Poole, E.M.; Zhang, X.; Michels, K.B.; Eliassen, A.H.; Chen, W.Y.; Holmes, M.D.; Tworoger, S.S.; Schernhammer, E.S. Sleep and survival among women with breast cancer: 30 years of follow-up within the Nurses’ Health Study. Br. J. Cancer 2017, 116, 1239–1246. [Google Scholar] [CrossRef]
- Stone, C.R.; Haig, T.R.; Fiest, K.M.; McNeil, J.; Brenner, D.R.; Friedenreich, C.M. The association between sleep duration and cancer-specific mortality: A systematic review and meta-analysis. Cancer Causes Control CCC 2019, 30, 501–525. [Google Scholar] [CrossRef]
- Collins, K.P.; Geller, D.A.; Antoni, M.; Donnell, D.M.; Tsung, A.; Marsh, J.W.; Burke, L.; Penedo, F.; Terhorst, L.; Kamarck, T.W.; et al. Sleep duration is associated with survival in advanced cancer patients. Sleep Med. 2017, 32, 208–212. [Google Scholar] [CrossRef]
- Charalambous, A.; Berger, A.M.; Matthews, E.; Balachandran, D.D.; Papastavrou, E.; Palesh, O. Cancer-related fatigue and sleep deficiency in cancer care continuum: Concepts, assessment, clusters, and management. Support. Care Cancer 2019, 27, 2747–2753. [Google Scholar] [CrossRef]
- Sohn, S.I.; Kim, D.H.; Lee, M.Y.; Cho, Y.W. The reliability and validity of the Korean version of the Pittsburgh Sleep Quality Index. Sleep Breath. Schlaf Atm. 2012, 16, 803–812. [Google Scholar] [CrossRef]
- Cho, Y.W.; Song, M.L.; Morin, C.M. Validation of a Korean Version of the Insomnia Severity Index. J. Clin. Neurol. (Seoul, Korea) 2014, 10, 210–215. [Google Scholar] [CrossRef]
- Hoddes, E.; Dement, W.; Zarcone, V. The development and use of the Stanford Sleepiness Scale (SSS). Psychophysiol., 1972, 9: 150. Johns, M.W. Reliability and Factor Analysis of the Epworth Sleepiness Scale. Sleep 1992, 15, 376–381. [Google Scholar]
- Chung, F.; Abdullah, H.R.; Liao, P. STOP-Bang Questionnaire: A Practical Approach to Screen for Obstructive Sleep Apnea. Chest 2016, 149, 631–638. [Google Scholar] [CrossRef]
- Zigmond, A.S.; Snaith, R.P. The Hospital Anxiety and Depression Scale. Acta Psychiatr. Scand. 1983, 67, 361–370. [Google Scholar] [CrossRef]
- Han, J.W.; Choi, H.; Jeon, Y.H.; Yoon, C.H.; Woo, J.M.; Kim, W. The Effects of Forest Therapy on Coping with Chronic Widespread Pain: Physiological and Psychological Differences between Participants in a Forest Therapy Program and a Control Group. Int. J. Environ. Res. Public Health 2016, 13, 255. [Google Scholar] [CrossRef]
- Yu, C.P.; Lin, C.M.; Tsai, M.J.; Tsai, Y.C.; Chen, C.Y. Effects of Short Forest Bathing Program on Autonomic Nervous System Activity and Mood States in Middle-Aged and Elderly Individuals. Int. J. Environ. Res. Public Health 2017, 14, 897. [Google Scholar] [CrossRef] [PubMed]
- Song, C.; Ikei, H.; Kobayashi, M.; Miura, T.; Taue, M.; Kagawa, T.; Li, Q.; Kumeda, S.; Imai, M.; Miyazaki, Y. Effect of forest walking on autonomic nervous system activity in middle-aged hypertensive individuals: A pilot study. Int. J. Environ. Res. Public Health 2015, 12, 2687–2699. [Google Scholar] [CrossRef] [PubMed]
- Li, Q.; Kobayashi, M.; Wakayama, Y.; Inagaki, H.; Katsumata, M.; Hirata, Y.; Hirata, K.; Shimizu, T.; Kawada, T.; Park, B.J.; et al. Effect of phytoncide from trees on human natural killer cell function. Int. J. Immunopathol. Pharmacol. 2009, 22, 951–959. [Google Scholar] [CrossRef] [PubMed]
- Li, Q.; Kawada, T. Effect of forest environments on human natural killer (NK) activity. Int. J. Immunopathol Pharmacol. 2011, 24 (Suppl. S1), 39–44. [Google Scholar]
- Im, S.G.; Choi, H.; Jeon, Y.-H.; Song, M.-K.; Kim, W.; Woo, J.-M. Comparison of Effect of Two-Hour Exposure to Forest and Urban Environments on Cytokine, Anti-Oxidant, and Stress Levels in Young Adults. Int. J. Environ. Res. Public Health 2016, 13, 625. [Google Scholar] [CrossRef] [PubMed]
- Song, C.; Ikei, H.; Park, B.J.; Lee, J.; Kagawa, T.; Miyazaki, Y. Psychological Benefits of Walking through Forest Areas. Int. J. Environ. Res. Public Health 2018, 15, 2804. [Google Scholar] [CrossRef] [PubMed]
- Danhauer, S.C.; Addington, E.L.; Sohl, S.J.; Chaoul, A.; Cohen, L. Review of yoga therapy during cancer treatment. Support. Care Cancer 2017, 25, 1357–1372. [Google Scholar] [CrossRef] [PubMed]
- McCarney, R.; Warner, J.; Iliffe, S.; van Haselen, R.; Griffin, M.; Fisher, P. The Hawthorne Effect: A randomised, controlled trial. BMC Med Res. Methodol. 2007, 7, 30. [Google Scholar] [CrossRef] [PubMed]

| Variables | |
|---|---|
| Age (Mean ± SD) | 53.6 ± 5.8 |
| Sex (M/F) | 1/8 |
| Height (Mean ± SD) | 155.5 ± 5.7 |
| Weight (Mean ± SD) | 53.1 ± 10.2 |
| BMI (Mean ± SD) | 21.9 ± 3.4 |
| Variables | Pre-Forest Therapy | Post-Forest Therapy | p |
|---|---|---|---|
| TST | 367.2 ± 33.4 | 398.0 ± 33.8 | 0.020 |
| Latency of sleep onset | 14.9 ± 19.8 | 6.5 ± 6.7 | 0.293 |
| Sleep efficiency | 80.5 ± 7.1 | 88.4 ± 5.2 | 0.027 |
| WASO | 65.1 ± 34.6 | 53.5 ± 26.3 | 0.514 |
| N1 | 22.1 ± 9.7 | 16.0 ± 6.6 | 0.084 |
| N2 | 49.7 ± 7.1 | 54.1 ± 5.6 | 0.074 |
| N3 | 11.9 ± 5.2 | 12.8 ± 5.8 | 0.543 |
| REM | 16.3 ± 6.4 | 17.1 ± 5.8 | 0.758 |
| AHI | 10.9 ± 4.1 | 13.4 ± 12.2 | 0.272 |
| PLMi | 8.9 ± 13.1 | 12.0 ± 19.9 | 0.524 |
| Variables | Pre-Forest Therapy | Post-Forest Therapy | p |
|---|---|---|---|
| PSQI-K | 8.0 ± 4.4 | 7.3 ± 4.9 | 0.299 |
| STOP BANG | 1.6 ± 1.1 | 1.5 ± 1.1 | 0.347 |
| SSS | 2.1 ± 1.2 | 2.0 ± 1.1 | 0.729 |
| ESS | 6.1 ± 4.9 | 6.9 ± 5.6 | 0.393 |
| HADS_Anxiety | 5.0 ± 4.0 | 4.9 ± 4.2 | 0.855 |
| HADS_Depression | 3.6 ± 3.2 | 3.2 ± 3.1 | 0.438 |
| ISI | 5.8 ± 4.6 | 6.3 ± 5.3 | 0.621 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kim, H.; Lee, Y.W.; Ju, H.J.; Jang, B.J.; Kim, Y.I. An Exploratory Study on the Effects of Forest Therapy on Sleep Quality in Patients with Gastrointestinal Tract Cancers. Int. J. Environ. Res. Public Health 2019, 16, 2449. https://doi.org/10.3390/ijerph16142449
Kim H, Lee YW, Ju HJ, Jang BJ, Kim YI. An Exploratory Study on the Effects of Forest Therapy on Sleep Quality in Patients with Gastrointestinal Tract Cancers. International Journal of Environmental Research and Public Health. 2019; 16(14):2449. https://doi.org/10.3390/ijerph16142449
Chicago/Turabian StyleKim, Hyeyun, Yong Won Lee, Hyo Jin Ju, Bong Jin Jang, and Yeong In Kim. 2019. "An Exploratory Study on the Effects of Forest Therapy on Sleep Quality in Patients with Gastrointestinal Tract Cancers" International Journal of Environmental Research and Public Health 16, no. 14: 2449. https://doi.org/10.3390/ijerph16142449
APA StyleKim, H., Lee, Y. W., Ju, H. J., Jang, B. J., & Kim, Y. I. (2019). An Exploratory Study on the Effects of Forest Therapy on Sleep Quality in Patients with Gastrointestinal Tract Cancers. International Journal of Environmental Research and Public Health, 16(14), 2449. https://doi.org/10.3390/ijerph16142449






