Use of an Integrated Research-Practice Partnership to Improve Outcomes of a Community-Based Strength-Training Program for Older Adults: Reach and Effect of Lifelong Improvements through Fitness Together (LIFT)
Abstract
:1. Introduction
2. Materials and Methods
2.1. Program Design
2.2. Interventions
2.3. Research Design
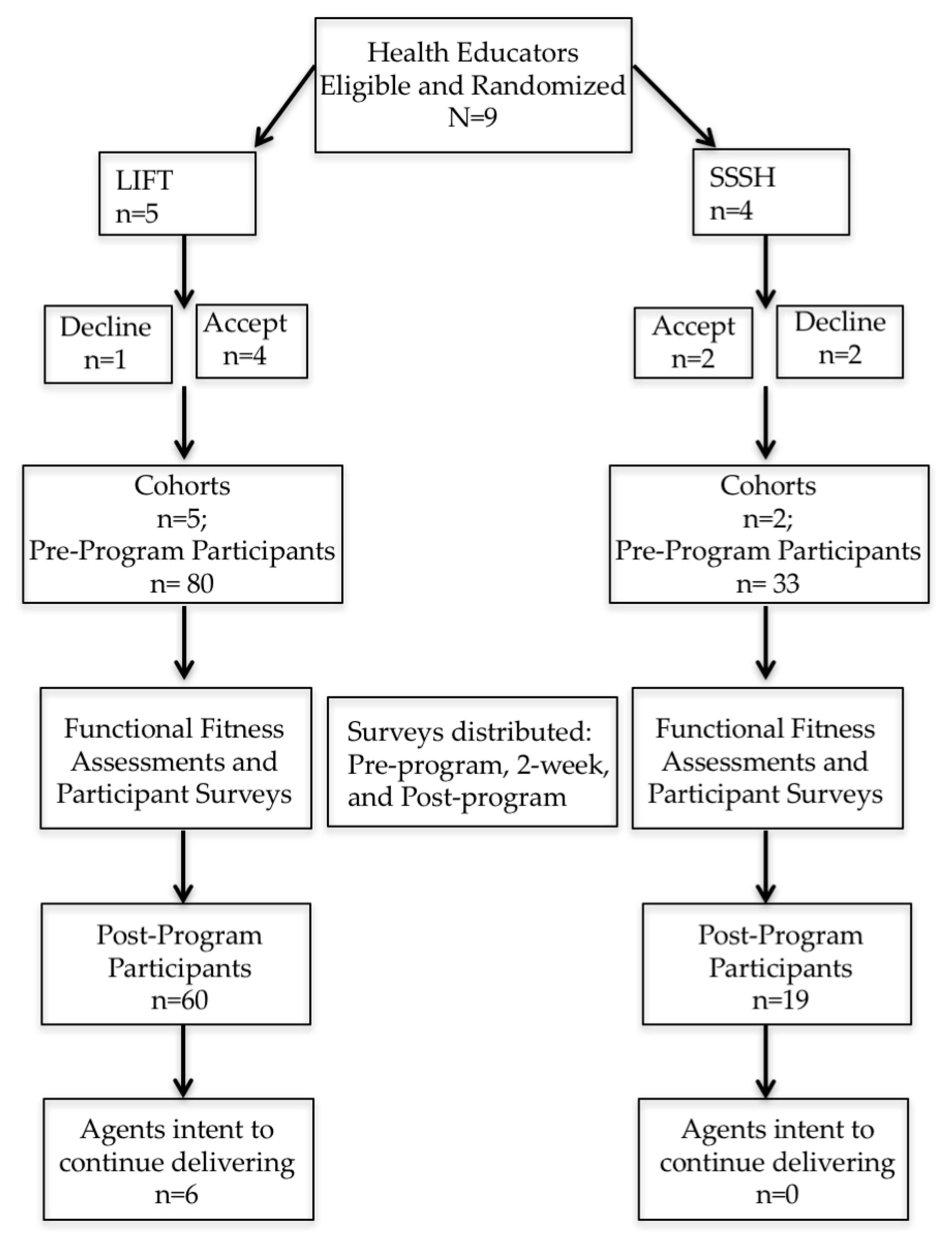
2.4. Older Adult Participants
2.5. Measures
2.5.1. Reach, Representativeness, and Retention
2.5.2. Cohesion
2.5.3. Effectiveness
2.5.4. System-Level Indicators
2.6. Statistical Analyses
3. Results
3.1. Reach, Representativeness, and Retention
3.2. Effectiveness: Functional Fitness and Balance Tests
3.3. System-Level Indicators
4. Discussion
5. Conclusions
Supplementary Materials
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Nelson, M.E.; Rejeski, W.J.; Blair, S.N.; Duncan, P.W.; Judge, J.O.; King, A.C.; Macera, C.A.; Castaneda-Sceppa, C. Physical activity and public health in older adults: Recommendation from the American college of sports medicine and the American heart association. Circulation 2007, 116, 1094–1105. [Google Scholar] [CrossRef] [PubMed]
- CDC. How Much Physical Activity Do Older Adults Need? Available online: http://www.cdc.gov/physicalactivity/basics/older_adults/index.htm (accessed on 18 November 2016).
- CDC. National Center for Health Statistics; National Health Interview Survey; Centers for Disease Control and Prevention: Atlanta, GA, USA, 2015.
- Brown, M.; Sinacore, D.R.; Host, H.H. The relationship of strength to function in the older adult. J. Gerontol. Ser. A Biol. Sci. Med. Sci. 1995, 50, 55–59. [Google Scholar]
- Latham, N.K.; Bennett, D.A.; Stretton, C.M.; Anderson, C.S. Systematic review of progressive resistance strength training in older adults. J. Gerontol. Ser. A Biol. Sci. Med. Sci. 2004, 59, 48–61. [Google Scholar] [CrossRef]
- Rikli, R.E.; Jones, C.J. Development and validation of a functional fitness test for community-residing older adults. J. Aging Phys. Act. 1999, 7, 129–161. [Google Scholar] [CrossRef]
- Seguin, R.; Nelson, M.E. The benefits of strength training for older adults. Am. J. Prev. Med. 2003, 25, 141–149. [Google Scholar] [CrossRef]
- Cavani, V.; Mier, C.M.; Musto, A.A.; Tummers, N. Effects of a 6-week resistance-training program on functional fitness of older adults. J. Aging Phys. Act. 2002, 10, 443–452. [Google Scholar] [CrossRef]
- Belza, B.; Shumway-Cook, A.; Phelan, E.A.; Williams, B.; Snyder, S.J.; LoGerfo, J.P. The effects of a community-based exercise program on function and health in older adults: The enhancefitness program. J. Appl. Gerontol. 2006, 25, 291–306. [Google Scholar] [CrossRef]
- Jette, A.M.; Lachman, M.; Giorgetti, M.M.; Assmann, S.F.; Harris, B.A.; Levenson, C.; Wernick, M.; Krebs, D. Exercise—It’s never too late: The strong-for-life program. Am. J. Public Health 1999, 89, 66–72. [Google Scholar] [CrossRef] [PubMed]
- Chase, J.A.D. Physical activity interventions among older adults: A literature review. Res. Theory Nurs. Pract. 2013, 27, 53–80. [Google Scholar] [CrossRef] [PubMed]
- Estabrooks, P.A.; Glasgow, R.E. Translating effective clinic-based physical activity interventions into practice. Am. J. Prev. Med. 2006, 31, S45–S56. [Google Scholar] [CrossRef] [PubMed]
- Glasgow, R.E.; Emmons, K.M. How can we increase translation of research into practice? Types of evidence needed. Annu. Rev. Public Health 2007, 28, 413–433. [Google Scholar] [CrossRef] [PubMed]
- Estabrooks, P.A.; Smith-Ray, R.L.; Dzewaltowski, D.A.; Dowdy, D.; Lattimore, D.; Rheaume, C.; Ory, M.G.; Bazzarre, T.; Griffin, S.F.; Wilcox, S. Sustainability of evidence-based community-based physical activity programs for older adults: Lessons from active for life. Transl. Behav. Med. 2011, 1, 208–215. [Google Scholar] [CrossRef] [PubMed]
- Shubert, T.E.; Smith, M.L.; Schneider, E.C.; Wilson, A.D.; Ory, M.G. Commentary: Public health system perspective on implementation of evidence-based fall-prevention strategies for older adults. Front. Public Health 2016, 4, 252. [Google Scholar] [CrossRef] [PubMed]
- Johnson, S.B.; Harden, S.M.; Estabrooks, P.A. Uptake of evidence-based physical activity programs: Comparing perceptions of adopters and nonadopters. Transl. Behav. Med. 2016, 6, 629–637. [Google Scholar] [CrossRef] [PubMed]
- Minkler, M. Using participatory action research to build healthy communities. Public Health Rep. 2000, 115, 191–197. [Google Scholar] [CrossRef] [PubMed]
- Harden, S.M.; Johnson, S.B.; Almeida, F.A.; Estabrooks, P.A. Improving phsical activity program adoption using integrated research-practice partnerships: An effectiveness-implementation trial. Transl. Behav. Med. Pract. Policy Res. 2016, 7, 28–38. [Google Scholar] [CrossRef] [PubMed]
- Harrison, M.B.; Graham, I.D. Roadmap for a participatory research-practice partnership to implement evidence. Worldviews Evid. Based Nurs. 2012, 9, 210–220. [Google Scholar] [CrossRef] [PubMed]
- Wilson, M.L.; Strayer, T.E., III; Davis, R.; Harden, S.M. Informed adaptations of a strength-training program through a research-practice partnership. Front. Public Health 2017. submitted for publication. [Google Scholar]
- Estabrooks, P.A.; Fox, E.H.; Doerksen, S.E.; Bradshaw, M.H.; King, A.C. Participatory research to promote physical activity at congregate-meal sites. J. Aging Phys. Act. 2005, 13, 121–144. [Google Scholar] [CrossRef] [PubMed]
- Klesges, L.M.; Estabrooks, P.A.; Dzewaltowski, D.A.; Bull, S.S.; Glasgow, R.E. Beginning with the application in mind: Designing and planning health behavior change interventions to enhance dissemination. Ann. Behav. Med. 2005, 29, 66–75. [Google Scholar] [CrossRef] [PubMed]
- Cooperative Extension System. Available online: https://nifa.usda.gov/cooperative-extension-system (accessed on 18 November 2016).
- Palmer-Keenan, D.M.; Corda, K. Should physical activity be included in nutrition education? A comparison of nutrition outcomes with and without in-class activities. J. Ext. 2014, 52, n4. [Google Scholar]
- Seguin, R.A.; Economos, C.D.; Hyatt, R.; Palombo, R.; Reed, P.N.T.; Nelson, M.E. Design and national dissemination of the strongwomen community strength training program. Prev. Chronic Dis. 2008, 5, A25. [Google Scholar] [PubMed]
- Teran, B.M.; Hongu, N. Successful statewide walking program websites. J. Ext. 2012, 50, 1TOT9. [Google Scholar]
- Ball, S.; Gammon, R.; Kelly, P.J.; Cheng, A.L.; Chertoff, K.; Kaume, L.; Abreu, E.L.; Brotto, M. Outcomes of stay strong, stay healthy in community settings. J. Aging Health 2013, 25, 1388–1397. [Google Scholar] [CrossRef] [PubMed]
- Chambers, D.A.; Norton, W.E. The adaptome: Advancing the science of intervention adaptation. Am. J. Prev. Med. 2016, 51, S124–S131. [Google Scholar] [CrossRef] [PubMed]
- Brand, T.; Pischke, C.R.; Steenbock, B.; Schoenbach, J.; Poettgen, S.; Samkange-Zeeb, F.; Zeeb, H. What works in community-based interventions promoting physical activity and healthy eating? A review of reviews. Int. J. Environ. Res. Public Health 2014, 11, 5866–5888. [Google Scholar] [CrossRef] [PubMed]
- Baker, P.R.; Francis, D.P.; Soares, J.; Weightman, A.L.; Foster, C. Community wide interventions for increasing physical activity. Cochrane Database Syst. Rev. 2011, CD008366. [Google Scholar] [CrossRef]
- Minkler, M.; Salvatore, A. Participatory approaches for study design and analysis in dissemination and implementation research. In Dissemination and Implementation Research in Health: Translating Science to Practice; Oxford University Press: New York, NY, USA, 2012; pp. 192–208. [Google Scholar]
- Thompson, P.D.; Arena, R.; Riebe, D.; Pescatello, L.S. American College of Sports Medicine. ACSM’s new preparticipation health screening recommendations from ACSM’s guidelines for exercise testing and prescription, ninth edition. Curr. Sports Med. Rep. 2013, 12, 215–217. [Google Scholar] [CrossRef] [PubMed]
- Glasgow, R.E.; Vogt, T.M.; Boles, S.M. Evaluating the public health impact of health promotion interventions: The re-aim framework. Am. J. Public Health 1999, 89, 1322–1327. [Google Scholar] [CrossRef] [PubMed]
- Estabrooks, P.A.; Carron, A.V. The physical activity group environment questionnaire: An instrument for the assessment of cohesion in exercise classes. Group Dyn. Theory Res. Pract. 2000, 4, 230–243. [Google Scholar] [CrossRef]
- Carron, A.V.; Brawley, L.R.; Widmeyer, W.N. The measurement of cohesiveness in sport groups. In Advances in Sport and Exercise Psychology Measurement; Duda, J.L., Ed.; Fitness Information Technology: Morgantown, WV, USA, 1998; pp. 213–226. [Google Scholar]
- Harden, S.M.; Estabrooks, P.A.; Mama, S.K.; Lee, R.E. Longitudinal analysis of minority women’s perceptions of cohesion: The role of cooperation, communication, and competition. Int. J. Behav. Nutr. Phys. Act. 2014, 11, 57. [Google Scholar] [CrossRef] [PubMed]
- Berg, K.O.; Wood-Dauphinee, S.L.; Williams, J.I.; Maki, B. Measuring balance in the elderly: Validation of an instrument. Can. J. Public Health 1992, 83, S7–S11. [Google Scholar] [PubMed]
- Harden, S.M.; Fanning, J.T.; Motl, R.W.; McAuley, E.; Estabrooks, P.A. Determining the reach of a home-based physical activity program for older adults within the context of a randomized controlled trial. Health Educ. Res. 2014, 29, 861–869. [Google Scholar] [CrossRef] [PubMed]
- Rikli, R.E.; Jones, C.J. Development and validation of criterion-referenced clinically relevant fitness standards for maintaining physical independence in later years. Gerontologist 2013, 53, 255–267. [Google Scholar] [CrossRef] [PubMed]
- King, A.C.; Rejeski, W.J.; Buchner, D.M. Physical activity interventions targeting older adults—A critical review and recommendations. Am. J. Prev. Med. 1998, 15, 316–333. [Google Scholar] [CrossRef]
- Estabrooks, P.A.; Bradshaw, M.; Dzewaltowski, D.A.; Smith-Ray, R.L. Determining the impact of walk kansas: Applying a team-building approach to community physical activity promotion. Ann. Behav. Med. 2008, 36, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Cramp, A.G.; Brawley, L.R. Moms in motion: A group-mediated cognitive-behavioral physical activity intervention. Int. J. Behav. Nutr. Phys. Act. 2006, 3, 23. [Google Scholar] [CrossRef] [PubMed]
- Wellman, N.S.; Kamp, B.; Kirk-Sanchez, N.J.; Johnson, P.M. Eat better & move more: A community-based program designed to improve diets and increase physical activity among older Americans. Am. J. Public Health 2007, 97, 710–717. [Google Scholar] [PubMed]
- Estabrooks, P.A.; Carron, A.V. Group cohesion in older adult exercisers: Prediction and intervention effects. J. Behav. Med. 1999, 22, 575–588. [Google Scholar] [CrossRef] [PubMed]
- Brawley, L.R.; Rejeski, W.J.; Lutes, L. A group-mediated cognitive-behavioral intervention for increasing adherence to physical activity in older adults. J. Appl. Biobehav. Res. 2000, 5, 47–65. [Google Scholar] [CrossRef]
- Warren-Findlow, J.; Prohaska, T.R.; Freedman, D. Challenges and opportunities in recruiting and retaining underrepresented populations into health promotion research. Gerontologist 2003, 43, 37–46. [Google Scholar] [CrossRef] [PubMed]
- Sullivan-Marx, E.M.; Mangione, K.K.; Ackerson, T.; Sidorov, I.; Maislin, G.; Volpe, S.L.; Craik, R. Recruitment and retention strategies among older African American women enrolled in an exercise study at a pace program. Gerontologist 2011, 51, S73–S81. [Google Scholar] [CrossRef] [PubMed]
- Harden, S.M.; Burke, S.M.; Haile, A.M.; Estabrooks, P.A. Generalizing the findings from group dynamics-based physical activity research to practice settings: What do we know? Eval. Health Prof. 2015, 38, 3–14. [Google Scholar] [CrossRef] [PubMed]
- Harden, S.M.; McEwan, D.; Sylvester, B.D.; Kaulius, M.; Ruissen, G.; Burke, S.M.; Estabrooks, P.A.; Beauchamp, M.R. Understanding for whom, under what conditions, and how group-based physical activity interventions are successful: A realist review. BMC Public Health 2015, 15, 958. [Google Scholar] [CrossRef] [PubMed]
- Estabrooks, P.A.; Harden, S.M.; Burke, S.M. Group dynamics in physical activity: What works? Soc. Personal. Psychol. Compass 2012, 6, 18–40. [Google Scholar] [CrossRef]
- Baron, R.M.; Kenny, D.A. The moderator mediator variable distinction in social psychological-research-conceptual, strategic, and statistical considerations. J. Personal. Soc. Psychol. 1986, 51, 1173–1182. [Google Scholar] [CrossRef]
- Mor, V.; Murphy, J.; Masterson-Allen, S.; Willey, C.; Razmpour, A.; Jackson, M.E.; Greer, D.; Katz, S. Risk of functional decline among well elders. J. Clin. Epidemiol. 1989, 42, 895–904. [Google Scholar] [CrossRef]
- Gillette, D.B.; Petrescu-Prahova, M.; Herting, J.R.; Belza, B. A pilot study of determinants of ongoing participation in enhancefitness: A community-based group exercise program for older adults. J. Geriatr. Phys. Ther. 2015, 38, 194–201. [Google Scholar] [CrossRef] [PubMed]
- McNamara, A.; Gunter, K. The influence of participation in better bones and balance on skeletal health: Evaluation of a community-based exercise program to reduce fall and fracture risk. Osteoporos. Int. 2012, 23, 1813–1822. [Google Scholar] [CrossRef] [PubMed]
- Hughes, S.L.; Seymour, R.B.; Campbell, R.; Pollak, N.; Huber, G.; Sharma, L. Impact of the fit and strong intervention on older adults with osteoarthritis. Gerontologist 2004, 44, 217–228. [Google Scholar] [CrossRef] [PubMed]
- Kraschnewski, J.L.; Sciamanna, C.N.; Poger, J.M.; Rovniak, L.S.; Lehman, E.B.; Cooper, A.B.; Ballentine, N.H.; Ciccolo, J.T. Is strength training associated with mortality benefits? A 15 year cohort study of US older adults. Prev. Med. 2016, 87, 121–127. [Google Scholar] [CrossRef] [PubMed]
- Volaklis, K.A.; Halle, M.; Meisinger, C. Muscular strength as a strong predictor of mortality: A narrative review. Eur. J. Intern. Med. 2015, 26, 303–310. [Google Scholar] [CrossRef] [PubMed]
- Nelson, M.E.; Fiatarone, M.A.; Morganti, C.M.; Trice, I.; Greenberg, R.A.; Evans, W.J. Effects of high-intensity strength training on multiple risk factors for osteoporotic fractures. A randomized controlled trial. JAMA 1994, 272, 1909–1914. [Google Scholar] [CrossRef] [PubMed]
- Chase, J.A.D. Interventions to increase physical activity among older adults: A meta-analysis. Gerontologist 2015, 55, 706–718. [Google Scholar] [CrossRef] [PubMed]
- Balis, L.; Strayer, T.; Ramalingam, N.; Wilson, M.; Harden, S.M. Open-access physical activity programs for older adults: A pragmatic and systematic review. Gerontologist 2018. [Google Scholar] [CrossRef] [PubMed]
| Component of Intervention | SSSH | LIFT |
|---|---|---|
| Duration | 1-h sessions Participants encouraged to attend 2 times a week for 8 weeks | 1-h sessions Participants encouraged to attend 2 times a week for 8 weeks Participants are encouraged to complete an additional thirty minutes of aerobic exercise outside of LIFT (e.g., walking, gardening, etc.) |
| Audience | Inactive, aging men and women | |
| Behavior change components | Not applicable | Observational learning Self-monitoring Self efficacy Group dynamics Relapse prevention Goal setting |
| Exercises | Active warm-up 8 core strength training exercises Cool down | |
| Group Dynamics | Not applicable | Group environment (e.g., small groups for interaction, group name) Group structure (e.g., group roles, group norms) Group processes (e.g., friendly competition, social support, group goal setting, etc.) |
| Goal | Increase muscle and bone density Decrease osteoporosis and frailty | Increase muscle and bone density Decrease osteoporosis and frailty Implement group dynamics-based behavior change strategies to increase program adherence and improve functional fitness of older adults |
| Characteristics | Population a (N = 1,019,857.52) | LIFT (n = 80) | SSSH (n = 33) |
|---|---|---|---|
| Age, M (SD) | 65+ | 72.55 (±11.06) | 73.63 (±9.68) |
| BMI, M (SD) | 27.8 | 30.56 (±6.23) | 33.77 (±8.11) |
| Sex, % | |||
| Male | 44 | 14 * | 9 * |
| Female | 56 | 73 * | 73 * |
| Not reported | - | 13 | 18 |
| Ethnicity, % | |||
| Hispanic | 3 | 3 | 0 * |
| Non-Hispanic | 97 | 78 | 82 * |
| Not reported | - | 19 | 18 |
| Race, % | |||
| White | 79 | 56 | 27 * |
| Black | 15 | 11 | 52 * |
| Other | 6 | 1 | 3 * |
| Not reported | - | 12 | 21 |
| Functional Fitness Assessment, M (SD) | Intervention | Baseline | Post-Program (ITT) a | Change Scores |
|---|---|---|---|---|
| Sit and stands b | LIFT | 10.58 (±3.21) | 13.07 (±5.14) | 2.67 (±3.73) * |
| SSSH | 9.40 (±4.29) | 10.71 (±3.22) | 1.31 (±2.17) * | |
| Arm curls b | LIFT | 13.89 (±4.0) | 17.65(±6.22) | 3.65 (±6.03) * |
| SSSH | 14.50 (±5.55) | 15.9 (±4.3) | 1.40 (±6.37) | |
| 2-min step test c | LIFT | 61.66 (±30.0) | 77.5 (±30.0) | 14.03 (±16.71) * |
| SSSH | 52.6 (±22.6) | 72.4 (±32.3) | 20.33 (±33.09) * | |
| Lower body flexibility d | LIFT | −1.74 (±3.86) | −0.0003 (±2.96) | 1.77 (±2.97) * |
| SSSH | −0.76 (±3.12) | 0.68 (±3.05) | 1.44 (±2.53) * | |
| Upper body flexibility d | LIFT | −5.05 (±4.93) | −4.2 (±5.51) | 1.24 (±3.17) * |
| SSSH | −6.05 (±5.69) | −4.8 (±4.06) | 1.25 (±1.94) * | |
| 8-foot up-and-go e | LIFT | 7.68 (±3.84) | 7.02 (±3.25) | −0.65 (±1.31) * |
| SSSH | 7.19(±2.92) | 6.6 (±1.94) | −0.60 (±1.97) | |
| Composite balance score f | LIFT | 2.44 (±1.3) | 2.79 (±1.5) | 0.35 (±1.18) * |
| SSSH | 2.00 (±1.0) | 2.42 (±1.4) | 0.42 (±0.99) * |
| Group Cohesion Dimension | Intervention | N | Baseline | N | Post Program | N | Change Score |
|---|---|---|---|---|---|---|---|
| Attraction to group: Task | LIFT | 65 | 4.36 (±0.60) | 40 | 4.38 (±0.72) | 36 | −0.19 (±0.48) |
| SSSH | 22 | 4.61 (±0.47) | 17 | 4.51 (±0.99) | 12 | −0.06 (±1.07) | |
| Attraction to group: Social | LIFT | 65 | 3.67 (±0.81) | 40 | 3.81(±0.84) | 36 | −0.12 (±0.69) |
| SSSH | 21 | 4.51 (±0.61) | 17 | 4.24 (±1.04) | 11 | −0.06 (±1.14) | |
| Group integration: Task | LIFT | 65 | 3.89 (±0.63) | 39 | 4.0 (±0.80) | 35 | −0.13 (±0.61) |
| SSSH | 22 | 4.58 (±0.51) | 17 | 4.06 (±1.09) | 12 | −0.47 (±1.06) * | |
| Group Integration: Social | LIFT | 65 | 3.14 (±0.88) | 35 | −3.28 (±0.80) | 32 | 0.04 (±0.94) |
| SSSH | 20 | 4.24 (±0.83) | 17 | 3.84 (±1.12) | 11 | −0.03 (±1.32) | |
| Cooperation | LIFT | 64 | 4.17 (±0.56) | 36 | 4.09 (±0.77) | 33 | −0.24 (±0.75) |
| SSSH | 21 | 4.38 (±0.60) | 18 | 4.20 (±1.02) | 12 | −0.17 (±1.08) | |
| Friendly Competition | LIFT | 64 | 3.70 (±0.72) | 35 | 3.53 (±0.86) | 32 | −0.23 (±0.76) |
| SSSH | 22 | 4.38(±0.73) | 17 | 4.16 (±1.02) | 12 | −0.17 (±1.01) | |
| Communication: Task | LIFT | 64 | 3.68 (±0.80) | 35 | 3.60 (±0.87) | 32 | −0.20 (±0.74) |
| SSSH | 22 | 4.14 (±0.71) | 17 | 4.0 (±1.05) | 12 | −0.15 (±1.39) * | |
| Communication: Social | LIFT | 64 | 3.62 (±0.76) | 35 | 3.74 (± 0.77) | 32 | 0.02 (± 0.92) |
| SSSH | 22 | 4.29 (±0.75) | 17 | 4.04 (±1.05) | 12 | −0.03 (±1.14) |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wilson, M.L.; Strayer, T.E., III; Davis, R.; Harden, S.M. Use of an Integrated Research-Practice Partnership to Improve Outcomes of a Community-Based Strength-Training Program for Older Adults: Reach and Effect of Lifelong Improvements through Fitness Together (LIFT). Int. J. Environ. Res. Public Health 2018, 15, 237. https://doi.org/10.3390/ijerph15020237
Wilson ML, Strayer TE III, Davis R, Harden SM. Use of an Integrated Research-Practice Partnership to Improve Outcomes of a Community-Based Strength-Training Program for Older Adults: Reach and Effect of Lifelong Improvements through Fitness Together (LIFT). International Journal of Environmental Research and Public Health. 2018; 15(2):237. https://doi.org/10.3390/ijerph15020237
Chicago/Turabian StyleWilson, Meghan L., Thomas E. Strayer, III, Rebecca Davis, and Samantha M. Harden. 2018. "Use of an Integrated Research-Practice Partnership to Improve Outcomes of a Community-Based Strength-Training Program for Older Adults: Reach and Effect of Lifelong Improvements through Fitness Together (LIFT)" International Journal of Environmental Research and Public Health 15, no. 2: 237. https://doi.org/10.3390/ijerph15020237
APA StyleWilson, M. L., Strayer, T. E., III, Davis, R., & Harden, S. M. (2018). Use of an Integrated Research-Practice Partnership to Improve Outcomes of a Community-Based Strength-Training Program for Older Adults: Reach and Effect of Lifelong Improvements through Fitness Together (LIFT). International Journal of Environmental Research and Public Health, 15(2), 237. https://doi.org/10.3390/ijerph15020237




