Breaking up Sedentary Time in Overweight/Obese Adults on Work Days and Non-Work Days: Results from a Feasibility Study
Abstract
1. Introduction
2. Methods
2.1. Participants
2.2. Study Design
2.3. Screening Visit
2.4. Measurement of Time Spent Sitting/Lying, Standing, Stepping and Daily Steps
2.5. Measurement of Physical Activity Intensity, Activity Energy Expenditure and Physical Activity Level
2.6. Perception of the Challenges Associated with the Conditions, Self-Perceived Vigor and Fatigue
2.7. Plasma Metabolic Outcomes
2.8. Statistical Analysis
3. Results
3.1. Subjects’ Characteristics and Compliance with the Interventions
3.2. Effect of the Physical Activity Interventions on Time Spent Sitting/Lying, Standing and Stepping
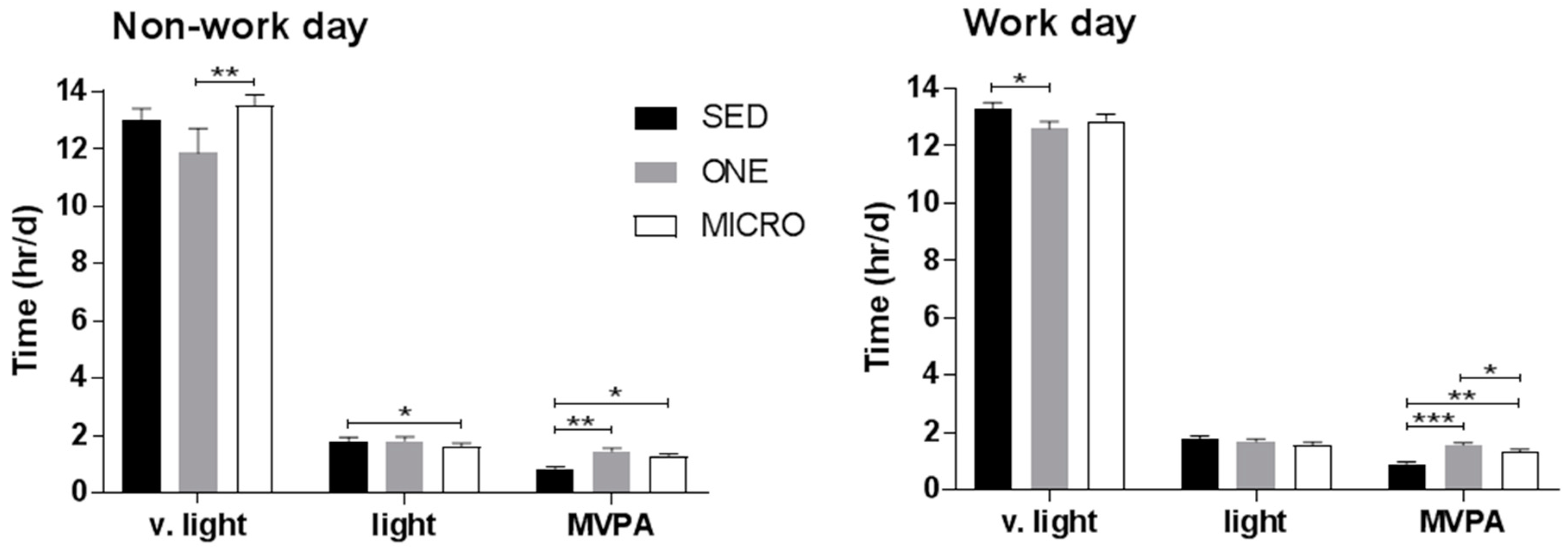
3.3. Effect of the Physical Activity Interventions on Time Spent in Very-Light, Light, Moderate and Vigorous Intensity Physical Activity
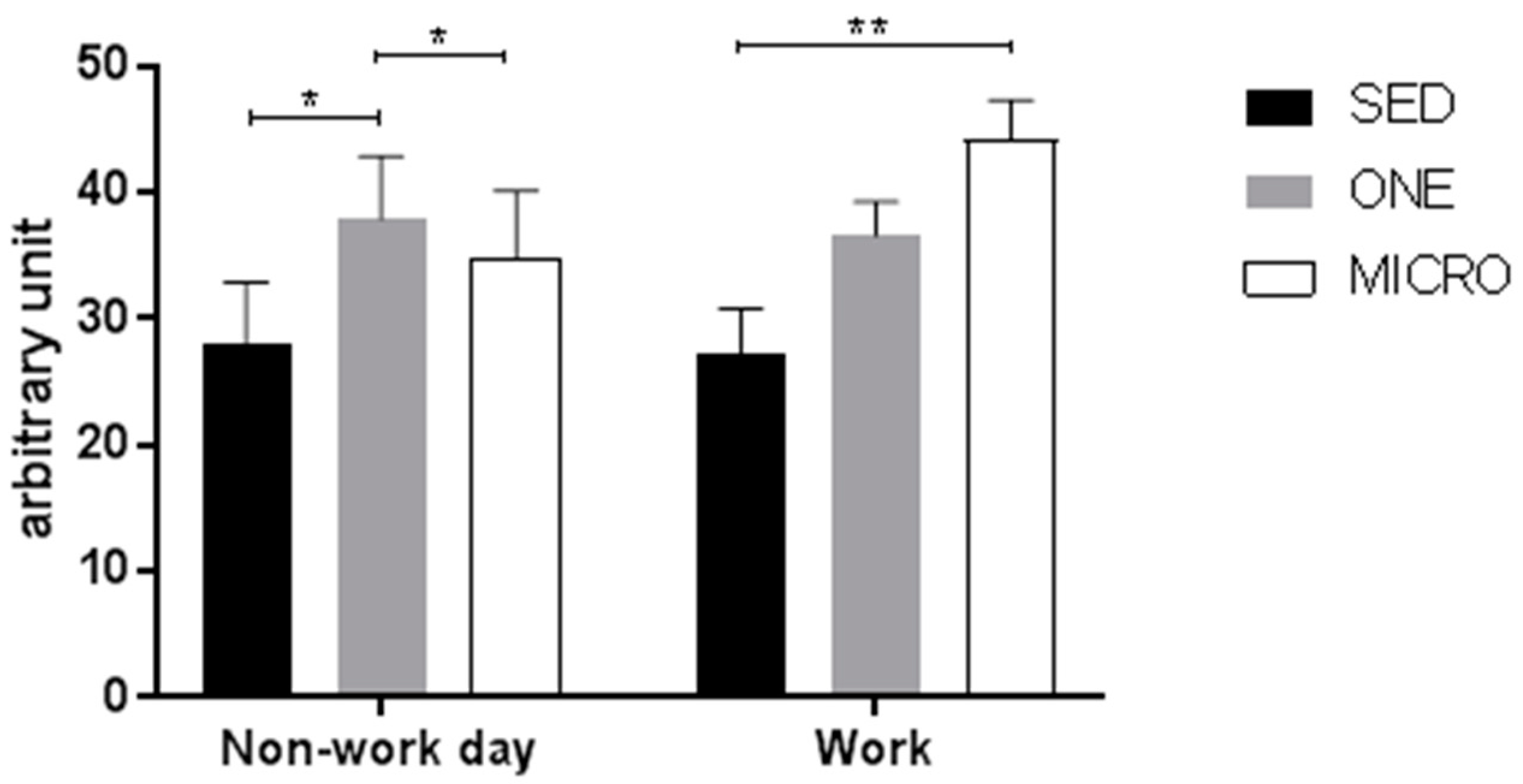
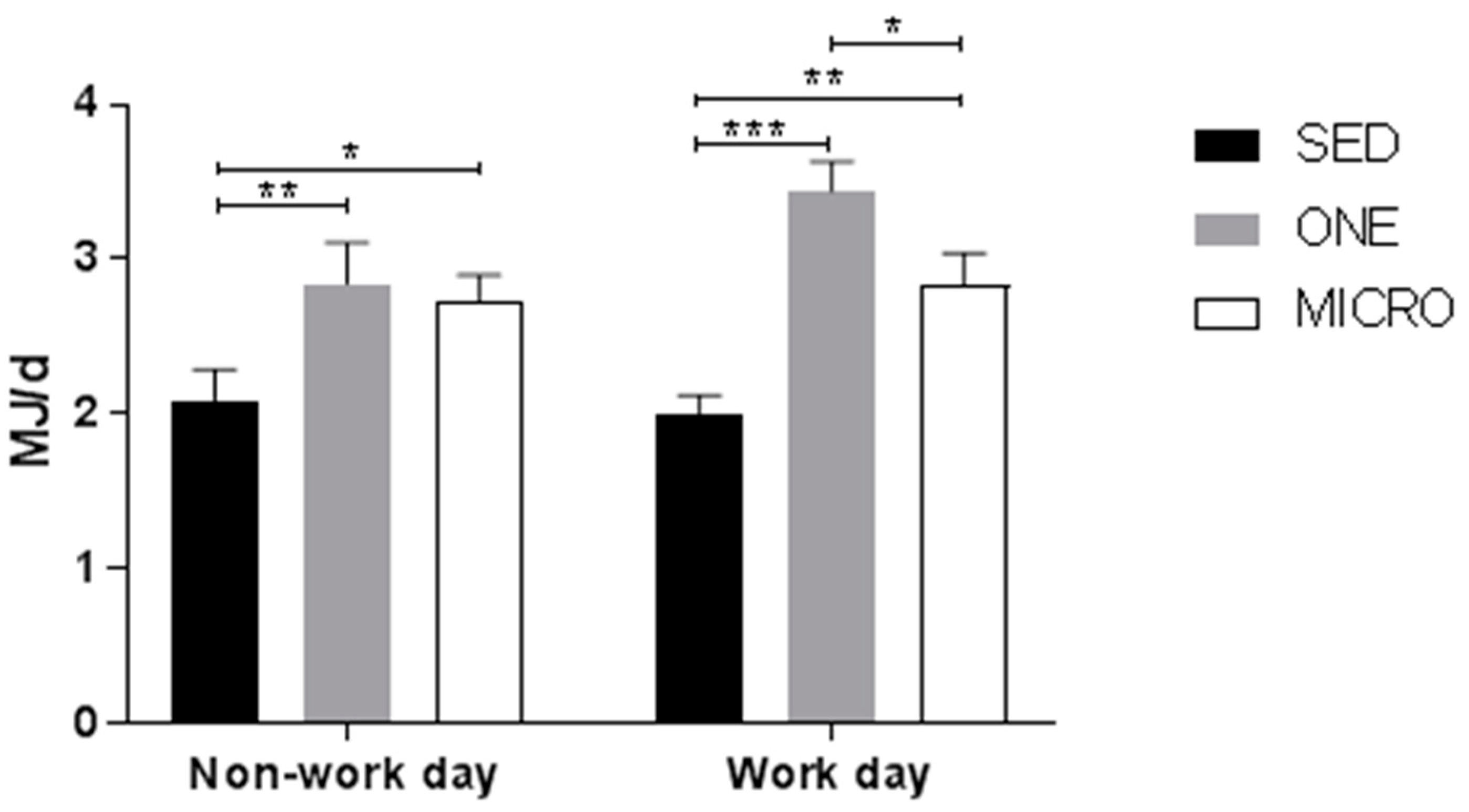
3.4. Effect of the Physical Activity Interventions on 24 h Activity Energy Expenditure and Physical Activity Level
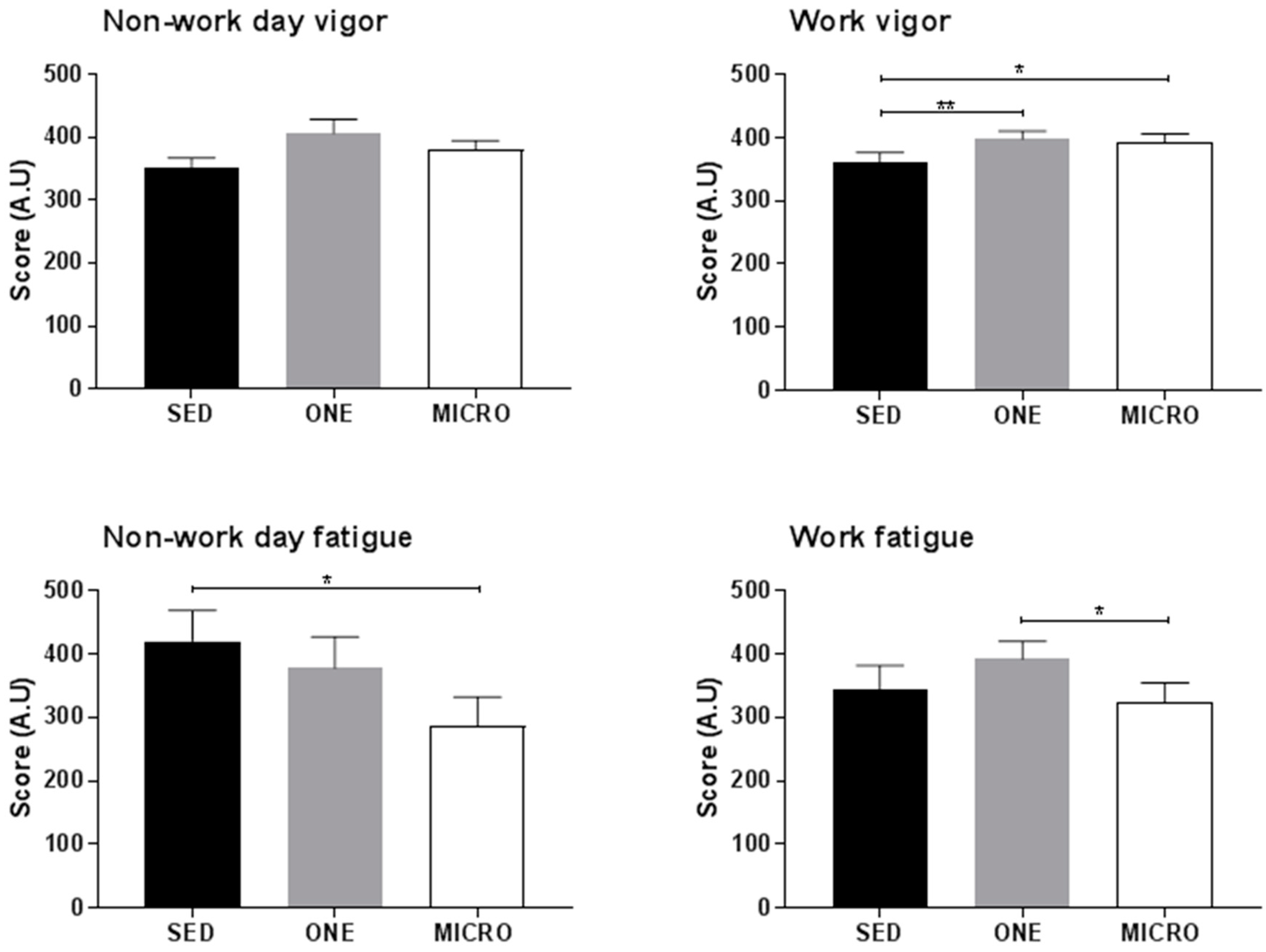
3.5. Effect of the Physical Activity Interventions on Self-Perceived Vigor and Fatigue
3.6. Effect of the Physical Activity Interventions on Index of Insulin Sensitivity
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgements
Conflicts of interest
References
- Owen, N.; Healy, G.N.; Matthews, C.E.; Dunstan, D.W. Too Much Sitting: The Population-Health Science of Sedentary Behavior. Exerc. Sport Sci. Rev. 2010, 38, 105–113. [Google Scholar] [CrossRef] [PubMed]
- Bauman, A.E.; Chau, J.Y.; Ding, D.; Bennie, J. Too Much Sitting and Cardio-Metabolic Risk: An Update of Epidemiological Evidence. Curr. Cardiovasc. Risk Rep. 2013, 7, 293–298. [Google Scholar] [CrossRef]
- Thorp, A.A.; Owen, N.; Neuhaus, M.; Dunstan, D.W. Sedentary behaviors and subsequent health outcomes in adults a systematic review of longitudinal studies, 1996–2011. Am. J. Prev. Med. 2011, 41, 207–215. [Google Scholar] [CrossRef] [PubMed]
- Wilmot, E.G.; Edwardson, C.L.; Achana, F.A.; Davies, M.J.; Gorely, T.; Gray, L.J.; Khunti, K.; Yates, T.; Biddle, S.J. Sedentary time in adults and the association with diabetes, cardiovascular disease and death: Systematic review and meta-analysis. Diabetologia 2012, 55, 2895–2905. [Google Scholar] [CrossRef] [PubMed]
- Edwardson, C.L.; Gorely, T.; Davies, M.J.; Gray, L.J.; Khunti, K.; Wilmot, E.G.; Yates, T.; Biddle, S.J. Association of sedentary behaviour with metabolic syndrome: A meta-analysis. PLoS ONE 2012, 7, e34916. [Google Scholar] [CrossRef] [PubMed]
- de Rezende, L.F.; Rodrigues Lopes, M.; Rey-Lopez, J.P.; Matsudo, V.K.; Luiz Odo, C. Sedentary behavior and health outcomes: An overview of systematic reviews. PLoS ONE 2014, 9, e105620. [Google Scholar] [CrossRef] [PubMed]
- Suchert, V.; Hanewinkel, R.; Isensee, B. Sedentary behavior and indicators of mental health in school-aged children and adolescents: A systematic review. Prev. Med. 2015, 76, 48–57. [Google Scholar] [CrossRef] [PubMed]
- van Uffelen, J.G.; van Gellecum, Y.R.; Burton, N.W.; Peeters, G.; Heesch, K.C.; Brown, W.J. Sitting-time, physical activity, and depressive symptoms in mid-aged women. Am. J. Prev. Med. 2013, 45, 276–281. [Google Scholar] [CrossRef] [PubMed]
- Rynders, C.A.; Blanc, S.; DeJong, N.; Bessesen, D.H.; Bergouignan, A. Sedentary behaviour is a key determinant of metabolic inflexibility. J. Physiol. 2017, 596, 1319–1330. [Google Scholar] [CrossRef] [PubMed]
- Judice, P.B.; Hamilton, M.T.; Sardinha, L.B.; Silva, A.M. Randomized controlled pilot of an intervention to reduce and break-up overweight/obese adults’ overall sitting-time. Trials 2015, 16, 490. [Google Scholar] [CrossRef] [PubMed]
- Healy, G.N.; Dunstan, D.W.; Salmon, J.; Cerin, E.; Shaw, J.E.; Zimmet, P.Z.; Owen, N. Breaks in sedentary time: Beneficial associations with metabolic risk. Diabetes Care 2008, 31, 661–666. [Google Scholar] [CrossRef] [PubMed]
- Healy, G.N.; Matthews, C.E.; Dunstan, D.W.; Winkler, E.A.; Owen, N. Sedentary time and cardio-metabolic biomarkers in US adults: NHANES 2003-06. Eur. Heart J. 2011, 32, 590–597. [Google Scholar] [CrossRef] [PubMed]
- McCrady, S.K.; Levine, J.A. Sedentariness at Work: How Much Do We Really Sit? Obesity 2009, 17, 2103–2105. [Google Scholar] [CrossRef] [PubMed]
- Ryan, C.G.; Dall, P.M.; Granat, M.H.; Grant, P.M. Sitting patterns at work: Objective measurement of adherence to current recommendations. Ergonomics 2011, 54, 531–538. [Google Scholar] [CrossRef]
- Church, T.S.; Thomas, D.M.; Tudor-Locke, C.; Katzmarzyk, P.T.; Earnest, C.P.; Rodarte, R.Q.; Martin, C.K.; Blair, S.N.; Bouchard, C. Trends over 5 decades in U.S. occupation-related physical activity and their associations with obesity. PLoS ONE 2011, 6, e19657. [Google Scholar] [CrossRef] [PubMed]
- Physical Activity Strategy for the WHO European Region. Available online: http://www.euro.who.int/__data/assets/pdf_file/0010/282961/65wd09e_PhysicalActivityStrategy_150474.pdf (accessed on 30 August 2018).
- Alkhajah, T.A.; Reeves, M.M.; Eakin, E.G.; Winkler, E.A.H.; Owen, N.; Healy, G.N. Sit–Stand Workstations: A Pilot Intervention to Reduce Office Sitting Time. Am. J. Prev. Med. 2012, 43, 298–303. [Google Scholar] [CrossRef] [PubMed]
- Carr, L.J.; Walaska, K.A.; Marcus, B.H. Feasibility of a portable pedal exercise machine for reducing sedentary time in the workplace. Br. J. Sports Med. 2012, 46, 430–435. [Google Scholar] [CrossRef] [PubMed]
- Jones, R.A.; Hinkley, T.; Okely, A.D.; Salmon, J. Tracking physical activity and sedentary behavior in childhood: A systematic review. Am. J. Prev. Med. 2013, 44, 651–658. [Google Scholar] [CrossRef] [PubMed]
- Gilson, N.D.; Suppini, A.; Ryde, G.C.; Brown, H.E.; Brown, W.J. Does the use of standing ‘hot’ desks change sedentary work time in an open plan office? Prev. Med. 2012, 54, 65–67. [Google Scholar] [CrossRef] [PubMed]
- Healy, G.N.; Eakin, E.G.; Owen, N.; Lamontagne, A.D.; Moodie, M.; Winkler, E.A.; Fjeldsoe, B.S.; Wiesner, G.; Willenberg, L.; Dunstan, D.W. A Cluster Randomized Controlled Trial to Reduce Office Workers’ Sitting Time: Effect on Activity Outcomes. Med. Sci. Sports Exerc. 2016, 48, 1787–1797. [Google Scholar] [CrossRef] [PubMed]
- Hutchinson, J.; Headley, S.; Matthews, T.; Spicer, G.; Dempsey, K.; Wooley, S.; Janssen, X. Changes in Sitting Time and Sitting Fragmentation after a Workplace Sedentary Behaviour Intervention. Int. J. Environ. Res. Public Health 2018, 15, 1148. [Google Scholar] [CrossRef] [PubMed]
- Evans, R.E.; Fawole, H.O.; Sheriff, S.A.; Dall, P.M.; Grant, P.M.; Ryan, C.G. Point-of-choice prompts to reduce sitting time at work: A randomized trial. Am. J. Prev. Med. 2012, 43, 293–297. [Google Scholar] [CrossRef] [PubMed]
- Carr, L.J.; Karvinen, K.; Peavler, M.; Smith, R.; Cangelosi, K. Multicomponent intervention to reduce daily sedentary time: A randomised controlled trial. BMJ Open 2013, 3, e003261. [Google Scholar] [CrossRef] [PubMed]
- Koepp, G.A.; Manohar, C.U.; McCrady-Spitzer, S.K.; Ben-Ner, A.; Hamann, D.J.; Runge, C.F.; Levine, J.A. Treadmill desks: A 1-year prospective trial. Obesity 2013, 21, 705–711. [Google Scholar] [CrossRef] [PubMed]
- Tudor-Locke, C.; Schuna, J.M., Jr.; Frensham, L.J.; Proenca, M. Changing the way we work: Elevating energy expenditure with workstation alternatives. Int. J. Obes. 2014, 38, 755–765. [Google Scholar] [CrossRef] [PubMed]
- Levine, J.A.; Miller, J.M. The energy expenditure of using a “walk-and-work” desk for office workers with obesity. Br. J. Sports Med. 2007, 41, 558. [Google Scholar] [CrossRef] [PubMed]
- Wennberg, P.; Boraxbekk, C.-J.; Wheeler, M.; Howard, B.; Dempsey, P.C.; Lambert, G.; Eikelis, N.; Larsen, R.; Sethi, P.; Occleston, J.; et al. Acute effects of breaking up prolonged sitting on fatigue and cognition: A pilot study. BMJ Open 2016, 6, e009630. [Google Scholar] [CrossRef] [PubMed]
- Thorp, A.A.; Kingwell, B.A.; Owen, N.; Dunstan, D.W. Breaking up workplace sitting time with intermittent standing bouts improves fatigue and musculoskeletal discomfort in overweight/obese office workers. Occup. Environ. Med. 2014, 71, 765–771. [Google Scholar] [CrossRef] [PubMed]
- Bergouignan, A.; Legget, K.T.; De Jong, N.; Kealey, E.; Nikolovski, J.; Groppel, J.L.; Jordan, C.; O’Day, R.; Hill, J.O.; Bessesen, D.H. Effect of frequent interruptions of prolonged sitting on self-perceived levels of energy, mood, food cravings and cognitive function. Int. J. Behav. Nutr. Phys. Act. 2016, 13, 113. [Google Scholar] [CrossRef] [PubMed]
- Dunstan, D.W.; Kingwell, B.A.; Larsen, R.; Healy, G.N.; Cerin, E.; Hamilton, M.T.; Shaw, J.E.; Bertovic, D.A.; Zimmet, P.Z.; Salmon, J.; et al. Breaking Up Prolonged Sitting Reduces Postprandial Glucose and Insulin Responses. Diabetes Care 2012, 35, 976–983. [Google Scholar] [CrossRef] [PubMed]
- Peddie, M.C.; Bone, J.L.; Rehrer, N.J.; Skeaff, C.M.; Gray, A.R.; Perry, T.L. Breaking prolonged sitting reduces postprandial glycemia in healthy, normal-weight adults: A randomized crossover trial. Am. J. Clin. Nutr. 2013, 98, 358–366. [Google Scholar] [CrossRef] [PubMed]
- van Dijk, J.W.; Venema, M.; van Mechelen, W.; Stehouwer, C.D.; Hartgens, F.; van Loon, L.J. Effect of moderate-intensity exercise versus activities of daily living on 24-hour blood glucose homeostasis in male patients with type 2 diabetes. Diabetes Care 2013, 36, 3448–3453. [Google Scholar] [CrossRef] [PubMed]
- Blankenship, J.M.; Granados, K.; Braun, B. Effects of subtracting sitting versus adding exercise on glycemic control and variability in sedentary office workers. Appl. Physiol. Nutr. Metab. 2014, 39, 1286–1293. [Google Scholar] [CrossRef] [PubMed]
- Buckley, J.P.; Mellor, D.D.; Morris, M.; Joseph, F. Standing-based office work shows encouraging signs of attenuating post-prandial glycaemic excursion. Occup. Environ. Med. 2014, 71, 109–111. [Google Scholar] [CrossRef] [PubMed]
- Holmstrup, M.; Fairchild, T.; Keslacy, S.; Weinstock, R.; Kanaley, J. Multiple short bouts of exercise over 12-h period reduce glucose excursions more than an energy-matched single bout of exercise. Metab. Clin. Exp. 2014, 63, 510–519. [Google Scholar] [CrossRef] [PubMed]
- Bailey, D.P.; Locke, C.D. Breaking up prolonged sitting with light-intensity walking improves postprandial glycemia, but breaking up sitting with standing does not. J. Sci. Med. Sport 2015, 18, 294–298. [Google Scholar] [CrossRef] [PubMed]
- Larsen, R.N.; Kingwell, B.A.; Robinson, C.; Hammond, L.; Cerin, E.; Shaw, J.E.; Healy, G.N.; Hamilton, M.T.; Owen, N.; Dunstan, D.W. Breaking up of prolonged sitting over three days sustains, but does not enhance, lowering of postprandial plasma glucose and insulin in overweight and obese adults. Clin. Sci. 2015, 129, 117–127. [Google Scholar] [CrossRef] [PubMed]
- Dempsey, P.C.; Blankenship, J.M.; Larsen, R.N.; Sacre, J.W.; Sethi, P.; Straznicky, N.E.; Cohen, N.D.; Cerin, E.; Lambert, G.W.; Owen, N.; et al. Interrupting prolonged sitting in type 2 diabetes: Nocturnal persistence of improved glycaemic control. Diabetologia 2017, 60, 499–507. [Google Scholar] [CrossRef] [PubMed]
- Dempsey, P.C.; Larsen, R.N.; Sethi, P.; Sacre, J.W.; Straznicky, N.E.; Cohen, N.D.; Cerin, E.; Lambert, G.W.; Owen, N.; Kingwell, B.A.; et al. Benefits for Type 2 Diabetes of Interrupting Prolonged Sitting With Brief Bouts of Light Walking or Simple Resistance Activities. Diabetes Care 2016, 39, 964–972. [Google Scholar] [CrossRef] [PubMed]
- Hadgraft, N.T.; Lynch, B.M.; Clark, B.K.; Healy, G.N.; Owen, N.; Dunstan, D.W. Excessive sitting at work and at home: Correlates of occupational sitting and TV viewing time in working adults. BMC Public Health 2015, 15, 899. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.; Shin, W. How to Do Random Allocation (Randomization). Clin. Orthop. Surg. 2014, 6, 103–109. [Google Scholar] [CrossRef] [PubMed]
- Booth, M. Assessment of physical activity: An international perspective. Res. Q. Exerc. Sport 2000, 71, 114–120. [Google Scholar] [CrossRef] [PubMed]
- Grant, P.M.; Ryan, C.G.; Tigbe, W.W.; Granat, M.H. The validation of a novel activity monitor in the measurement of posture and motion during everyday activities. Br. J. Sports Med. 2006, 40, 992–997. [Google Scholar] [CrossRef] [PubMed]
- Godfrey, A.; Culhane, K.M.; Lyons, G.M. Comparison of the performance of the activPAL Professional physical activity logger to a discrete accelerometer-based activity monitor. Med. Eng. Phys. 2007, 29, 930–934. [Google Scholar] [CrossRef] [PubMed]
- Kozey-Keadle, S.; Libertine, A.; Lyden, K.; Staudenmayer, J.; Freedson, P.S. Validation of wearable monitors for assessing sedentary behavior. Med. Sci. Sports Exerc. 2011, 43, 1561–1567. [Google Scholar] [CrossRef] [PubMed]
- Ryan, C.G.; Grant, P.M.; Tigbe, W.W.; Granat, M.H. The validity and reliability of a novel activity monitor as a measure of walking. Br. J. Sports Med. 2006, 40, 779–784. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Li, H.; Keadle, S.; Matthews, C.E.; Carroll, R. PAactivPAL: Summarize Daily Physical Activity from ‘activPAL’ Accelerometer Data. Available online: https://rdrr.io/cran/PAactivPAL/ (accessed on 31 August 2018).
- Actigraph Support Center. What Is the Difference among the Energy Expenditure Algorithms? Available online: https://actigraph.desk.com/customer/en/portal/articles/2515835-what-is-the-difference-among-the-energy-expenditure-algorithms- (accessed on 5 May 2018).
- Sasaki, J.E.; John, D.; Freedson, P.S. Validation and comparison of ActiGraph activity monitors. J. Sci. Med. Sport 2011, 14, 411–416. [Google Scholar] [CrossRef] [PubMed]
- Tremblay, M.S.; Aubert, S.; Barnes, J.D.; Saunders, T.J.; Carson, V.; Latimer-Cheung, A.E.; Chastin, S.F.M.; Altenburg, T.M.; Chinapaw, M.J.M.; Altenburg, T.M.; et al. Sedentary Behavior Research Network (SBRN)—Terminology Consensus Project process and outcome. Int. J. Behav. Nutr. Phys. Act. 2017, 14, 75. [Google Scholar] [CrossRef] [PubMed]
- Reips, U.D.; Funke, F. Interval-level measurement with visual analogue scales in Internet-based research: VAS Generator. Behav. Res. Methods 2008, 40, 699–704. [Google Scholar] [CrossRef] [PubMed]
- McNair, D.M.; Lorr, M.; Droppleman, L.F. Manual Profile of Mood States; Educational & Industrial Testing Service: San Diego, CA, USA, 1971. [Google Scholar]
- Parry, S.; Straker, L. The contribution of office work to sedentary behaviour associated risk. BMC Public Health 2013, 13, 296. [Google Scholar] [CrossRef] [PubMed]
- Haskell, W.L.; Lee, I.M.; Pate, R.R.; Powell, K.E.; Blair, S.N.; Franklin, B.A.; Macera, C.A.; Heath, G.W.; Thompson, P.D.; Bauman, A. Physical activity and public health: Updated recommendation for adults from the American College of Sports Medicine and the American Heart Association. Med. Sci. Sports Exerc. 2007, 39, 1423–1434. [Google Scholar] [CrossRef] [PubMed]
- Hill, J.O. Understanding and addressing the epidemic of obesity: An energy balance perspective. Endocr. Rev. 2006, 27, 750–761. [Google Scholar] [CrossRef] [PubMed]
- Bergouignan, A.; Latouche, C.; Heywood, S.; Grace, M.S.; Reddy-Luthmoodoo, M.; Natoli, A.K.; Owen, N.; Dunstan, D.W.; Kingwell, B.A. Frequent interruptions of sedentary time modulates contraction- and insulin-stimulated glucose uptake pathways in muscle: Ancillary analysis from randomized clinical trials. Sci. Rep. 2016, 6, 32044. [Google Scholar] [CrossRef] [PubMed]
- Black, A.E. Physical activity levels from a meta-analysis of doubly labeled water studies for validating energy intake as measured by dietary assessment. Nutr. Rev. 1996, 54, 170–174. [Google Scholar] [CrossRef] [PubMed]
- Clemes, S.A.; O’Connell, S.E.; Edwardson, C.L. Office workers’ objectively measured sedentary behavior and physical activity during and outside working hours. J. Occup. Environ. Med. 2014, 56, 298–303. [Google Scholar] [CrossRef] [PubMed]
- Bessesen, D.; Bergouignan, A. Behavior Change Strategies for Increasing Exercise and Decreasing Sedentary Behaviors in Diabetes. In Diabetes and Exercise: From Pathophysiology to Clinical Implementation; Reusch, J.E.B., Regensteiner, J.G., Stewart, K.J., Veves, A., Eds.; Springer International Publishing: Cham, Switzerland, 2018; pp. 201–219. [Google Scholar]
- Clemes, S.A.; Parker, R.A. Increasing our understanding of reactivity to pedometers in adults. Med. Sci. Sports Exerc. 2009, 41, 674–680. [Google Scholar] [CrossRef] [PubMed]
- Behrens, T.K.; Dinger, M.K. Motion sensor reactivity in physically active young adults. Res. Q. Exerc. Sport 2007, 78, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Davis, R.E.; Loprinzi, P.D. Examination of Accelerometer Reactivity among a Population Sample of Children, Adolescents, and Adults. J. Phys. Act. Health 2016, 13, 1325–1332. [Google Scholar] [CrossRef] [PubMed]
| Parameters | Males | Females | All |
|---|---|---|---|
| n | 10 | 12 | 22 |
| Age (year) | 31.5 ± 7.4 | 32.0 ± 6.1 | 31.8 ± 6.6 |
| BMI (kg/m2) | 28.8 ± 2.9 | 31.7 ± 1.8 | 30.5 ± 2.7 |
| FM (kg) | 24.6 ± 4.3 *** | 36.0 ± 4.7 | 30.9 ± 7.3 |
| FFM (kg) | 63.1 ± 9.9 *** | 49.9 ± 5.0 | 56.0 ± 10.1 |
| FM (%) | 28.1 ± 2.4 *** | 41.8 ± 2.4 | 35.6 ± 7.4 |
| Self-reported sitting time (h/d) | 9.0 ± 3.2 | 10.6 ± 1.1 | 9.5 ± 4.1 |
| Physical Activity Outcomes | SED | ONE | MICRO | |||
|---|---|---|---|---|---|---|
| Non-work day | Work | Non-work day | Work | Non-work day | Work | |
| Sitting/lying (h/d) | 9.8 ± 2.0 | 10.6 ± 2.3 | 9.6 ± 1.9 | 10.2 ± 2.4 | 9.6 ± 2.5 | 10.5 ± 2.2 |
| Standing (h/d) | 3.5 ± 1.8 | 3.4 ± 1.8 | 3.0 ± 1.8 | 3.4 ± 1.5 | 3.6 ± 2.1 | 3.2 ± 1.9 |
| Stepping (h/d) | 1.4 ± 0.5 | 1.4 ± 0.5 | 1.7 ± 0.4 | 2.1 ± 0.5 *** | 1.7 ± 0.4 | 1.7 ± 0.7 **δ |
| Sitting (% waking time) | 66.6 ± 14.2 | 68.4 ± 13.5 | 67.2 ± 12.7 | 64.5 ± 10.4 | 64.0 ± 15.3 | 67.8 ± 14.1 |
| Standing (% waking time) | 23.9 ± 12.3 | 22.3 ± 11.6 | 20.7 ± 11.9 | 21.4 ±8.8 | 24.0 ± 14.5 | 20.7 ± 12.6 |
| Stepping (% waking time) | 9.4 ± 3.6 | 9.2 ±3.4 | 11.9 ± 2.4 | 13.9 ± 3.5 *** | 11.9 ± 2.9 | 11.4 ± 4.7 **δ |
| Sit-to-stand transitions (#) | 48.8 ± 15.1 | 47.2 ± 17.7 | 42.5 ± 13.6 | 50.1 ± 22.3 | 46.1 ± 12.4 | 50.7 ± 21.3 |
| Sitting bouts > 30-min (#) | 5.6 ± 1.7 | 6.2 ± 2.2 | 5.5 ± 1.7 | 6.1 ± 1.7 | 6.7 ± 2.7 *δ | 7.4 ± 2.7 |
| Sitting bouts > 60-min (#) | 3.1 ± 1.4 | 3.1 ± 1.5 | 2.6 ± 1.1 | 3.1 ± 1.6 | 2.3 ± 1.6 | 2.8 ± 2.0 |
| Step count (#) | 6409 ± 2843 | 7125 ± 2554 | 9376 ± 2387 ** | 12,257 ± 3149 *** | 9250 ± 2291 * | 10,036 ± 4262 **δδ |
| Parameters | SED | ONE | MICRO |
|---|---|---|---|
| Fasting glucose (mg/dL) | 90.1 ± 7.3 | 88.4 ± 7.7 | 88.7 ± 10.6 |
| Fasting insulin (uI/mL) | 10.8 ± 8.9 | 6.1 ± 3.0 * | 6.7 ± 6.1 * |
| I/G | 0.121 ± 0.101 | 0.069 ± 0.341 * | 0.075 ± 0.063 * |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
De Jong, N.P.; Debache, I.; Pan, Z.; Garnotel, M.; Lyden, K.; Sueur, C.; Simon, C.; Bessesen, D.H.; Bergouignan, A. Breaking up Sedentary Time in Overweight/Obese Adults on Work Days and Non-Work Days: Results from a Feasibility Study. Int. J. Environ. Res. Public Health 2018, 15, 2566. https://doi.org/10.3390/ijerph15112566
De Jong NP, Debache I, Pan Z, Garnotel M, Lyden K, Sueur C, Simon C, Bessesen DH, Bergouignan A. Breaking up Sedentary Time in Overweight/Obese Adults on Work Days and Non-Work Days: Results from a Feasibility Study. International Journal of Environmental Research and Public Health. 2018; 15(11):2566. https://doi.org/10.3390/ijerph15112566
Chicago/Turabian StyleDe Jong, Nathan P., Isaac Debache, Zhaoxing Pan, Mael Garnotel, Kate Lyden, Cédric Sueur, Chantal Simon, Daniel H. Bessesen, and Audrey Bergouignan. 2018. "Breaking up Sedentary Time in Overweight/Obese Adults on Work Days and Non-Work Days: Results from a Feasibility Study" International Journal of Environmental Research and Public Health 15, no. 11: 2566. https://doi.org/10.3390/ijerph15112566
APA StyleDe Jong, N. P., Debache, I., Pan, Z., Garnotel, M., Lyden, K., Sueur, C., Simon, C., Bessesen, D. H., & Bergouignan, A. (2018). Breaking up Sedentary Time in Overweight/Obese Adults on Work Days and Non-Work Days: Results from a Feasibility Study. International Journal of Environmental Research and Public Health, 15(11), 2566. https://doi.org/10.3390/ijerph15112566






