Investigating Motor Competence in Association with Sedentary Behavior and Physical Activity in 7- to 11-Year-Old Children
Abstract
:1. Introduction
2. Materials and Methods
2.1. Physical Activity and Sedentary Behavior
2.2. Anthropometry
2.3. Motor Competence
2.4. Procedure
2.5. Statistical Analyses
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Weggemans, R.M.; Backx, F.J.G.; Borghouts, L.; Chinapaw, M.; Hopman, M.T.E.; Koster, A.; Kremers, S.; van Loon, L.J.C.; May, A.; Mosterd, A.; et al. The 2017 Dutch Physical Activity Guidelines. Int. J. Behav. Nutr. Phys. Act. 2018, 15, 58. [Google Scholar] [CrossRef] [PubMed]
- Owen, N.; Sparling, P.B.; Healy, G.N.; Dunstan, D.W.; Matthews, C.E. Sedentary Behavior: Emerging Evidence for a New Health Risk. Mayo Clin. Proc. 2010, 85, 1138–1141. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hoare, E.; Milton, K.; Foster, C.; Allender, S. The associations between sedentary behaviour and mental health among adolescents: A systematic review. Int. J. Behav. Nutr. Phys. Act. 2016, 13, 108. [Google Scholar] [CrossRef] [PubMed]
- Jones, R.A.; Hinkley, T.; Okely, A.D.; Salmon, J. Tracking physical activity and sedentary behavior in childhood: A systematic review. Am. J. Prev. Med. 2013, 44, 651–658. [Google Scholar] [CrossRef] [PubMed]
- Telama, R. Tracking of Physical Activity from Childhood to Adulthood: A Review. Obesity Facts 2009, 2, 187–195. [Google Scholar] [CrossRef] [PubMed]
- Hallal, P.C.; Andersen, L.B.; Bull, F.C.; Guthold, R.; Haskell, W.; Ekelund, U. Global physical activity levels: Surveillance progress, pitfalls, and prospects. Lancet 2012, 380, 247–257. [Google Scholar] [CrossRef]
- Burghard, M.; Knitel, K.; van Oost, I.; Tremblay, M.S.; Takken, T. Is our Youth Cycling to Health? Results From the Netherlands’ 2016 Report Card on Physical Activity for Children and Youth. J. Phys. Act. Health 2016, 13, S218–S224. [Google Scholar] [CrossRef] [PubMed]
- Kremers, S.P.; de Bruijn, G.-J.; Visscher, T.L.; van Mechelen, W.; de Vries, N.K.; Brug, J. Environmental influences on energy balance-related behaviors: A dual-process view. Int. J. Behav. Nutr. Phys. Act. 2006, 3, 9. [Google Scholar] [CrossRef] [PubMed]
- De Meester, A.; Stodden, D.; Goodway, J.; True, L.; Brian, A.; Ferkel, R.; Haerens, L. Identifying a motor proficiency barrier for meeting physical activity guidelines in children. J. Sci. Med. Sport 2018, 21, 58–62. [Google Scholar] [CrossRef] [PubMed]
- Lubans, D.R.; Morgan, P.J.; Cliff, D.P.; Barnett, L.M.; Okely, A.D. Fundamental Movement Skills in Children and Adolescents. Sports Med. 2010, 40, 1019–1035. [Google Scholar] [CrossRef] [PubMed]
- Wormhoudt, R.; Savelsbergh, G.; Teunissen, J.; Davids, K. The Athletic Skills Model; Routledge: Abingdon, UK, 2018. [Google Scholar]
- Runhaar, J.; Collard, D.C.M.; Singh, A.S.; Kemper, H.C.G.; van Mechelen, W.; Chinapaw, M. Motor fitness in Dutch youth: Differences over a 26-year period (1980–2006). J. Sci. Med. Sport 2010, 13, 323–328. [Google Scholar] [CrossRef] [PubMed]
- Tester, G.; Ackland, T.R.; Houghton, L. A 30-Year Journey of Monitoring Fitness and Skill Outcomes in Physical Education: Lessons Learned and a Focus on the Future. J. Adv. Phys. Educ. 2014, 4, 11. [Google Scholar] [CrossRef]
- Roetert, E.P.; Ellenbecker, T.S.; Kriellaars, D. Physical literacy: Why should we embrace this construct? Br. J. Sports Med. 2018. [Google Scholar] [CrossRef] [PubMed]
- Stodden, D.F.; Goodway, J.D.; Langendorfer, S.J.; Roberton, M.A.; Rudisill, M.E.; Garcia, C.; Garcia, L.E. A developmental perspective on the role of motor skill competence in physical activity: An emergent relationship. Quest 2008, 60, 290–306. [Google Scholar] [CrossRef]
- Lima, R.A.; Pfeiffer, K.; Larsen, L.R.; Bugge, A.; Moller, N.C.; Anderson, L.B.; Stodden, D.F. Physical Activity and Motor Competence Present a Positive Reciprocal Longtiudinal Relationship Across Children and Early Adolescence. J. Phys. Act. Health 2017, 14, 440–447. [Google Scholar] [CrossRef] [PubMed]
- Da Costa, B.G.G.; Da Silva, K.S.; George, A.M.; De Assis, M.A.A. Sedentary behavior during school-time: Sociodemographic, weight status, physical education class, and school performance correlates in Brazilian schoolchildren. J. Sci. Med. Sport 2017, 20, 70–74. [Google Scholar] [CrossRef] [PubMed]
- Keane, E.; Li, X.; Harrington, J.M.; Fitzgerald, A.P.; Perry, I.J.; Kearney, P.M. Physical Activity, Sedentary Behavior and the Risk of Overweight and Obesity in School-Aged Children. Pediatr. Exerc. Sci. 2017, 29, 408–418. [Google Scholar] [CrossRef] [PubMed]
- Okely, A.D.; Booth, M.L.; Chey, T. Relationships between Body Composition and Fundamental Movement Skills among Children and Adolescents. Res. Q. Exerc. Sport 2004, 75, 238–247. [Google Scholar] [CrossRef] [PubMed]
- Foweather, L.; Knowles, Z.; Ridgers, N.D.; O’Dwyer, M.V.; Foulkes, J.D.; Stratton, G. Fundamental movement skills in relation to weekday and weekend physical activity in preschool children. J. Sci. Med. Sport 2015, 18, 691–696. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Slykerman, S.; Ridgers, N.D.; Stevenson, C.; Barnett, L.M. How important is young children’s actual and perceived movement skill competence to their physical activity? J. Sci. Med. Sport 2016, 19, 488–492. [Google Scholar] [CrossRef] [PubMed]
- Telford, R.M.; Telford, R.D.; Olive, L.S.; Cochrane, T.; Davey, R. Why Are Girls Less Physically Active than Boys? Findings from the LOOK Longitudinal Study. PLoS ONE 2016, 11, e0150041. [Google Scholar] [CrossRef] [PubMed]
- Ishii, K.; Shibata, A.; Adachi, M.; Nonoue, K.; Oka, K. Gender and grade differences in objectively measured physical activity and sedentary behavior patterns among Japanese children and adolescents: A cross-sectional study. BMC Public Health 2015, 15, 1254. [Google Scholar] [CrossRef] [PubMed]
- Pearce, M.S.; Basterfield, L.; Mann, K.D.; Parkinson, K.N.; Adamson, A.J.; Reilly, J.J. Early predictors of objectively measured physical activity and sedentary behaviour in 8-10 year old children: The Gateshead Millennium Study. PLoS ONE 2012, 7, e37975. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wang, C.; Chen, P.; Zhuang, J. A National Survey of Physical Activity and Sedentary Behavior of Chinese City Children and Youth Using Accelerometers. Res. Q. Exerc. Sport 2013, 84, 2. [Google Scholar] [CrossRef] [PubMed]
- Farooq, M.A.; Parkinson, K.N.; Adamson, A.J.; Pearce, M.S.; Reilly, J.K.; Hughes, A.R.; Janssen, X.; Basterfield, L.; Reilly, J.J. Timing of the decline in physical activity in childhood and adolescence: Gateshead Millennium Cohort Study. Br. J. Sports Med. 2017. [Google Scholar] [CrossRef] [PubMed]
- Trost, S.G.; Pate, R.R.; Sallis, J.F.; Freedson, P.S.; Taylor, W.C.; Dowda, M.; Sirard, J. Age and gender differences in objectively measured physical activity in youth. Med. Sci. Sports Exerc. 2002, 34, 350–355. [Google Scholar] [CrossRef] [Green Version]
- Van Kann, D.H.H.; Kremers, S.P.J.; de Vries, N.K.; de Vries, S.I.; Jansen, M.W.J. The effect of a school-centered multicomponent intervention on daily physical activity and sedentary behavior in primary school children: The Active Living study. Prev. Med. 2016, 89, 64–69. [Google Scholar] [CrossRef] [PubMed]
- Evenson, K.R.; Catellier, D.J.; Gill, K.; Ondrak, K.S.; McMurray, R.G. Calibration of two objective measures of physical activity for children. J. Sports Sci. 2008, 26, 1557–1565. [Google Scholar] [CrossRef] [PubMed]
- Choi, L.; Liu, Z.; Matthews, C.E.; Buchowski, M.S. Validation of Accelerometer Wear and Nonwear Time Classification Algorithm. Med. Sci. Sports Exerc. 2011, 43, 357–364. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dössegger, A.; Ruch, N.; Jimmy, G.; Braun-Fahrländer, C.; Mäder, U.; Hänggi, J.; Hofmann, H.; Puder, J.J.; Kriemler, S.; Bringolf-Isler, B. Reactivity to Accelerometer Measurement of Children and Adolescents. Med. Sci. Sports Exerc. 2014, 46, 1140–1146. [Google Scholar] [CrossRef] [Green Version]
- Schönbeck, Y.; Talma, H.; van Dommelen, P.; Bakker, B.; Buitendijk, S.E.; HiraSing, R.A.; van Buuren, S. Increase in Prevalence of Overweight in Dutch Children and Adolescents: A Comparison of Nationwide Growth Studies in 1980, 1997 and 2009. PLoS ONE 2011, 6, e27608. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Barlow, S.E. Expert Committee Recommendations Regarding the Prevention, Assessment, and Treatment of Child and Adolescent Overweight and Obesity: Summary Report. Pediatrics 2007, 120, S164. [Google Scholar] [CrossRef] [PubMed]
- D’Hondt, E.; Deforche, B.; De Bourdeaudhuij, I.; Lenoir, M. Relationship between Motor Skill and Body Mass Index in 5- to 10-Year-Old Children. Adapt. Phys. Act. Q. 2009, 26, 21–37. [Google Scholar] [CrossRef]
- Hoeboer, J.; Krijger-Hombergen, M.; Savelsbergh, G.; De Vries, S. Reliability and concurrent validity of a motor skill competence test among 4- to 12-year old children. J. Sports Sci. 2018, 36, 1607–1613. [Google Scholar] [CrossRef] [PubMed]
- Hoeboer, J.J.A.A.M.; Ongena, G.; Krijger-Hombergen, M.; Stolk, E.; Savelsbergh, G.J.P.; de Vries, S.I. The Athletic Skills Track: Age- and gender-related normative values of a motor skills test for 4- to 12-year-old children. J. Sci. Med. Sport 2018, 21, 975–979. [Google Scholar] [CrossRef] [PubMed]
- Barnett, L.M.; Lai, S.K.; Veldman, S.L.C.; Hardy, L.L.; Cliff, D.P.; Morgan, P.J.; Zask, A.; Lubans, D.R.; Shultz, S.P.; Ridgers, N.D.; et al. Correlates of Gross Motor Competence in Children and Adolescents: A Systematic Review and Meta-Analysis. Sports Med. 2016, 46, 1663–1688. [Google Scholar] [CrossRef] [PubMed]
- Castelli, D.M.; Valley, J.A. Chapter 3: The Relationship of Physical Fitness and Motor Competence to Physical Activity. J. Teach. Phys. Educ. 2007, 26, 358–374. [Google Scholar] [CrossRef]
- Fisher, A.; Reilly, J.J.; Kelly, L.A.; Montgomery, C.; Williamson, A.; Paton, J.Y.; Grant, S. Fundamental movement skills and habitual physical activity in young children. Med. Sci. Sports Exerc. 2005, 37, 684–688. [Google Scholar] [CrossRef] [PubMed]
- Cohen, K.E.; Morgan, P.J.; Plotnikoff, R.C.; Callister, R.; Lubans, D.R.J.I.J.o.B.N.; Activity, P. Fundamental movement skills and physical activity among children living in low-income communities: A cross-sectional study. Int. J. Behav. Nutr. Phys. Act. 2014, 11, 49. [Google Scholar] [CrossRef] [PubMed]
- Wrotniak, B.H.; Epstein, L.H.; Dorn, J.M.; Jones, K.E.; Kondilis, V.A. The Relationship Between Motor Proficiency and Physical Activity in Children. Pediatrics 2006, 118, e1758–e1765. [Google Scholar] [CrossRef] [PubMed]
- Lopes, L.; Santos, R.; Pereira, B.; Lopes, V.P. Associations between sedentary behavior and motor coordination in children. Am. J. Hum. Biol. 2012, 24, 746–752. [Google Scholar] [CrossRef] [PubMed]
- Hardy, L.L.; Reinten-Reynolds, T.; Espinel, P.; Zask, A.; Okely, A.D. Prevalence and Correlates of Low Fundamental Movement Skill Competency in Children. Pediatrics 2012, 130, e390–e398. [Google Scholar] [CrossRef] [PubMed]
- Loprinzi, P.D.; Davis, R.E.; Fu, Y.-C. Early motor skill competence as a mediator of child and adult physical activity. Prev. Med. Rep. 2015, 2, 833–838. [Google Scholar] [CrossRef] [PubMed]
- Engel, A.C.; Broderick, C.R.; van Doorn, N.; Hardy, L.L.; Parmenter, B.J.J.S.M. Exploring the Relationship Between Fundamental Motor Skill Interventions and Physical Activity Levels in Children: A Systematic Review and Meta-analysis. Sports Med. 2018, 48, 1845–1857. [Google Scholar] [CrossRef] [PubMed]
- Barnett, L.M.; Hardy, L.L.; Lubans, D.R.; Cliff, D.P.; Okely, A.D.; Hills, A.P.; Morgan, P.J.; Physical Activity and Sedentary Behaviour Stream of the Australasian Child and Adolescent Obesity Research Network. Australian children lack the basic movement skills to be active and healthy. Health Promot. J. Austr. 2013, 24, 82–84. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Verjans-Janssen, S.R.B.; van de Kolk, I.; Van Kann, D.H.H.; Kremers, S.P.J.; Gerards, S.M.P.L. Effectiveness of school-based physical activity and nutrition interventions with direct parental involvement on children’s BMI and energy balance-related behaviors—A systematic review. PLoS ONE 2018, 13, e0204560. [Google Scholar] [CrossRef] [PubMed]
- Verloigne, M.; Lippevelde, W.; Maes, L.; Yıldırım, M.; Chinapaw, M.; Manios, Y.; Androutsos, O.; Kovacs, E.; Bringolf-Isler, B.; Brug, J.; et al. Levels of physical activity and sedentary time among 10- to 12-year-old boys and girls across 5 European countries using accelerometers: An observational study within the ENERGY-project. Int. J. Behav. Nutr. Phys. Act. 2012, 9. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Telford, R.M.; Telford, R.D.; Cunningham, R.B.; Cochrane, T.; Davey, R.; Waddington, G. Longitudinal patterns of physical activity in children aged 8 to 12 years: The LOOK study. Int. J. Behav. Nutr. Phys. Act. 2013, 10, 81. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization (WHO). Physical activity in adolescents. In Health Behaviour in School-aged Children Study 2013-2014; World Health Organization—Europe Vol. Factsheet, WHO: Geneva, Switzerland, 15 March 2016. [Google Scholar]
- Barnes, J.D.; Colley, R.C.; Borghese, M.; Janson, K.; Fink, A.; Tremblay, M.S. Results from the Active Healthy Kids Canada 2012 Report Card on Physical Activity for Children and Youth. Pediatr. Child. Health 2013, 18, 301–304. [Google Scholar] [CrossRef]
- Konstabel, K.; Veidebaum, T.; Verbestel, V.; Moreno, L.A.; Bammann, K.; Tornaritis, M.; Eiben, G.; Molnár, D.; Siani, A.; Sprengeler, O.; et al. Objectively measured physical activity in European children: The IDEFICS study. Int. J. Obes. 2014, 38, S135. [Google Scholar] [CrossRef] [PubMed]
- Brittin, J.; Frerichs, L.; Sirard, J.R.; Wells, N.M.; Myers, B.M.; Garcia, J.; Sorensen, D.; Trowbridge, M.J.; Huang, T. Impacts of active school design on school-time sedentary behavior and physical activity: A pilot natural experiment. PLoS ONE 2017, 12, e189236. [Google Scholar] [CrossRef] [PubMed]
- Kriemler, S.; Meyer, U.; Martin, E.; van Sluijs, E.M.F.; Andersen, L.B.; Martin, B.W. Effect of school-based interventions on physical activity and fitness in children and adolescents: A review of reviews and systematic update. Br. J. Sports Med. 2011, 45, 923. [Google Scholar] [CrossRef] [PubMed]
- Hegarty, L.M.; Mair, J.L.; Kirby, K.; Murtagh, E.; Murphy, M.H. School-based Interventions to Reduce Sedentary Behaviour in Children: A Systematic Review. AIMS Public Health 2016, 3, 520–541. [Google Scholar] [CrossRef] [PubMed]
- Atkin, A.J.; Sharp, S.J.; Harrison, F.L.O.; Brage, S.; Van Sluijs, E.M.F. Seasonal Variation in Children’s Physical Activity and Sedentary Time. Med. Sci. Sports Exerc. 2016, 48, 449–456. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bürgi, R.; de Bruin, E.D. Differences in Spatial Physical Activity Patterns between Weekdays and Weekends in Primary School Children: A Cross-sectional Study Using Accelerometry and Global Positioning System. Sports 2016, 4, 36. [Google Scholar] [CrossRef] [PubMed]
| Schoolday | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Total Mean (SD) N = 595 | Boys Mean (SD) N = 291 | Girls Mean (SD) N = 304 | Boys–Girls p (t) | Grade 4 Mean (SD) N = 288 | Grade 6 Mean (SD) N = 307 | Grade 4-Grade 6 p (t) | Non-Overweight Mean (SD) N = 528 | Overweight Mean (SD) N = 67 | Non-Overweight-Overweight p (t) | |
| Age | 9.1 (1.1) | 9.1 (1.1) | 9.2 (1.1) | ns | 8.1 (0.4) | 10.1 (0.5) | <0.01 (−57.54) | 9.1 (1.1) | 9.1 (1.1) | ns |
| MC | 3.18 (1.01) | 3.25 (1.07) | 3.12 (0.95) | ns | 3.49 (0.92) | 2.90 (1.01) | <0.01 (7.36) | 3.23 (1.0) | 2.85 (0.9) | <0.01 (2.88) |
| BMI (z-score) * | −0.22 (0.96) | −0.27 (1.01) | −0.17 (0.92) | ns | −0.19 (0.92) | −0.24 (1.00) | ns | −0.44 (0.77) | 1.52 (0.44) | <0.01 (−30.71) |
| Wear time | 766.4 (64.7) | 766.6 (64.3) | 766.2 (65.3) | ns | 752.5 (62.8) | 779.5 (63.9) | <0.01 (−5.19) | 767.4 (64.2) | 758.3 (68.6) | ns |
| % SB | 62.6 (6.4) | 60.9 (6.7) | 64.2 (5.6) | <0.01 (6.56) | 60.5 (6.2) | 64.5 (6.0) | <0.01 (−7.83) | 62.6 (6.2) | 62.6 (7.8) | ns |
| % LPA | 29.8 (4.9) | 30.4 (5.1) | 29.2 (4.6) | <0.01 (−3.04) | 31.6 (4.5) | 28.2 (4.6) | <0.01 (9.25) | 29.8 (4.7) | 30.4 (5.9) | ns |
| % MVPA | 7.6 (2.7) | 8.7 (2.8) | 6.6 (2.1) | <0.01 (−10.57) | 7.9 (2.7) | 7.4 (2.7) | <0.05 (2.19) | 7.7 (2.7) | 7.0 (2.6) | <0.05 (2.11) |
| Data (N = 622) | % SB | % LPA | % MVPA | |||
|---|---|---|---|---|---|---|
| Beta (95% CI) | p | Beta (95% CI) | p | Beta (95% CI) | p | |
| Age | 1.46 (1.02–1.90) | <0.01 | −1.42 (−1.76–−1.08) | <0.01 | −0.04 (−0.23–0.14) | 0.64 |
| BMI-z score | −0.26 (−0.73–0.21) | 0.28 | 0.37 (−0.01–0.74) | <0.05 | −0.11 (−0.31–0.08) | 0.26 |
| Gender (ref = female) | −3.25 (−4.15–−2.35) | <0.01 | 1.19 (0.49–1.89) | <0.01 | 2.06 (1.69–2.44) | <0.01 |
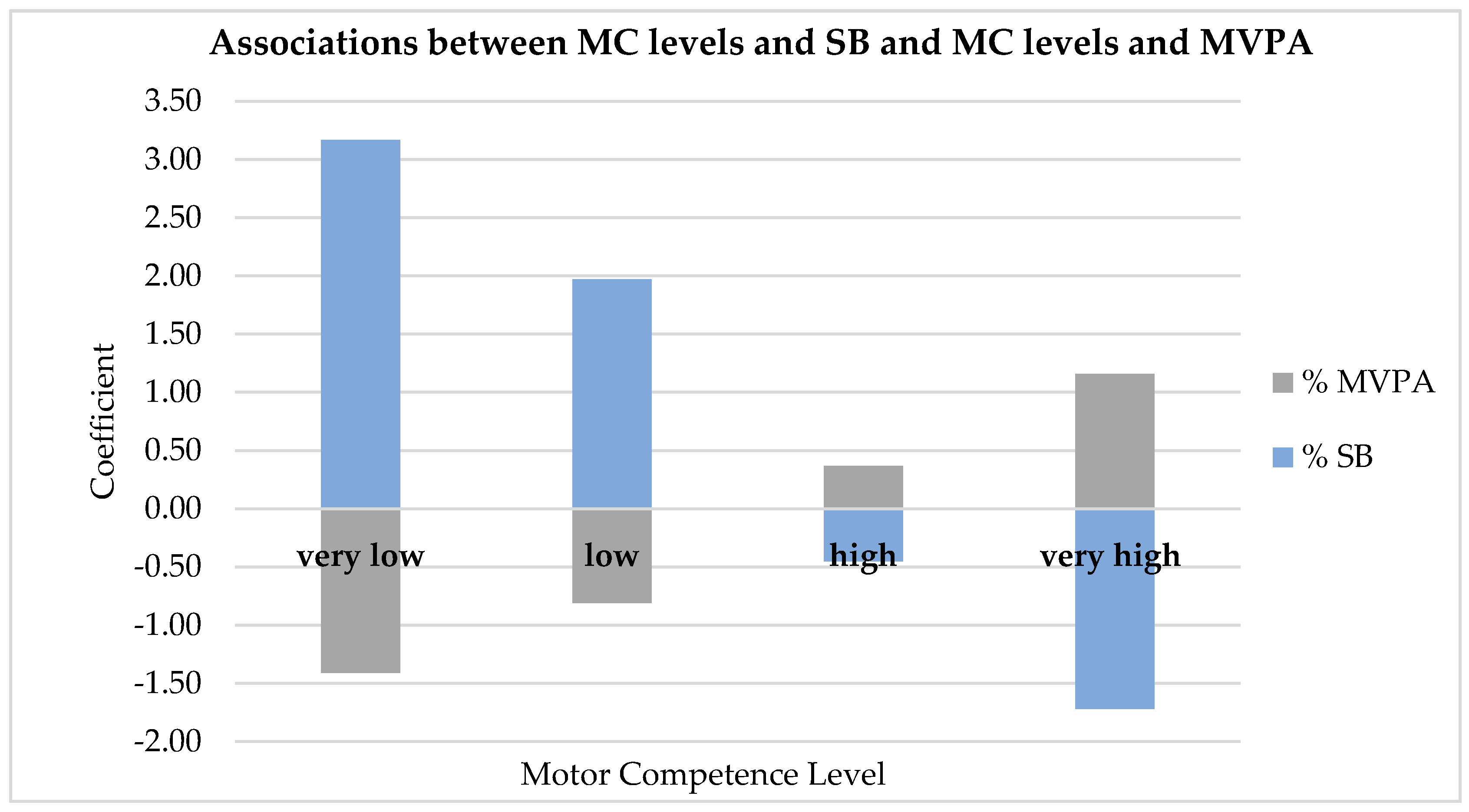
| Motor Competence (ref = average) | ||||||
| Very low | 3.17 (1.28–5.05) | <0.01 | −1.75 (−3.21–−0.29) | <0.05 | −1.41 (−2.19–−0.63) | <0.01 |
| Low | 1.97 (0.44–3.49) | <0.05 | −1.15 (−2.34–0.03) | 0.06 | −0.81 (−1.44–−0.18) | <0.05 |
| High | −0.45 (−1.71–0.81) | 0.48 | 0.08 (−.90–1.06) | 0.87 | 0.37 (−0.16–0.89) | 0.17 |
| Very high | −1.72 (−3.18–−0.27) | <0.05 | 0.56 (−0.57–1.69) | 0.33 | 1.16 (0.56–1.76) | <0.01 |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
M. Adank, A.; H. H. Van Kann, D.; A. A. Hoeboer, J.J.; I. de Vries, S.; P. J. Kremers, S.; B. Vos, S. Investigating Motor Competence in Association with Sedentary Behavior and Physical Activity in 7- to 11-Year-Old Children. Int. J. Environ. Res. Public Health 2018, 15, 2470. https://doi.org/10.3390/ijerph15112470
M. Adank A, H. H. Van Kann D, A. A. Hoeboer JJ, I. de Vries S, P. J. Kremers S, B. Vos S. Investigating Motor Competence in Association with Sedentary Behavior and Physical Activity in 7- to 11-Year-Old Children. International Journal of Environmental Research and Public Health. 2018; 15(11):2470. https://doi.org/10.3390/ijerph15112470
Chicago/Turabian StyleM. Adank, Anoek, Dave H. H. Van Kann, Joris J. A. A. Hoeboer, Sanne I. de Vries, Stef P. J. Kremers, and Steven B. Vos. 2018. "Investigating Motor Competence in Association with Sedentary Behavior and Physical Activity in 7- to 11-Year-Old Children" International Journal of Environmental Research and Public Health 15, no. 11: 2470. https://doi.org/10.3390/ijerph15112470
APA StyleM. Adank, A., H. H. Van Kann, D., A. A. Hoeboer, J. J., I. de Vries, S., P. J. Kremers, S., & B. Vos, S. (2018). Investigating Motor Competence in Association with Sedentary Behavior and Physical Activity in 7- to 11-Year-Old Children. International Journal of Environmental Research and Public Health, 15(11), 2470. https://doi.org/10.3390/ijerph15112470





