WHO European Childhood Obesity Surveillance Initiative: School Nutrition Environment and Body Mass Index in Primary Schools
Abstract
:1. Introduction
2. Methods
2.1. COSI Project
2.2. Sampling of Schools and Children
2.3. School Nutrition Environment Score (Proxy Indicator)
2.4. School BMI-for-Age Z-Score (Proxy Indicator)
2.5. Statistical Analyses
3. Results and Discussion
3.1. Results
3.1.1. School Environment Characteristics on Nutrition and Physical Activity
| Characteristics | BGR | CZE | IRL | LVA | LTU | MLT | NOR | PRT | SVN | SWE |
|---|---|---|---|---|---|---|---|---|---|---|
| Number of schools (n) | 179 | 548 | 154 | 190 | 155 | 95 | 127 | 176 | 118 | 89 |
| Availability at school (%) | ||||||||||
| Food Items that Can be Obtained on the School Premises | ||||||||||
| 1 Fresh fruit † | 36.9 a,b | 55.5 c | 22.7 a | 52.6 b,c | 72.9 d,e | 22.1 a | 70.1 c,d,e | 35.2 a,b | 75.0 §,e | 65.2 c,d,e |
| 2 Vegetables † | 17.9 a,b | 48.2 c | 3.9 d | 40.5 c,e | 80.7 f | 11.6 a,d | 48.0 c,e | 25.6 a,b,e | 36.4 b,c,e | 88.8 f |
| 3 100% fruit juice without sugar † | 19.0 a,b | 25.7 a,b | 4.6 c | 21.6 a,b | 54.2 d | 11.6 a,c | 15.0 a,c | 4.0 c | 39.0 b,d | 11.2 a,c |
| 4 Fruit juice containing sugar † | 69.3 a | 51.6 b | 4.6 c,d | 48.4 b | 63.2 a,b | 7.4 c,d | 0.0 c | 5.7 c,d | 19.5 d | 1.1 c |
| 5 Cold drinks without sugar † | 33.0 a,b | 43.3 a | 2.6 c,d | 36.3 a,b | 49.0 a | 3.2 c,d | 0.0 §,c | 1.1 c | 42.4 a,b | 20.2 b,d |
| 6 Cold drinks containing sugar † | 68.2 a | 56.6 a,b | 0.7 c | 40.5 b | 70.3 a | 2.1 c | 0.0 §,c | 2.8 c | 40.7 b | 6.7 c |
| 7 Hot drinks without sugar † | 43.6 a | 30.8 a | 0.0 b | 36.8 a | 46.5 a | 0.0 b | 0.0 §,b | 5.1 b | 40.7 a | 3.4 b |
| 8 Hot drinks containing sugar † | 57.5 a | 55.7 a | 0.0 b | 42.6 a,c | 87.1 d | 1.1 b | 0.0 §,b | 3.4 b | 28.0 c | 5.6 b |
| 9 Diet or “light” soft drinks † | 27.4 a,b | 18.6 a | 0.0 c | 37.9 b | 14.2 a,d | 3.2 c,d | 0.0 §,c | 0.6 c | 26.5 §,a,b | 3.4 c,d |
| 10 Milk † | 33.5 a | 57.7 b | 33.1 a | 42.1 a,b | 42.6 a,b | 59.0 b,c | 95.3 d | 77.3 c,e | 94.9 d | 86.5 d,e |
| 11 Flavoured milk † | 21.8 a,b | 54.0 c | 1.3 d | 15.8 a | 18.1 a,b | 2.1 d | 38.6 b,c | 35.8 b | 23.7 a,b | 12.5 §,a,d |
| 12 Water † | 67.6 a,b | 54.2 a | 46.1 a | 57.4 a,b | 76.8 b | 47.4 a | 99.2 c | 55.1 a | 44.1 a | 95.5 c |
| 13 Yoghurt † | 37.4 a | 54.7 b,c | 13.0 d | 37.4 a | 70.3 b | 11.6 d | 15.8 d,e | 21.0 a,d,e | 34.8 a,c,e | 25.8 a,d,e |
| 14 Sweet snacks † | 76.5 a | 45.6 b | 0.7 c | 51.1 b,d | 69.0 a,d | 8.4 c | 0.0 c | 9.1 c | 3.4 c | 3.4 c |
| 15 Salted snacks † | 73.7 a | 18.6 b | 0.0 c | 14.7 b,d | 22.6 b | 1.1 c | 0.0 c | 3.4 c,d | 9.3 b,c,d | 2.3 c |
| Physical Activity-Related Characteristics | ||||||||||
| 16 Availability of outside playgrounds or inside play areas where children can play during school breaks † | 99.4 §,a | 78.4 §,b | 98.7 a,c | 92.6 a,c,d | 88.2 §,b,c | 100.0 a | 100.0 a | 98.3 §,a,c | 82.1 §,b,d | 100.0 §,a |
| 17 Provision of ≥60 min per week of physical education to pupils from participating classes † | 99.4 §,a | 97.9 §,a,b | 92.9 a,b | 99.5 a | 99.3 §,a | 83.2 b | 92.9 §,a,b | 90.7 §,a,b | 100.0 a | 76.2 §,b |
| General Characteristic | ||||||||||
| 18 Any initiatives/projects organized to promote a healthy lifestyle among pupils from participating classes † | 42.4 §,a | 87.7 §,b | 88.3 b,c | 96.8 c | 54.2 §,a | 89.5 b,c | 62.0 §,a | 64.3 §,a | 61.5 §,a | 89.7 §,b,c |
| Characteristics | CZE | GRC | HUN | IRL | LVA | LTU | NOR | PRT | SVN |
|---|---|---|---|---|---|---|---|---|---|
| Number of schools (n) | 882 | 123 | 98 | 154 | 169 | 160 | 125 | 167 | 167 |
| Availability at school (%) | |||||||||
| Food Items that Can be Obtained on the School Premises | |||||||||
| 1 Fresh fruit † | 47.1 a | 12.2 b | 82.7 c,d | 24.0 b | 53.9 a,e | 67.5 c,e | 67.2 c,e | 64.1 c,e | 95.2 d |
| 2 Vegetables † | 39.0 a | 4.9 b | 23.5 a | 4.6 b | 44.4 a,c | 72.5 d | 37.6 a,c | 27.0 a | 56.9 c,d |
| 3 100% fruit juice without sugar † | 18.3 a | 46.3 b,c | 29.6 a,b | 7.1 d,e | 20.1 a,d | 63.1 c | 17.6 a,d | 2.4 e | 22.2 a,d |
| 4 Fruit juice containing sugar † | 30.7 a | 32.5 a,b | 52.0 b,c | 4.6 d | 47.3 b,c | 59.4 c | 0.0 d | 3.6 d | 35.9 a,b |
| 5 Cold drinks without sugar † | 27.7 a | 12.2 b,c | 28.6 a,b | 1.3 c,d | 34.3 a | 42.5 a | 0.0 §,d | 1.8 c,d | 28.1 a,b |
| 6 Cold drinks containing sugar † | 35.8 a | 11.4 b,c | 49.0 a,d | 0.0 e | 42.0 a | 68.1 d | 0.0 §,e | 1.8 b,e | 28.7 a,c |
| 7 Hot drinks without sugar † | 19.7 a | 6.5 b,c | 17.4 a,b | 0.7 c | 37.9 d | 50.0 d | 0.0 §,c | 3.6 b,c | 31.7 a,d |
| 8 Hot drinks containing sugar † | 37.6 a | 7.3 b | 40.8 a | 0.0 b | 46.8 a | 77.5 c | 0.0 §,b | 4.2 b | 48.5 a |
| 9 Diet or “light” soft drinks † | 8.5 a | 3.3 a,b | 20.4 a,c | 0.0 b | 27.8 c | 6.3 a,b | 0.0 §,b | 1.2 b | 4.2 a,b |
| 10 Milk † | 40.9 a | 17.9 b | 38.8 a,b | 35.7 a,b | 27.2 a,b | 39.4 a | 95.2 c | 95.8 c | 91.6 c |
| 11 Flavoured milk † | 36.7 a | 18.7 b | 32.7 a,b | 3.3 c | 18.3 b | 15.6 b,c | 43.2 a | 41.9 a | 18.6 b |
| 12 Water † | 35.5 a | 56.1 b | 62.2 b | 50.7 a,b | 55.0 b | 68.1 b | 99.2 c | 47.3 a,b | 3.0 d |
| 13 Yoghurt † | 35.2 a | 4.9 b | 28.6 a,c | 13.6 b,c | 37.3 a | 70.0 d | 13.6 b,c | 15.6 b,c | 29.3 a,c |
| 14 Sweet snacks † | 26.8 a | 17.9 a,b | 51.0 c | 1.3 d | 48.5 c | 60.0 c | 0.0 d | 4.8 b,d | 4.8 b,d |
| 15 Salted snacks † | 12.2 a | 13.8 a,b | 36.7 c | 1.3 §,b,d | 11.2 a,b | 20.6 a,c | 0.0 d | 1.2 b,d | 0.0 d |
| Physical Activity-Related Characteristics | |||||||||
| 16 Availability of outside playgrounds or inside play areas where children can play during school breaks † | 78.2 §,a | 98.1 §,b | 81.4 §,a,c | 100.0 §,b | 94.0 §,b,c | 90.9 §,b,c | 100.0 b | 99.4 §,b | 83.2 a,c |
| 17 Provision of ≥60 min per week of physical education to pupils from participating classes † | 98.5 §,a,b | 95.4 §,a,b | 100.0 §,a | 88.2 §,b | 98.8 a,b | 100.0 §,a | 95.8 §,a,b | 91.5 §,a,b | 100.0 a |
| General Characteristic | |||||||||
| 18 Any initiatives/projects organized to promote a healthy lifestyle among pupils from participating classes † | 87.0 §,a | 42.3 §,b | 88.4 §,a | 93.5 §,a | 95.2 a | 50.4 §,b | 58.1 §,b | 92.0 §,a | 84.4 a |
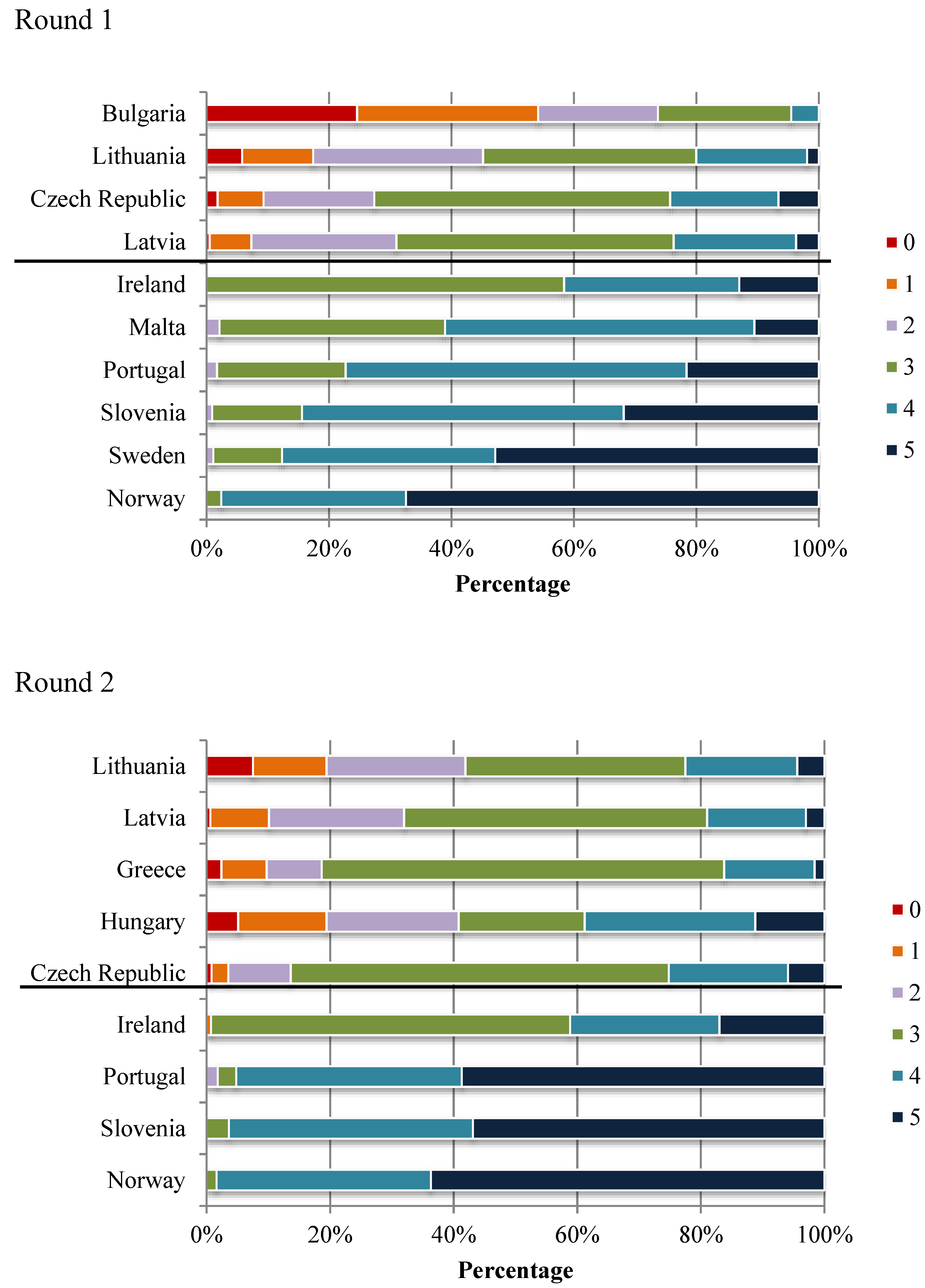
3.1.2. School Nutrition Environment Score
| Countries | Number of Schools | School Nutrition Environment Score | ||
|---|---|---|---|---|
| n | Mean ± SD (CV (%)) | |||
| Round 1 | Round 2 | Round 1 † | Round 2 † | |
| Same Schools in Both Rounds | ||||
| Ireland | 154 | 153 | 0.71 ± 0.14 a (20.2) | 0.71 ± 0.16 a (22.2) |
| Lithuania | 155 | 160 | 0.51 ± 0.23 b (45.2) | 0.52 ± 0.25 b (48.5) |
| Norway | 126 | 124 | 0.93 ± 0.11 c (11.3) | 0.92 ± 0.10 c (11.2) |
| Portugal § | 176 | 167 | 0.79 ± 0.14 d,e (17.7) | 0.90 ± 0.13 c (14.3) |
| New Sample of Schools in Both Rounds | ||||
| Bulgaria | 179 | – | 0.30 ± 0.24 f (79.3) | – |
| Czech Republic § | 548 | 882 | 0.58 ± 0.21 g (35.5) | 0.63 ± 0.17 d (26.6) |
| Greece | – | 123 | – | 0.57 ± 0.18 b,d (31.2) |
| Hungary | – | 98 | – | 0.57 ± 0.28 b,d (49.3) |
| Latvia | 190 | 169 | 0.58 ± 0.19 b,g (32.8) | 0.56 ± 0.19 b (33.8) |
| Malta | 95 | – | 0.74 ± 0.14 a,d (18.5) | – |
| Slovenia § | 116 | 167 | 0.83 ± 0.14 e,h (16.7) | 0.91 ± 0.11 c (12.5) |
| Sweden | 89 | – | 0.88 ± 0.15 c,h (16.7) | – |
3.1.3. School BMI/A Z-Score
3.2. Discussion
3.2.1. School Nutrition Environment
| Countries | Number of Schools | School BMI/A Z-Score | Linear Regression with School Categories | |||
|---|---|---|---|---|---|---|
| n | Mean ± SD (CV (%)) | α; ß (Probability F-Value) | ||||
| Round 1 | Round 2 | Round 1 § | Round 2 § | Round 1 | Round 2 | |
| Same Schools in Both Rounds | ||||||
| Ireland | 98 | 72 ‼ | 0.54 ± 0.28 a,b (52.2) | 0.50 ± 0.28 a,b (55.0) | 0.46; 0.02 (0.688) | 0.56; −0.01 (0.767) |
| Lithuania | 135 | 136 ‼ | 0.25 ± 0.28 c (111.7) | 0.20 ± 0.38 c (191.6) | 0.14; 0.03 (0.140) | 0.16; 0.01 (0.667) |
| Norway | 80 | 72 | 0.32 ± 0.27 c (84.7) | 0.38 ± 0.33 a,d (86.2) | −0.10; 0.08 (0.197) | −0.59; 0.18 (0.015) |
| Portugal ° | 113 | 112 | 0.73 ± 0.32 d (43.7) | 0.60 ± 0.34 b (56.2) | 0.99; −0.05 (0.216) | 0.59; 0.00 (0.972) |
| New Sample of Schools in Both Rounds | ||||||
| Bulgaria | 140 | – | 0.36 ± 0.45 c,e (123.7) | – | 0.48; −0.05 (0.128) | – |
| Greece | – | 114 | – | 1.02 ± 0.23 e (22.3) | – | 1.11; −0.02 (0.329) |
| Hungary | – | 38 | – | 0.29 ± 0.38 a,c,d (132.1) | – | 0.24; 0.01 (0.734) |
| Latvia | 100 | 92 | 0.23 ± 0.25 c (109.7) | 0.27 ± 0.33 c,d (120.5) | 0.22; 0.00 (0.924) | 0.43; −0.05 (0.190) |
| Malta | 74 | – | 0.59 ± 0.26 a (43.4) | – | 0.45; 0.03 (0.468) | – |
| Slovenia | 116 | 164 ‼ | 0.46 ± 0.28 b,e (60.9) | 0.40 ± 0.31 a,d (79.1) | 0.70; −0.05 (0.223) | 0.49; −0.02 (0.703) |
| Sweden | 86 | – | 0.33 ± 0.21 c (64.4) | – | 0.73; −0.07 (0.019) | – |
| Total countries | 942 | 800 | 0.42 ± 0.34 (82.2) | 0.47 ± 0.41 (87.5) | 0.29; 0.02 (0.0002) ‡ | 0.44; 0.09 (<0.0001) ‡ |
3.2.2. School BMI/A Z-Score
3.2.3. Association between School Nutrition Environment and School BMI/A Z-Score
4. Conclusions
Supplementary Files
Supplementary File 1Acknowledgments
Author Contributions
Disclaimer
Conflicts of Interest
References
- World Health Organization. Why Does Childhood Overweight and Obesity Matter? Available online: http://www.who.int/dietphysicalactivity/childhood_consequences/en/ (accessed on 10 May 2014).
- Branca, F.; Nikogosian, H.; Lobstein, T. (Eds.) The Challenge of Obesity in the WHO European Region and the Strategies for Response; WHO Regional Office for Europe: Copenhagen, Denmark, 2007. Available online: http://www.euro.who.int/__data/assets/pdf_file/0010/74746/E90711.pdf (accessed on 10 May 2014).
- WHO European Ministerial Conference on Counteracting Obesity; WHO Regional Office for Europe: Copenhagen, Denmark, 2007. Available online: http://www.euro.who.int/__data/assets/pdf_file/0006/96459/E90143.pdf (accessed on 10 May 2014).
- WHO European Ministerial Conference on Nutrition and Noncommunicable Diseases in the Context of Health 2020; WHO Regional Office for Europe: Copenhagen, Denmark, 2013. Available online: http://www.euro.who.int/__data/assets/pdf_file/0020/237035/WHO-European-Ministerial-Conference-on-Nutrition-and-Noncommunicable-Diseases-in-the-Context-of-Health-2020.pdf (accessed on 10 May 2014).
- EU Action Plan on Childhood Obesity 2014−2020; European Commission: Brussels, Belgium, 2014.
- Wijnhoven, T.; van Raaij, J.; Breda, J. WHO European Childhood Obesity Surveillance Initiative: Implementation of Round 1 (2007/2008) and Round 2 (2009/2010); WHO Regional Office for Europe: Copenhagen, Denmark, 2014. Available online: http://www.euro.who.int/__data/assets/pdf_file/0004/258781/COSI-report-round-1-and-2_final-for-web.pdf?ua=1 (accessed on 18 September 2014).
- Wijnhoven, T.; Branca, F. WHO European Childhood Obesity Surveillance Initiative. Protocol, Version January 2008; WHO Regional Office for Europe: Copenhagen, Denmark, 2008. [Google Scholar]
- WHO European Childhood Obesity Surveillance Initiative. Protocol, Version August 2010; WHO Regional Office for Europe: Copenhagen, Denmark, 2010.
- Williams, J.; Scarborough, P.; Matthews, A.; Cowburn, G.; Foster, C.; Roberts, N.; Rayner, M. A systematic review of the influence of the retail food environment around schools on obesity-related outcomes. Obes. Rev. 2014, 15, 359–374. [Google Scholar] [CrossRef] [PubMed]
- Kirk, S.F.; Penney, T.L.; McHugh, T.L. Characterizing the obesogenic environment: The state of the evidence with directions for future research. Obes. Rev. 2010, 11, 109–117. [Google Scholar] [CrossRef]
- Gorman, N.; Lackney, J.A.; Rollings, K.; Huang, T.T. Designer schools: The role of school space and architecture in obesity prevention. Obesity 2007, 15, 2521–2530. [Google Scholar] [CrossRef] [PubMed]
- Kumanyika, S.; Jeffery, R.W.; Morabia, A.; Ritenbaugh, C.; Antipatis, V.J. Obesity prevention: The case for action. Public Health Approaches to the Prevention of Obesity (PHAPO) working group of the International Obesity Task Force (IOTF). Int. J. Obes. Relat. Metab. Disord. 2002, 26, 425–436. [Google Scholar] [CrossRef] [PubMed]
- European Commission Directorate-General for Agriculture and Rural Development. School Fruit Scheme. Available online: http://ec.europa.eu/agriculture/sfs/eu-countries/index_en.htm (accessed on 10 May 2014).
- Population-Based Approaches to Childhood Obesity Prevention; World Health Organization: Geneva, Switzerland, 2012. Available online: http://apps.who.int/iris/bitstream/10665/80149/1/9789241504782_eng.pdf (accessed on 10 May 2014).
- School Policy Framework: Implementation of the WHO Global Strategy on Diet, Physical Activity and Health; World Health Organization: Geneva, Switzerland, 2008. Available online: http://www.who.int/dietphysicalactivity/SPF-en-2008.pdf (accessed on 10 May 2014).
- Steps to Health: A European Framework to Promote Physical Activity for Health; WHO Regional Office for Europe: Copenhagen, Denmark, 2007. Available online: http://www.euro.who.int/__data/assets/pdf_file/0020/101684/E90191.pdf (accessed on 10 May 2014).
- Food and Nutrition Policy for Schools: A Tool for the Development of School Nutrition Programmes in the WHO European Region; WHO Regional Office for Europe: Copenhagen, Denmark, 2006. Available online: http://www.euro.who.int/__data/assets/pdf_file/0019/152218/E89501.pdf (accessed on 10 May 2014).
- Promoting Physical Activity in Schools: An Important Element of a Health-Promoting School. WHO Information Series on School Health Document 12; World Health Organization: Geneva, Switzerland, 2007. Available online: http://www.who.int/school_youth_health/resources/information_series/FINAL%20Final.pdf (accessed on 12 August 2014).
- World Health Organization; Food and Agriculture Organization of the United Nations; Education International. Healthy Nutrition: An Essential Element of a Health-Promoting School. WHO Information Series on School Health Document 4; World Health Organization: Geneva, Switzerland, 1998. Available online: http://www.who.int/school_youth_health/media/en/428.pdf?ua=1 (accessed on 12 August 2014).
- World Health Organization; United Nations Educational, Scientific and Cultural Organization; United Nations Children’s Fund; Education Development Center; World Bank; Partnership for Child Development; Education International. The Physical School Environment: An Essential Component of a Health-Promoting School. WHO Information Series on School Health Document 2; World Health Organization: Geneva, Switzerland, 2003. Available online: http://www.who.int/school_youth_health/media/en/physical_sch_environment_v2.pdf?ua=1 (accessed on 12 August 2014).
- Wijnhoven, T.M.; van Raaij, J.M.; Spinelli, A.; Rito, A.I.; Hovengen, R.; Kunesova, M.; Starc, G.; Rutter, H.; Sjöberg, A.; Petrauskiene, A.; et al. WHO European childhood obesity surveillance initiative 2008: Weight, height and body mass index in 6–9-year-old children. Pediatr. Obes. 2013, 8, 79–97. [Google Scholar] [CrossRef]
- Wijnhoven, T.M.; van Raaij, J.M.; Spinelli, A.; Starc, G.; Hassapidou, M.; Spiroski, I.; Rutter, H.; Martos, É.; Rito, A.I.; Hovengen, R.; et al. WHO European childhood obesity surveillance initiative: Body mass index and level of overweight among 6–9-year-old children from school year 2007/2008 to school year 2009/2010. BMC Public Health. 2014, 14. [Google Scholar] [CrossRef] [Green Version]
- International Ethical Guidelines for Biomedical Research Involving Human Subjects; Council for International Organizations of Medical Sciences: Geneva, Switzerland, 2002. Available online: http://www.cioms.ch/publications/guidelines/guidelines_nov_2002_blurb.htm (accessed on 10 May 2014).
- European Commission Directorate-General for Agriculture and Rural Development. The European School Milk Programme. Available online: http://ec.europa.eu/agriculture/drinkitup/index_en.htm (accessed on 10 May 2014).
- Marketing of Foods High in Fat, Salt and Sugar to Children: Update 2012–2013; WHO Regional Office for Europe: Copenhagen, Denmark, 2013. Available online: http://www.euro.who.int/__data/assets/pdf_file/0019/191125/e96859.pdf (accessed on 10 May 2014).
- Van den Berg, S.W.; Mikolajczak, J.; Bemelmans, W.J. Changes in school environment, awareness and actions regarding overweight prevention among Dutch secondary schools between 2006−2007 and 2010−2011. BMC Public Health 2013, 13. [Google Scholar] [CrossRef]
- Thomson, J.L.; Tussing-Humphreys, L.M.; Martin, C.K.; LeBlanc, M.M.; Onufrak, S.J. Associations among school characteristics and foodservice practices in a nationally representative sample of U.S. schools. J. Nutr. Educ. Behav. 2012, 44, 423–431. [Google Scholar] [CrossRef] [PubMed]
- Van der Horst, K.; Timperio, A.; Crawford, D.; Roberts, R.; Brug, J.; Oenema, A. The school food environment: Associations with adolescent soft drink and snack consumption. Amer. J. Prev. Med. 2008, 35, 217–223. [Google Scholar] [CrossRef]
- Kim, B.; Lee, C.Y.; Kim, H.S.; Ko, I.S.; Park, C.G.; Kim, G.S. Ecological risk factors of childhood obesity in Korean elementary school students. West. J. Nurs. Res. 2012, 34, 952–972. [Google Scholar] [CrossRef] [PubMed]
- Wall, R.; Litchfield, R.; Carriquiry, A.; McDonnell, E.T.; Woodward-Lopez, G.M. Local wellness policy strength and perceived implementation of school nutrition standards across three states. Child. Obes. 2012, 8, 331–338. [Google Scholar] [PubMed]
- Interventions on Diet and Physical Activity: What Works: Summary Report; World Health Organization: Geneva, Switzerland, 2009. Available online: http://who.int/dietphysicalactivity/summary-report-09.pdf?ua=1 (accessed on 10 May 2014).
- Physical Status: The Use and Interpretation of Anthropometry. Report of a WHO Expert Committee; World Health Organization: Geneva, Switzerland, 1995. Available online: http://apps.who.int/iris/bitstream/10665/37003/1/WHO_TRS_854.pdf (accessed on 10 May 2014).
- De Onis, M.; Onyango, A.W.; Borghi, E.; Siyam, A.; Nishida, C.; Siekmann, J. Development of a WHO growth reference for school-aged children and adolescents. Bull. WHO 2007, 85, 660–667. [Google Scholar] [PubMed]
- Blössner, M.; Siyam, A.; Borghi, E.; Onyango, A.; de Onis, M. WHO AnthroPlus for Personal Computers Manual: Software for Assessing Growth of the World’s Children and Adolescents; World Health Organization: Geneva, Switzerland, 2009. Available online: http://www.who.int/growthref/tools/who_anthroplus_manual.pdf (accessed on 10 May 2014).
- Marascuilo, L.A. Large-sample multiple comparison. Psychol. Bull. 1966, 65, 280–290. [Google Scholar] [CrossRef] [PubMed]
- Games, P.A.; Howell, J.F. Pairwise multiple comparison procedures with unequal N’s and/or variances: A Monte Carlo study. J. Educ. Stat. 1976, 1, 113–125. [Google Scholar] [CrossRef]
- Turner, L.; Chaloupka, F.J. Slow progress in changing the school food environment: Nationally representative results from public and private elementary schools. J. Acad. Nutr. Diet. 2012, 112, 1380–1389. [Google Scholar]
- Schools for Health in Europe. State of the Art: Health Promoting Schools in Europe; Dutch Institute for Healthcare Improvement: Utrecht, the Netherlands, 2013. Available online: http://upload.sitesystem.ch/B2DBB48B7E/5B4613A676/83EF2D5F63.pdf (accessed on 10 May 2014).
- He, C.; Mikkelsen, B.E. The association between organic school food policy and school food environment: Results from an observational study in Danish schools. Perspect. Public Health 2014, 134, 110–116. [Google Scholar] [CrossRef] [PubMed]
- Nicholas, J.; Wood, L.; Harper, C.; Nelson, M. The impact of the food-based and nutrient-based standards on lunchtime food and drink provision and consumption in secondary schools in England. Public Health Nutr. 2013, 16, 1052–1065. [Google Scholar] [CrossRef]
- Scholtens, S.; Middelbeek, L.; Rutz, S.I.; Buijs, G.; Bemelmans, W.J. Differences in school environment, school policy and actions regarding overweight prevention between Dutch schools. A nationwide survey. BMC Public Health 2010, 10. [Google Scholar] [CrossRef] [PubMed]
- Vereecken, C.A.; Bobelijn, K.; Maes, L. School food policy at primary and secondary schools in Belgium-Flanders: Does it influence young people’s food habits? Eur. J. Clin. Nutr. 2005, 59, 271–277. [Google Scholar]
- L’Abbé, M.; Schermel, A.; Minaker, L.; Kelly, B.; Lee, A.; Vandevijvere, S.; Twohig, P.; Barquera, S.; Friel, S; Hawkes, C.; et al. Monitoring foods and beverages provided and sold in public sector settings. Obes. Rev. 2013, 14, S96–S107. [Google Scholar] [CrossRef] [PubMed]
- Van Ansem, W.J.; Schrijvers, C.T.; Rodenburg, G.; Schuit, A.J.; van de Mheen, D. School food policy at Dutch primary schools: Room for improvement? Cross-sectional findings from the INPACT study. BMC Public Health 2013, 13. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Haug, E.; Torsheim, T.; Samdal, O. Local school policies increase physical activity in Norwegian secondary schools. Health Promot. Int. 2009, 25, 63–72. [Google Scholar] [CrossRef] [PubMed]
- Ministry of Health. Výživa ve Výchovĕ ke Zdravi (Nutrition in Health Education). Available online: http://www.viscojis.cz/teens/index.php?option=com_content&view=featured&Itemid=186 (accessed on 22 August 2014). (in Czech).
- Regional Health Pardubice Region. Výchova ke Zdravi (Health Education). Available online: http://www.vychovakezdravi.cz/ (accessed on 22 August 2014). (in Czech).
- Regional Department of Public Health North. Programa Alimentação Saudável em Saúde Escolar (Healthy Eating in School Health Program). Available online: http://www.passe.com.pt/ (accessed on 10 May 2014). (in Portuguese).
- Ministry of Agriculture and the Environment. Shema Šolskega Sadja in Zelenjave (School Fruit and Vegetables Scheme). Available online: http://www.shemasolskegasadja.si/ (accessed on 19 August 2014). (in Slovene).
- Risvas, G.; Papaioannou, I.; Panagiotakos, D.B.; Farajian, P.; Bountziouka, V.; Zampelas, A. Perinatal and family factors associated with preadolescence overweight/obesity in Greece: The GRECO study. J. Epidemiol. Glob. Health 2012, 2, 145–153. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Keane, E.; Layte, R.; Harrington, J.; Kearney, P.M.; Perry, I.J. Measured parental weight status and familial socio-economic status correlates with childhood overweight and obesity at age 9. PLoS One 2012, 7. [Google Scholar] [CrossRef] [PubMed]
- Van Stralen, M.M.; te Velde, S.J.; van Nassau, F.; Brug, J.; Grammatikaki, E.; Maes, L.; de Bourdeaudhuij, I.; Verbestel, V.; Galcheva, S.; Iotova, V.; et al. Weight status of European preschool children and associations with family demographics and energy balance-related behaviours: A pooled analysis of six European studies. Obes. Rev. 2012, 13, S29–S41. [Google Scholar] [CrossRef] [PubMed]
- Bammann, K.; Gwozdz, W.; Lanfer, A.; Barba, G.; de Henauw, S.; Eiben, G.; Fernandez-Alvira, J.M.; Kovács, E.; Lissner, L.; Moreno, L.A.; et al. Socioeconomic factors and childhood overweight in Europe: Results from the multi-centre IDEFICS study. Pediatr. Obes. 2013, 8, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Jaime, P.C.; Lock, K. Do school based food and nutrition policies improve diet and reduce obesity? Prev. Med. 2009, 48, 45–53. [Google Scholar]
- Silveira, J.A.; Taddei, J.A.; Guerra, P.H.; Nobre, M.R. The effect of participation in school-based nutrition education interventions on body mass index: A meta-analysis of randomized controlled community trials. Prev. Med. 2013, 56, 237–243. [Google Scholar] [CrossRef] [PubMed]
- Sbruzzi, G.; Eibel, B.; Barbiero, S.M.; Petkowicz, R.O.; Ribeiro, R.A.; Cesa, C.C.; Martins, C.C.; Marobin, R.; Schaan, C.W.; Souza, W.B.; et al. Educational interventions in childhood obesity: A systematic review with meta-analysis of randomized clinical trials. Prev. Med. 2013, 56, 254–264. [Google Scholar] [CrossRef] [PubMed]
- Verstraeten, R.; Roberfroid, D.; Lachat, C.; Leroy, J.L.; Holdsworth, M.; Maes, L.; Kolsteren, P.W. Effectiveness of preventive school-based obesity interventions in low- and middle-income countries: A systematic review. Amer. J. Clin. Nutr. 2012, 96, 415–438. [Google Scholar] [CrossRef] [PubMed]
- De Bourdeaudhuij, I.; van Cauwenberghe, E.; Spittaels, H.; Oppert, J.M.; Rostami, C.; Brug, J.; van Lenthe, F.; Lobstein, T.; Maes, L. School-based interventions promoting both physical activity and healthy eating in Europe: A systematic review within the HOPE project. Obes. Rev. 2011, 12, 205–216. [Google Scholar] [CrossRef] [PubMed]
- Park, S.; Choi, B.Y.; Wang, Y.; Colantuoni, E.; Gittelsohn, J. School and neighborhood nutrition environment and their association with students’ nutrition behaviors and weight status in Seoul, South Korea. J. Adolesc. Health 2013, 53, 655–662. [Google Scholar] [CrossRef] [PubMed]
- Birch, L.L.; Davison, K.K. Family environmental factors influencing the developing behavioral controls of food intake and childhood overweight. Pediatr. Clin. North. Am. 2001, 48, 893–907. [Google Scholar] [CrossRef] [PubMed]
- Miller, L.J.; Joyce, S.; Carter, S.; Yun, G. Associations between childhood obesity and the availability of food outlets in the local environment: A retrospective cross-sectional study. Amer. J. Health Promot. 2013, 28, 137–145. [Google Scholar] [CrossRef]
- Van Hook, J.; Altman, C.E. Competitive food sales in schools and childhood obesity: A longitudinal study. Sociol. Educ. 2012, 85, 23–29. [Google Scholar] [CrossRef]
© 2014 by the World Health Organization; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution IGO license (http://creativecommons.org/licenses/by/3.0/igo).
Share and Cite
Wijnhoven, T.M.A.; Van Raaij, J.M.A.; Sjöberg, A.; Eldin, N.; Yngve, A.; Kunešová, M.; Starc, G.; Rito, A.I.; Duleva, V.; Hassapidou, M.; et al. WHO European Childhood Obesity Surveillance Initiative: School Nutrition Environment and Body Mass Index in Primary Schools. Int. J. Environ. Res. Public Health 2014, 11, 11261-11285. https://doi.org/10.3390/ijerph111111261
Wijnhoven TMA, Van Raaij JMA, Sjöberg A, Eldin N, Yngve A, Kunešová M, Starc G, Rito AI, Duleva V, Hassapidou M, et al. WHO European Childhood Obesity Surveillance Initiative: School Nutrition Environment and Body Mass Index in Primary Schools. International Journal of Environmental Research and Public Health. 2014; 11(11):11261-11285. https://doi.org/10.3390/ijerph111111261
Chicago/Turabian StyleWijnhoven, Trudy M.A., Joop M.A. Van Raaij, Agneta Sjöberg, Nazih Eldin, Agneta Yngve, Marie Kunešová, Gregor Starc, Ana I. Rito, Vesselka Duleva, Maria Hassapidou, and et al. 2014. "WHO European Childhood Obesity Surveillance Initiative: School Nutrition Environment and Body Mass Index in Primary Schools" International Journal of Environmental Research and Public Health 11, no. 11: 11261-11285. https://doi.org/10.3390/ijerph111111261
APA StyleWijnhoven, T. M. A., Van Raaij, J. M. A., Sjöberg, A., Eldin, N., Yngve, A., Kunešová, M., Starc, G., Rito, A. I., Duleva, V., Hassapidou, M., Martos, É., Pudule, I., Petrauskiene, A., Sant'Angelo, V. F., Hovengen, R., & Breda, J. (2014). WHO European Childhood Obesity Surveillance Initiative: School Nutrition Environment and Body Mass Index in Primary Schools. International Journal of Environmental Research and Public Health, 11(11), 11261-11285. https://doi.org/10.3390/ijerph111111261






