Screening and Assessment of Hypoglycemic Active Peptide from Natural Edible Pigment Phycobiliprotein Based on Molecular Docking, Network Pharmacology, Enzyme Inhibition Assay Analyses, and Cell Experiments
Abstract
1. Introduction
2. Results and Discussion
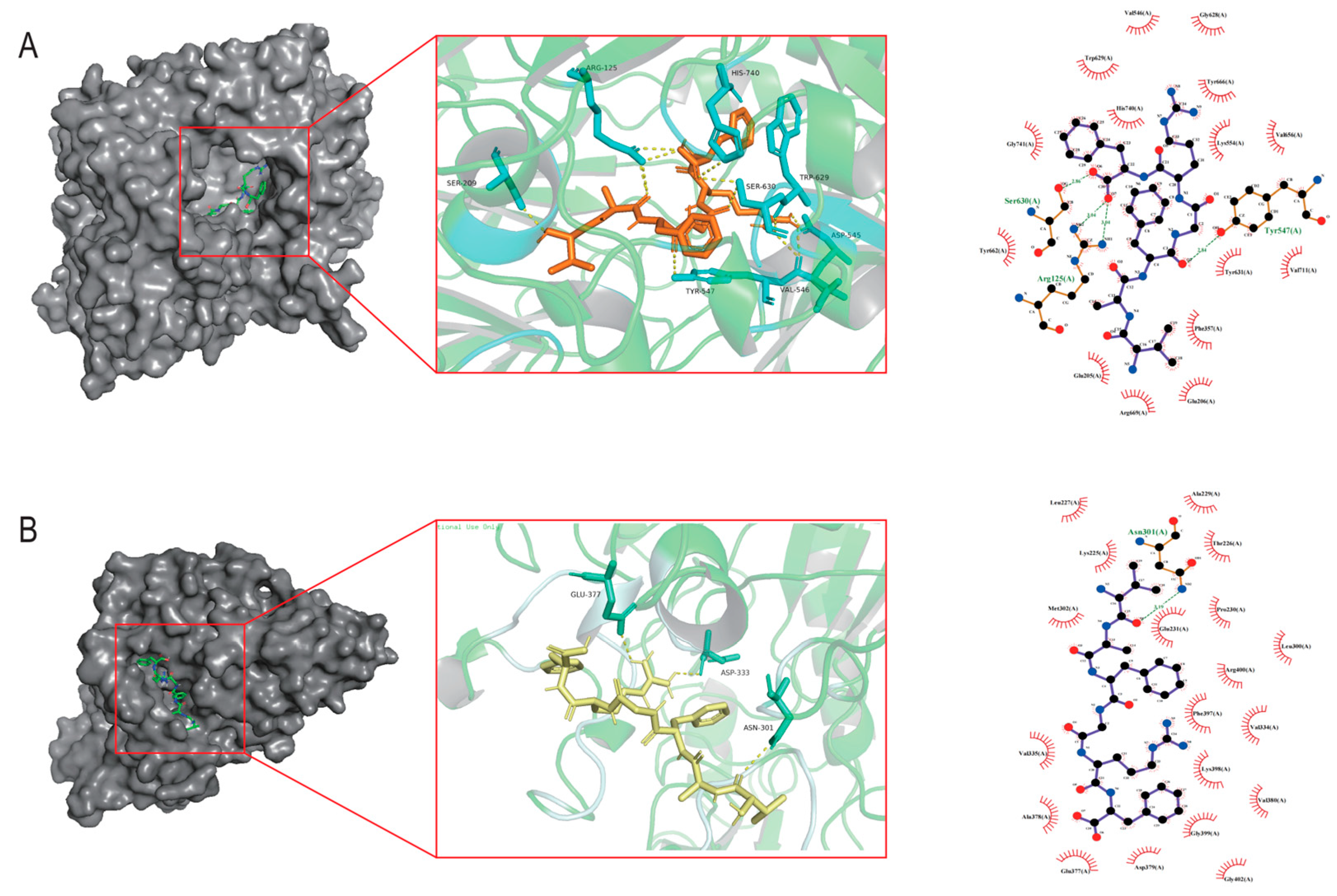
2.1. Molecular Docking Analysis
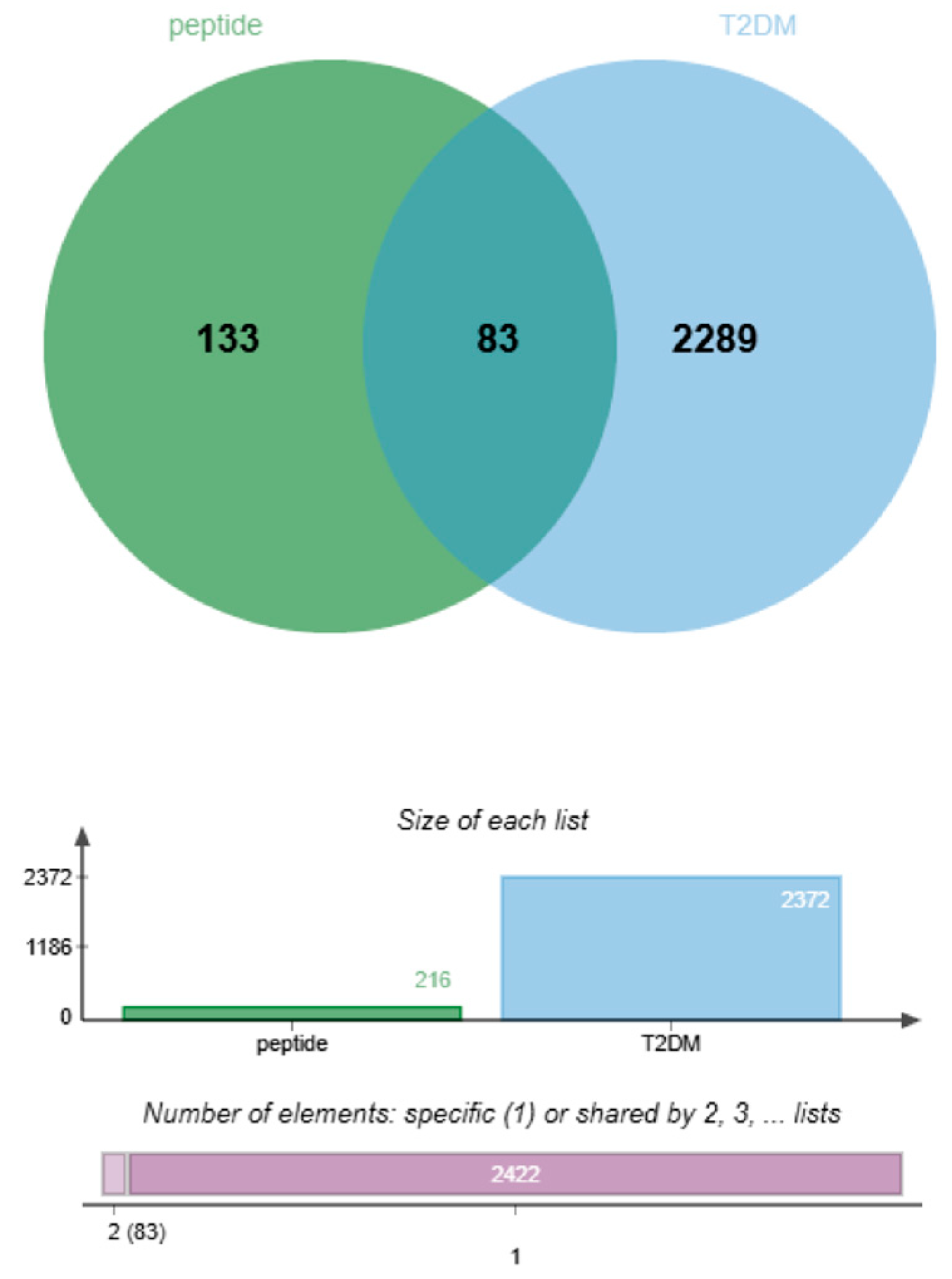
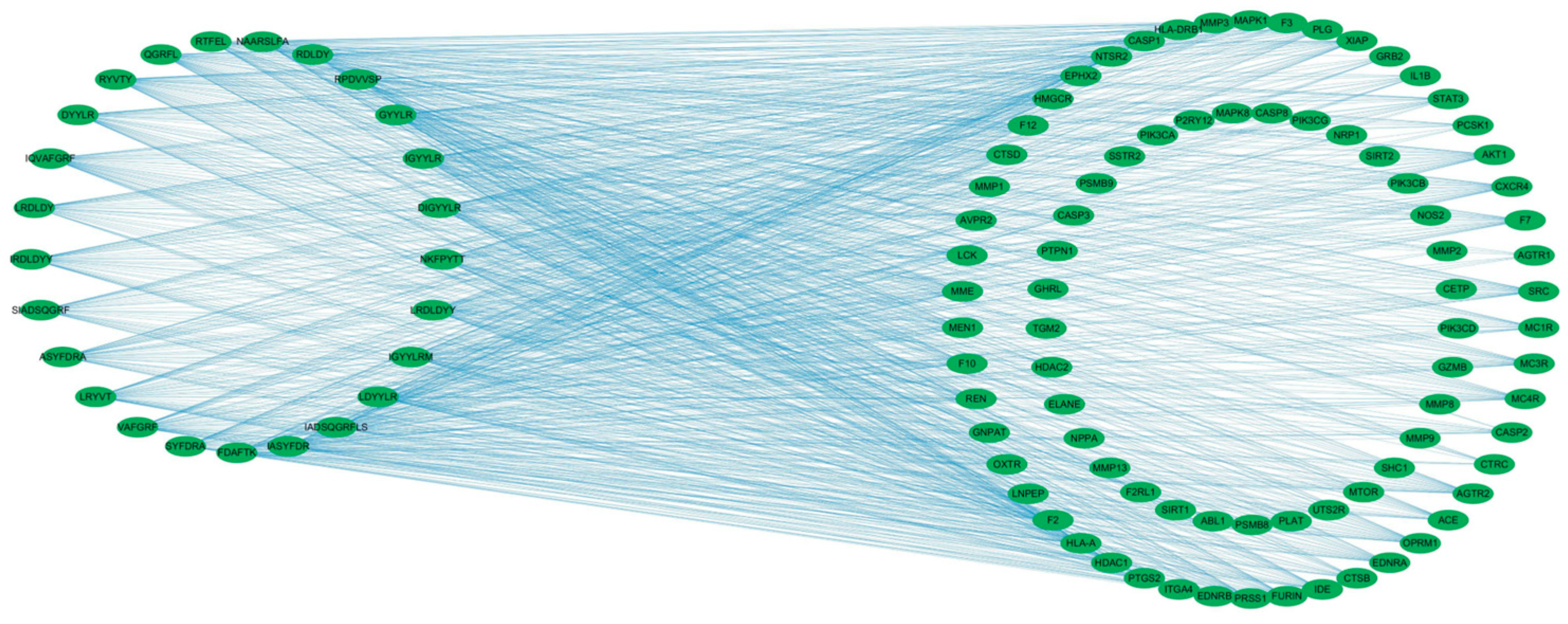
2.2. Hypoglycemic Mechanism Analysis of Active Peptides in T2DM Treatment
2.2.1. Screening for Potential T2DM-Related Interaction Targets
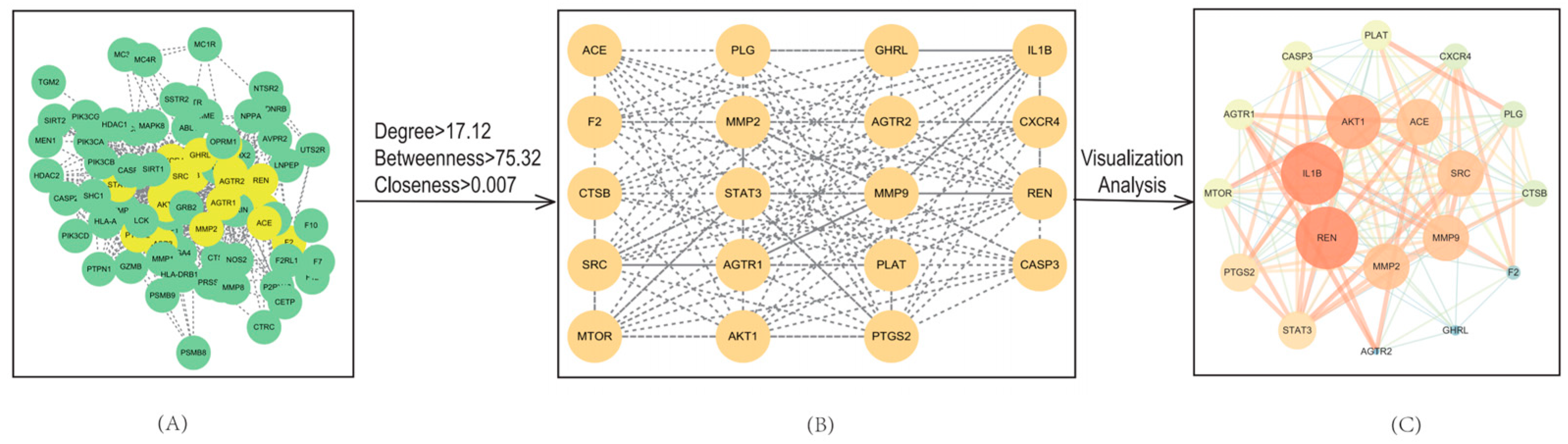
2.2.2. PPI Network Analysis
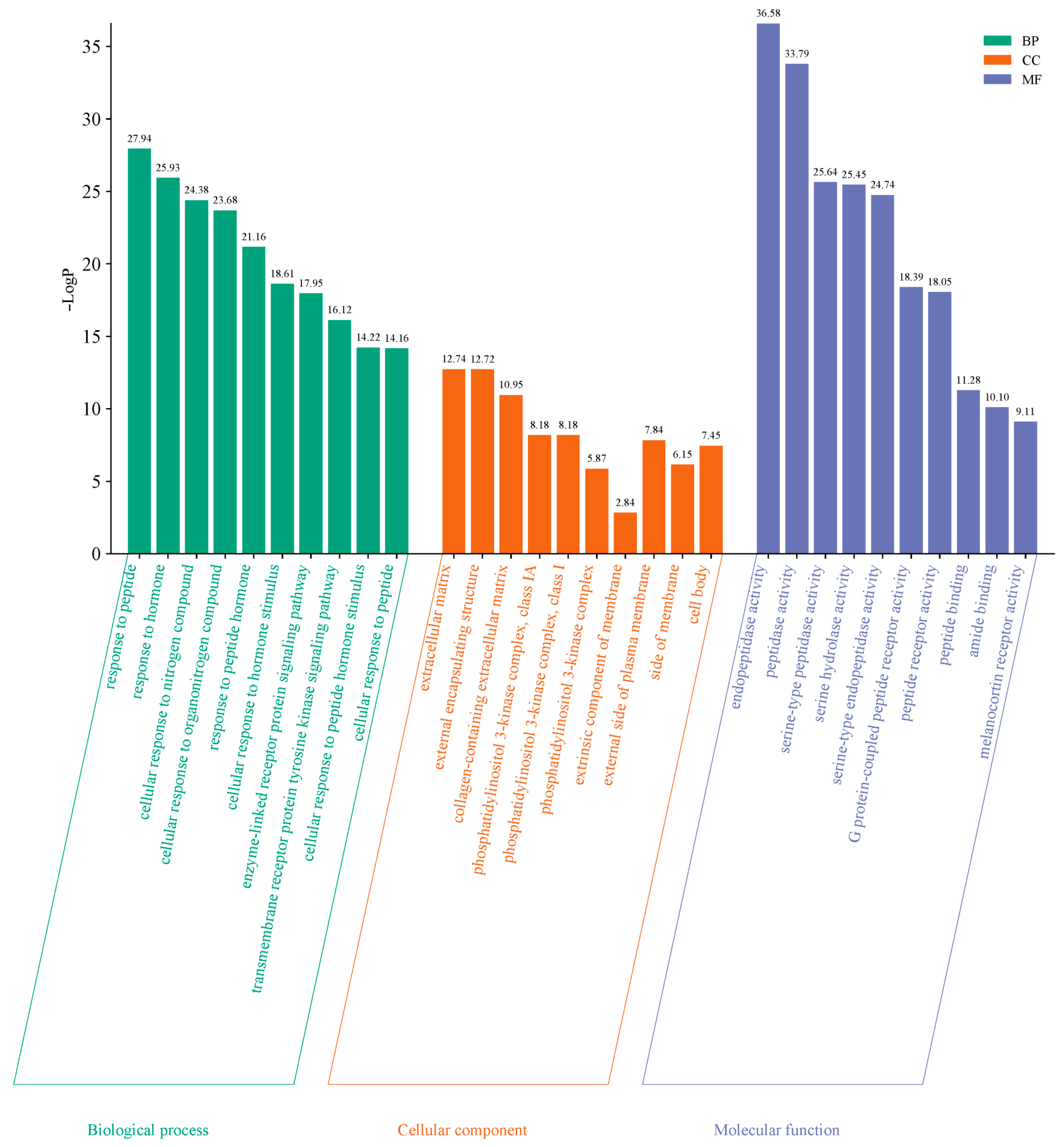
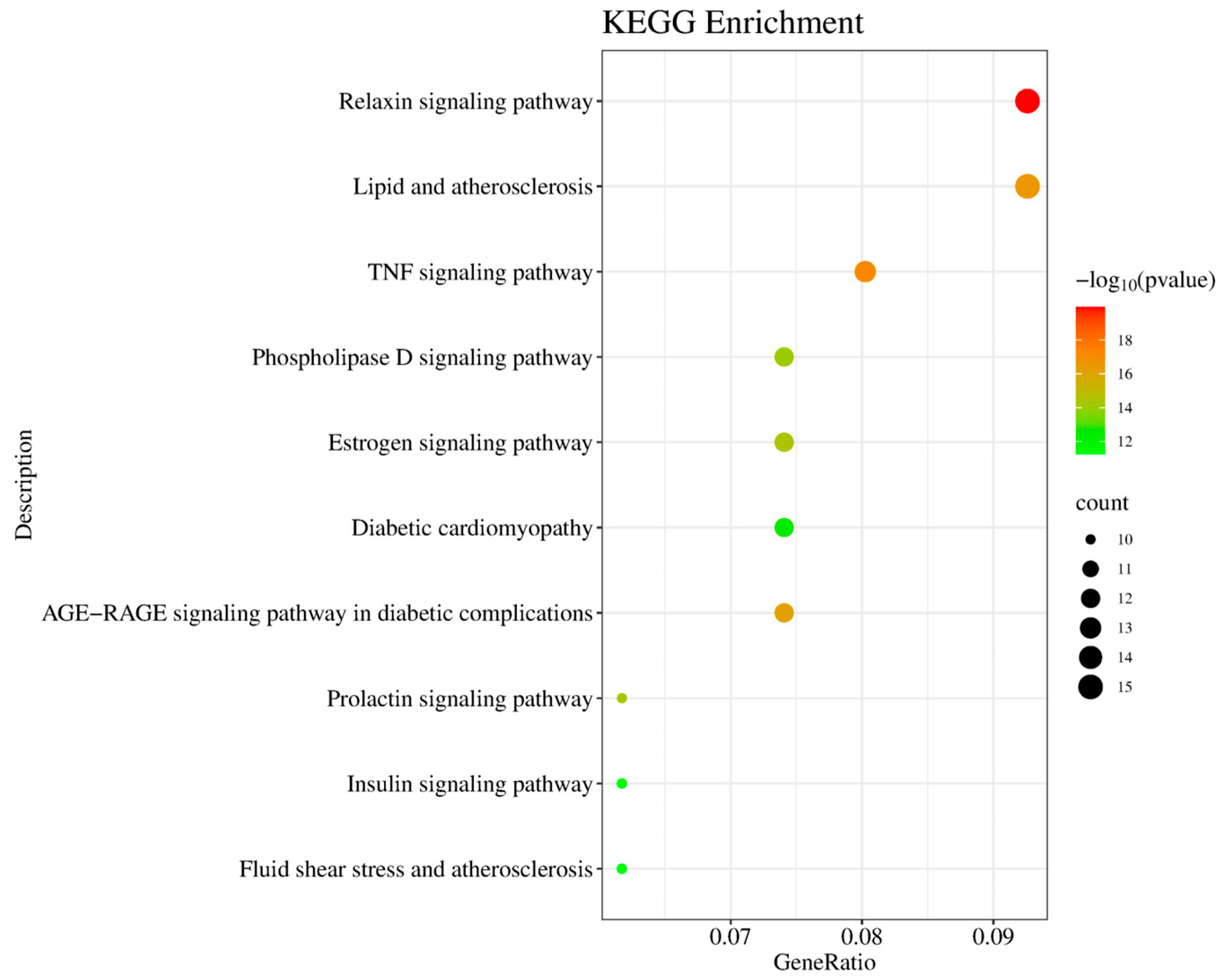
2.2.3. GO and KEGG Pathway Enrichment Analysis
2.3. Validation of Synthetic Active Peptides
2.3.1. Purity and Molecular Weight of the Hypoglycemic Active Peptides
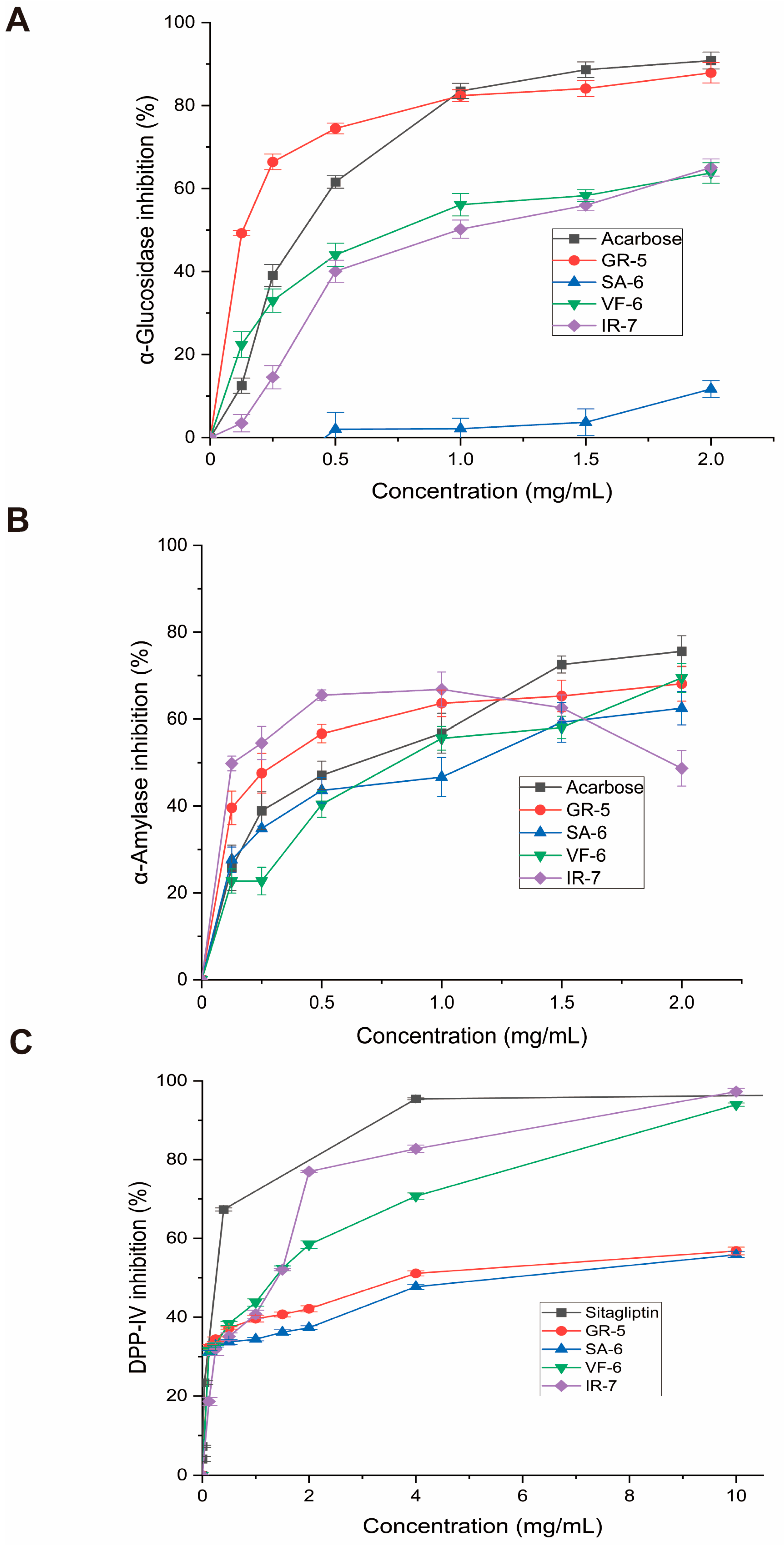
2.3.2. α-Glucosidase Inhibition Activity
2.3.3. α-Amylase Inhibition Activity
2.3.4. DPP-IV Inhibition Activity
2.4. Effect of Peptides on IR-HepG2 Cells
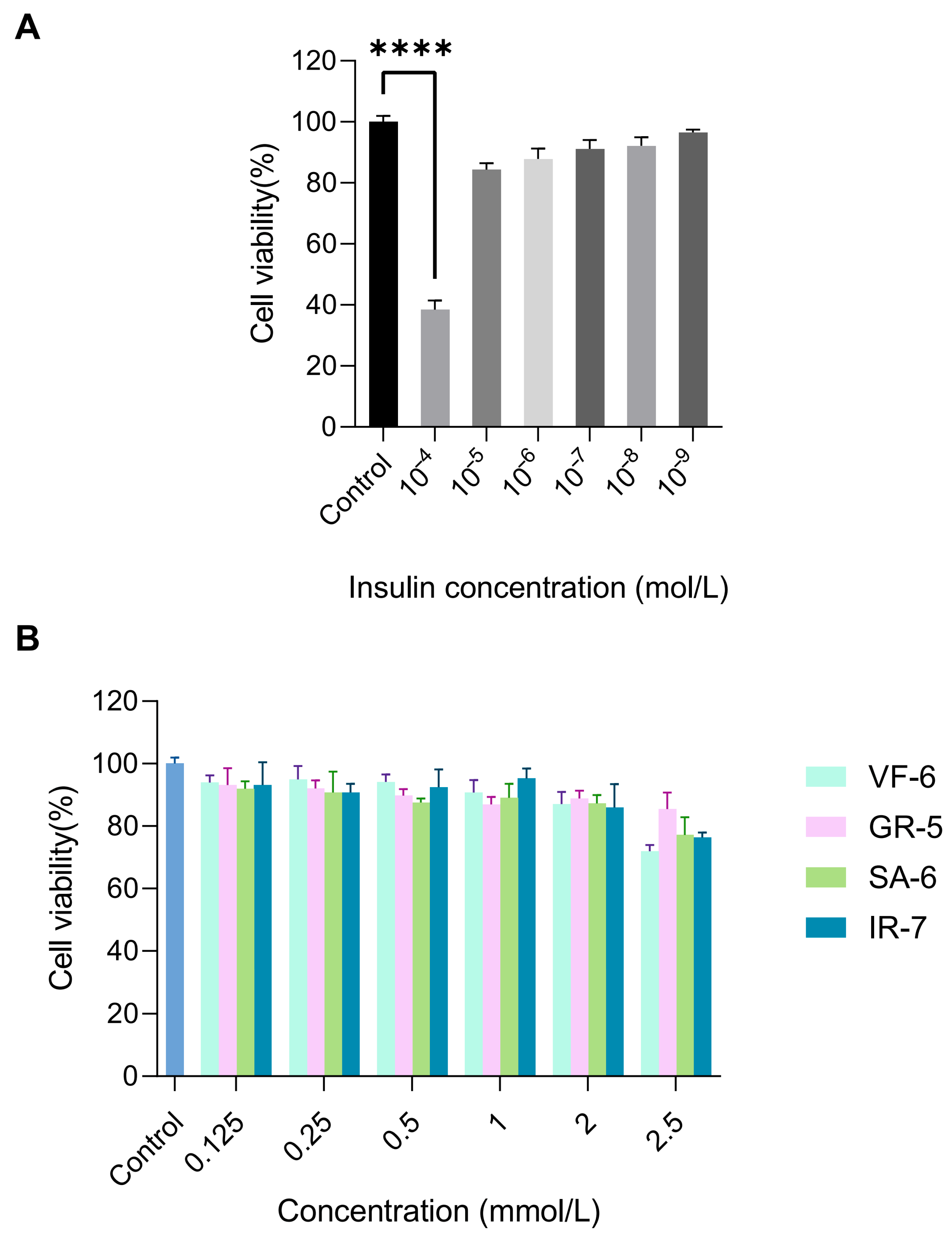
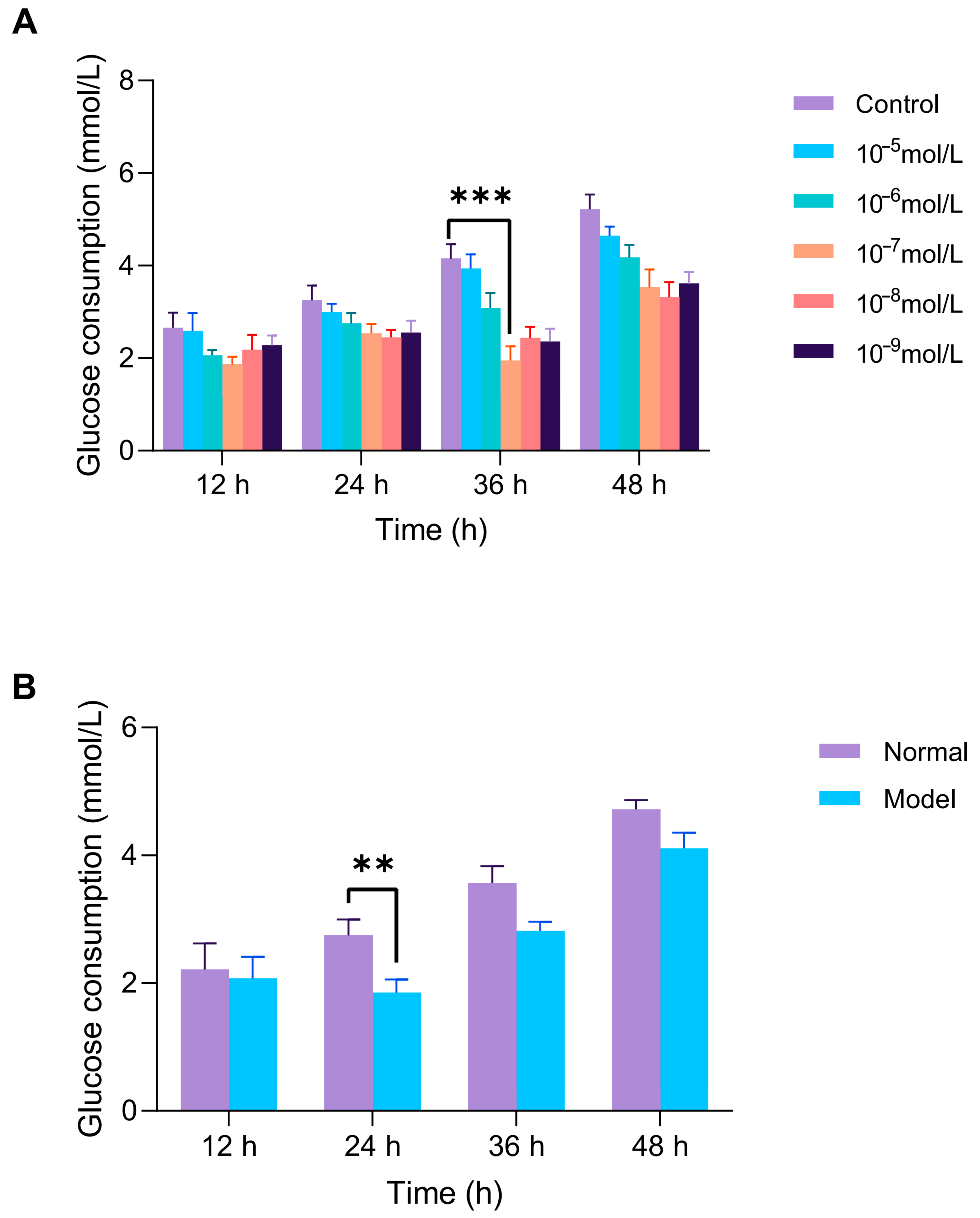
2.4.1. Establishment of the IR-HepG2 Cell Model
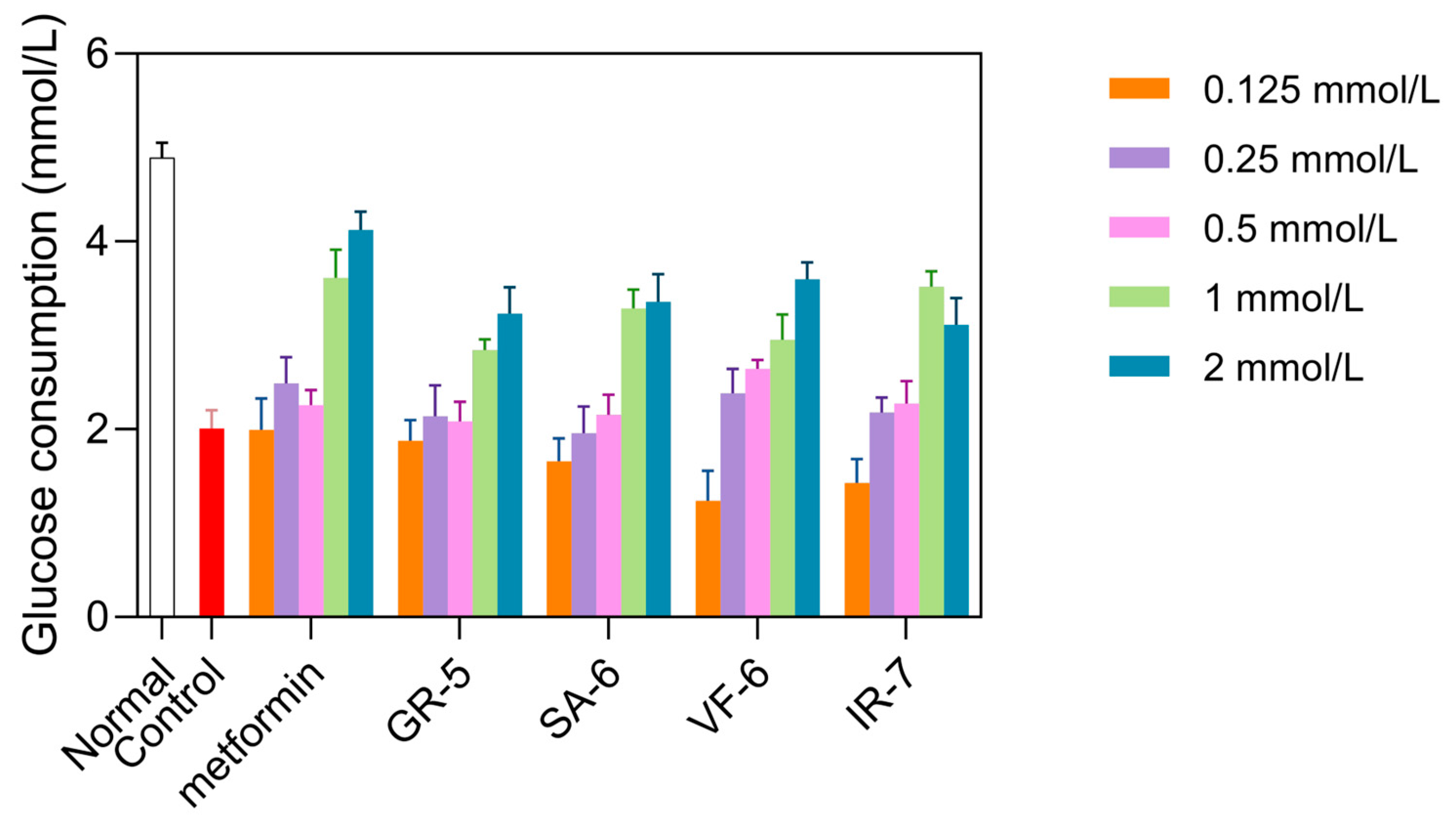
2.4.2. Effect of Peptides on Glucose Consumption in IR-HepG2 Cells
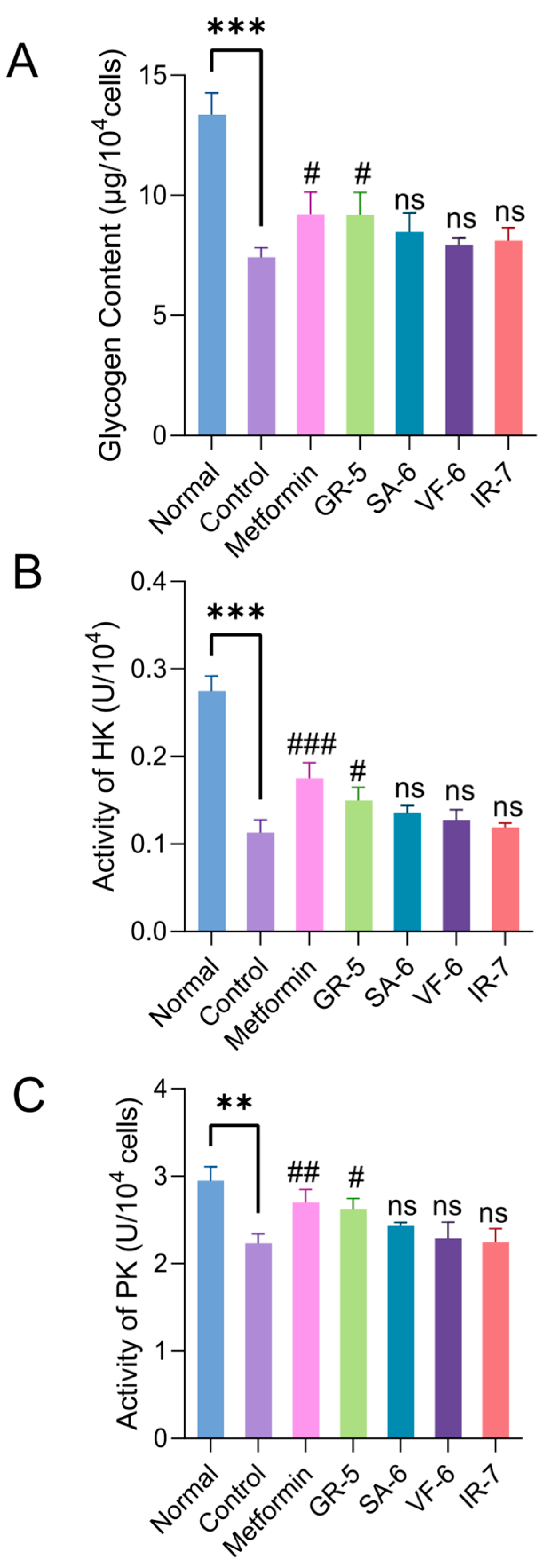
2.4.3. Effect of Peptides on Glucose Metabolism in IR-HepG2 Cells
3. Materials and Methods
3.1. Materials and Reagents
3.2. Bioactive Peptides from Phycobiliproteins
3.3. Virtual Screening of Hypoglycemic Active Peptides by Molecular Docking
3.4. Assessment of Regulatory Mechanisms Through Network Pharmacology
3.5. Solid-Phases Synthesis and Validation of Hypoglycemic Active Peptides
3.6. Cell Culture and Model Establishment
3.7. Determination of Glucose Metabolism
3.8. Statistical Analysis
4. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| T2DM | Type 2 diabetes mellitus |
| KEGG | Kyoto Encyclopedia of Genes and Genomes |
| GO | Gene Ontology |
| PPI | Related protein–protein interaction |
| PI3K/AKT | Phosphatidylinositol 3-kinase/protein kinase B |
| IL-1β | Interleukin-1β |
| STAT3 | Signal transducer and activator of transcription 3 |
| CASP3 | Cysteine aspartase |
| MMP9 | Matrix metalloprotein 9 |
| AGEs | Advanced glycation end products |
| HK | Hexokinase |
| PK | Pyruvate kinase |
| IR-HepG2 | Insulin-resistant HepG2 |
References
- Petersmann, S.; Spoerk, M.; Van De Steene, W.; Ucal, M.; Wiener, J.; Pinter, G.; Arbeiter, F. Mechanical Properties of Polymeric Implant Materials Produced by Extrusion-Based Additive Manufacturing. J. Mech. Behav. Biomed. Mater. 2020, 104, 103611. [Google Scholar] [CrossRef]
- Cuenco, J.; Dalmas, E. Islet Inflammation and β Cell Dysfunction in Type 2 Diabetes. In From Obesity to Diabetes; Eckel, J., Clément, K., Eds.; Springer International Publishing: Cham, Switzerland, 2022; pp. 227–251. ISBN 978-3-030-99995-7. [Google Scholar]
- Kido, Y. Gene–Environment Interaction in Type 2 Diabetes. Diabetol. Int. 2017, 8, 7–13. [Google Scholar] [CrossRef] [PubMed]
- Harnedy, P.A.; FitzGerald, R.J. In Vitro Assessment of the Cardioprotective, Anti-Diabetic and Antioxidant Potential of Palmaria Palmata Protein Hydrolysates. J. Appl. Phycol. 2013, 25, 1793–1803. [Google Scholar] [CrossRef]
- Pan, J.; Nawaz, M.; Liu, J.; Liu, H.; Lv, Z.; Yang, W.; Jiao, Z.; Zhang, Q. Exploring Synergistic Inhibitory Mechanisms of Flavonoid Mixtures on α-Glucosidase by Experimental Analysis and Molecular Dynamics Simulation. Food Chem. 2025, 464, 141560. [Google Scholar] [CrossRef]
- Fallah, Z.; Tajbakhsh, M.; Alikhani, M.; Larijani, B.; Faramarzi, M.A.; Hamedifar, H.; Mohammadi-Khanaposhtani, M.; Mahdavi, M. A Review on Synthesis, Mechanism of Action, and Structure-Activity Relationships of 1,2,3-Triazole-Based α-Glucosidase Inhibitors as Promising Anti-Diabetic Agents. J. Mol. Struct. 2022, 1255, 132469. [Google Scholar] [CrossRef]
- Gul, S.; Jan, F.; Alam, A.; Shakoor, A.; Khan, A.; AlAsmari, A.F.; Alasmari, F.; Khan, M.; Bo, L. Synthesis, Molecular Docking and DFT Analysis of Novel Bis-Schiff Base Derivatives with Thiobarbituric Acid for α-Glucosidase Inhibition Assessment. Sci. Rep. 2024, 14, 3419. [Google Scholar] [CrossRef]
- Li, X.; Bai, Y.; Jin, Z.; Svensson, B. Food-Derived Non-Phenolic α-Amylase and α-Glucosidase Inhibitors for Controlling Starch Digestion Rate and Guiding Diabetes-Friendly Recipes. LWT 2022, 153, 112455. [Google Scholar] [CrossRef]
- Oyedemi, S.O.; Oyedemi, B.O.; Ijeh, I.I.; Ohanyerem, P.E.; Coopoosamy, R.M.; Aiyegoro, O.A. Alpha-Amylase Inhibition and Antioxidative Capacity of Some Antidiabetic Plants Used by the Traditional Healers in Southeastern Nigeria. Sci. World J. 2017, 2017, 3592491. [Google Scholar] [CrossRef]
- Skalli, S.; Hassikou, R.; Arahou, M. An Ethnobotanical Survey of Medicinal Plants Used for Diabetes Treatment in Rabat, Morocco. Heliyon 2019, 5, e01421. [Google Scholar] [CrossRef]
- Jia, Y.; Cai, S.; Muhoza, B.; Qi, B.; Li, Y. Advance in Dietary Polyphenols as Dipeptidyl Peptidase-IV Inhibitors to Alleviate Type 2 Diabetes Mellitus: Aspects from Structure-Activity Relationship and Characterization Methods. Crit. Rev. Food Sci. Nutr. 2023, 63, 3452–3467. [Google Scholar] [CrossRef]
- Nongonierma, A.B.; Cadamuro, C.; Le Gouic, A.; Mudgil, P.; Maqsood, S.; FitzGerald, R.J. Dipeptidyl Peptidase IV (DPP-IV) Inhibitory Properties of a Camel Whey Protein Enriched Hydrolysate Preparation. Food Chem. 2019, 279, 70–79. [Google Scholar] [CrossRef] [PubMed]
- Gilbert, M.P.; Pratley, R.E. GLP-1 Analogs and DPP-4 Inhibitors in Type 2 Diabetes Therapy: Review of Head-to-Head Clinical Trials. Front. Endocrinol. 2020, 11, 178. [Google Scholar] [CrossRef] [PubMed]
- Deacon, C.F. Dipeptidyl Peptidase 4 Inhibitors in the Treatment of Type 2 Diabetes Mellitus. Nat. Rev. Endocrinol. 2020, 16, 642–653. [Google Scholar] [CrossRef]
- Xiao, T.; Zeng, J.; Qiu, L.; Wang, R.; Li, N.; Deng, Z.; Zheng, L. Combining in Silico and in Vitro Approaches to Identify Endogenous Hypoglycemic Peptides from Human Milk. Food Funct. 2022, 13, 2899–2912. [Google Scholar] [CrossRef]
- Chandrasekaran, S.; de Mejia, E.G. Optimization, Identification, and Comparison of Peptides from Germinated Chickpea (Cicer Arietinum) Protein Hydrolysates Using Either Papain or Ficin and Their Relationship with Markers of Type 2 Diabetes. Food Chem. 2022, 374, 131717. [Google Scholar] [CrossRef]
- Li, Q. Isolation, Synthesis, and Activity Study of Hypoglycemic Peptides from Laminaria japonica. Master’s Thesis, Dalian University of Technology, Dalian, China, 2022. [Google Scholar]
- Liu, Y.; Zhang, J.; An, C.; Liu, C.; Zhang, Q.; Ding, H.; Ma, S.; Xue, W. Identification of Potential Mechanisms of Rk1 Combination with Rg5 in the Treatment of Type II Diabetes Mellitus by Integrating Network Pharmacology and Experimental Validation. Int. J. Mol. Sci. 2023, 24, 14828. [Google Scholar] [CrossRef]
- Xu, S.; Tang, L.; Qian, X.; Wang, Y.; Gong, J.; Yang, H.; Su, D. Molecular Mechanism of Ginkgo Biloba in Treating Type 2 Diabetes Mellitus Combined with Non-alcoholic Fatty Liver Disease Based on Network Pharmacology, Molecular Docking, and Experimental Evaluations. J. Food Biochem. 2022, 46, e14419. [Google Scholar] [CrossRef]
- Duan, X.; Huang, S.; Peng, D.; Han, L.; Wang, X.; Wang, Y.; Pan, L. Application of Network Pharmacology in the Study of Traditional Chinese Medicine Formulas. Chin. Pharmacol. Bull. 2020, 36, 303–308. [Google Scholar]
- Yu, X. Study on the Extraction and Purification of Phycocyanin from Spirulina platensis. Master’s Thesis, Jiangsu University, Zhenjiang, China, 2023. [Google Scholar]
- Li, Y.; Aiello, G.; Bollati, C.; Bartolomei, M.; Arnoldi, A.; Lammi, C. Phycobiliproteins from Arthrospira Platensis (Spirulina): A New Source of Peptides with Dipeptidyl Peptidase-IV Inhibitory Activity. Nutrients 2020, 12, 794. [Google Scholar] [CrossRef]
- Yu, Z.; Wang, Y.; Shuian, D.; Liu, J.; Zhao, W. Identification and Molecular Mechanism of Novel Immunomodulatory Peptides from Gelatin Hydrolysates: Molecular Docking, Dynamic Simulation, and Cell Experiments. J. Agric. Food Chem. 2023, 71, 2924–2934. [Google Scholar] [CrossRef] [PubMed]
- Chaudhary, S.; Vats, I.D.; Chopra, M.; Biswas, P.; Pasha, S. Effect of Varying Chain Length between P1 and P1′ Position of Tripeptidomimics on Activity of Angiotensin-Converting Enzyme Inhibitors. Bioorg. Med. Chem. Lett. 2009, 19, 4364–4366. [Google Scholar] [CrossRef]
- Pantaleao, S.Q.; Philot, E.A.; de Resende-Lara, P.T.; Lima, A.N.; Perahia, D.; Miteva, M.A.; Scott, A.L.; Honorio, K.M. Structural Dynamics of DPP-4 and Its Influence on the Projection of Bioactive Ligands. Molecules 2018, 23, 490. [Google Scholar] [CrossRef]
- Gandhimathi, R.; Anbuselvi, S.; Saranya, R. In-Vitro Antidiabetic Activity, Theoretical Investigation by DFT and Molecular Docking of Mono Oxo Vanadyl (IV) Azomethine Macromolecule. J. Indian Chem. Soc. 2023, 100, 101033. [Google Scholar] [CrossRef]
- Li, J.; Wang, X.; Wei, Y.; Lin, B.; Liu, R.; Wu, H. Study on Hypoglycemic Peptides from Pinctada martensii Based on Network Pharmacology and Molecular Docking. Food Ferment. Ind. 2022, 48, 176–184. [Google Scholar] [CrossRef]
- Dong, S.; Tang, C. Research Progress on the Role of PI3K/AKT Signaling Pathway in Osseointegration of Dental Implants in Patients with Type 2 Diabetes. Stomatology 2022, 42, 10216–1030+1035. [Google Scholar] [CrossRef]
- Tomita, T. Apoptosis in Pancreatic β-Islet Cells in Type 2 Diabetes. Bosnian J. Basic Med. Sci. 2016, 16, 162–179. [Google Scholar] [CrossRef] [PubMed]
- Jud, P.; Sourij, H. Therapeutic Options to Reduce Advanced Glycation End Products in Patients with Diabetes Mellitus: A Review. Diabetes Res. Clin. Pract. 2019, 148, 54–63. [Google Scholar] [CrossRef] [PubMed]
- LaRock, C.N.; Todd, J.; LaRock, D.L.; Olson, J.; O’Donoghue, A.J.; Robertson, A.A.B.; Cooper, M.A.; Hoffman, H.M.; Nizet, V. IL-1β Is an Innate Immune Sensor of Microbial Proteolysis. Sci. Immunol. 2016, 1, eaah3539. [Google Scholar] [CrossRef]
- Tziastoudi, M.; Theoharides, T.C.; Nikolaou, E.; Efthymiadi, M.; Eleftheriadis, T.; Stefanidis, I. Key Genetic Components of Fibrosis in Diabetic Nephropathy: An Updated Systematic Review and Meta-Analysis. Int. J. Mol. Sci. 2022, 23, 15331. [Google Scholar] [CrossRef]
- Sato, H.; Nagashima, K.; Ogura, M.; Sato, Y.; Tahara, Y.; Ogura, K.; Yamano, G.; Sugizaki, K.; Fujita, N.; Tatsuoka, H.; et al. Src Regulates Insulin Secretion and Glucose Metabolism by Influencing Subcellular Localization of Glucokinase in Pancreatic-Cells. J. Diabetes Investig. 2016, 7, 171–178. [Google Scholar] [CrossRef]
- Pipicz, M.; Demjan, V.; Sarkoezy, M.; Csont, T. Effects of Cardiovascular Risk Factors on Cardiac STAT3. Int. J. Mol. Sci. 2018, 19, 3572. [Google Scholar] [CrossRef]
- Hayes, H.L.; Peterson, B.S.; Haldeman, J.M.; Newgard, C.B.; Hohmeier, H.E.; Stephens, S.B. Delayed Apoptosis Allows Islet β-Cells to Implement an Autophagic Mechanism to Promote Cell Survival. PLoS ONE 2017, 12, e0172567. [Google Scholar] [CrossRef]
- Zhou, L.; Liu, H. Correlation Analysis of Microvascular Complications in Elderly Patients with Type 2 Diabetes with Endothelin, Matrix Metalloproteinase-9, and Other Risk Factors. Pract. J. Med. Pharm 2020, 37, 397–400. [Google Scholar] [CrossRef]
- Flores-Medellín, S.A.; Camacho-Ruiz, R.M.; Guízar-González, C.; Rivera-Leon, E.A.; Llamas-Covarrubias, I.M.; Mojica, L. Protein Hydrolysates and Phenolic Compounds from Fermented Black Beans Inhibit Markers Related to Obesity and Type-2 Diabetes. Legume Sci. 2021, 3, e64. [Google Scholar] [CrossRef]
- Ye, C.; Zhang, R.; Dong, L.; Chi, J.; Huang, F.; Dong, L.; Zhang, M.; Jia, X. α-Glucosidase Inhibitors from Brown Rice Bound Phenolics Extracts (BRBPE): Identification and Mechanism. Food Chem. 2022, 372, 131306. [Google Scholar] [CrossRef]
- Abudurexiti, A.; Abdurahman, A.; Zhang, R.; Zhong, Y.; Lei, Y.; Qi, S.; Hou, W.; Ma, X. Screening of α-Glucosidase Inhibitors in Cichorium Glandulosum Boiss. et Huet Extracts and Study of Interaction Mechanisms. ACS Omega 2024, 9, 19401–19417. [Google Scholar] [CrossRef]
- Li, H.; Yang, J.; Wang, M.; Ma, X.; Peng, X. Studies on the Inhibition of α-Glucosidase by Biflavonoids and Their Interaction Mechanisms. Food Chem. 2023, 420, 136113. [Google Scholar] [CrossRef] [PubMed]
- Bischoff, H. The Mechanism of Alpha-Glucosidase Inhibition in the Management of Diabetes. Clin. Investig. Med. 1995, 18, 303–311. [Google Scholar]
- Saidi, I.; Baccari, W.; Teka, S.; El Oudi, M.; Alsaif, B.; Mohamed, N.; Waffo-Teguo, P.; Ben Jannet, H. Verbascoside and Rare Flavone Glucosides from Citharexylum Spinosum L. Flowers as Antihyperglycemic Agents: Isolation, α-Amylase Inhibition, Molecular Docking and Drug-Likeness Prediction. J. Mol. Struct. 2024, 1312, 138529. [Google Scholar] [CrossRef]
- Ge, X. Preparation and Inhibitory Mechanism of Sea Cucumber α-Amylase Inhibitory Peptides. Master’s Thesis, Tianjin University of Science and Technology, Tianjin, China, 2023. [Google Scholar]
- Poovitha, S.; Parani, M. In Vitro and in Vivo α-Amylase and α-Glucosidase Inhibiting Activities of the Protein Extracts from Two Varieties of Bitter Gourd (Momordica charantia L.). BMC Complement. Altern. Med. 2016, 16, 185. [Google Scholar] [CrossRef] [PubMed]
- Xiong, Y.; Ng, K.; Zhang, P.; Warner, R.D.; Shen, S.; Tang, H.-Y.; Liang, Z.; Fang, Z. In Vitro α-Glucosidase and α-Amylase Inhibitory Activities of Free and Bound Phenolic Extracts from the Bran and Kernel Fractions of Five Sorghum Grain Genotypes. Foods 2020, 9, 1301. [Google Scholar] [CrossRef]
- Bollati, C.; Xu, R.; Boschin, G.; Bartolomei, M.; Rivardo, F.; Li, J.; Arnoldi, A.; Lammi, C. Integrated Evaluation of the Multifunctional DPP-IV and ACE Inhibitory Effect of Soybean and Pea Protein Hydrolysates. Nutrients 2022, 14, 2379. [Google Scholar] [CrossRef]
- Amanatidou, D.; Eleftheriou, P.; Petrou, A.; Geronikaki, A.; Lialiaris, T. Τhiazolidine-4-One Derivatives with Variable Modes of Inhibitory Action Against DPP4, a Drug Target with Multiple Activities and Established Role in Diabetes Mellitus Type II. Pharmaceuticals 2025, 18, 52. [Google Scholar] [CrossRef]
- Kahn, S.E.; Cooper, M.E.; Del Prato, S. Pathophysiology and Treatment of Type 2 Diabetes: Perspectives on the Past, Present, and Future. Lancet 2014, 383, 1068–1083. [Google Scholar] [CrossRef] [PubMed]
- Liu, Y.; Li, Y.; Zhang, W.; Sun, M.; Zhang, Z. Hypoglycemic Effect of Inulin Combined with Ganoderma Lucidum Polysaccharides in T2DM Rats. J. Funct. Foods 2019, 55, 381–390. [Google Scholar] [CrossRef]
- Bai, Z.; Huang, X.; Wu, G.; Zhou, Y.; Deng, X.; Yang, J.; Yin, J.; Nie, S. Hepatic Metabolism-Related Effects of Polysaccharides from Red Kidney Bean and Small Black Soybean on Type 2 Diabetes. Food Chem. 2023, 403, 134334. [Google Scholar] [CrossRef]
- Wang, C.; Luo, D.; Zheng, L.; Zhao, M. Anti-Diabetic Mechanism and Potential Bioactive Peptides of Casein Hydrolysates in STZ/HFD-Induced Diabetic Rats. J. Sci. Food Agric. 2024, 104, 2947–2958. [Google Scholar] [CrossRef] [PubMed]
- Liu, J.; Bai, X.P.; Fu, P.C. In Silico and in Vitro Assessment of Bioactive Peptides from Arthrospira Platensis Phycobiliproteins for DPP-IV Inhibitory Activity, ACE Inhibitory Activity, and Antioxidant Activity. J. Appl. Phycol. 2022, 34, 1497–1511. [Google Scholar] [CrossRef]
- Cai, L.; Wu, S.; Jia, C.; Cui, C.; Sun-Waterhouse, D. Active Peptides with Hypoglycemic Effect Obtained from Hemp (Cannabis sativa L.) Protein through Identification, Molecular Docking, and Virtual Screening. Food Chem. 2023, 429, 136912. [Google Scholar] [CrossRef]
- Chen, Y.; Qiu, Z.; Liu, X.; Ren, G.; Li, W.; Zhang, M.; Zhao, Y.; Zhang, B. Bioinformatics Analysis of the Activity of Simulated Digest of Mytilus edulis Proteins Based on In Silico Digestion. Food Ferment. Ind. 2022, 48, 185–192. [Google Scholar] [CrossRef]
- Liu, J.; Zhen, D.; Hu, C.; Liu, Y.; Shen, X.; Fu, P.; He, Y. Reconfiguration of Gut Microbiota and Reprogramming of Liver Metabolism with Phycobiliproteins Bioactive Peptides to Rehabilitate Obese Rats. Nutrients 2022, 14, 3635. [Google Scholar] [CrossRef] [PubMed]
- Zhang, L.-S.; Wang, X.; Dong, L.-L. Antioxidation and Antiglycation of Polysaccharides from Misgurnus Anguillicaudatus. Food Chem. 2011, 124, 183–187. [Google Scholar] [CrossRef]
- Yang, Q.; Zhu, Z.; Wang, L.; Xia, H.; Mao, J.; Wu, J.; Kato, K.; Li, H.; Zhang, J.; Yamanaka, K.; et al. The Protective Effect of Silk Fibroin on High Glucose Induced Insulin Resistance in HepG2 Cells. Environ. Toxicol. Pharmacol. 2019, 69, 66–71. [Google Scholar] [CrossRef] [PubMed]
| Peptide Sequence | Affinity | The Number of Hydrogen Bonds | The Shortest Hydrogen Bond Distance | |||
|---|---|---|---|---|---|---|
| 3wy1 | 4a5s | 3wy1 | 4a5s | 3wy1 | 4a5s | |
| VF-6 | −8 | −9.4 | 3 | 13 | 2.4 Å | 2.2 Å |
| GR-5 | −8 | −8.9 | 8 | 8 | 2.2 Å | 1.9 Å |
| SA-6 | −8 | −8.5 | 8 | 8 | 1.9 Å | 2.4 Å |
| IR-7 | −8.2 | −8.9 | 7 | 8 | 2.1 Å | 2.2 Å |
| No. | Target Name | Gene Name | Uniprot ID | Degree |
|---|---|---|---|---|
| 1 | Signal transducer and activator of transcription 3 | STAT3 | P40763 | 42 |
| 2 | Caspase-3 | CASP3 | P42574 | 38 |
| 3 | Serine/threonine-protein kinase mTOR | MTOR | P42345 | 32 |
| 4 | Serine/threonine-protein kinase AKT | AKT1 | P31749 | 56 |
| 5 | C-X-C chemokine receptor type 4 | CXCR4 | P61073 | 30 |
| 6 | Tyrosine-protein kinase SRC | SRC | P12931 | 45 |
| 7 | Angiotensin-converting enzyme | ACE | P12821 | 33 |
| 8 | Matrix metalloproteinase 2 | MMP2 | P08253 | 31 |
| 9 | Tissue-type plasminogen activator | PLAT | P00750 | 25 |
| 10 | Interleukin-1 beta | IL1B | P01584 | 54 |
| 11 | Renin | REN | P00797 | 29 |
| 12 | Cathepsin (B and K) | CTSB | P07858 | 27 |
| 13 | Cyclooxygenase-2 | PTGS2 | P35354 | 32 |
| 14 | Plasminogen | PLG | P00747 | 28 |
| 15 | Thrombin | F2 | P00734 | 23 |
| 16 | Matrix metalloproteinase 9 | MMP9 | P14780 | 39 |
| 17 | Angiotensin II receptor | AGTR2 | P50052 | 18 |
| 18 | Type-1 angiotensin II receptor | AGTR1 | P30556 | 31 |
| 19 | Appetite-regulating hormone | GHRL | Q9UBU3 | 19 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zhu, Z.; Zhang, Y.; He, B.; He, L.; Fang, G.; Ning, Y.; Fu, P.; Liu, J. Screening and Assessment of Hypoglycemic Active Peptide from Natural Edible Pigment Phycobiliprotein Based on Molecular Docking, Network Pharmacology, Enzyme Inhibition Assay Analyses, and Cell Experiments. Mar. Drugs 2025, 23, 331. https://doi.org/10.3390/md23080331
Zhu Z, Zhang Y, He B, He L, Fang G, Ning Y, Fu P, Liu J. Screening and Assessment of Hypoglycemic Active Peptide from Natural Edible Pigment Phycobiliprotein Based on Molecular Docking, Network Pharmacology, Enzyme Inhibition Assay Analyses, and Cell Experiments. Marine Drugs. 2025; 23(8):331. https://doi.org/10.3390/md23080331
Chicago/Turabian StyleZhu, Zhimin, Yan Zhang, Bingbing He, Limin He, Guihong Fang, Yi Ning, Pengcheng Fu, and Jing Liu. 2025. "Screening and Assessment of Hypoglycemic Active Peptide from Natural Edible Pigment Phycobiliprotein Based on Molecular Docking, Network Pharmacology, Enzyme Inhibition Assay Analyses, and Cell Experiments" Marine Drugs 23, no. 8: 331. https://doi.org/10.3390/md23080331
APA StyleZhu, Z., Zhang, Y., He, B., He, L., Fang, G., Ning, Y., Fu, P., & Liu, J. (2025). Screening and Assessment of Hypoglycemic Active Peptide from Natural Edible Pigment Phycobiliprotein Based on Molecular Docking, Network Pharmacology, Enzyme Inhibition Assay Analyses, and Cell Experiments. Marine Drugs, 23(8), 331. https://doi.org/10.3390/md23080331







