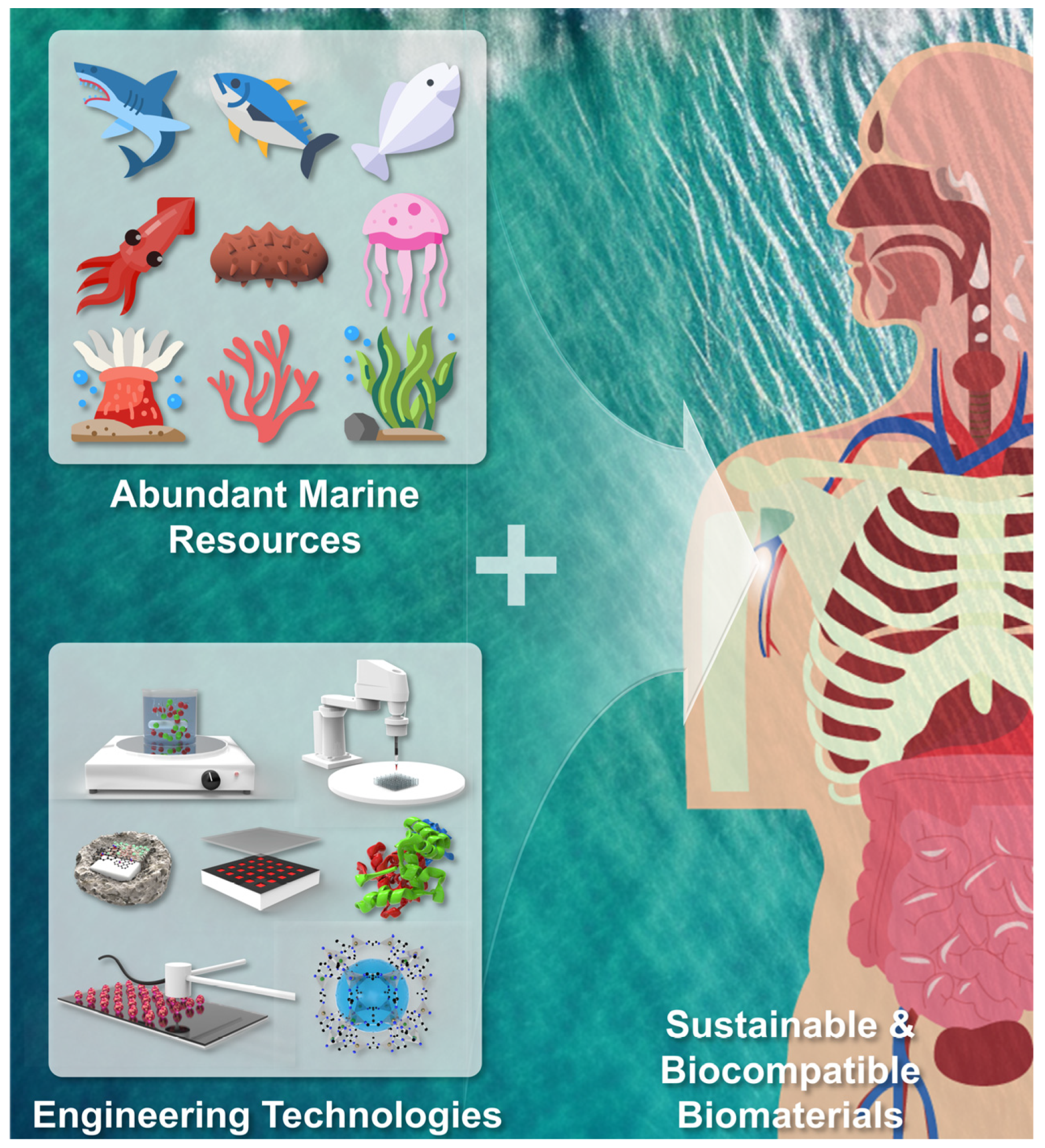
Recent Advances in Marine Biomaterials Tailored and Primed for the Treatment of Damaged Soft Tissues
Abstract
:1. Introduction
2. Application of Marine Polysaccharides in Soft Tissue Engineering

| Engineered Forms | Applications | Marine Biomaterials | Sources | Cells/Animal Tested | Key Findings | Ref. |
|---|---|---|---|---|---|---|
| Acidic isolated chitin | Cartilage | Chitin | Porifera (Lanthella basta) | Human mesenchymal stromal cells | Cell viability and adipogenic potential were retained after cryopreservation. | [24] |
| Deproteinized chitin | Skin and neural tissues | Chitin | Porifera (Aplysina fistularis) |
| Skin and neural cells exhibited inherent phenotypes on the scaffolds. | [25] |
| PIAC hydrogel | Skin |
|
| L929 fibroblast | The prepared hydrogel provided fibroblasts favorable for ECM-mimicking 3D microenvironment. | [29] |
| KaMA hydrogel | Skin |
|
|
| Injectable and sprayable KaMA hydrogel supports survival and growth of skin cells. | [33] |
| GEL-MOD/CAR-MOD hydrogel film | SC engineering |
|
| ASCs | GEL-MOD/CAR-MOD hybrid hydrogel supported viability and proliferation of ASCs. | [34] |
| Bioprinted Mw-κCa-MA hydrogel | Cartilage |
|
| ATDC5 cell | Microwave-assisted methacrylation resulted in improved cell viability, chondrogenic differentiation, and ECM deposition in κCa-MA hydrogels. | [35] |
| CS-F NP | Nerve | Fucoidan | Brown seaweed (Fucus vesiculosus) | PC12 cell | CS-F NPs exhibited sustained bFGF release to induce neurogenic differentiation of PC12 cells. | [42] |
| MeLam microparticle | Skin | Laminarin | Brown algae | L929 cell | Encapsulated PL promoted the enhancement of L929 cell adhesion and proliferation. | [43] |
| Cellulose-PLLA, PDLLA, and PDX electrospun nanofiber | Skin | Ulvan | Green seaweed |
| Ulvan cellulose accelerated fibroblasts’ growth and in vivo angiogenesis. | [46] |
| Bioprinted UlMA-GelMA hydrogel | Skin | Ulvan | Ul-84 |
| Ul84 supported fibroblast growth and deposition of key dermal ECM components. | [48] |
| FA hydrogel | Skin | Agarose | Red algae (Gracilaria and Gelidium) |
| FA hydrogel showed excellent biocompatibility with pro-regenerative process with M2-type CD206-positive macrophages. | [54] |
| Si-HPMC/GY785 hydrogel | Cartilage | GY785 | Deep-sea bacteria (Alteromonas infernus) | RACs Swiss nude mice | Si-HPMC/GY785 facilitated chondrogenesis through interactions with growth factors, gene expression, and in vivo cartilage-like ECM formation. | [58] |
| HE800/GY785-Si-HPMChydrogel | Cartilage | HE800 and GY785 | NA | MC3T3-E1 cells C28/I2 cells | Addition of HE800 and GY785 in Si-HPMC hydrogel increased the mechanical properties and induced polysaccharide-specific effects on cell viability and spatial organization. | [59] |
3. Application of Marine Proteins in Soft Tissue Engineering
| Engineered Forms | Application | Marine Biomaterials | Sources | Cells/Animal Tested | Key Findings | Ref. |
|---|---|---|---|---|---|---|
| Bilayered CA:L-CSPG nanofibrous sponge | Skin | Col | Stellate pufferfish (Arothron stellatus) |
| CA:L-CSPG membranes exhibited excellent biocompatibility, antioxidant activity, and antibacterial activity with no hemolysis. | [68] |
| Freeze-dried FSC scaffold | Skin | Col | Grass carp (Ctenopharyngodon idellus) | L929 cell
| FSC promoted wound recovery in a burn wound with no scars. | [69] |
| Cryogelated HA-Col scaffold | Cartilage | Col | Shark skin (Prionace glauca) | hASC | HA-Col supports early chondrogenic differentiation, but external stimulation is needed for phenotype maintenance. | [73] |
| Freeze-dried Jellagen/TGF-β3 implants | Cartilage | Col | Jelly fish (Rhizostoma pulmo) | hMSCs | Incorporated TGF-β3 nanoreservoir in jellyfish collagen promoted up-regulation of chondrogenic markers of hMSCs. | [77] |
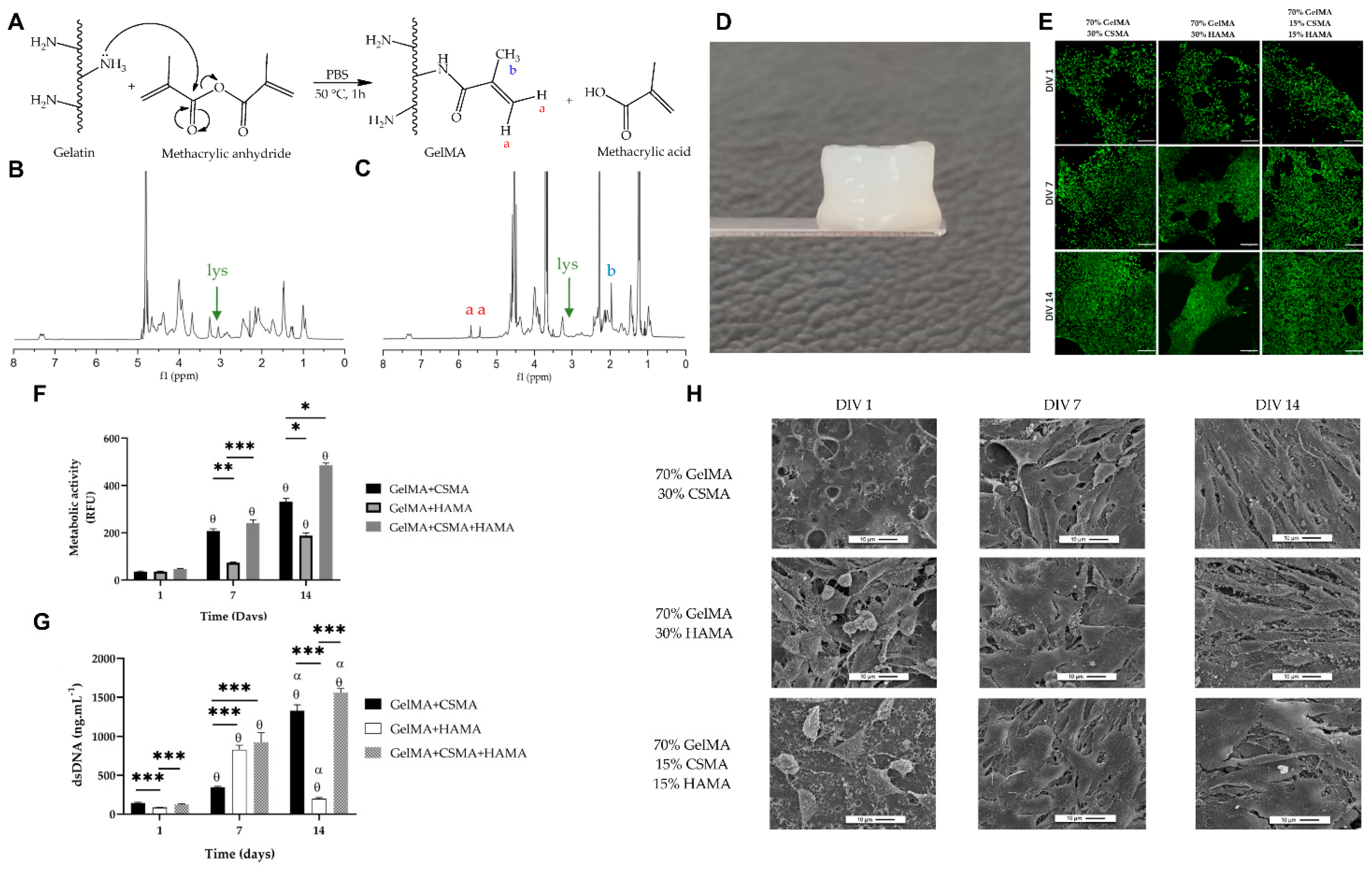
| GelMA-HAMA/CSMA hydrogel | Cartilage | Gel | Greenland halibut (Reinhardtius hippoglossoides) | ATDC-5 cell | The gelatin hydrogel provided cytocompatible environment to ATDC-5 cells. | [82] |
| GelMA/AA hydrogel | Cornea | Gel | Codfish (Gadus morhua) | Human KCs | AA in the GelMA facilitated Col production and corneal regeneration. | [80] |
| Col-CS-fucoidan cryogel | Skin |
|
| L929 fibroblast | Marine Col-CS-fucoidan cryogels can be engineered as acellular biomaterials or cell-laden cryogels. | [85] |
| Col-CS-fucoidan cryogel | Cartilage |
|
| hASCs | Marine Col-CS-fucoidan cryogels showed excellent biomechanical properties and support behaviors of hASCs. | [86] |
4. Conclusion and Future Perspectives
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Clark, R.A.; Ghosh, K.; Tonnesen, M.G. Tissue engineering for cutaneous wounds. J. Investig. Dermatol. 2007, 127, 1018–1029. [Google Scholar] [CrossRef] [PubMed]
- Halim, A.S.; Khoo, T.L.; Yussof, S.J.M. Biologic and synthetic skin substitutes: An overview. Indian. J. Plast. Surg. 2010, 43, S23–S28. [Google Scholar] [CrossRef] [PubMed]
- Mehta, S.A.; Saharia, K.K.; Nellore, A.; Blumberg, E.A.; Fishman, J.A. Infection and clinical xenotransplantation: Guidance from the Infectious Disease Community of Practice of the American Society of Transplantation. Am. J. Transpl. 2023, 23, 309–315. [Google Scholar] [CrossRef]
- Khademhosseini, A.; Langer, R. A decade of progress in tissue engineering. Nat. Protoc. 2016, 11, 1775–1781. [Google Scholar] [CrossRef] [PubMed]
- Cho, S.; Discher, D.E.; Leong, K.W.; Vunjak-Novakovic, G.; Wu, J.C. Challenges and opportunities for the next generation of cardiovascular tissue engineering. Nat. Methods 2022, 19, 1064–1071. [Google Scholar] [CrossRef]
- Kwon, H.; Brown, W.E.; Lee, C.A.; Wang, D.; Paschos, N.; Hu, J.C.; Athanasiou, K.A. Surgical and tissue engineering strategies for articular cartilage and meniscus repair. Nat. Rev. Rheumatol. 2019, 15, 550–570. [Google Scholar] [CrossRef]
- Abbasian, M.; Massoumi, B.; Mohammad-Rezaei, R.; Samadian, H.; Jaymand, M. Scaffolding polymeric biomaterials: Are naturally occurring biological macromolecules more appropriate for tissue engineering? Int. J. Biol. Macromol. 2019, 134, 673–694. [Google Scholar] [CrossRef]
- Yang, D.; Xiao, J.; Wang, B.; Li, L.; Kong, X.; Liao, J. The immune reaction and degradation fate of scaffold in cartilage/bone tissue engineering. Mater. Sci. Eng. C 2019, 104, 109927. [Google Scholar] [CrossRef]
- Williams, D.F. Challenges with the development of biomaterials for sustainable tissue engineering. Front. Bioeng. Biotechnol. 2019, 7, 127. [Google Scholar] [CrossRef]
- Tümerkan, E.A.; Kozaci, L.; Miri, A.; Maharjan, S.; Cecen, B. Sustainable aquatic waste and by-products processing: Biomaterials in tissue engineering facts and gaps. Mater. Today Sustain. 2023, 23, 100445. [Google Scholar] [CrossRef]
- Govindharaj, M.; Roopavath, U.K.; Rath, S.N. Valorization of discarded Marine Eel fish skin for collagen extraction as a 3D printable blue biomaterial for tissue engineering. J. Clean. Prod. 2019, 230, 412–419. [Google Scholar] [CrossRef]
- Alves, A.; Costa-Gouveia, J.; de Castro, J.V.; Sotelo, C.; Vázquez, J.A.; Pérez-Martín, R.I.; Torrado, E.; Neves, N.; Reis, R.L.; Castro, A. Study of the immunologic response of marine-derived collagen and gelatin extracts for tissue engineering applications. Acta Biomater. 2022, 141, 123–131. [Google Scholar] [CrossRef] [PubMed]
- Carvalho, D.N.; Williams, D.S.; Sotelo, C.G.; Pérez-Martín, R.I.; Mearns-Spragg, A.; Reis, R.L.; Silva, T.H. Marine origin biomaterials using a compressive and absorption methodology as cell-laden hydrogel envisaging cartilage tissue engineering. Biomater. Adv. 2022, 137, 212843. [Google Scholar] [CrossRef] [PubMed]
- Kang, M.S.; Park, R.; Jo, H.J.; Shin, Y.C.; Kim, C.-S.; Hyon, S.-H.; Hong, S.W.; Oh, J.; Han, D.-W. Spontaneous Osteogenic Differentiation of Human Mesenchymal Stem Cells by Tuna-Bone-Derived Hydroxyapatite Composites with Green Tea Polyphenol-Reduced Graphene Oxide. Cells 2023, 12, 1448. [Google Scholar] [CrossRef] [PubMed]
- Kostopoulos, V.; Kotrotsos, A.; Fouriki, K.; Kalarakis, A.; Portan, D. Fabrication and characterization of polyetherimide electrospun scaffolds modified with graphene nano-platelets and hydroxyapatite nano-particles. Int. J. Mol. Sci. 2020, 21, 583. [Google Scholar] [CrossRef]
- Roy, V.C.; Islam, M.R.; Sadia, S.; Yeasmin, M.; Park, J.-S.; Lee, H.-J.; Chun, B.-S. Trash to treasure: An up-to-date understanding of the valorization of seafood by-products, targeting the major bioactive compounds. Mar. Drug 2023, 21, 485. [Google Scholar] [CrossRef]
- Brunner, E.; Ehrlich, H.; Schupp, P.; Hedrich, R.; Hunoldt, S.; Kammer, M.; Machill, S.; Paasch, S.; Bazhenov, V.; Kurek, D. Chitin-based scaffolds are an integral part of the skeleton of the marine demosponge Ianthella basta. J. Struct. Biol. 2009, 168, 539–547. [Google Scholar] [CrossRef]
- Ehrlich, H.; Ilan, M.; Maldonado, M.; Muricy, G.; Bavestrello, G.; Kljajic, Z.; Carballo, J.; Schiaparelli, S.; Ereskovsky, A.; Schupp, P. Three-dimensional chitin-based scaffolds from Verongida sponges (Demospongiae: Porifera). Part I. Isolation and identification of chitin. Int. J. Biol. Macromol. 2010, 47, 132–140. [Google Scholar] [CrossRef]
- Mohan, K.; Muralisankar, T.; Jayakumar, R.; Rajeevgandhi, C. A study on structural comparisons of α-chitin extracted from marine crustacean shell waste. Carbohydr. Polym. Technol. Appl. 2021, 2, 100037. [Google Scholar] [CrossRef]
- Shaala, L.A.; Asfour, H.Z.; Youssef, D.T.; Żółtowska-Aksamitowska, S.; Wysokowski, M.; Tsurkan, M.; Galli, R.; Meissner, H.; Petrenko, I.; Tabachnick, K. New source of 3D chitin scaffolds: The Red Sea demosponge Pseudoceratina arabica (Pseudoceratinidae, Verongiida). Mar. Drugs 2019, 17, 92. [Google Scholar] [CrossRef]
- Kunze, K.; Niemann, H.; Ueberlein, S.; Schulze, R.; Ehrlich, H.; Brunner, E.; Proksch, P.; van Pée, K.-H. Brominated skeletal components of the marine demosponges, Aplysina cavernicola and Ianthella basta: Analytical and biochemical investigations. Mar. Drugs 2013, 11, 1271–1287. [Google Scholar] [CrossRef] [PubMed]
- Wysokowski, M.; Petrenko, I.; Stelling, A.L.; Stawski, D.; Jesionowski, T.; Ehrlich, H. Poriferan chitin as a versatile template for extreme biomimetics. Polymers 2015, 7, 235–265. [Google Scholar] [CrossRef]
- Wysokowski, M.; Motylenko, M.; Beyer, J.; Makarova, A.; Stöcker, H.; Walter, J.; Galli, R.; Kaiser, S.; Vyalikh, D.; Bazhenov, V.V. Extreme biomimetic approach for developing novel chitin-GeO2 nanocomposites with photoluminescent properties. Nano Res. 2015, 8, 2288–2301. [Google Scholar] [CrossRef]
- Mutsenko, V.V.; Gryshkov, O.; Lauterboeck, L.; Rogulska, O.; Tarusin, D.N.; Bazhenov, V.V.; Schütz, K.; Brüggemeier, S.; Gossla, E.; Akkineni, A.R. Novel chitin scaffolds derived from marine sponge Ianthella basta for tissue engineering approaches based on human mesenchymal stromal cells: Biocompatibility and cryopreservation. Int. J. Biol. Macromol. 2017, 104, 1955–1965. [Google Scholar] [CrossRef]
- Machałowski, T.; Rusak, A.; Wiatrak, B.; Haczkiewicz-Leśniak, K.; Popiel, A.; Jaroszewicz, J.; Żak, A.; Podhorska-Okołów, M.; Jesionowski, T. Naturally formed chitinous skeleton isolated from the marine demosponge Aplysina fistularis as a 3D scaffold for tissue engineering. Materials 2021, 14, 2992. [Google Scholar] [CrossRef] [PubMed]
- Bacakova, L.; Filova, E.; Parizek, M.; Ruml, T.; Svorcik, V. Modulation of cell adhesion, proliferation and differentiation on materials designed for body implants. Biotechnol. Adv. 2011, 29, 739–767. [Google Scholar] [CrossRef]
- Thankam, F.G.; Muthu, J. Influence of plasma protein–hydrogel interaction moderated by absorption of water on long-term cell viability in amphiphilic biosynthetic hydrogels. RSC Adv. 2013, 3, 24509–24520. [Google Scholar] [CrossRef]
- Rastogi, P.; Kandasubramanian, B. Review of alginate-based hydrogel bioprinting for application in tissue engineering. Biofabrication 2019, 11, 042001. [Google Scholar] [CrossRef]
- Radhakrishnan, A.; Jose, G.M.; Kurup, M. PEG-penetrated chitosan–alginate co-polysaccharide-based partially and fully cross-linked hydrogels as ECM mimic for tissue engineering applications. Prog. Biomater. 2015, 4, 101–112. [Google Scholar] [CrossRef]
- Lim, Y.-M.; Gwon, H.-J.; Choi, J.-H.; Shin, J.; Nho, Y.-C.; Jeong, S.I.; Chong, M.S.; Lee, Y.-M.; Kwon, I.K.; Kim, S.E. Preparation and biocompatibility study of gelatin/kappa-carrageenan scaffolds. Macromol. Res. 2010, 18, 29–34. [Google Scholar] [CrossRef]
- Distantina, S.; Rochmadi, R.; Fahrurrozi, M.; Wiratni, W. Preparation and characterization of glutaraldehyde-crosslinked kappa carrageenan hydrogel. Eng. J. 2013, 17, 57–66. [Google Scholar] [CrossRef]
- Prajapati, V.D.; Maheriya, P.M.; Jani, G.K.; Solanki, H.K. RETRACTED: Carrageenan: A natural seaweed polysaccharide and its applications. Carbohydr. Polym. 2014, 105, 97–112. [Google Scholar] [CrossRef] [PubMed]
- Tavakoli, S.; Kharaziha, M.; Kermanpur, A.; Mokhtari, H. Sprayable and injectable visible-light Kappa-carrageenan hydrogel for in-situ soft tissue engineering. Int. J. Biol. Macromol. 2019, 138, 590–601. [Google Scholar] [CrossRef] [PubMed]
- Tytgat, L.; Vagenende, M.; Declercq, H.; Martins, J.; Thienpont, H.; Ottevaere, H.; Dubruel, P.; Van Vlierberghe, S. Synergistic effect of κ-carrageenan and gelatin blends towards adipose tissue engineering. Carbohydr. Polym. 2018, 189, 1–9. [Google Scholar] [CrossRef]
- Thakur, A.; Jaiswal, M.K.; Peak, C.W.; Carrow, J.K.; Gentry, J.; Dolatshahi-Pirouz, A.; Gaharwar, A.K. Injectable shear-thinning nanoengineered hydrogels for stem cell delivery. Nanoscale 2016, 8, 12362–12372. [Google Scholar] [CrossRef] [PubMed]
- İlhan, G.T.; Irmak, G.; Gümüşderelioğlu, M. Microwave assisted methacrylation of Kappa carrageenan: A bioink for cartilage tissue engineering. Int. J. Biol. Macromol. 2020, 164, 3523–3534. [Google Scholar] [CrossRef]
- Li, B.; Lu, F.; Wei, X.; Zhao, R. Fucoidan: Structure and bioactivity. Molecules 2008, 13, 1671–1695. [Google Scholar] [CrossRef]
- Millet, J.; Jouault, S.C.; Mauray, S.; Theveniaux, J.; Sternberg, C.; Vidal, B.C.; Fischer, A. Antithrombotic and anticoagulant activities of a low molecular weight fucoidan by the subcutaneous route. Thromb. Haemost. 1999, 81, 391–395. [Google Scholar]
- Luthuli, S.; Wu, S.; Cheng, Y.; Zheng, X.; Wu, M.; Tong, H. Therapeutic effects of fucoidan: A review on recent studies. Mar. Drugs 2019, 17, 487. [Google Scholar] [CrossRef]
- Wang, Y.; Xing, M.; Cao, Q.; Ji, A.; Liang, H.; Song, S. Biological activities of fucoidan and the factors mediating its therapeutic effects: A review of recent studies. Mar. Drugs 2019, 17, 183. [Google Scholar] [CrossRef]
- Abdel-Latif, H.M.; Dawood, M.A.; Alagawany, M.; Faggio, C.; Nowosad, J.; Kucharczyk, D. Health benefits and potential applications of fucoidan (FCD) extracted from brown seaweeds in aquaculture: An updated review. Fish Shellfish Immunol. 2022, 122, 115–130. [Google Scholar] [CrossRef]
- Huang, Y.C.; Yang, Y.T. Effect of basic fibroblast growth factor released from chitosan–fucoidan nanoparticles on neurite extension. J. Tissue Eng. Regen. Med. 2016, 10, 418–427. [Google Scholar] [CrossRef] [PubMed]
- Martins, C.; Custódio, C.; Mano, J. Multifunctional laminarin microparticles for cell adhesion and expansion. Carbohydr. Polym. 2018, 202, 91–98. [Google Scholar] [CrossRef] [PubMed]
- Kuznetsova, T.A.; Andryukov, B.G.; Besednova, N.N.; Zaporozhets, T.S.; Kalinin, A.V. Marine algae polysaccharides as basis for wound dressings, drug delivery, and tissue engineering: A review. J. Mar. Sci. Eng. 2020, 8, 481. [Google Scholar] [CrossRef]
- Tziveleka, L.-A.; Ioannou, E.; Roussis, V. Ulvan, a bioactive marine sulphated polysaccharide as a key constituent of hybrid biomaterials: A review. Carbohydr. Polym. 2019, 218, 355–370. [Google Scholar] [CrossRef] [PubMed]
- Madub, K.; Goonoo, N.; Gimié, F.; Arsa, I.A.; Schönherr, H.; Bhaw-Luximon, A. Green seaweeds ulvan-cellulose scaffolds enhance in vitro cell growth and in vivo angiogenesis for skin tissue engineering. Carbohydr. Polym. 2021, 251, 117025. [Google Scholar] [CrossRef]
- Chen, X.; Yue, Z.; Winberg, P.C.; Dinoro, J.N.; Hayes, P.; Beirne, S.; Wallace, G.G. Development of rhamnose-rich hydrogels based on sulfated xylorhamno-uronic acid toward wound healing applications. Biomater. Sci. 2019, 7, 3497–3509. [Google Scholar] [CrossRef]
- Chen, X.; Yue, Z.; Winberg, P.C.; Lou, Y.-R.; Beirne, S.; Wallace, G.G. 3D bioprinting dermal-like structures using species-specific ulvan. Biomater. Sci. 2021, 9, 2424–2438. [Google Scholar] [CrossRef]
- Irastorza-Lorenzo, A.; Sánchez-Porras, D.; Ortiz-Arrabal, O.; de Frutos, M.J.; Esteban, E.; Fernández, J.; Janer, A.; Campos, A.; Campos, F.; Alaminos, M. Evaluation of marine agarose biomaterials for tissue engineering applications. Int. J. Mol. Sci. 2021, 22, 1923. [Google Scholar] [CrossRef]
- Zarrintaj, P.; Manouchehri, S.; Ahmadi, Z.; Saeb, M.R.; Urbanska, A.M.; Kaplan, D.L.; Mozafari, M. Agarose-based biomaterials for tissue engineering. Carbohydr. Polym. 2018, 187, 66–84. [Google Scholar] [CrossRef]
- Sivashankari, P.; Prabaharan, M. Three-dimensional porous scaffolds based on agarose/chitosan/graphene oxide composite for tissue engineering. Int. J. Biol. Macromol. 2020, 146, 222–231. [Google Scholar] [CrossRef] [PubMed]
- Gaspar, A.; Moldovan, L.; Constantin, D.; Stanciuc, A.; Boeti, P.S.; Efrimescu, I. Collagen–based scaffolds for skin tissue engineering. J. Med. Life 2011, 4, 172. [Google Scholar] [PubMed]
- Alaminos, M.; Sánchez-Quevedo, M.D.C.; Munoz-Ávila, J.I.; Serrano, D.; Medialdea, S.; Carreras, I.; Campos, A. Construction of a complete rabbit cornea substitute using a fibrin-agarose scaffold. Investig. Ophthalmol. Vis. Sci. 2006, 47, 3311–3317. [Google Scholar] [CrossRef] [PubMed]
- Ortiz-Arrabal, O.; Irastorza-Lorenzo, A.; Campos, F.; Martín-Piedra, M.Á.; Carriel, V.; Garzón, I.; Ávila-Fernández, P.; de Frutos, M.J.; Esteban, E.; Fernández, J. Fibrin and Marine-Derived Agaroses for the Generation of Human Bioartificial Tissues: An Ex Vivo and In Vivo Study. Mar. Drugs 2023, 21, 187. [Google Scholar] [CrossRef]
- Guezennec, J. Deep-sea hydrothermal vents: A new source of innovative bacterial exopolysaccharides of biotechnological interest? J. Ind. Microbiol. Biotechnol. 2002, 29, 204–208. [Google Scholar] [CrossRef]
- Matou, S.; Colliec-Jouault, S.; Galy-Fauroux, I.; Ratiskol, J.; Sinquin, C.; Guezennec, J.; Fischer, A.-M.; Helley, D. Effect of an oversulfated exopolysaccharide on angiogenesis induced by fibroblast growth factor-2 or vascular endothelial growth factor in vitro. Biochem. Pharmacol. 2005, 69, 751–759. [Google Scholar] [CrossRef]
- Merceron, C.; Portron, S.; Masson, M.; Lesoeur, J.; Fellah, B.H.; Gauthier, O.; Geffroy, O.; Weiss, P.; Guicheux, J.; Vinatier, C. The effect of two-and three-dimensional cell culture on the chondrogenic potential of human adipose-derived mesenchymal stem cells after subcutaneous transplantation with an injectable hydrogel. Cell Transpl. 2011, 20, 1575–1588. [Google Scholar] [CrossRef]
- Rederstorff, E.; Réthoré, G.; Weiss, P.; Sourice, S.; Beck-Cormier, S.; Mathieu, E.; Maillasson, M.; Jacques, Y.; Colliec-Jouault, S.; Fellah, B. Enriching a cellulose hydrogel with a biologically active marine exopolysaccharide for cell-based cartilage engineering. J. Tissue Eng. Regen. Med. 2017, 11, 1152–1164. [Google Scholar] [CrossRef]
- Rederstorff, E.; Weiss, P.; Sourice, S.; Pilet, P.; Xie, F.; Sinquin, C.; Colliec-Jouault, S.; Guicheux, J.; Laïb, S. An in vitro study of two GAG-like marine polysaccharides incorporated into injectable hydrogels for bone and cartilage tissue engineering. Acta Biomater. 2011, 7, 2119–2130. [Google Scholar] [CrossRef]
- Rougeaux, H.; Kervarec, N.; Pichon, R.; Guezennec, J. Structure of the exopolysaccharide of Vibriodiabolicus isolated from a deep-sea hydrothermal vent. Carbohydr. Res. 1999, 322, 40–45. [Google Scholar] [CrossRef]
- Zhang, Y.; Liu, W.; Li, G.; Shi, B.; Miao, Y.; Wu, X. Isolation and partial characterization of pepsin-soluble collagen from the skin of grass carp (Ctenopharyngodon idella). Food Chem. 2007, 103, 906–912. [Google Scholar] [CrossRef]
- Avila Rodríguez, M.I.; Rodríguez Barroso, L.G.; Sánchez, M.L. Collagen: A review on its sources and potential cosmetic applications. J. Cosmet. Dermatol. 2018, 17, 20–26. [Google Scholar] [CrossRef] [PubMed]
- Felician, F.F.; Xia, C.; Qi, W.; Xu, H. Collagen from marine biological sources and medical applications. Chem. Biodivers. 2018, 15, e1700557. [Google Scholar] [CrossRef]
- Langasco, R.; Cadeddu, B.; Formato, M.; Lepedda, A.J.; Cossu, M.; Giunchedi, P.; Pronzato, R.; Rassu, G.; Manconi, R.; Gavini, E. Natural collagenic skeleton of marine sponges in pharmaceutics: Innovative biomaterial for topical drug delivery. Mater. Sci. Eng. C 2017, 70, 710–720. [Google Scholar] [CrossRef]
- Coppola, D.; Oliviero, M.; Vitale, G.A.; Lauritano, C.; D’Ambra, I.; Iannace, S.; de Pascale, D. Marine collagen from alternative and sustainable sources: Extraction, processing and applications. Mar. Drugs 2020, 18, 214. [Google Scholar] [CrossRef] [PubMed]
- Jesionowski, T.; Norman, M.; Żółtowska-Aksamitowska, S.; Petrenko, I.; Joseph, Y.; Ehrlich, H. Marine spongin: Naturally prefabricated 3D scaffold-based biomaterial. Mar. Drugs 2018, 16, 88. [Google Scholar] [CrossRef] [PubMed]
- Heinemann, S.; Ehrlich, H.; Douglas, T.; Heinemann, C.; Worch, H.; Schatton, W.; Hanke, T. Ultrastructural studies on the collagen of the marine sponge Chondrosia reniformis Nardo. Biomacromolecules 2007, 8, 3452–3457. [Google Scholar] [CrossRef]
- Ramanathan, G.; Seleenmary Sobhanadhas, L.S.; Sekar Jeyakumar, G.F.; Devi, V.; Sivagnanam, U.T.; Fardim, P. Fabrication of biohybrid cellulose acetate-collagen bilayer matrices as nanofibrous spongy dressing material for wound-healing application. Biomacromolecules 2020, 21, 2512–2524. [Google Scholar] [CrossRef]
- Shi, Y.; Zhang, H.; Zhang, X.; Chen, Z.; Zhao, D.; Ma, J. A comparative study of two porous sponge scaffolds prepared by collagen derived from porcine skin and fish scales as burn wound dressings in a rabbit model. Regen. Biomater. 2020, 7, 63–70. [Google Scholar] [CrossRef]
- Burnsed, O.A.; Schwartz, Z.; Marchand, K.O.; Hyzy, S.L.; Olivares-Navarrete, R.; Boyan, B.D. Hydrogels derived from cartilage matrices promote induction of human mesenchymal stem cell chondrogenic differentiation. Acta Biomater. 2016, 43, 139–149. [Google Scholar] [CrossRef]
- Fernandes-Silva, S.; Moreira-Silva, J.; Silva, T.H.; Perez-Martin, R.I.; Sotelo, C.G.; Mano, J.F.; Duarte, A.R.C.; Reis, R.L. Porous hydrogels from shark skin collagen crosslinked under dense carbon dioxide atmosphere. Macromol. Biosci. 2013, 13, 1621–1631. [Google Scholar] [CrossRef] [PubMed]
- Sotelo, C.G.; Comesaña, M.B.; Ariza, P.R.; Pérez-Martín, R.I. Characterization of collagen from different discarded fish species of the west coast of the Iberian Peninsula. J. Aquat. Food Prod. Technol. 2016, 25, 388–399. [Google Scholar] [CrossRef]
- Diogo, G.S.; Carneiro, F.; Freitas-Ribeiro, S.; Sotelo, C.G.; Pérez-Martín, R.I.; Pirraco, R.P.; Reis, R.L.; Silva, T.H. Prionace glauca skin collagen bioengineered constructs as a promising approach to trigger cartilage regeneration. Mater. Sci. Eng. C 2021, 120, 111587. [Google Scholar] [CrossRef] [PubMed]
- Chiarelli, P.G.; Suh, J.H.; Pegg, R.B.; Chen, J.; Solval, K.M. The emergence of jellyfish collagen: A comprehensive review on research progress, industrial applications, and future opportunities. Trends Food Sci. Technol. 2023, 141, 104206. [Google Scholar] [CrossRef]
- Bonaccorsi, G.; Garamella, G.; Cavallo, G.; Lorini, C. A systematic review of risk assessment associated with jellyfish consumption as a potential novel food. Foods 2020, 9, 935. [Google Scholar] [CrossRef] [PubMed]
- Ruzicka, J.J.; Brodeur, R.D.; Emmett, R.L.; Steele, J.H.; Zamon, J.E.; Morgan, C.A.; Thomas, A.C.; Wainwright, T.C. Interannual variability in the Northern California Current food web structure: Changes in energy flow pathways and the role of forage fish, euphausiids, and jellyfish. Prog. Ocean. 2012, 102, 19–41. [Google Scholar] [CrossRef]
- Pugliano, M.; Vanbellinghen, X.; Schwinté, P.; Benkirane-Jessel, N.; Keller, L. Combined jellyfish collagen type II, human stem cells and Tgf-β3 as a therapeutic implant for cartilage repair. J. Stem Cell Res. Ther. 2017, 7, 2. [Google Scholar]
- Ullm, S.; Krüge, A.; Tondera, C.; Gebauer, T.P.; Neffe, A.T.; Lendlein, A.; Jung, F.; Pietzsch, J. Biocompatibility and inflammatory response in vitro and in vivo to gelatin-based biomaterials with tailorable elastic properties. Biomaterials. 2014, 35, 9755–9766. [Google Scholar] [CrossRef]
- Gaspar-Pintiliescu, A.; Stefan, L.M.; Anton, E.D.; Berger, D.; Matei, C.; Negreanu-Pirjol, T.; Moldovan, L. Physicochemical and biological properties of gelatin extracted from marine snail Rapana venosa. Mar. Drugs 2019, 17, 589. [Google Scholar] [CrossRef]
- Alves, A.L.; Carvalho, A.C.; Machado, I.; Diogo, G.S.; Fernandes, E.M.; Castro, V.I.; Pires, R.A.; Vázquez, J.A.; Pérez-Martín, R.I.; Alaminos, M. Cell-Laden Marine Gelatin Methacryloyl Hydrogels Enriched with Ascorbic Acid for Corneal Stroma Regeneration. Bioengineering 2023, 10, 62. [Google Scholar] [CrossRef]
- Martins, E.; Fernandes, R.; Alves, A.L.; Sousa, R.O.; Reis, R.L.; Silva, T.H. Skin byproducts of reinhardtius hippoglossoides (Greenland Halibut) as ecosustainable source of marine collagen. Appl. Sci. 2022, 12, 11282. [Google Scholar] [CrossRef]
- Machado, I.; Marques, C.F.; Martins, E.; Alves, A.L.; Reis, R.L.; Silva, T.H. Marine Gelatin-Methacryloyl-Based Hydrogels as Cell Templates for Cartilage Tissue Engineering. Polymers 2023, 15, 1674. [Google Scholar] [CrossRef] [PubMed]
- Carretero, A.; da Costa, D.S.; Reis, R.L.; Pashkuleva, I. Extracellular matrix-inspired assembly of glycosaminoglycan–collagen fibers. J. Mater. Chem. B 2017, 5, 3103–3106. [Google Scholar] [CrossRef] [PubMed]
- Reys, L.L.; Silva, S.S.; Soares da Costa, D.; Oliveira, N.M.; Mano, J.F.; Reis, R.L.; Silva, T.H. Fucoidan hydrogels photo-cross-linked with visible radiation as matrices for cell culture. ACS Biomater. Sci. Eng. 2016, 2, 1151–1161. [Google Scholar] [CrossRef] [PubMed]
- Carvalho, D.N.; López-Cebral, R.; Sousa, R.O.; Alves, A.L.; Reys, L.L.; Silva, S.S.; Oliveira, J.M.; Reis, R.L.; Silva, T.H. Marine collagen-chitosan-fucoidan cryogels as cell-laden biocomposites envisaging tissue engineering. Biomed. Mater. 2020, 15, 055030. [Google Scholar] [CrossRef]
- Carvalho, D.N.; Gelinsky, M.; Williams, D.S.; Mearns-Spragg, A.; Reis, R.L.; Silva, T.H. Marine collagen-chitosan-fucoidan/chondroitin sulfate cryo-biomaterials loaded with primary human cells envisaging cartilage tissue engineering. Int. J. Biol. Macromol. 2023, 241, 124510. [Google Scholar] [CrossRef]


| Classification | Marine Biomaterials | Reported Marine Sources | Chemical Composition | Specific Features |
|---|---|---|---|---|
| Polysaccharides | Chitin |
|
|
|
| Alginate |
| Interconnected β-D-mannuronic (M) and α-L-guluronic (G) monomers |
| |
| Chitosan |
| Linear polysaccharide consisting of D-glucosamine and N-acetylglucosamine |
| |
| κ-Carrageenan |
| Polysaccharide containing sulphate groups per disaccharide alternating G-, D-, or DA-units |
| |
| Fucoidan |
| Heteropolysaccharide with L-fucose-4-sulfate predominantly composed of extra L-fucose and sulphate groups |
| |
| Laminarin |
| Branched polysaccharide consisting of (1–3)- β-d-glucan with β (1–6)-linkages/branching |
| |
| Ulvan |
| Sulfated polysaccharide of L-rhamnose, D-xylose, D-glucose, and D-glucuronic acid |
| |
| Agarose |
| Copolymer of β-1,3-linked d-galactose and α-1,4-linked 3,6-anhydro-α-l-galactose residues |
| |
| GY785 |
| Sulfated nonasaccharide repeating unit with glucose, galactose, glucuronic acid, and galacturonic acid |
| |
| Proteins | Collagen |
| Repeating sequences of glycine–proline–hydroxyproline amino acid triplets |
|
| Gelatin |
| Hydrolyzed collagen |
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kang, M.S.; Jo, H.J.; Jang, H.J.; Kim, B.; Jung, T.G.; Han, D.-W. Recent Advances in Marine Biomaterials Tailored and Primed for the Treatment of Damaged Soft Tissues. Mar. Drugs 2023, 21, 611. https://doi.org/10.3390/md21120611
Kang MS, Jo HJ, Jang HJ, Kim B, Jung TG, Han D-W. Recent Advances in Marine Biomaterials Tailored and Primed for the Treatment of Damaged Soft Tissues. Marine Drugs. 2023; 21(12):611. https://doi.org/10.3390/md21120611
Chicago/Turabian StyleKang, Moon Sung, Hyo Jung Jo, Hee Jeong Jang, Bongju Kim, Tae Gon Jung, and Dong-Wook Han. 2023. "Recent Advances in Marine Biomaterials Tailored and Primed for the Treatment of Damaged Soft Tissues" Marine Drugs 21, no. 12: 611. https://doi.org/10.3390/md21120611
APA StyleKang, M. S., Jo, H. J., Jang, H. J., Kim, B., Jung, T. G., & Han, D.-W. (2023). Recent Advances in Marine Biomaterials Tailored and Primed for the Treatment of Damaged Soft Tissues. Marine Drugs, 21(12), 611. https://doi.org/10.3390/md21120611









