Combination Formulation of Tetrodotoxin and Lidocaine as a Potential Therapy for Severe Arrhythmias
Abstract
1. Introduction
2. Results and Discussion
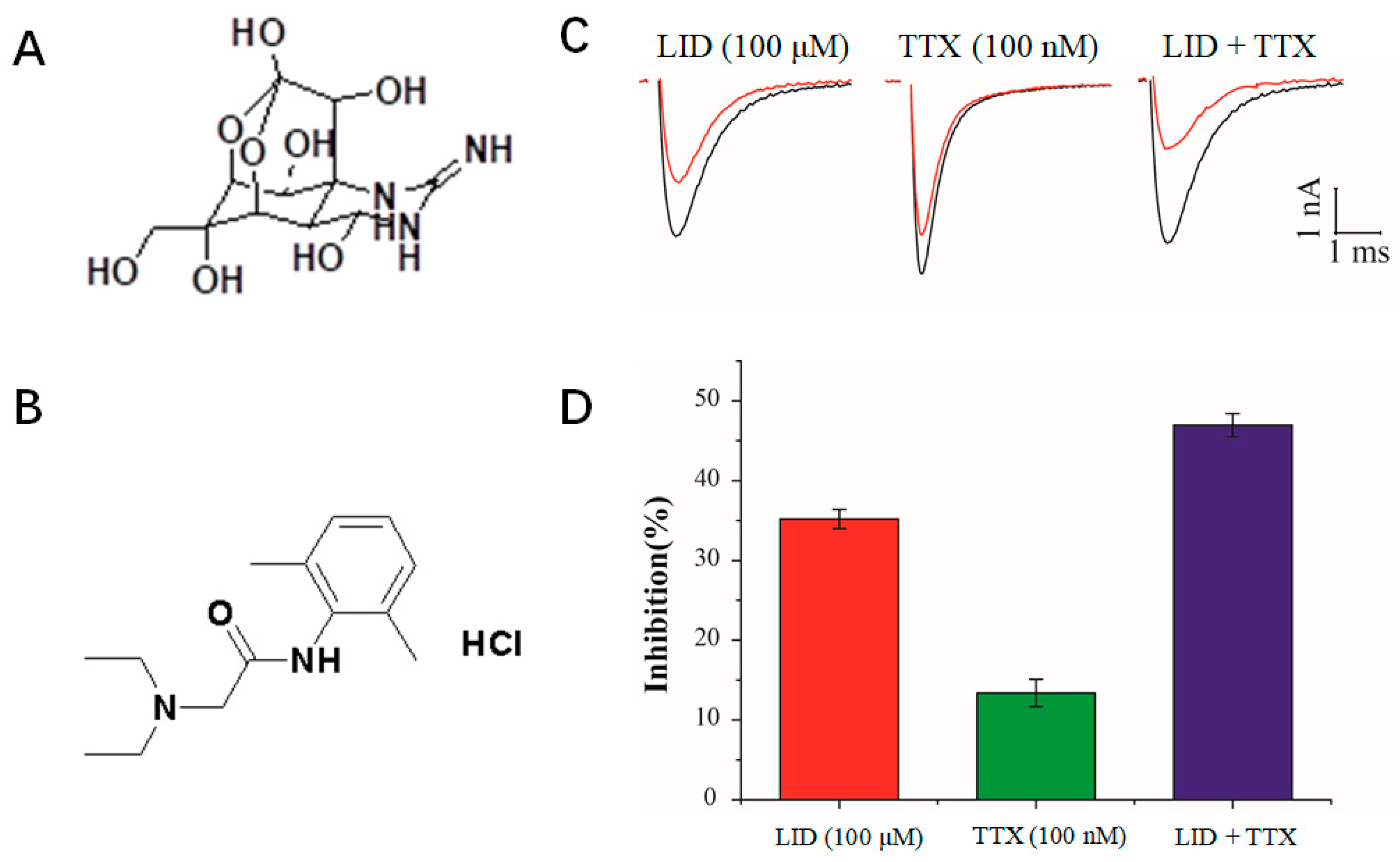
2.1. Inhibition of Nav1.5 Currents by LID, TTX and LID+TTX Mixture
2.2. HPLC Analysis of LID + TTX Formulations
2.3. Preparation and Stability of a Combination Formulation of LID + TTX
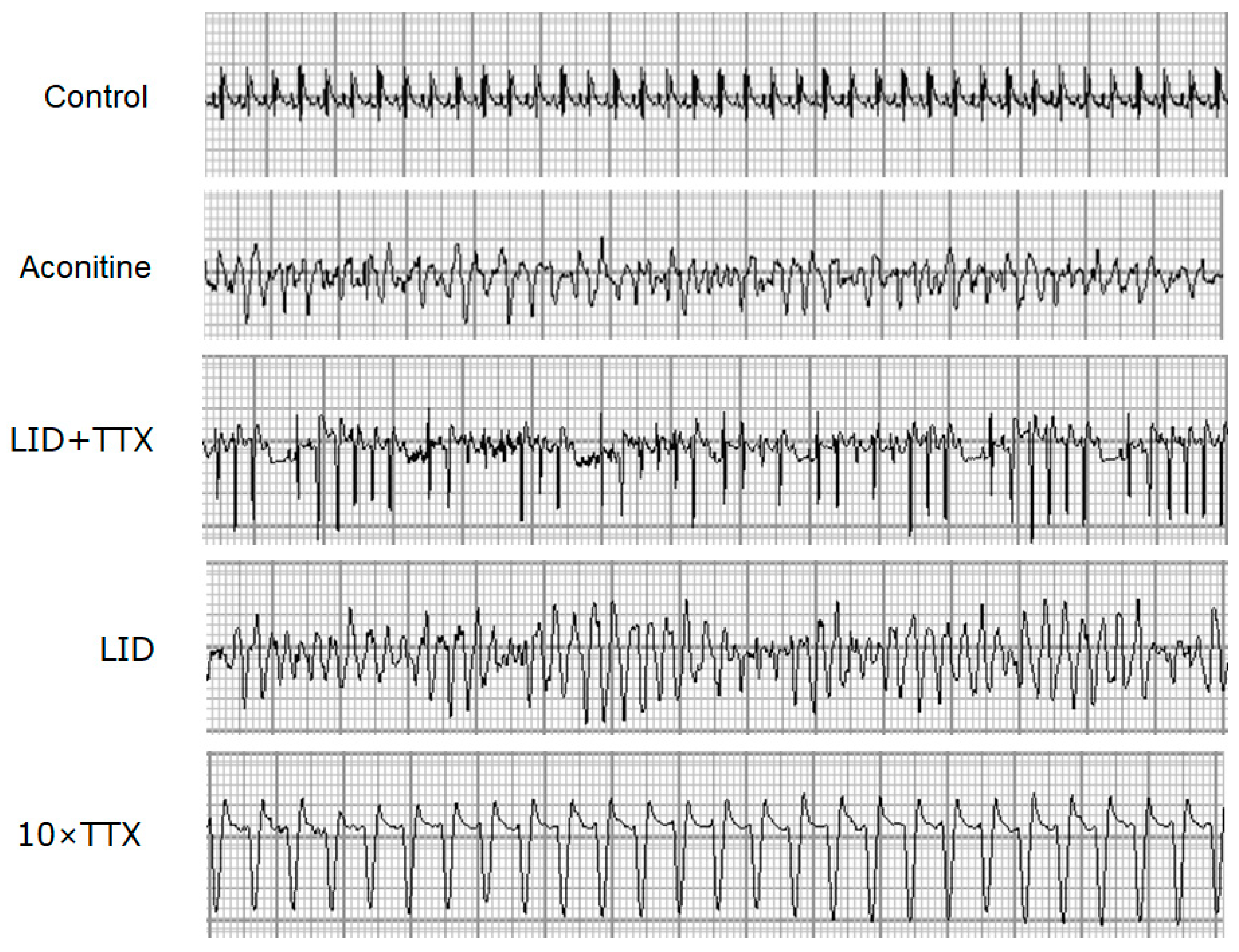
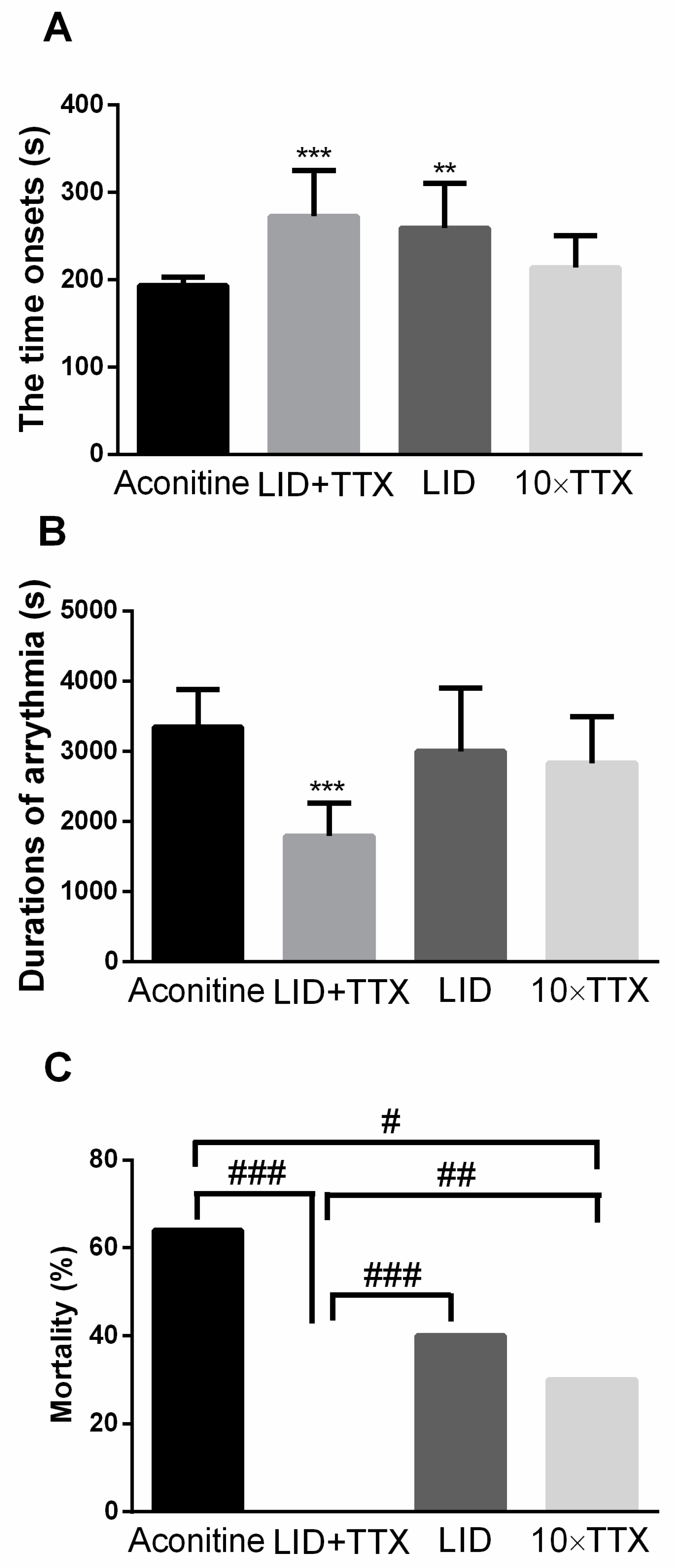
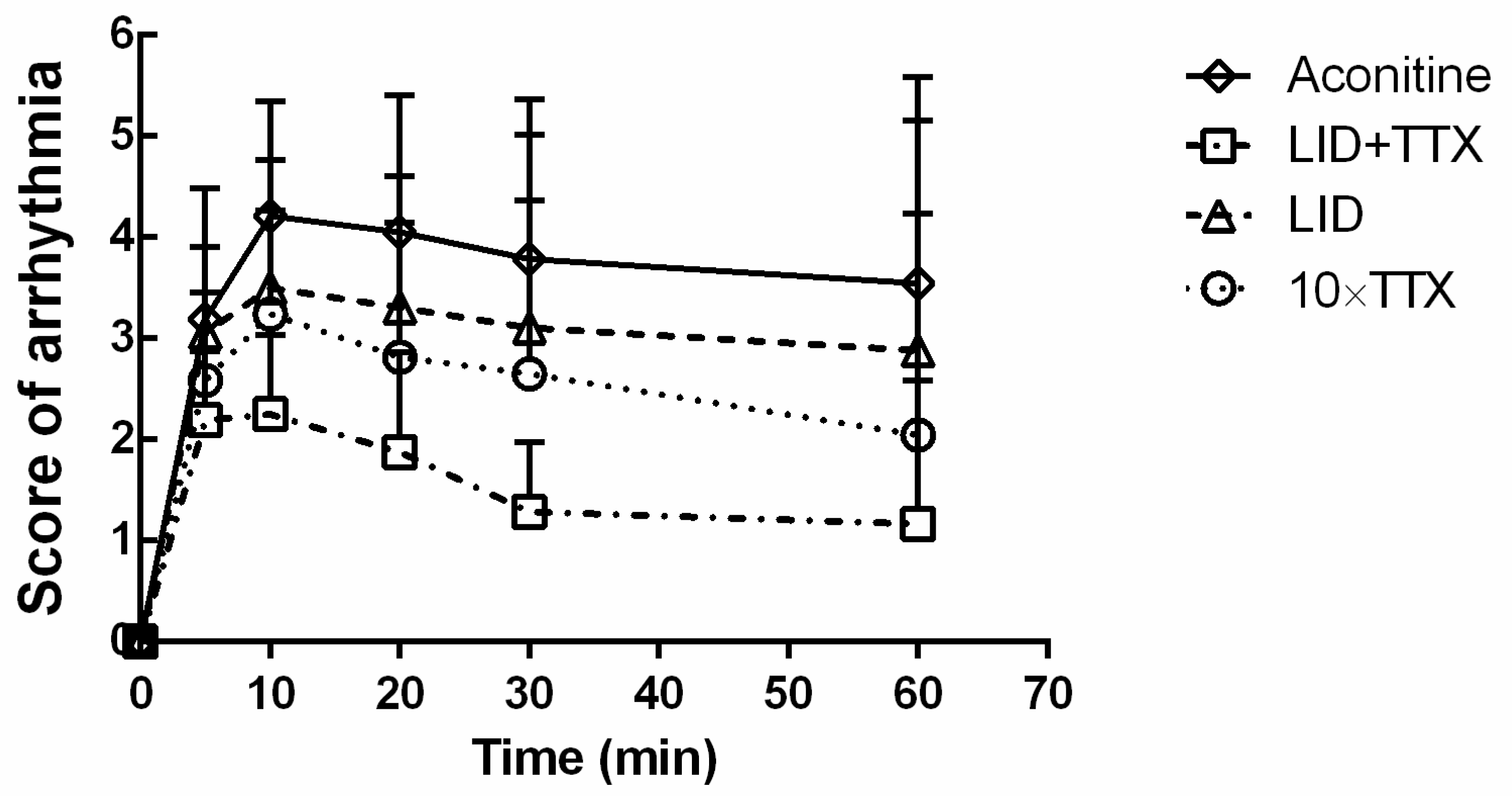
2.4. The LID + TTX Formulation Significantly Reduced Aconitine-Induced Arrhythmia and Mortality
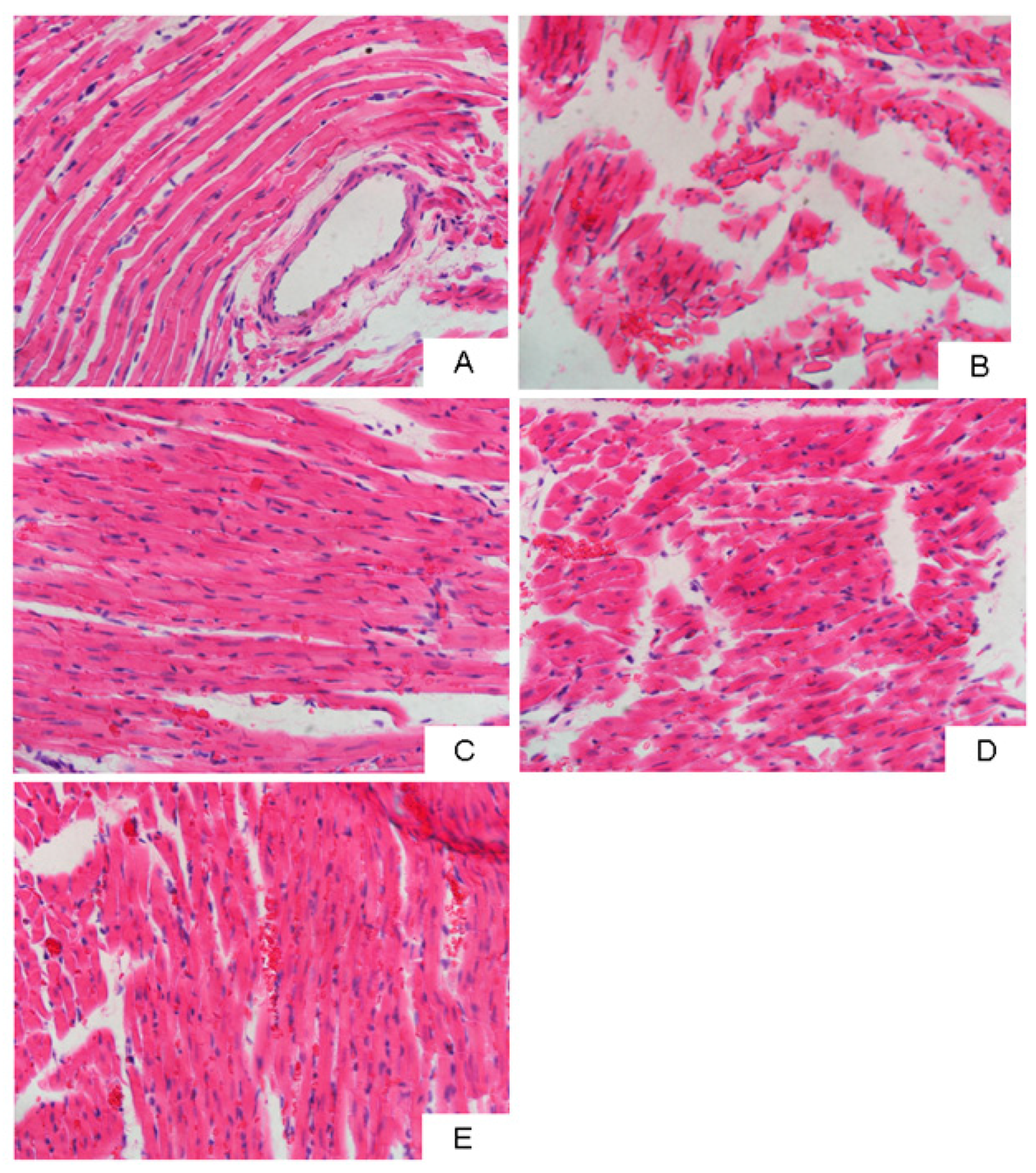
2.5. Combination of LID and TTX Significantly Reduced Aconitine-Induced Myocardial Injury
3. Materials and Methods
3.1. Drugs and Chemicals
3.2. Cell Culture
3.3. Patch Clamp Recording
3.4. Determination of TTX Content and Impurities
3.5. Determination of LID Content and Impurities
3.6. Preparation of the Formulation of TTX and LID
3.7. Stability Studies
3.8. In Vivo Experiments
3.9. Histological Assessment
3.10. Statistical Analysis
4. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Salerno, D.M.; Jeanne Fifield, R.N.; Morrison Hodges, M.D. Antiarrhythmic drug therapy for suppression of ventricular arrhythmia: Experience with 122 patients treated for two years. J. Clin. Pharmacol. 1990, 30, 226–234. [Google Scholar] [CrossRef] [PubMed]
- Johannes, C.B.; Varas-Lorenzo, C.; Mcquay, L.J.; Midkiff, K.D.; Fife, D. Risk of serious ventricular arrhythmia and sudden cardiac death in a cohort of users of domperidone: A nested case-control study. Pharmacoepidemiol. Drug Saf. 2010, 19, 881–888. [Google Scholar] [CrossRef] [PubMed]
- John, R.M.; Tedrow, U.B.; Koplan, B.A.; Albert, C.M.; Epstein, L.M.; Sweeney, M.O.; Amy Leigh, M.; Michaud, G.F.; Stevenson, W.G. Ventricular arrhythmias and sudden cardiac death. Lancet 2012, 48, 426–444. [Google Scholar] [CrossRef]
- Samarin, M.J.; Mohrien, K.M.; Oliphant, C.S. Continuous intravenous antiarrhythmic agents in the intensive care unit: Strategies for safe and effective use of amiodarone, lidocaine, and procainamide. Crit. Care Nurs. Q. 2015, 38, 329–344. [Google Scholar] [CrossRef]
- Koji, Y.; Takeshi, T.; Takahiro, T.; Ayako, O.; Takashi, M.; Hirohiko, M.; Uichi, I. Renewed impact of lidocaine on refractory ventricular arrhythmias in the amiodarone era. Int. J. Cardiol. 2014, 176, 936–940. [Google Scholar]
- Do, H.K.; Kogure, K.; Imada, C.; Noguchi, T.; Ohwada, K.; Simidu, U. Tetrodotoxin production of actinomycetes isolated from marine sediment. J. Appl. Microbiol. 2010, 70, 464–468. [Google Scholar] [CrossRef]
- Schwartz, D.M.; Duncan, K.G.; Duncan, J.L. Experimental use of tetrodotoxin for corneal pain after excimer laser keratectomy. Cornea 1998, 17, 196–199. [Google Scholar] [CrossRef]
- Schwartz, D.M.; Fields, H.L.; Duncan, K.G.; Duncan, J.L.; Jones, M.R. Experimental study of tetrodotoxin, a long-acting topical anesthetic. Am. J. Ophthalmol. 1998, 125, 481–487. [Google Scholar] [CrossRef]
- Chang, F.C.; Benton, B.J.; Salyer, J.L.; Foster, R.E.; Franz, D.R. Respiratory and cardiovascular effects of tetrodotoxin in urethane-anesthetized guinea pigs. Brain Res. 1990, 528, 259–268. [Google Scholar] [CrossRef]
- Cohen, C.J.; Bean, B.P.; Colatsky, T.J.; Tsien, R.W. Tetrodotoxin block of sodium channels in rabbit Purkinje fibers. Interactions between toxin binding and channel gating. J. Gen. Physiol. 1981, 78, 383–411. [Google Scholar] [CrossRef]
- Bernstein, M.E. Pharmacologic effects of tetrodotoxin: Cardiovascular and antiarrhythmic activities. Toxicon Off. J. Int. Soc. Toxinol. 1969, 7, 287–302. [Google Scholar] [CrossRef]
- Duff, H.J.; Sheldon, R.S.; Cannon, N.J. Tetrodotoxin: Sodium channel specific anti-arrhythmic activity. Cardiovasc. Res. 1988, 22, 800–807. [Google Scholar] [CrossRef] [PubMed]
- Abraham, S.; Beatch, G.N.; MacLeod, B.A.; Walker, M.J. Antiarrhythmic properties of tetrodotoxin against occlusion-induced arrhythmias in the rat: A novel approach to the study of the antiarrhythmic effects of ventricular sodium channel blockade. J. Pharmacol. Exp. Ther. 1989, 251, 1166–1173. [Google Scholar] [PubMed]
- Bagal, S.K.; Marron, B.E.; Owen, R.M.; Storer, R.I.; Swain, N.A. Voltage gated sodium channels as drug discovery targets. Channels 2015, 9, 360–366. [Google Scholar] [CrossRef]
- Ono, T.; Hayashida, M.; Tezuka, A.; Hayakawa, H.; Ohno, Y. Antagonistic effects of tetrodotoxin on aconitine-induced cardiac toxicity. J. Nippon Med. Sch. 2013, 80, 350–361. [Google Scholar] [CrossRef]
- Varro, A.; Nakaya, Y.; Elharrar, V.; Surawicz, B. Use-dependent effects of amiodarone on Vmax in cardiac Purkinje and ventricular muscle fibers. Eur. J. Pharmacol. 1985, 112, 419–422. [Google Scholar] [CrossRef]
- Aomine, M. Comparative effects of tetrodotoxin, lidocaine, and amiodarone on Vmax in guinea pig cardiac Purkinje and papillary muscle fibers. Gen. Pharmacol. 1989, 20, 575–579. [Google Scholar] [CrossRef]
- Rook, M.B.; Evers, M.M.; Vos, M.A.; Bierhuizen, M.F. Biology of cardiac sodium channel Nav1.5 expression. Cardiovasc. Res. 2012, 93, 12–23. [Google Scholar] [CrossRef]
- Zhorov, B.S. Structural models of ligand-bound sodium channels. Handb. Exp. Pharmacol. 2017, 246, jeb.164160. [Google Scholar]
- Nguyen, P.T.; Demarco, K.R.; Vorobyov, I.; Clancy, C.E.; Yarovyarovoy, V. Structural basis for antiarrhythmic drug interactions with the human cardiac sodium channel. Proc. Natl. Acad. Sci. USA 2019, 116, 2945–2954. [Google Scholar] [CrossRef]
- Mccormack, K.; Santos, S.; Chapman, M.L.; Krafte, D.S.; Marron, B.E.; West, C.W.; Krambis, M.J.; Antonio, B.M.; Zellmer, S.; Printzenhoff, D. Voltage sensor interaction site for selective small molecule inhibitors of voltage-gated sodium channels. Proc. Natl. Acad. Sci. USA 2013, 110, 201220844. [Google Scholar] [CrossRef] [PubMed]
- Woodward, R.B.; Gougoutas, J.Z. The Structure of Tetrodotoxin. J. Am. Chem. Soc. 1964, 86, 5030. [Google Scholar] [CrossRef]
- Goto, T.; Kishi, Y.; Takahashi, S.; Hirata, Y. Tetrodotoxin. Tetrahedron 1965, 21, 2059–2088. [Google Scholar] [CrossRef]
- Yi, R.; Chen, H.; Hong, B.; Xie, R. Freeze-Dried Powder Preparation of Tetrodotoxin and the Producing Method Thereof. C.A. Patent 2737463A1, 4 March 2010. [Google Scholar]
- Hong, K.Y. Preliminary study on the stability of tetrodotoxin injection. Chin. J. Mod. Appl. Pharm. 2003, 20, 485–487. [Google Scholar]
- Bestetti, R.B.; Baroldi, G.; Sales-Neto, V.N.; Soares, E.G.; Oliveira, J.S.M. The usefulness of the resting electrocardiogram for characterizing acute Chagas’ heart disease in the rat. Int. J. Cardiol. 1988, 18, 305–315. [Google Scholar] [CrossRef]
- Dewhurst, M.; Adeyemi, O.; Harris, J.; West, H.; Brabham, T. Application of modified ECG lead placement technique in rat telemetry safety studies; outcome and potential use. J. Pharmacol. Toxicol. Methods 2008, 58, 158. [Google Scholar] [CrossRef]
- Loeffler, R.F. Use of a telemeterized rat ECG model to identify potential non-QT cardiovascular conduction risk of compounds in early stages of development. J. Pharmacol. Toxicol. Methods 2009, 60, 239. [Google Scholar] [CrossRef]
- Kniffen, F.J.; Lomas, T.E.; Nobel-Allen, N.L.; Lucchesi, B.R. The comparative antiarrhythmic actions of lidocaine and its quarternary derivative, methyl lidocaine. Circulation 1974, 49, 264–271. [Google Scholar] [CrossRef]
- Liu, J.; Lv, X. The pharmacokinetics and pharmacodynamics of lidocaine- loaded biodegradable poly(lactic-co-glycolic acid) microspheres. Int. J. Mol. Sci. 2014, 15, 17469–17477. [Google Scholar] [CrossRef]
- Zimmer, T. Effects of tetrodotoxin on the mammalian cardiovascular system. Mar. Drugs 2010, 8, 741–762. [Google Scholar] [CrossRef]
- Benowitz, N.; Forsyth, F.P.; Melmon, K.L.; Rowland, M. Lidocaine disposition kinetics in monkey and man. I. Prediction by a perfusion model. Clin. Pharmacol. Ther. 1974, 16, 87–98. [Google Scholar] [CrossRef] [PubMed]
- Chen, W.Z.; Hong, Z.; Zhang, Y.P.; Rui-Zao, Y.I. Study on quantitative determination of tetrodotoxin by high performance liquid chromatography-fluorescent detection. Chin. J. Health Lab. Technol. 2009, 2, 261–262. [Google Scholar]
- Shan, X.; Miao, L.; Bing, H. Determination of lidocaine hydrochloride injection by HPLC. China Pharm. 2004, 12, 942–943. [Google Scholar]
| Groups | TL001 | TL002 | TL003 | TL004 | TL005 | TL006 | TL007 |
|---|---|---|---|---|---|---|---|
| TTX (mg) | 1 | 1 | 1 | 1 | 0 | 10 | 0 |
| LID (g) | 5 | 5 | 5 | 5 | 5 | 0 | 0 |
| Mannitol (g) | 0 | 0 | 6 | 6 | 6 | 6 | 6 |
| Hydroxypropyl- beta-cyclodextrin (g) | 10 | 0 | 0 | 4 | 0 | 0 | 0 |
| Dextran 40 (g) | 0 | 10 | 4 | 0 | 4 | 4 | 4 |
| Groups | Appearance | Content (%) | Total Impurities (%) | |||
|---|---|---|---|---|---|---|
| (40 °C, 75%/25 °C, 90%) | TTX | LID | TTX | LID | ||
| TL001 | 0 day | White, cake shaped | 99.16/99.16 | 99.91/99.91 | 0.94/0.94 | 0.10/0.10 |
| 5 days | Partly shrunk/White, cake shaped | 98.90/99.13 | 99.89/99.89 | 1.15/0.81 | 0.10/0.10 | |
| 10 days | Completely shrunk/White, cake shaped | 98.75/99.14 | 99.90/99.89 | 1.20/0.81 | 0.10/0.10 | |
| TL002 | 0 day | White, cake shaped | 99.30/99.30 | 99.89/99.89 | 0.76/0.76 | 0.10/0.10 |
| 5 days | Partly shrunk/White, cake shaped | 98.61/99.19 | 99.88/99.89 | 1.40/0.80 | 0.10/0.11 | |
| 10 days | Completely shrunk/White, cake shaped | 98.40/99.24 | 99.90/99.87 | 1.67/0.89 | 0.30/0.11 | |
| TL003 | 0 day | White, cake shaped | 98.95/98.95 | 99.90/99.90 | 1.32/1.32 | 0.11/0.11 |
| 5 days | White, cake shaped | 98.11/98.76 | 99.88/99.90 | 1.74/1.34 | 0.12/0.11 | |
| 10 days | White, cake shaped | 97.64/98.64 | 99.88/99.88 | 1.87/1.43 | 0.12/0.12 | |
| TL004 | 0 day | White, cake shaped | 99.22/99.22 | 99.90/99.90 | 0.96/0.96 | 0.10/0.10 |
| 5 days | White, cake shaped | 98.67/98.66 | 99.90/99.89 | 1.39/1.34 | 0.11/0.11 | |
| 10 days | White, cake shaped | 97.96/98.56 | 99.86/99.89 | 2.35/1.45 | 0.13/0.11 | |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hong, B.; He, J.; Le, Q.; Bai, K.; Chen, Y.; Huang, W. Combination Formulation of Tetrodotoxin and Lidocaine as a Potential Therapy for Severe Arrhythmias. Mar. Drugs 2019, 17, 685. https://doi.org/10.3390/md17120685
Hong B, He J, Le Q, Bai K, Chen Y, Huang W. Combination Formulation of Tetrodotoxin and Lidocaine as a Potential Therapy for Severe Arrhythmias. Marine Drugs. 2019; 17(12):685. https://doi.org/10.3390/md17120685
Chicago/Turabian StyleHong, Bihong, Jianlin He, Qingqing Le, Kaikai Bai, Yongqiang Chen, and Wenwen Huang. 2019. "Combination Formulation of Tetrodotoxin and Lidocaine as a Potential Therapy for Severe Arrhythmias" Marine Drugs 17, no. 12: 685. https://doi.org/10.3390/md17120685
APA StyleHong, B., He, J., Le, Q., Bai, K., Chen, Y., & Huang, W. (2019). Combination Formulation of Tetrodotoxin and Lidocaine as a Potential Therapy for Severe Arrhythmias. Marine Drugs, 17(12), 685. https://doi.org/10.3390/md17120685






