Autonomic Nervous System Dysfunction in Diabetic Patients After Myocardial Infarction: Prognostic Role of the Valsalva Maneuver
Abstract
1. Introduction
2. Materials and Methods
Statistical Analysis
3. Results
4. Discussion
Study Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Byrne, R.A.; Rossello, X.; Coughlan, J.J.; Barbato, E.; Berry, C.; Chieffo, A.; Claeys, M.J.; Dan, G.A.; Dweck, M.R.; Galbraith, M.; et al. 2023 ESC Guidelines for the management of acute coronary syndromes. Eur. Heart J. 2023, 44, 3720–3826. [Google Scholar] [CrossRef]
- Kasim, S.; Amir Rudin, P.N.F.; Malek, S.; Aziz, F.; Wan Ahmad, W.A.; Ibrahim, K.S.; Hamidi, M.H.M.; Shariff, R.E.R.; Fong, A.Y.Y.; Song, C. Data analytics approach for short- and long-term mortality prediction following acute non-ST-elevation myocardial infarction (NSTEMI) and Unstable Angina (UA) in Asians. PLoS ONE 2024, 19, e0298036. [Google Scholar] [CrossRef] [PubMed]
- Hwang, S.Y.; Kim, S.H.; Uhm, I.A.; Shin, J.H.; Lim, Y.H. Prognostic implications for patients after myocardial infarction: An integrative literature review and in-depth interviews with patients and experts. BMC Cardiovasc. Disord. 2022, 22, 348. [Google Scholar] [CrossRef]
- Marx, N.; Federici, M.; Schütt, K.; Müller-Wieland, D.; Ajjan, R.A.; Antunes, M.J.; Christodorescu, R.M.; Crawford, C.; Di Angelantonio, E.; Eliasson, B.; et al. 2023 ESC Guidelines for the management of cardiovascular disease in patients with diabetes. Eur. Heart J. 2023, 44, 4043–4140, Erratum in Eur. Heart J. 2023, 44, 5060. https://doi.org/10.1093/eurheartj/ehad774.. [Google Scholar] [CrossRef]
- Kerkmeijer, L.S.; Farhan, S.; Mehran, R.; Dangas, G.D. Diabetes mellitus and multivessel coronary artery disease: An ongoing battle for an ideal treatment strategy. Ann. Transl. Med. 2017, 5, 261. [Google Scholar] [CrossRef]
- Eleftheriadou, A.; Spallone, V.; Tahrani, A.A.; Alam, U. Cardiovascular autonomic neuropathy in diabetes: An update with a focus on management. Diabetologia 2024, 67, 2611–2625. [Google Scholar] [CrossRef]
- Vinik, A.I.; Ziegler, D. Diabetic cardiovascular autonomic neuropathy. Circulation 2007, 115, 387–397. [Google Scholar] [CrossRef]
- Theofilis, P.; Antonopoulos, A.S.; Sagris, M.; Papanikolaou, A.; Oikonomou, E.; Tsioufis, K.; Tousoulis, D. Silent Myocardial Ischemia: From Pathophysiology to Diagnosis and Treatment. Biomedicines 2024, 12, 259. [Google Scholar] [CrossRef]
- Goldberger, J.J.; Arora, R.; Buckley, U.; Shivkumar, K. Autonomic Nervous System Dysfunction: JACC Focus Seminar. J. Am. Coll. Cardiol. 2019, 73, 1189–1206. [Google Scholar] [CrossRef] [PubMed]
- Rajendran, P.S.; Nakamura, K.; Ajijola, O.A.; Vaseghi, M.; Armour, J.A.; Ardell, J.L.; Shivkumar, K. Myocardial infarction induces structural and functional remodelling of the intrinsic cardiac nervous system. J. Physiol. 2016, 594, 321–341. [Google Scholar] [CrossRef] [PubMed]
- Zipes, D.P.; Jalife, J.; Stevenson, W.G. (Eds.) Cardiac Electrophysiology: From Cell to Bedside, 7th ed.; Elsevier: Philadelphia, PA, USA, 2018; p. 1. [Google Scholar]
- Hayano, J.; Ueda, N.; Kisohara, M.; Yuda, E.; Carney, R.M.; Blumenthal, J.A. Survival Predictors of Heart Rate Variability After Myocardial Infarction with and Without Low Left Ventricular Ejection Fraction. Front. Neurosci. 2021, 15, 610955. [Google Scholar] [CrossRef]
- Rizas, K.D.; Eick, C.; Doller, A.J.; Hamm, W.; Von Stuelpnagel, L.; Zuern, C.S.; Barthel, P.; Schmidt, G.; Bauer, A. Bedside autonomic risk stratification after myocardial infarction by means of short-term deceleration capacity of heart rate. EP Eur. 2018, 20, f129–f136. [Google Scholar] [CrossRef]
- Abramkin, D.V.; Iavelov, I.S.; Gratsianskiĭ, N.A. Simple cardiovascular reflex test during hospitalization due to myocardial infarction predicts sudden but not non-sudden cardiac death during 2 years follow up. Kardiologiia 2004, 44, 37–46. [Google Scholar] [PubMed]
- Ren, L.; Fang, X.; Wang, Y.; Qi, G. T-wave alternans and heart rate variability: A comparison in patients with myocardial infarction with or without diabetes mellitus. Ann. Noninvasive Electrocardiol. 2011, 16, 232–238. [Google Scholar] [CrossRef]
- Stoičkov, V.; Deljanin-Ilić, M.; Stojanović, D.; Ilić, S.; Šarić, S.; Petrović, D.; Kostić, T.; Cvetković, J.; Stojanović, S.; Golubović, M. The influence of type 2 diabetes mellitus on the frequency and complexity of ventricular arrhythmias and heart rate variability in patients after myocardial infarction. Vojn. Pregl. 2016, 73, 1050–1055. [Google Scholar] [CrossRef] [PubMed]
- Windecker, S.; Hernández-Antolín, R.A.; Stefanini, G.G.; Wijns, W.; Zamorano, J.L. Management of ST-elevation myocardial infarction according to European and American guidelines. EuroIntervention 2014, 10, T23–T31. [Google Scholar] [CrossRef] [PubMed]
- Silva, F.M.; Pesaro, A.E.; Franken, M.; Wajngarten, M. Acute management of unstable angina and non-ST segment elevation myocardial infarction. Einstein 2015, 13, 454–461. [Google Scholar] [CrossRef]
- Chengode, S. Left ventricular global systolic function assessment by echocardiography. Ann. Card. Anaesth. 2016, 19, S26–S34. [Google Scholar] [CrossRef]
- Ewing, D.J.; Clarke, B.F. Diagnosis and management of diabetic autonomic neuropathy. Br. Med. J. (Clin. Res. Ed.) 1982, 285, 916–918. [Google Scholar] [CrossRef]
- Bellavere, F.; Bosello, G.; Fedele, D.; Cardone, C.; Ferri, M. Diagnosis and management of diabetic autonomic neuropathy. Br. Med. J. (Clin. Res. Ed.) 1983, 287, 61. [Google Scholar] [CrossRef]
- Milcent, C.; Dormont, B.; Durand-Zaleski, I.; Steg, P.G. Gender differences in hospital mortality and use of percutaneous coronary intervention in acute myocardial infarction: Microsimulation analysis of the 1999 nationwide French hospitals database. Circulation 2007, 115, 833–839. [Google Scholar] [CrossRef] [PubMed]
- Bouisset, F.; Bataille, V.; Schiele, F.; Puymirat, E.; Fayol, A.; Simon, T.; Danchin, N.; Ferrières, J. Type 2 diabetes mellitus in acute myocardial infarction: A persistent significant burden on long-term mortality. Front. Cardiovasc. Med. 2024, 11, 1401569. [Google Scholar] [CrossRef]
- Serhiyenko, V.A.; Serhiyenko, A.A. Cardiac autonomic neuropathy: Risk factors, diagnosis and treatment. World J. Diabetes 2018, 9, 1–24. [Google Scholar] [CrossRef] [PubMed]
- Hall, J.E.; Hall, M.E.; Guyton, A.C. Guyton and Hall Textbook of Medical Physiology, 14th ed.; Elsevier: Philadelphia, PA, USA, 2021; p. 1132. [Google Scholar]
- Raje, S.; Maiya, G.A.; Ramachandran, P.; Prabhu, M.A.; Nayak, K.; Shivashankara, K.N.; Shastry, B.A.; Nataraj, M.; Mayya, S.S. Prediction of cardiac autonomic dysfunction using heart rate response to deep breathing test among type 2 diabetes mellitus. BMC Endocr. Disord. 2025, 25, 117. [Google Scholar] [CrossRef] [PubMed]
- Rueda-Ochoa, O.L.; Osorio-Romero, L.F.; Sanchez-Mendez, L.D. Which indices of heart rate variability are the best predictors of mortality after acute myocardial infarction? Meta-analysis of observational studies. J. Electrocardiol. 2024, 84, 42–48. [Google Scholar] [CrossRef]
- Nolan, J.; Batin, P.D.; Andrews, R.; Lindsay, S.J.; Brooksby, P.; Mullen, M.; Baig, W.; Flapan, A.D.; Cowley, A.; Prescott, R.J.; et al. Prospective study of heart rate variability and mortality in chronic heart failure: Results of the United Kingdom heart failure evaluation and assessment of risk trial (UK-heart). Circulation 1998, 98, 1510–1516. [Google Scholar] [CrossRef]
- Li, C.; Meng, X.; Pan, Y.; Li, Z.; Wang, M.; Wang, Y. The Association Between Heart Rate Variability and 90-Day Prognosis in Patients With Transient Ischemic Attack and Minor Stroke. Front. Neurol. 2021, 12, 636474. [Google Scholar] [CrossRef]
- Shaffer, F.; Ginsberg, J.P. An Overview of Heart Rate Variability Metrics and Norms. Front. Public Health 2017, 5, 258. [Google Scholar] [CrossRef]
- Jha, R.K.; Acharya, A.; Nepal, O. Autonomic Influence on Heart Rate for Deep Breathing and Valsalva Maneuver in Healthy Subjects. JNMA J. Nepal Med. Assoc. 2018, 56, 670–673. [Google Scholar] [CrossRef]
- Low, P.A.; Benarroch, E.E. Clinical Autonomic Disorders, 3rd ed.; Wolters Kluwer Health: Philadelphia, PA, USA, 2008; p. 808. [Google Scholar]
- Cui, J.; Gao, Z.; Blaha, C.; Herr, M.D.; Mast, J.; Sinoway, L.I. Distension of central great vein decreases sympathetic outflow in humans. Am. J. Physiol.-Heart Circ. Physiol. 2013, 305, H378–H385. [Google Scholar] [CrossRef]
- Koeppen, B.M. Berne and Levy Physiology E-Book, 8th ed.; Elsevier: Philadelphia, PA, USA, 2023; p. 1. [Google Scholar]
- Huynh, T.; Perron, S.; O’Loughlin, J.; Joseph, L.; Labrecque, M.; Tu, J.V.; Théroux, P. Comparison of Primary Percutaneous Coronary Intervention and Fibrinolytic Therapy in ST-Segment-Elevation Myocardial Infarction: Bayesian Hierarchical Meta-Analyses of Randomized Controlled Trials and Observational Studies. Circulation 2009, 119, 3101–3109. [Google Scholar] [CrossRef] [PubMed]
- Fox, K.; Poole-Wilson, P.; Henderson, R.; Clayton, T.; Chamberlain, D.; Shaw, T.; Wheatley, D.J.; Pocock, S.J.; for the Randomized Intervention Trial of unstable Angina (RITA) investigators. Interventional versus conservative treatment for patients with unstable angina or non-ST-elevation myocardial infarction: The British Heart Foundation RITA 3 randomised trial. Lancet 2002, 360, 743–751. [Google Scholar] [CrossRef]
- Task Force of the European Society of Cardiology and the North American Society of Pacing and Electrophysiology. Heart rate variability: Standards of measurement, physiological interpretation and clinical use. Circulation 1996, 93, 1043–1065. [Google Scholar] [CrossRef]
- Sehgal, D.; Bonifanti, L.; Tran, J.; Lound, M.; Manfredi, A.; Mayrovitz, H.N. The Effects of Hypertension Treatment on Heart Rate Variability: A Scoping Review. Cureus 2025, 17, e91659. [Google Scholar] [CrossRef]
- Nguyen, T.M.; Melichova, D.; Aabel, E.W.; Lie, Ø.H.; Klæboe, L.G.; Grenne, B.; Sjøli, B.; Brunvand, H.; Haugaa, K.; Edvardsen, T. Mortality in Patients with Acute Coronary Syndrome—A Prospective 5-Year Follow-Up Study. J. Clin. Med. 2023, 12, 6598. [Google Scholar] [CrossRef]
- Baumann, A.A.W.; Mishra, A.; Worthley, M.I.; Nelson, A.J.; Psaltis, P.J. Management of multivessel coronary artery disease in patients with non-ST-elevation myocardial infarction: A complex path to precision medicine. Ther. Adv. Chronic Dis. 2020, 11, 2040622320938527. [Google Scholar] [CrossRef] [PubMed]
- Cole, A.; Weight, N.; Misra, S.; Grapsa, J.; Rutter, M.K.; Siudak, Z.; Moledina, S.; Kontopantelis, E.; Khunti, K.; Mamas, M.A. Addressing disparities in the long-term mortality risk in individuals with non-ST segment myocardial infarction (NSTEMI) by diabetes mellitus status: A nationwide cohort study. Diabetologia 2024, 67, 2711–2725. [Google Scholar] [CrossRef]
- Echouffo-Tcheugui, J.B.; Kolte, D.; Khera, S.; Aronow, H.D.; Abbott, J.D.; Bhatt, D.L.; Fonarow, G.C. Diabetes Mellitus and Cardiogenic Shock Complicating Acute Myocardial Infarction. Am. J. Med. 2018, 131, 778–786.e1. [Google Scholar] [CrossRef] [PubMed]
- Luo, C.; Chen, F.; Liu, L.; Ge, Z.; Feng, C.; Chen, Y. Impact of diabetes on outcomes of cardiogenic shock: A systematic review and meta-analysis. Diab. Vasc. Dis. Res. 2022, 19, 14791641221132242. [Google Scholar] [CrossRef]
| 1. MI/DM N = 93 | 2. MI N = 229 | 3. DM N = 53 | p Value | |
|---|---|---|---|---|
| Basic characteristics of study population | ||||
| Age (yrs.) (mean ± SD) | 63.3 ± 8.6 2,3 | 58.9 ± 9.9 1,3 | 53.6 ± 10.7 1,2 | <0.001 a |
| Male (n,%) | 56 (60.2%) | 158 (69%) | 31 (58.5%) | 0.171 b |
| Previous MI (n,%) | 13 (14%) | 27 (11.8%) | 0.590 b | |
| Treatment strategy | ||||
| Fibrinolytic therapy | 27 (29%) | 76 (33.2%) | 0.469 b | |
| Clinical status at admission | ||||
| AS MI (n,%) | 38 (40.9%) | 67 (29.3%) | 0.203 b | |
| IP MI (n,%) | 38 (40.9%) | 119 (52%) | ||
| NSTEMI (n,%) | 15 (16.1%) | 36 (15.7%) | ||
| Other loc. (n,%) | 2 (2.2%) | 7 (3.1%) | ||
| Killip I (n,%) | 51 (61.3%) | 160 (69.9%) | 0.128 c | |
| Killip II (n,%) | 28 (30.1%) | 58 (25.3%) | ||
| Killip III (n,%) | 8 (8.6%) | 8 (3.5%) | ||
| Killip IV (n,%) | 0 | 3 (1.3%) | ||
| BBB (n,%) | 7 (7.5%) | 29 (12.7%) | 0.185 b | |
| VF (n,%) | 3 (3.2%) | 12 (5.2%) | 0.567 b | |
| VT (n,%) | 17 (17.2%) | 45 (19.7%) | 0.612 b | |
| A.fib (n,%) | 11 (11.8%) | 17 (7.4%) | 0.204 b | |
| AV block gr. I (n,%) | 5 (5.4%) | 19 (8.3%) | 0.366 b | |
| AV block gr. II–III (n,%) | 5 (5.4%) | 13 (5.7%) | 0.915 b | |
| Echocardiography | ||||
| EF (%) (mean ± SD) | 47.8 + 11 | 49.2 ± 12.3 | 0.351 a | |
| 1. MI/DM N = 93 | 2. MI N = 229 | 3. DM N = 53 | p Value | |
|---|---|---|---|---|
| Abnormal HGT (n,%) | 69 (74.2%) | 177 (77.3%) | 49 (92.5%) | 0.025 a |
| OH (n,%) | 18 (19.4%) | 31 (13.5%) | 6 (11.3%) | 0.310 a |
| DS (n,%) | 75 (80.6%) | 181 (79%) | 50 (94.3%) | 0.034 a |
| Abnormal VM (n,%) | 45 (48.4%) | 111 (48.5%) | 20 (37.7%) | 0.351 a |
| HRB (n,%) | 69 (74.2%) 2,3 | 137 (59.8%) 1,3 | 22 (41.5%) 1,2 | <0.001 a |
| HRS (n,%) | 70 (75.3%) | 156 (68.1%) | 39 (73.6%) | 0.390 a |
| Without DP (n,%) | 1 (1.1%) 2,3 | 18 (7.9%)1,3 | 9 (17%) 1,2 | 0.002 a |
| Early DP (n,%) | 20 (21.5%) | 73 (31.9%) | 19 (35.8%) | 0.159 a |
| Definite DP (n,%) | 71 (76.3%) 2,3 | 138 (60.3%) 1 | 25 (47.2%) 1 | 0.001 a |
| CAN (n,%) | 74 (79.6%) | 166 (72.5%) | 43 (81.1%) | 0.239 a |
| Score of AN (mean ± SD) | 6.9 ± 1.6 2 | 6.2 ± 1.9 1 | 6.3 ± 2 | 0.011 b |
| 1. MI/DM N = 93 | 2. MI N = 229 | 3. DM N = 53 | p Value | |
|---|---|---|---|---|
| Mean HR (bpm) (mean ± SD) | 71.8 ± 10.9 3 | 70.6 ± 10.4 3 | 76.4 ± 9.4 1,2 | 0.004 a |
| SDNN (ms) (mean ± SD) | 93.7 ± 34.6 1,2 | 104.4 ± 39 1,3 | 135.2 ± 35.4 1,2 | <0.001 a |
| SDANN (ms) (Mdn (IQR)) | 79 (57–99.5) 3 | 87.5 (68–109) 3 | 124 (96–147) 1,2 | <0.001 b |
| RMSSD (ms) (Mdn (IQR)) | 41 (26.5–62) | 47 (29–75.5) | 47 (34.3–68) | 0.226 b |
| LF (ms2) Mdn (IQR) | 1030 (385.3–2770.1) | 1751.3 (704.5–4225.5) | 1776.3 (491–3312.2) | 0.034 b |
| HF (ms2) Mdn (IQR) | 336.1 (99.8–861.2) | 441.1 (159.7–1337.5) | 428.3 (169.8–1270.4) | 0.118 b |
| LF/HF (mean ± SD) | 3.7 ± 1.9 | 3.9 ± 1.7 | 3.6 ± 1.6 | 0.415 a |
| MI/DM Died N = 16 | MI/DM Survived N = 77 | p Value | |
|---|---|---|---|
| Abnormal HGT (n,%) | 11 (68.8%) | 58 (75.3%) | 0.549 a |
| OH (n,%) | 1 (6.3%) | 17 (22.1%) | 0.183 a |
| DS (n,%) | 12 (75%) | 63 (81.8%) | 0.503 a |
| Abnormal VM (n,%) | 12 (75%) | 33 (42.9%) | 0.019 b |
| HRB (n,%) | 13 (81.3%) | 56 (72.7%) | 0.754 a |
| HRS (n,%) | 11 (68.8%) | 59 (76.9%) | 0.532 a |
| Without DP (n,%) | 0 | 1 (1.3%) | 1.000 a |
| Early DP (n,%) | 2 (12.5%) | 19 (24.7%) | 0.511 a |
| Definite DP (n,%) | 14 (87.5%) | 57 (74%) | 0.342 a |
| CAN (n,%) | 12 (75%) | 62 (80.5%) | 0.734 a |
| Score of AN (mean ± SD) | 6.8 ± 1.3 | 6.9 ± 1.6 | 0.893 c |
| N (%) of Patients | Mean Survival (Months) (95 CI%) | Univariable HR (95% CI) | Multivariable HR (95% CI) | |
|---|---|---|---|---|
| Basic characteristics of study population | ||||
| Age (yrs.) | 1.054 (0.990–1.123) | |||
| Age (<65 yrs.) | 6 (13.6%) | 52.5 (47–58) | 1 | |
| Age (≥65 yrs.) | 10 (20.4%) | 49.5 (43.8–55.2) | 1.630 (0.591–4.495) | |
| Treatment strategy | ||||
| Conservative treatment | 14 (21.2%) | 49.4 (44.4–54.3) | 1 | |
| Fibrinolytic therapy | 2 (7.4%) | 56 (50.7–61.3) | 0.344 (0.078–1.516) | |
| Clinical status at admission | ||||
| AS MI | 3 (7.9%) | 55.6 (50.8–60.4) | 1 | 1 |
| IP MI | 8 (21.1%) | 50.7 (44.8–56.5) | 2.376 (0.630–8.959) | 2.351 (0.624–8.861) |
| NSTEMI | 5 (33.3) | 41.1 (28.5–53.7) | 5.257 (1.251–22.088) * | 6.029 (1.424–25.534) * |
| Other loc. | 0 | |||
| Killip I | 8 (14%) | 52.6 (47.9–57.4) | 1 | |
| Killip II | 4 (14.3%) | 52.1 (45–59.2) | 1.080 (0.325–3.592) | |
| Killip III | 4 (50%) | 37.9 (22.8–53) | 3.971 (1.193–13.213) * | |
| Echocardiography | ||||
| EF (%) | 0.997 (0.949–1.047) | |||
| EF (>40%) | 12 (18.2%) | 50.8 (46.1–55.5) | 1 | |
| EF (≤40%) | 4 (14.8%) | 52 (44.8–59.1) | 0.815 (0.263–2.526) | |
| 24 h Holter ECG | ||||
| Mean Heart rate (bpm) | 1.022 (0.974–1.072) | |||
| Mean Heart rate (<60/min) | 5 (33.3%) | 44.8 (33.6–56.1) | 1 | |
| Mean Heart rate (60–80/min) | 7 (11.9%) | 54.1 (50–58.2) | 2.872 (0.911–9.053) | |
| Mean Heart rate (>80/min) | 4 (21.6%) | 47 (35.8–58.1) | 2.402 (0.700–8.249) | |
| CART | ||||
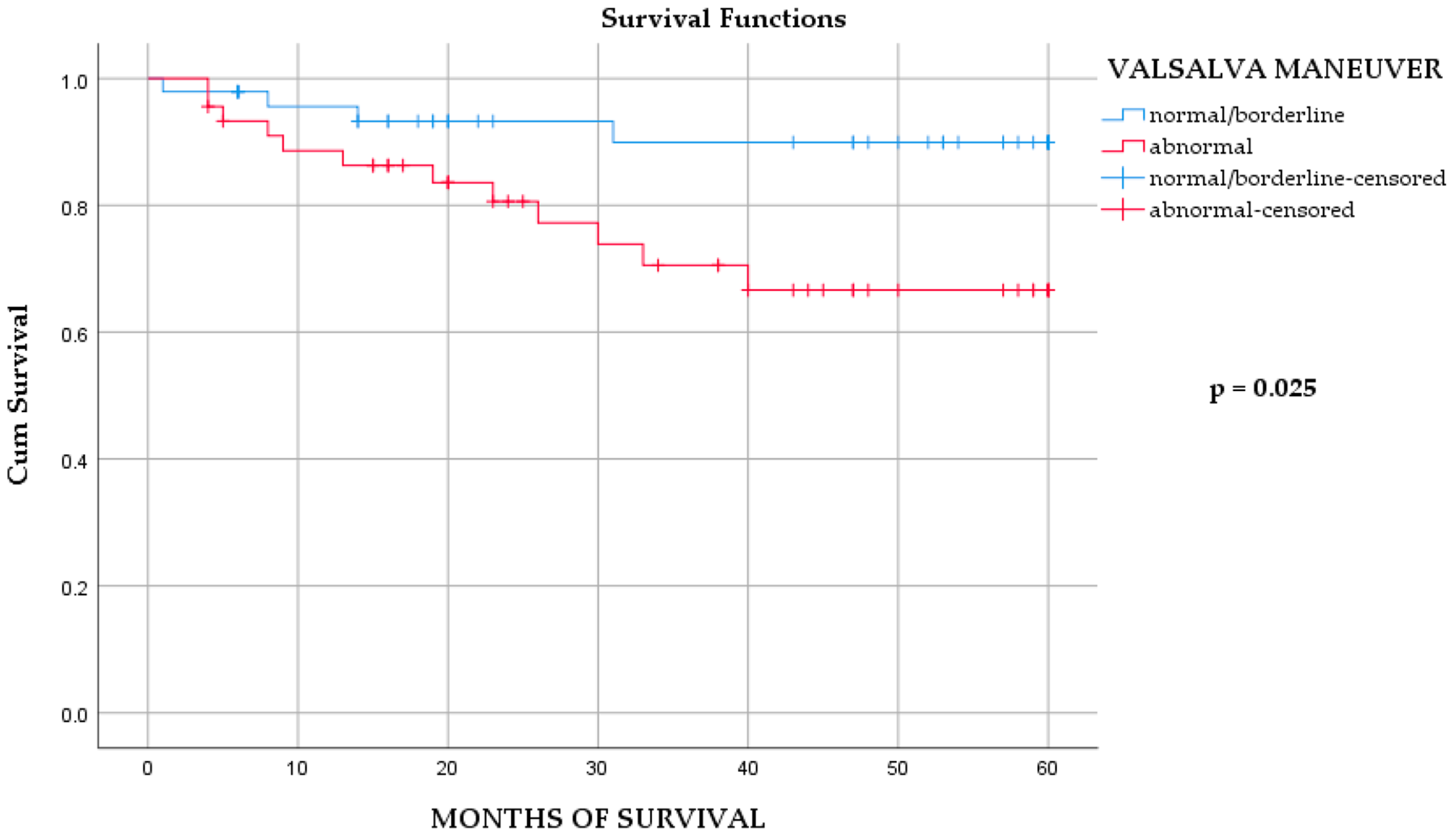
| VM (normal) | 4 (8.3%) | 55.5 (51.3–59.7) | 1 | |
| VM (abnormal) | 12 (26.7%) | 46.7 (40.3–53.1) | 3.390 (1.092–10.521) * | 3.713 (1.188–11.601) * |
| HRB (normal) | 3 (12.5%) | 53.8 (47.2–60.3) | 1 | |
| HRB (abnormal) | 13 (18.8%) | 50.3 (45.5–55) | 1.456 (0.415–5.110) | |
| HRS (normal) | 5 (21.7%) | 49.3 (40.9–57.6) | 1 | |
| HRS (abnormal) | 11 (15.7%) | 52 (47.6–56.3) | 0.723 (0.251–2.084) | |
| OH (normal) | 15 (20%) | 50.1 (45.6–54.6) | 1 | |
| OH (abnormal) | 1 (5.6%) | 56.4 (49.7–63) | 0.323 (0.043–2.448) | |
| HGT (normal) | 5 (20.8%) | 50.9 (43.6–58.1) | 1 | |
| HGT (abnormal) | 11 (15.9%) | 51.4 (46.7–56) | 0.937 (0.325–2.702) | |
| Without DS | 4 (22.2%) | 49.7 (40.8–58.7) | 1 | |
| With DS | 12 (16%) | 51.5 (47.2–55.9) | 0.846 (0.273–2.629) | |
| Without DP | 0 | 1 | ||
| With early DP | 2 (9.5%) | 55.3 (49.2–61.5) | ||
| With definite DP | 14 (19.7%) | 49.9 (45.2–54.6) | 2.279 (0.518–10.032) | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2026 by the authors. Published by MDPI on behalf of the Lithuanian University of Health Sciences. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license.
Share and Cite
Marković, N.; Petrović, M.; Žugić, V.; Bulatović, S.; Bojić, M.; Milovanović, B. Autonomic Nervous System Dysfunction in Diabetic Patients After Myocardial Infarction: Prognostic Role of the Valsalva Maneuver. Medicina 2026, 62, 96. https://doi.org/10.3390/medicina62010096
Marković N, Petrović M, Žugić V, Bulatović S, Bojić M, Milovanović B. Autonomic Nervous System Dysfunction in Diabetic Patients After Myocardial Infarction: Prognostic Role of the Valsalva Maneuver. Medicina. 2026; 62(1):96. https://doi.org/10.3390/medicina62010096
Chicago/Turabian StyleMarković, Nikola, Maša Petrović, Vasko Žugić, Sulin Bulatović, Milovan Bojić, and Branislav Milovanović. 2026. "Autonomic Nervous System Dysfunction in Diabetic Patients After Myocardial Infarction: Prognostic Role of the Valsalva Maneuver" Medicina 62, no. 1: 96. https://doi.org/10.3390/medicina62010096
APA StyleMarković, N., Petrović, M., Žugić, V., Bulatović, S., Bojić, M., & Milovanović, B. (2026). Autonomic Nervous System Dysfunction in Diabetic Patients After Myocardial Infarction: Prognostic Role of the Valsalva Maneuver. Medicina, 62(1), 96. https://doi.org/10.3390/medicina62010096






