Are We Still Mediterranean? Dietary Quality and Adherence in Sicilian Women Undergoing ART: A Prospective Observational Cohort Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Participants
2.2. ART Procedures
2.3. Dietary Assessment and MEDAS Questionnaire
2.4. Statistical Analysis
2.5. Ethical Approval
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Rees, K.; Takeda, A.; Martin, N.; Ellis, L.; Wijesekara, D.; Vepa, A.; Das, A.; Hartley, L.; Stranges, S. Mediterranean-style diet for the primary and secondary prevention of cardiovascular disease. Cochrane Database Syst. Rev. 2019, 3, CD009825. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Feng, J.; Wu, Q.; Liang, Y.; Liang, Y.; Bin, Q. Epidemiological characteristics of infertility, 1990–2021, and 15-year forecasts: An analysis based on the global burden of disease study 2021. Reprod. Health 2025, 22, 26. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Garolla, A.; Pizzol, D.; Carosso, A.R.; Borini, A.; Ubaldi, F.M.; Calogero, A.E.; Ferlin, A.; Lanzone, A.; Tomei, F.; Engl, B.; et al. Practical Clinical and Diagnostic Pathway for the Investigation of the Infertile Couple. Front. Endocrinol. 2021, 11, 591837. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Rooney, K.L.; Domar, A.D. The relationship between stress and infertility. Dialogues Clin. Neurosci. 2018, 20, 41–47. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Karayiannis, D.; Kontogianni, M.D.; Mendorou, C.; Mastrominas, M.; Yiannakouris, N. Adherence to the Mediterranean diet and IVF success rate among non-obese women attempting fertility. Hum. Reprod. 2018, 33, 494–502. [Google Scholar] [CrossRef] [PubMed]
- Gaskins, A.J.; Nassan, F.L.; Chiu, Y.H.; Arvizu, M.; Williams, P.L.; Keller, M.G.; Souter, I.; Hauser, R.; Chavarro, J.E. EARTH Study Team. Dietary patterns and outcomes of assisted reproduction. Am. J. Obstet. Gynecol. 2019, 220, 567.e1–567.e18. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Toledo, E.; Lopez-del Burgo, C.; Ruiz-Zambrana, A.; Donazar, M.; Navarro-Blasco, I.; Martínez-González, M.A.; de Irala, J. Dietary patterns and difficulty conceiving: A nested case-control study. Fertil. Steril. 2011, 96, 1149–1153. [Google Scholar] [CrossRef] [PubMed]
- Cristodoro, M.; Zambella, E.; Fietta, I.; Inversetti, A.; Di Simone, N. Dietary Patterns and Fertility. Biology 2024, 13, 131. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Martínez-González, M.A.; García-Arellano, A.; Toledo, E.; Salas-Salvadó, J.; Buil-Cosiales, P.; Corella, D.; Covas, M.I.; Schröder, H.; Arós, F.; Gómez-Gracia, E.; et al. A 14-Item Mediterranean Diet Assessment Tool and Obesity Indexes among High-Risk Subjects: The PREDIMED Trial. PLoS ONE 2012, 7, e43134. [Google Scholar] [CrossRef] [PubMed]
- Donato, M.; Capalbo, A.; Morizio, E.; Fratini, R.M.; Pilenzi, L.; D’Antonio, F.; Stuppia, L.; Vitacolonna, E.; Gatta, V.; Konstantinidou, F. The Role of Lifestyle Intervention in Female Fertility: A Modifiable Factor for Preconception Health. Nutrients 2025, 17, 2101. [Google Scholar] [CrossRef] [PubMed]
- Kazemi, M.; Kim, J.Y.; Wan, C.; Xiong, J.D.; Michalak, J.; Xavier, I.B.; Ganga, K.; Tay, C.T.; Grieger, J.A.; Parry, S.A.; et al. Comparison of dietary and physical activity behaviors in women with and without polycystic ovary syndrome: A systematic review and meta-analysis of 39471 women. Hum. Reprod. Update 2022, 28, 910–955, Erratum in Hum. Reprod. Update 2023, 29, 155. https://doi.org/10.1093/humupd/dmac036. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Keys, A.; Fidanza, F.; Karvonen, M.J.; Kimura, N.; Taylor, H.L. Indices of relative weight and obesity. J. Chronic Dis. 1972, 25, 329–343. [Google Scholar] [CrossRef] [PubMed]
- Emokpae, M.A.; Brown, S.I. Effects of lifestyle factors on fertility: Practical recommendations for modification. Reprod. Fertil. 2021, 2, R13–R26. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Baroutis, D.; Kalampokas, T.; Katsianou, E.; Psarris, A.; Daskalakis, G.; Panoulis, K.; Eleftheriades, M. The Role of the Mediterranean Diet in Assisted Reproduction: A Literature Review. Nutrients. 2024, 16, 2807. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Yang, J.; Song, Y.; Gaskins, A.J.; Li, L.J.; Huang, Z.; Eriksson, J.G.; Hu, F.B.; Chong, Y.S.; Zhang, C. Mediterranean diet and female reproductive health over lifespan: A systematic review and meta-analysis. Am. J. Obstet. Gynecol. 2023, 229, 617–631. [Google Scholar] [CrossRef] [PubMed]
- Muffone, A.R.M.C.; de Oliveira Lübke, P.D.P.; Rabito, E.I. Mediterranean diet and infertility: A systematic review with meta-analysis of cohort studies. Nutr. Rev. 2023, 81, 775–789. [Google Scholar] [CrossRef] [PubMed]
- Karayiannis, D.; Kontogianni, M.D.; Mendorou, C.; Douka, L.; Mastrominas, M.; Yiannakouris, N. Association between adherence to the Mediterranean diet and semen quality parameters in male partners of couples attempting fertility. Hum. Reprod. 2017, 32, 215–222. [Google Scholar] [CrossRef] [PubMed]
- Winter, H.G.; Rolnik, D.L.; Mol, B.W.J.; Torkel, S.; Alesi, S.; Mousa, A.; Habibi, N.; Silva, T.R.; Oi Cheung, T.; Thien Tay, C.; et al. Can Dietary Patterns Impact Fertility Outcomes? A Systematic Review and Meta-Analysis. Nutrients 2023, 15, 2589. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
| Characteristics | Female Factor (n = 37) | Male Factor (n = 43) | Idiopathic (n = 20) |
|---|---|---|---|
| Age (years), mean | 36.4 | 34.8 | 36.5 |
| BMI (kg/m2), mean | 24.99 | 23.50 | 23.68 |
| Smoking, n (%) | 6 (16%) | 12 (28%) | 5 (25%) |
| AMH (mean ± SD) | 3.20 ± 3.13 ng/mL | 2.31 ± 0.94 ng/mL | 2.55 ± 2.13 ng/mL |
| Total oocytes retrieved (mean ± SD) | 8.68 ± 3.22 | 9.77 ± 2.87 | 9.50 ± 3.07 |
| MII oocytes, mean | 6.65 ± 2.68 | 7.37 ± 2.38 | 7.20 ± 2.6 |
| Clinical pregnancy, (%) | 32 (40.6%) | 22 (53.7%) | 8 (44.4%) |
| Characteristics | Value |
|---|---|
| Age (years), mean ± SD | 35.7 ± 3.8 |
| BMI (kg/m2), mean ± SD | 24.1 ± 4.7 |
| BMI categories, n (%) | Underweight 7 (7%) |
| Normal weight 56 (56%); | |
| Overweight 23 (23%); | |
| Obese 14 (14%) | |
| Smoking, n (%) | Smokers 23 (23%) |
| Cause of infertility, n (%) | Female factor 37 (37%); |
| Male factor 43 (43%); | |
| Idiopathic 20 (20%) | |
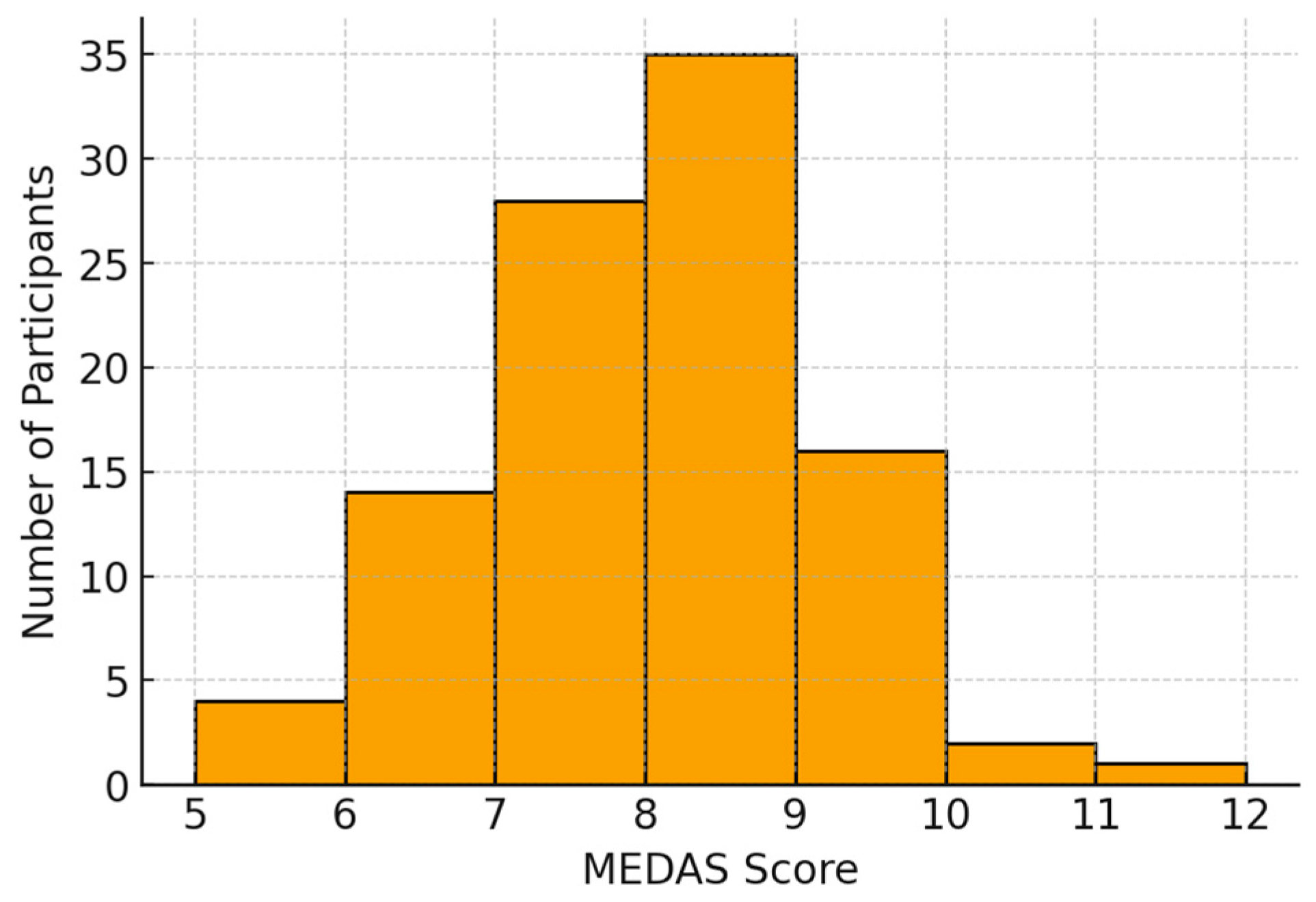
| MEDAS score, mean ± SD (range) | 7.6 ± 1.2 (4–11) |
| MEDAS adherence categories, n (%) | Low (0–5) 4 (4%); |
| Moderate (6–9) 93 (93%); | |
| High (≥10) 3 (3%) | |
| AMH (ng/mL), mean ± SD | 2.69 ± 2.23 |
| Items | Scoring | |
|---|---|---|
| Yes | 0–1 |
| ≥4 tablespoons/day | 0–1 |
| ≥2 servings/day | 0–1 |
| ≥3 servings/day | 0–1 |
| <1 serving/day | 0–1 |
| <1 serving/day | 0–1 |
| <1 serving/day | 0–1 |
| 1–7 glasses/week | 0–1 |
| ≥3 servings/week | 0–1 |
| ≥3 servings/week | 0–1 |
| <3 times/week | 0–1 |
| ≥3 servings/week | 0–1 |
| Yes | 0–1 |
| ≥2 times/week | 0–1 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Published by MDPI on behalf of the Lithuanian University of Health Sciences. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license.
Share and Cite
Liprino, A.; Corsetti, V.; Giacone, F.; Russo, G.I.; Asmundo, M.G.; Chamayou, S.; Guglielmino, A. Are We Still Mediterranean? Dietary Quality and Adherence in Sicilian Women Undergoing ART: A Prospective Observational Cohort Study. Medicina 2026, 62, 23. https://doi.org/10.3390/medicina62010023
Liprino A, Corsetti V, Giacone F, Russo GI, Asmundo MG, Chamayou S, Guglielmino A. Are We Still Mediterranean? Dietary Quality and Adherence in Sicilian Women Undergoing ART: A Prospective Observational Cohort Study. Medicina. 2026; 62(1):23. https://doi.org/10.3390/medicina62010023
Chicago/Turabian StyleLiprino, Annalisa, Veronica Corsetti, Filippo Giacone, Giorgio Ivan Russo, Maria Giovanna Asmundo, Sandrine Chamayou, and Antonino Guglielmino. 2026. "Are We Still Mediterranean? Dietary Quality and Adherence in Sicilian Women Undergoing ART: A Prospective Observational Cohort Study" Medicina 62, no. 1: 23. https://doi.org/10.3390/medicina62010023
APA StyleLiprino, A., Corsetti, V., Giacone, F., Russo, G. I., Asmundo, M. G., Chamayou, S., & Guglielmino, A. (2026). Are We Still Mediterranean? Dietary Quality and Adherence in Sicilian Women Undergoing ART: A Prospective Observational Cohort Study. Medicina, 62(1), 23. https://doi.org/10.3390/medicina62010023








