Magnesium, Zinc and Copper in Lung Fibrosis: A Narrative Review
Abstract
1. Introduction
2. Oxidative Stress
3. Inflammation
4. Mitochondrial Dysfunctions
5. Excessive Extracellular Matrix Accumulation
6. Fibroblast and Myofibroblast Differentiation and Fibrosis
7. Alveolar Macrophages
8. Alveolar Epithelial Cells
9. Some Active Endogenous Substances Involved in IPF Pathogeny
9.1. Fatty Acids
9.2. Eicosanoids
9.3. Protein p53
9.4. Sirtuin 1 (SIRT 1) and Sirtuin 3 (SIRT3)
10. Apoptosis
11. Genetics
12. Therapeutics
13. Conclusions
Limitations
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
References
- Richeldi, L.; Collard, H.R.; Jones, M.G. Idiopathic pulmonary fibrosis. Lancet 2017, 389, 1941–1952. [Google Scholar] [CrossRef]
- Niccoli, T.; Partridge, L. Ageing as a Risk Factor for Disease. Curr. Biol. 2012, 22, R741–R752. [Google Scholar] [CrossRef]
- Giriyappagoudar, M.; Vastrad, B.; Horakeri, R.; Vastrad, C. Study on Potential Differentially Expressed Genes in Idiopathic Pulmonary Fibrosis by Bioinformatics and Next-Generation Sequencing Data Analysis. Biomedicines 2023, 11, 3109. [Google Scholar] [CrossRef] [PubMed]
- Martinez, F.J.; Collard, H.R.; Pardo, A.; Raghu, G.; Richeldi, L.; Selman, M.; Swigris, J.J.; Taniguchi, H.; Athol, U.; Wells, A.U. Idiopathic pulmonary fibrosis. Nat. Rev. Dis. Primers 2017, 3, 17074. [Google Scholar] [CrossRef] [PubMed]
- Raghu, G.; Collard, H.R.; Egan, J.J.; Martinez, F.J.; Behr, J.; Brown, K.K.; Colby, T.V.; Cordier, J.-F.; Flaherty, K.R.; Lasky, J.A.; et al. An official ATS/ERS/JRS/ALAT statement: Idiopathic pulmonary fibrosis: Evidence-based guidelines for diagnosis and management. Am. J. Respir. Crit. Care Med. 2011, 183, 788–824. [Google Scholar] [CrossRef] [PubMed]
- Chanda, D.; Otoupalova, E.; Smith, S.R.; Volckaert, T.; De Langhe, S.P.; Thannickal, V.J. Developmental pathways in the pathogenesis of lung fibrosis. Mol. Asp. Med. 2019, 65, 56–69. [Google Scholar] [CrossRef]
- Raghu, G.; Chen, S.Y.; Yeh, W.S.; Maroni, B.; Li, Q.; Lee, Y.C. Idiopathic pulmonary fibrosis in US Medicare beneficiaries aged 65 years and older: Incidence, prevalence, and survival, 2001–11. Lancet Respir. Med. 2014, 2, 566–572. [Google Scholar] [CrossRef]
- American Thoracic Society. Idiopathic pulmonary fibrosis: Diagnosis and treatment. International consensus statement. American Thoracic Society (ATS), and the European Respiratory Society. Am. J. Respir. Crit. Care Med. 2000, 161, 646–664. [Google Scholar] [CrossRef]
- Chianese, M.; Screm, G.; Salton, F.; Confalonieri, P.; Trotta, L.; Barbieri, M.; Ruggero, L.; Mari, M.; Reccardini, N.; Geri, P.; et al. Pirfenidone and Nintedanib in Pulmonary Fibrosis: Lights and Shadows. Pharmaceuticals 2024, 17, 709. [Google Scholar] [CrossRef]
- Finnerty, J.P.; Ponnuswamy, A.; Dutta, P.; Abdelaziz, A.; Kamil, H. Efficacy of antifibrotic drugs, nintedanib and pirfenidone, in treatment of progressive pulmonary fibrosis in both idiopathic pulmonary fibrosis (IPF) and non-IPF: A systematic review and meta-analysis. BMC Pulm. Med. 2021, 21, 411. [Google Scholar] [CrossRef]
- Wang, D.; Ma, Y.; Tong, X.; Zhang, Y.; Fan, H. Diabetes Mellitus Contributes to Idiopathic Pulmonary Fibrosis: A Review From Clinical Appearance to Possible Pathogenesis. Front. Public Health 2020, 8, 196. [Google Scholar] [CrossRef]
- Mzimela, N.; Dimba, N.; Sosibo, A.; Khathi, A. Evaluating the impact of type 2 diabetes mellitus on pulmonary vascular function and the development of pulmonary fibrosis. Front. Endocrinol. 2024, 15, 1431405. [Google Scholar] [CrossRef]
- Lawson, W.E.; Crossno, P.F.; Polosukhin, V.V.; Roldan, J.; Cheng, D.-S.; Lane, K.B.; Blackwell, T.R.; Xu, C.; Markin, C.; Ware, L.B.; et al. Endoplasmic reticulum stress in alveolar epithelial cells is prominent in IPF: Association with altered surfactant protein processing and herpesvirus infection. Am. J. Physiol. Lung Cell Mol. Physiol. 2008, 294, L1119–L1126. [Google Scholar] [CrossRef] [PubMed]
- Molyneaux, P.L.; Cox, M.J.; Willis-Owen, S.A.G.; Mallia, P.; Russell, K.E.; Russell, A.-M.; Murphy, E.; Johnston, S.L.; Schwartz, D.A.; Wells, A.U.; et al. The role of bacteria in the pathogenesis and progression of idiopathic pulmonary fibrosis. Am. J. Respir. Crit. Care Med. 2014, 190, 906–913. [Google Scholar] [CrossRef]
- Goto, T. Measuring Surgery Outcomes of Lung Cancer Patients with Concomitant Pulmonary Fibrosis: A Review of the Literature. Cancers 2018, 10, 223. [Google Scholar] [CrossRef] [PubMed]
- Kinoshita, T.; Goto, T. Molecular Mechanisms of Pulmonary Fibrogenesis and Its Progression to Lung Cancer: A Review. Int. J. Mol. Sci. 2019, 20, 1461. [Google Scholar] [CrossRef] [PubMed]
- Romani, A.M.P. Intracellular magnesium homeostasis. In Magnesium in the Central Nervous System; Vink, R., Nechifor, M., Eds.; University of Adelaide Press: Adelaide, Australia, 2011; pp. 13–58. [Google Scholar]
- Micke, O.; Vormann, J.; Kraus, A.; Kisters, K. Serum magnesium: Time for a standardized and evidence-based reference range. Magnes. Res. 2021, 34, 84–89. [Google Scholar]
- Rosanoff, A.; West, C.; Elin, R.J.; Micke, O.; Baniasadi, S.; Barbagallo, M.; Campbell, E.; Cheng, F.-C.; Costello, R.B.; Gamboa-Gomez, C.; et al. Recommendation on an updated standardization of serum magnesium reference ranges. Eur. J. Nutr. 2022, 61, 3697–3706. [Google Scholar] [CrossRef]
- Barbagallo, M.; Dominguez, L.J. Magnesium and aging. Curr. Pharm. Des. 2010, 16, 832–839. [Google Scholar] [CrossRef]
- Thannickal, V.J. Mechanistic Links between Aging and Lung Fibrosis. Biogerontology 2013, 14, 609–615. [Google Scholar] [CrossRef]
- Lutsenko, S. Human copper homeostasis: A network of interconnected pathways. Curr. Opin. Nephrol. Hypertens. 2010, 4, 211–217. [Google Scholar] [CrossRef] [PubMed]
- Lech, T.; Sadlik, J.K. Copper concentration in body tissues and fluids in normal subjects of southern Poland. Biol. Trace Elem. Res. 2007, 118, 10–15. [Google Scholar] [CrossRef]
- Lin, J.; Xu, F.; Zhang, C.; Wu, B. The effect of some trace elements on the expression of telomerase gene in lung cancer. Cell. Mol. Biol. 2022, 68, 86–90. [Google Scholar] [CrossRef] [PubMed]
- Hasanato, R.M.W. Trace elements in type 2 diabetes mellitus and their association with glycemic control. Afr. Health Sci. 2020, 20, 287–293. [Google Scholar] [CrossRef]
- Bost, M.; Houdart, S.; Oberli, M.; Kalonji, E.; Huneau, J.F.; Margaritis, I. Dietary copper and human health: Current evidence and unresolved issues. J. Trace Elem. Med. Biol. 2016, 35, 107–115. [Google Scholar] [CrossRef]
- Prasad, A.P. Discovery of human zinc deficiency: Its impact on human health and disease. Adv. Nutr. 2013, 4, 176–190. [Google Scholar] [CrossRef]
- Warthon-Medina, M.; Moran, V.H.; Stammers, A.-L.; Dillon, S.; Qualter, P.; Nissensohn, M.; Serra-Majem, L.; Lowe, N.M. Zinc intake, status and indices of cognitive function in adults and children: A systematic review and meta-analysis. Eur. J. Clin. Nutr. 2015, 69, 649–661. [Google Scholar] [CrossRef]
- Khan, N.A.; Singla, M.; Samal, S.; Lodha, R.; Medigeshi, G.R. Respiratory Syncytial Virus-Induced Oxidative Stress Leads to an Increase in Labile Zinc Pools in Lung Epithelial Cells. mSphere 2020, 5, e00447-20. [Google Scholar] [CrossRef]
- Bargagli, E.; Monaci, F.; Bianchi, N.; Bucci, C.; Rottoli, P. Analysis of trace elements in bronchoalveolar lavage of patients with diffuse lung diseases. Biol. Trace Elem. Res. 2008, 124, 225–235. [Google Scholar] [CrossRef]
- Wang, Y.; Sun, Z.; Li, A.; Zhang, Y. Association between serum zinc levels and lung cancer: A meta-analysis of observational studies. World J. Surg. Oncol. 2019, 17, 78. [Google Scholar] [CrossRef] [PubMed]
- Zhang, L.; Shao, J.; Tan, S.W.; Ye, H.P.; Shan, X.Y. Association between serum copper/zinc ratio and lung cancer: A systematic review with meta-analysis. J. Trace Elem. Med. Biol. 2022, 74, 127061. [Google Scholar] [CrossRef]
- Moss, B.J.; Ryter, S.W.; Rosas, I.O. Pathogenic Mechanisms Underlying Idiopathic Pulmonary Fibrosis. Annu. Rev. Pathol. 2022, 17, 515–546. [Google Scholar] [CrossRef]
- Wynn, T.A. Integrating mechanisms of pulmonary fibrosis. J. Exp. Med. 2011, 208, 1339–1350. [Google Scholar] [CrossRef]
- Matsuzawa, Y.; Kawashima, T.; Kuwabara, R.; Hayakawa, S.; Irie, T.; Yoshida, T.; Rikitake, H.; Wakabayashi, T.; Okada, N.; Kawashima, K.; et al. Change in serum marker of oxidative stress in the progression of idiopathic pulmonary fibrosis. Pulm. Pharmacol. Ther. 2015, 32, 1–6. [Google Scholar] [CrossRef]
- Yamazaki, C.; Hoshino, J.; Hori, Y.; Sekiguchi, T.; Miyauchi, S.; Mizuno, S.; Hori, K. Effect of lecithinized-superoxide dismutase on the interstitial pneumonia model induced by bleomycin in mice. Jpn. J. Pharmacol. 1997, 75, 97–100. [Google Scholar] [CrossRef]
- Kurys, E.; Kurys, P.; Kuźniar, A.R.; Kieszko, R. Analysis of antioxidant enzyme activity and magnesium level in chronic obstructive pulmonary disease (COPD). Ann. Univ. Marie Curie Sklodowska Med. 2001, 56, 261–266. [Google Scholar]
- Luan, R.; Luo, M.; Ding, D.; Su, X.; Yang, J. Zinc deficiency increases lung inflammation and fibrosis in obese mice by promoting oxidative stress. Biochim. Biophys. Acta Gen. Subj. 2024, 1868, 130518. [Google Scholar] [CrossRef] [PubMed]
- Lee, C.Y.; Jan, W.C.; Tsai, P.S.; Huang, C.J. Magnesium sulfate mitigates acute lung injury in endotoxemia rats. J. Trauma 2011, 70, 1177–1185. [Google Scholar] [CrossRef]
- Wang, J.; Ma, C.; Wang, S. Effects of acteoside on lipopolysaccharide-induced inflammation in acute lung injury via regulation of NF-κB pathway in vivo and in vitro. Toxicol. Appl. Pharmacol. 2015, 285, 128–135. [Google Scholar] [CrossRef]
- Jiang, J.; Chen, Q.; Chen, X.; Li, J.; Li, S.; Yang, B. Magnesium sulfate ameliorates sepsis-induced diaphragm dysfunction in rats via inhibiting HMGB1/TLR4/NF-κB pathway. NeuroReport 2020, 31, 902–908. [Google Scholar] [CrossRef] [PubMed]
- Zhang, L.; Yang, L.; Xie, X.; Zheng, H.; Zheng, H.; Zhang, L.; Liu, C.; Piao, J.-G.; Li, F. Baicalin Magnesium Salt Attenuates Lipopolysaccharide-Induced Acute Lung Injury via Inhibiting of TLR4/NF-κ B Signaling Pathway. J. Immunol. Res. 2021, 2021, 6629531. [Google Scholar] [CrossRef]
- Zhang, Z.; Weichenthal, S.; Kwong, J.C.; Burnett, R.T.; Hatzopoulou, M.; Jerrett, M.; van Donkelaar, A.; Bai, L.; Martin, R.V.; Copes, R.; et al. A Population-Based Cohort Study of Respiratory Disease and Long-Term Exposure to Iron and Copper in Fine Particulate Air Pollution and Their Combined Impact on Reactive Oxygen Species Generation in Human Lungs. Environ. Sci. Technol. 2021, 55, 3807–3818. [Google Scholar] [CrossRef] [PubMed]
- Lu, S.C. Glutathione synthesis. Biochim. Biophys. Acta 2013, 1830, 3143–3153. [Google Scholar] [CrossRef] [PubMed]
- Walther, U.I.; Walther, S.C.; Temrück, O. Effect of enlarged glutathione on zinc-mediated toxicity in lung-derived cell lines. Toxicol. Vitr. 2007, 21, 380–386. [Google Scholar] [CrossRef] [PubMed]
- Türüt, H.; Kurutas, E.B.; Bulbuloglu, E.; Yasim, A.; Ozkaya, M.; Onder, A.; Imrek, S.S. Zinc aspartate alleviates lung injury induced by intestinal ischemia-reperfusion in rats. J. Surg. Res. 2009, 151, 62–67. [Google Scholar] [CrossRef]
- Sacan, O.; Turkyilmaz, I.B.; Bayrak, B.B.; Mutlu, O.; Akev, N.; Yanardag, R. Zinc supplementation ameliorates glycoprotein components and oxidative stress changes in the lung of streptozotocin diabetic rats. Biometals 2016, 29, 239–248. [Google Scholar] [CrossRef]
- Gursel, F.E.; Tekeli, S.K. The effects of feeding with different levels of zinc and chromium on plasma thiobarbituric acid reactive substances and antioxidant enzymes in rats. Pol. J. Vet. Sci. 2009, 12, 35–39. [Google Scholar]
- Jing, Y.L.; Zhao, C.X.; Duan, G.X.; Wang, Y.L.; Hu, Y.Q.; Zhang, L.Y. Therapeutic effect of zinc sulfate on lung injury during superior mesenteric artery occlusion(SMAO) shock. Zhongguo Ying Yong Sheng Li Xue Za Zhi 2006, 22, 90–93. [Google Scholar]
- Kouadri, A.; Cormenier, J.; Gemy, K.; Macari, L.; Charbonnier, P.; Richaud, P.; Michaud-Soret, I.; Alfaidy, N.; Benharouga, M. Copper-Associated Oxidative Stress Contributes to Cellular Inflammatory Responses in Cystic Fibrosis. Biomedicines 2021, 9, 329. [Google Scholar] [CrossRef]
- Ngamchuea, K.; Batchelor-McAuley, C.; Richard, G.; Compton, R.G. The Copper(II)-Catalyzed Oxidation of Glutathione. Chemistry 2016, 22, 15937–15944. [Google Scholar] [CrossRef]
- Koudstaal, T.; Wijsenbeek, M.S. Idiopathic pulmonary fibrosis. Presse Med. 2023, 52, 104166. [Google Scholar] [CrossRef]
- May, R.D.; Fung, M. Strategies targeting the IL-4/IL-13 axes in disease. Cytokine 2015, 75, 89–116. [Google Scholar] [CrossRef]
- Peng, L.; Wen, L.; Shi, Q.-F.; Gao, F.; Huang, B.; Meng, J.; Hu, C.-P.; Wang, C.-M. Scutellarin ameliorates pulmonary fibrosis through inhibiting NF-κB/NLRP3-mediated epithelial-mesenchymal transition and inflammation. Cell Death Dis. 2020, 11, 978. [Google Scholar] [CrossRef] [PubMed]
- Prasad, A.S. Zinc: Mechanisms of host defense. J. Nutr. 2007, 137, 1345–1349. [Google Scholar] [CrossRef] [PubMed]
- Liu, M.-J.; Bao, S.; Gálvez-Peralta, M.; Pyle, C.J.; Rudawsky, A.C.; Pavlovicz, R.E.; Killilea, D.W.; Li, C.; Nebert, D.W.; Wewers, M.D.; et al. ZIP8 regulates host defense through zinc-mediated inhibition of NF-κB. Cell Rep. 2013, 3, 386–400. [Google Scholar] [CrossRef] [PubMed]
- Biaggio, V.S.; Pérez Chaca, M.V.; Valdéz, S.R.; Gómez, N.N.; Gimenez, M.S. Alteration in the expression of inflammatory parameters as a result of oxidative stress produced by moderate zinc deficiency in rat lung. Exp. Lung Res. 2010, 36, 31–44. [Google Scholar] [CrossRef]
- Yang, Y.; Huang, L.; Tian, C.; Qian, B. Magnesium isoglycyrrhizinate inhibits airway inflammation in rats with chronic obstructive pulmonary disease. BMC Pulm. Med. 2021, 21, 371. [Google Scholar] [CrossRef]
- Chinju, A.; Moriyama, M.; Kakizoe-Ishiguro, N.; Chen, H.; Miyahara, Y.; Rafiul Haque, A.S.M.; Furusho, K.; Sakamoto, M.; Kai, K.; Kibe, K.; et al. CD163+ M2 Macrophages Promote Fibrosis in IgG4-Related Disease Via Toll-like Receptor 7/Interleukin-1 Receptor-Associated Kinase 4/NF-κB Signaling. Arthritis Rheumatol. 2022, 74, 892–901. [Google Scholar] [CrossRef]
- Onuma, S.; Manabe, A.; Yoshino, Y.; Matsunaga, T.; Asai, T.; Ikari, A. Upregulation of Chemoresistance by Mg2+ Deficiency through Elevation of ATP Binding Cassette Subfamily B Member 1 Expression in Human Lung Adenocarcinoma A549 Cells. Cells 2021, 10, 1179. [Google Scholar] [CrossRef]
- Ahmadi, S.; Naderifar, M.; Samimi, M.; Mirhosseini, N.; Amirani, E.; Aghadavod, E.; Asemi, Z. The effects of magnesium supplementation on gene expression related to inflammatory markers, vascular endothelial growth factor, and pregnancy outcomes in patients with gestational diabetes. Magnes. Res. 2018, 31, 131–142. [Google Scholar]
- Sonaglioni, A.; Caminati, A.; Lipsi, R.; Lombardo, M.; Harari, S. Association between C-reactive protein and carotid plaque in mild-to-moderate idiopathic pulmonary fibrosis. Intern. Emerg. Med. 2021, 16, 1529–1539. [Google Scholar] [CrossRef]
- Cottin, V.; Valenzuela, C. C-reactive protein as a candidate biomarker in fibrotic interstitial lung disease. Respirology 2024, 29, 195–198. [Google Scholar] [CrossRef] [PubMed]
- Zanforlini, B.M.; Ceolin, C.; Trevisan, C.; Alessi, A.; Seccia, D.M.; Noale, M.; Maggi, S.; Guarnieri, G.; Vianello, A.; Sergi, G. Clinical trial on the effects of oral magnesium supplementation in stable-phase COPD patients. Aging Clin. Exp. Res. 2022, 34, 167–174. [Google Scholar] [CrossRef]
- Lominadze, D.; Saari, J.T.; Percival, S.S.; Schuschke, D.A. Proinflammatory effects of copper deficiency on neutrophils and lung endothelial cells. Immunol. Cell Biol. 2004, 82, 231–238. [Google Scholar] [CrossRef]
- Persichini, T.; Percario, Z.; Mazzon, E.; Colasanti, M.; Cuzzocrea, S.; Musci, G. Copper activates the NF-κB pathway in vivo. Antioxid. Redox Signal 2006, 8, 1897–1904. [Google Scholar] [CrossRef] [PubMed]
- Kennedy, T.; Ghio, A.J.; Reed, W.; Samet, J.; Zagorski, J.; Quay, J.; Carter, J.; Dailey, L.; Hoidal, J.R.; Devlin, R.B. Copper-dependent inflammation and nuclear factor-κB activation by particulate air pollution. Am. J. Respir. Cell Mol. Biol. 1998, 19, 366–378. [Google Scholar] [CrossRef]
- Touyz, R.M.; Yao, G. Modulation of vascular smooth muscle cell growth by magnesium-role of mitogen-activated protein kinases. J. Cell. Physiol. 2003, 197, 326–335. [Google Scholar] [CrossRef] [PubMed]
- Salucci, S.; Giordani, M.; Betti, M.; Valentini, L.; Gobbi, P.; Mattioli, M. The in vitro cytotoxic effects of natural (fibrous epsomite crystals) and synthetic (Epsom salt) magnesium sulfate. Microsc. Res. Tech. 2024, 87, 685–694. [Google Scholar] [CrossRef]
- Xie, C.; Li, X.; Zhu, J.; Wu, J.; Geng, S.; Zhong, C. Magnesium isoglycyrrhizinate suppresses LPS-induced inflammation and oxidative stress through inhibiting NF-κB and MAPK pathways in RAW264.7 cells. Bioorg Med. Chem. 2019, 27, 516–524. [Google Scholar] [CrossRef]
- Nuttall, J.R.; Oteiza, P.I. Zinc and the ERK kinases in the developing brain. Neurotox. Res. 2012, 21, 128–141. [Google Scholar] [CrossRef]
- Azriel-Tamir, H.; Sharir, H.; Schwartz, B.; Hershfinkel, M. Extracellular zinc triggers ERK-dependent activation of Na+/H+ exchange in colonocytes mediated by the zinc-sensing receptor. J. Biol. Chem. 2004, 279, 51804–51816. [Google Scholar] [CrossRef]
- Liu, Y.; Xiao, Y.; Liu, J.; Feng, L.; Kang, Y.J. Copper-induced reduction in myocardial fibrosis is associated with increased matrix metalloproteins in a rat model of cardiac hypertrophy. Metallomics 2018, 10, 201–208. [Google Scholar] [CrossRef]
- Boilan, E.; Winant, V.; Dumortier, E.; Piret, J.-P.; Bonfitto, F.; Osiewacz, H.D.; Debacq-Chainiaux, F.; Toussaint, O. Role of p38MAPK and oxidative stress in copper-induced senescence. Age 2013, 35, 2255–2271. [Google Scholar] [CrossRef]
- Gaun, S.; Ali, S.A.; Singh, P.; Patwa, J.; Flora, S.J.S.; Datusalia, A.K. Melatonin ameliorates chronic copper-induced lung injury. Environ. Sci. Pollut. Res. Int. 2023, 30, 24949–24962. [Google Scholar] [CrossRef] [PubMed]
- Janssen, R.; de Brouwer, B.; Jan, H.; Wouters, E.F. Copper as the most likely pathogenic divergence factor between lung fibrosis and emphysema. Med. Hypotheses 2018, 120, 49–54. [Google Scholar] [CrossRef] [PubMed]
- Bueno, M.; Calyeca, J.; Rojas, M.; Mora, A.M. Mitochondria dysfunction and metabolic reprogramming as drivers of idiopathic pulmonary fibrosis. Redox Biol. 2020, 33, 101509. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.J.; Cheresh, P.; Jablonski, R.P.; Morales-Nebreda, L.; Cheng, Y.; Hogan, E. Mitochondrial catalase overexpressed transgenic mice are protected against lung fibrosis in part via preventing alveolar epithelial cell mitochondrial DNA damage. Free Radic. Biol. Med. 2016, 101, 482–490. [Google Scholar] [CrossRef]
- Zhong, C.C.; Zhao, T.; Hogstrand, C.; Chen, F.; Song, C.C.; Luo, Z. Copper (Cu) induced changes of lipid metabolism through oxidative stress-mediated autophagy and Nrf2/PPARγ pathways. J. Nutr. Biochem. 2022, 100, 108883. [Google Scholar] [CrossRef]
- Mashayekhi, V.K.; Hashemzaei, M.; Tabrizian, K.; Shahraki, J.; Hosseini, M.J. Mechanistic approach for the toxic effects of perfluorooctanoic acid on isolated rat liver and brain mitochondria. Hum. Exp. Toxicol. 2015, 34, 985–996. [Google Scholar] [CrossRef]
- McKeown, S.; Richter, A.G.; O’Kane, C.; McAuley, D.F.; Thickett, D.R. MMP expression and abnormal lung permeability are important determinants of outcome in IPF. Eur. Respir. J. 2009, 33, 77–84. [Google Scholar] [CrossRef]
- Xiao, Z.W.; Zhang, W.; Ma, L.; Qiu, Z.W. Therapeutic effect of magnesium isoglycyrrhizinate in rats on lung injury induced by paraquat poisoning. Eur. Rev. Med. Pharmacol. Sci. 2014, 18, 311–320. [Google Scholar]
- Guo, H.; Lee, J.-D.; Uzui, H.; Yue, H.; Wang, J.; Toyoda, K.; Geshi, T.; Ueda, T. Effects of folic acid and magnesium on the production of homocysteine-induced extracellular matrix metalloproteinase-2 in cultured rat vascular smooth muscle cells. Circ. J. 2006, 70, 141–146. [Google Scholar] [CrossRef] [PubMed]
- Mohtashamian, A.; Soleimani, A.; Gilasi, H.R.; Kheiripour, N.; Taba, S.M.M.; Sharifi, N. Association of Zinc Status with Matrix Metalloproteinases, Advanced Glycation End-Products, and Blood Pressure in Patients with Chronic Kidney Disease. Biol. Trace Elem. Res. 2023, 201, 4275–4285. [Google Scholar] [CrossRef] [PubMed]
- Xu, C.; Huang, Z.; Liu, L.; Luo, C.; Lu, G.; Li, Q.; Gao, X. Zinc Regulates Lipid Metabolism and MMPs Expression in Lipid Disturbance Rabbits. Biol. Trace Elem. Res. 2015, 168, 411–420. [Google Scholar] [CrossRef]
- Siméon, A.; Monier, F.; Emonard, H.; Gillery, P.; Birembaut, P.; Hornebeck, W.; Maquart, F.X. Expression and activation of matrix metalloproteinases in wounds: Modulation by the tripeptide-copper complex glycyl-L-histidyl-L-lysine-Cu2+. J. Investig. Dermatol. 1999, 112, 957–964. [Google Scholar] [CrossRef] [PubMed]
- Varzaneh, M.B.; Rahmani, H.; Jahanian, R.; Mahdavi, A.H.; Perreau, C.; Perrot, G.; Brézillon, S.; Maquart, F.-X. Effects of Dietary Copper-Methionine on Matrix Metalloproteinase-2 in the Lungs of Cold-Stressed Broilers as an Animal Model for Pulmonary Hypertension. Biol. Trace Elem. Res. 2016, 172, 504–510. [Google Scholar] [CrossRef]
- Upagupta, C.; Shimbori, C.; Alsilmi, R.; Kolb, M. Matrix abnormalities in pulmonary fibrosis. Eur. Respir. Rev. 2018, 27, 180033. [Google Scholar] [CrossRef]
- Lee, C.-M.; Park, J.W.; Cho, W.-K.; Zhou, Y.; Han, B.; Yoon, P.O.; Chae, J.; Elias, J.A.; Lee, C.G. Modifiers of TGF-beta1 effector function as novel therapeutic targets of pulmonary fibrosis. Korean J. Intern. Med. 2014, 29, 281–290. [Google Scholar] [CrossRef]
- Bellocq, A.; Azoulay, E.; Marullo, S.; Flahault, A.; Fouqueray, B.; Philippe, C.; Cadranel, J.; Baud, L. Reactive oxygen and nitrogen intermediates increase transforming growth factor-beta1 release from human epithelial alveolar cells through two different mechanisms. Am. J. Respir. Cell Mol. Biol. 1999, 21, 128–136. [Google Scholar] [CrossRef]
- Khalil, N.; O’Connor, R.N.; Unruh, H.W.; Warren, P.W.; Flanders, K.C.; Kemp, A.; Bereznay, O.H.; Greenberg, A.H. Increased production and immunohistochemical localization of transforming growth factor-beta in idiopathic pulmonary fibrosis. Am. J. Respir. Cell Mol. Biol. 1991, 5, 155–162. [Google Scholar] [CrossRef]
- Raghow, B.; Irish, P.; Kang, A.H. Coordinate regulation of transforming growth factor beta gene expression and cell proliferation in hamster lungs undergoing bleomycin-induced pulmonary fibrosis. J. Clin. Investig. 1989, 84, 1836–1842. [Google Scholar] [CrossRef] [PubMed]
- Coker, R.K.; Laurent, G.J.; Shahzeidi, S.; Lympany, P.A.; du Bois, R.M.; Jeffery, P.K.; McAnulty, R.J. Transforming growth factors-beta 1, -beta 2, and -beta 3 stimulate fibroblast procollagen production in vitro but are differentially expressed during bleomycin-induced lung fibrosis. Am. J. Pathol. 1997, 150, 981–991. [Google Scholar]
- Conte, E.; Gili, E.; Fagone, E.; Fruciano, M.; Iemmolo, M.; Vancheri, C. Effect of pirfenidone on proliferation, TGF-beta-induced myofibroblast differentiation and fibrogenic activity of primary human lung fibroblasts. Eur. J. Pharm. Sci. 2014, 58, 13–19. [Google Scholar] [CrossRef] [PubMed]
- Choi, J.Y.; Kang, M.; Jung, J.H.; Kim, W.J.; Yang, H.S.; Lee, K.; Lee, J.; Yang, S.-R.; Rhee, C.K.; Hong, S.H. Exposure of lung fibroblasts to PM2.5 and lead (Pb) induces fibrosis and apoptosis in alveolar epithelial cells via a paracrine effect. Ecotoxicol. Environ. Saf. 2024, 288, 117401. [Google Scholar] [CrossRef]
- Shivakumar, K.; Kumar, B.P. Magnesium deficiency enhances oxidative stress and collagen synthesis in vivo in the aorta of rats. Int. J. Biochem. Cell Biol. 1997, 29, 1273–1278. [Google Scholar] [CrossRef]
- Zeitlmayr, S.; Zierler, S.; Staab-Weijnitz, C.A.; Dietrich, A.; Geiger, F.; Horgen, F.D.; Gudermann, T.; Breit, A. TRPM7 restrains plasmin activity and promotes transforming growth factor-β1 signaling in primary human lung fibroblasts. Arch. Toxicol. 2022, 96, 2767–2783. [Google Scholar] [CrossRef]
- Gu, L.; Zhu, Y.J.; Yang, X.; Guo, Z.J.; Xu, W.B.; Tian, X.L. Effect of TGF-beta/Smad signaling pathway on lung myofibroblast differentiation. Acta Pharmacol. Sin. 2007, 28, 382–391. [Google Scholar] [CrossRef]
- Yang, Q.; Zhang, P.; Liu, T.; Zhang, X.; Pan, X.; Cen, Y.; Liu, Y.; Zhang, H.; Chen, X. Magnesium isoglycyrrhizinate ameliorates radiation-induced pulmonary fibrosis by inhibiting fibroblast differentiation via the p38MAPK/Akt/Nox4 pathway. Biomed. Pharmacother. 2019, 115, 108955. [Google Scholar] [CrossRef]
- Luo, X.; Deng, Q.; Xue, Y.; Zhang, T.; Wu, Z.; Peng, H.; Xuan, L.; Pan, G. Anti-Fibrosis Effects of Magnesium Lithospermate B in Experimental Pulmonary Fibrosis: By Inhibiting TGF-βRI/Smad Signaling. Molecules 2021, 26, 1715. [Google Scholar] [CrossRef] [PubMed]
- Anttinen, H.; Oikarinen, A.; Puistola, U.; Pääkkö, P.; Ryhänen, L. Prevention by zinc of rat lung collagen accumulation in carbon tetrachloride injury. Am. Rev. Respir. Dis. 1985, 132, 536–540. [Google Scholar]
- Elwej, A.; Ghorbel, I.; Chaabane, M.; Chelly, S.; Boudawara, T.; Zeghal, N. Mitigating effects of selenium and zinc on oxidative stress and biochemical and histopathological changes in lung during prenatal and lactational exposure rats to barium chloride. Environ. Sci. Pollut. Res. Int. 2024, 31, 50892–50904. [Google Scholar] [CrossRef]
- Tian, B.; Patrikeev, I.; Ochoa, L.; Vargas, G.; Belanger, K.K.; Litvinov, J.; Boldogh, I.; Ameredes, B.T.; Motamedi, M.; Brasier, A.R. NF-κB Mediates Mesenchymal Transition, Remodeling, and Pulmonary Fibrosis in Response to Chronic Inflammation by Viral RNA Patterns. Am. J. Respir. Cell Mol. Biol. 2017, 56, 506–520. [Google Scholar] [CrossRef]
- Wen, X.; Liu, Y.; Bai, Y.; Li, M.; Fu, Q.; Zheng, Y. LOXL2, a copper-dependent monoamine oxidase, activates lung fibroblasts through the TGF-β/Smad pathway. Int. J. Mol. Med. 2018, 42, 3530–3541. [Google Scholar] [CrossRef] [PubMed]
- Niu, Y.-Y.; Zhang, Y.-Y.; Zhu, Z.; Zhang, X.-Q.; Liu, X.; Zhu, S.-Y.; Song, Y.; Jin, X.; Lindholm, B.; Yu, C. Elevated intracellular copper contributes a unique role to kidney fibrosis by lysyl oxidase mediated matrix crosslinking. Cell Death Dis. 2020, 11, 211. [Google Scholar] [CrossRef]
- Chung, K.W.; Song, S.H.; Kim, M.S. Synergistic effect of copper and amino acid mixtures on the production of extracellular matrix proteins in skin fibroblasts. Mol. Biol. Rep. 2021, 48, 3277–32784. [Google Scholar] [CrossRef]
- Nguyen, X.X.; Nishimoto, T.; Takihara, T.; Mlakar, L.; Bradshaw, A.D.; Feghali-Bostwick, C. Lysyl oxidase directly contributes to extracellular matrix production and fibrosis in systemic sclerosis. Am. J. Physiol. Lung Cell Mol. Physiol. 2021, 320, L29–L40. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.; Lee, D.-K.; Jeon, S.; Kim, S.-H.; Jeong, J.; Kim, J.S.; Cho, J.H.; Park, H.; Cho, W.-S. Combination effect of nanoparticles on the acute pulmonary inflammogenic potential: Additive effect and antagonistic effect. Nanotoxicology 2021, 15, 276–288. [Google Scholar] [CrossRef]
- Besiktepe, N.; Kayalar, O.; Ersen, E.; Oztay, F. The copper dependent-lysyl oxidases contribute to the pathogenesis of pulmonary emphysema in chronic obstructive pulmonary disease patients. J. Trace Elem. Med. Biol. 2017, 44, 247–255. [Google Scholar] [CrossRef]
- Marttila-Ichihara, F.; Elima, K.; Auvinen, K.; Veres, T.Z.; Rantakari, P.; Weston, C.; Miyasaka, M.; Adams, D.; Jalkanen, S.; Salmi, M. Amine oxidase activity regulates the development of pulmonary fibrosis. FASEB J. 2017, 31, 2477–24791. [Google Scholar] [CrossRef] [PubMed]
- Chaudhary, N.I.; Roth, G.J.; Hilberg, F.; Müller-Quernheim, J.; Prasse, A.; Zissel, G.; Schnapp, A.; Park, J.E. Inhibition of PDGF, VEGF and FGF signalling attenuates fibrosis. Eur. Respir. J. 2007, 29, 976–985. [Google Scholar] [CrossRef]
- Hilberg, F.; Roth, G.J.; Krssak, M.; Kautschitsch, S.; Sommergruber, W.; Tontsch-Grunt, U.; Garin-Chesa, P.; Bader, G.; Zoephel, A.; Quant, J.; et al. BIBF 1120: Triple angiokinase inhibitor with sustained receptor blockade and good antitumor efficacy. Cancer Res. 2008, 68, 4774–4782. [Google Scholar] [CrossRef]
- Chiou, H.Y.C.; Wang, C.W.; Chen, S.C.; Tsai, M.L.; Lin, M.H.; Hung, C.H.; Kuo, C.H. Copper Exposure Induces Epithelial-Mesenchymal Transition-Related Fibrotic Change via Autophagy and Increase Risk of Lung Fibrosis in Human. Antioxidants 2023, 12, 532. [Google Scholar] [CrossRef] [PubMed]
- Skoczyńska, A.; Gruszczyński, L.; Wojakowska, A.; Ścieszka, M.; Turczyn, B.; Schmidt, E. Association between the Type of Workplace and Lung Function in Copper Miners. BioMed Res. Int. 2016, 2016, 5928572. [Google Scholar] [CrossRef]
- Pohanka, M. Copper and copper nanoparticles toxicity and their impact on basic functions in the body. Bratisl. Lek. Listy 2019, 120, 397–409. [Google Scholar] [CrossRef]
- Waas, W.F.; Dalby, K.N. Physiological concentrations of divalent magnesium ion activate the serine/threonine specific protein kinase ERK2. Biochemistry 2003, 42, 2960–2970. [Google Scholar] [CrossRef]
- Barbagallo, M.; Dominguez, L.J. Magnesium metabolism in type 2 diabetes mellitus, metabolic syndrome and insulin resistance. Arch. Biochem. Biophys. 2007, 458, 40–47. [Google Scholar] [CrossRef]
- Iyer, A.K.V.; Ramesh, V.; Castro, C.A.; Kaushik, V.; Kulkarni, Y.M.; Wright, C.A.; Venkatadri, R.; Rojanasakul, Y.; Azad, N. Nitric oxide mediates bleomycin-induced angiogenesis and pulmonary fibrosis via regulation of VEGF. J. Cell Biochem. 2015, 116, 2484–2493. [Google Scholar] [CrossRef] [PubMed]
- Fehrenbach, H.; Kasper, M.; Haase, M.; Schuh, D.; Muller, M. Differential immunolocalization of VEGF in rat and human adult lung, and in experimental rat lung fibrosis: Light, fluorescence, and electron microscopy. Anat. Rec. 1999, 254, 61–73. [Google Scholar] [CrossRef]
- Cameli, P.; Bergantini, L.; Salvini, M.; Refini, R.M.; Pieroni, M.; Bargagli, E.; Sestini, S. Alveolar concentration of nitric oxide as a prognostic biomarker in idiopathic pulmonary fibrosis. Nitric Oxide 2019, 89, 41–45. [Google Scholar] [CrossRef]
- Xu, F.; Wang, Q.; Jiang, L.; Zhu, F.; Yang, L.; Zhang, S. Evaluation of Nitric Oxide Fluctuation via a Fast, Responsive Fluorescent Probe in Idiopathic Pulmonary Fibrosis Cells and Mice Models. Anal. Chem. 2022, 94, 4072–4077. [Google Scholar] [CrossRef] [PubMed]
- Rock, E.; Astier, C.; Lab, C.; Malpuech, C.; Nowacki, W.; Gueux, E.; Mazur, A.; Rayssiguier, Y. Magnesium deficiency in rats induces a rise in plasma nitric oxide. Magnes. Res. 1995, 8, 237–242. [Google Scholar]
- Gomez, N.N.; Davicino, R.C.; Biaggio, V.S.; Bianco, G.A.; Alvarez, S.M.; Fischer, P.; Masnatta, L.; Rabinovich, G.A.; Gimenez, M.S. Overexpression of inducible nitric oxide synthase and cyclooxygenase-2 in rat zinc-deficient lung: Involvement of a NF-κB dependent pathway. Nitric Oxide 2006, 14, 30–38. [Google Scholar] [CrossRef] [PubMed]
- Cuzzocrea, S.; Persichini, T.; Dugo, L.; Colasanti, M.; Musci, G. Copper induces type II nitric oxide synthase in vivo. Free Radic. Biol. Med. 2003, 34, 1253–1262. [Google Scholar] [CrossRef]
- Murray, P.J. Macrophage polarization. Annu. Rev. Physiol. 2017, 79, 541–566. [Google Scholar] [CrossRef] [PubMed]
- Lech, M.; Anders, H.-J. Macrophages and fibrosis: How resident and infiltrating mononuclear phagocytes orchestrate all phases of tissue injury and repair. Biochim. Biophys. Acta 2013, 1832, 989–997. [Google Scholar] [CrossRef]
- Song, E.; Ouyang, N.; Hörbelt, M.; Antus, B.; Wang, M.; Exton, M.S. Influence of alternatively and classically activated macrophages on fibrogenic activities of human fibroblasts. Cell. Immunol. 2000, 204, 19–28. [Google Scholar] [CrossRef] [PubMed]
- Luo, Q.; Deng, D.; Li, Y.; Shi, H.; Zhao, J.; Qian, Q.; Wang, W.; Cai, J.; Yu, W.; Liu, J. TREM2 Insufficiency Protects against Pulmonary Fibrosis by Inhibiting M2 Macrophage Polarization. Int. Immunopharmacol. 2023, 118, 110070. [Google Scholar] [CrossRef]
- Zhang, M.; Zhang, J.; Hu, H.; Zhou, Y.; Lin, Z.W.; Jing, H.; Sun, B. Multiomic analysis of monocyte-derived alveolar macrophages in idiopathic pulmonary fibrosis. J. Transl. Med. 2024, 22, 598. [Google Scholar] [CrossRef]
- Yokoyama, T.; Oono, H.; Miyamoto, A.; Ishiguro, S.; Nishio, A. Magnesium-deficient medium enhances NO production in alveolar macrophages isolated from rats. Life Sci. 2003, 72, 1247–1257. [Google Scholar] [CrossRef]
- Lang, C.J.; Hansen, M.; Roscioli, E.; Jones, J.; Murgia, C.; Ackland, M.L.; Zalewski, P.; Anderson, G.; Ruffin, R. Dietary zinc mediates inflammation and protects against wasting and metabolic derangement caused by sustained cigarette smoke exposure in mice. Biometals 2011, 24, 23–39. [Google Scholar] [CrossRef]
- Abul, H.T.; Abul, A.T.; Al-Athary, E.A.; Behbehani, A.E.; Khadadah, M.E.; Dashti, H.M. Interleukin-1α (IL-1α) production by alveolar macrophages in patients with acute lung diseases: The influence of zinc supplementation. Mol. Cell. Biochem. 1995, 146, 139–145. [Google Scholar] [CrossRef]
- Hodgkinson, V.; Petris, M.J. Copper homeostasis at the host-pathogen interface. J. Biol. Chem. 2012, 287, 13549–13555. [Google Scholar] [CrossRef]
- Kim, H.W.; Chan, Q.; Afton, S.E.; Caruso, J.A.; Lai, B.; Weintraub, N.L.; Qin, Z. Human macrophage ATP7A is localized in the trans-Golgi apparatus, controls intracellular copper levels, and mediates macrophage responses to dermal wounds. Inflammation 2012, 35, 167–175. [Google Scholar] [CrossRef] [PubMed]
- Oyarzún, G.M.J.; Sánchez, S.A.; Dussaubat, D.N.; Miller, A.M.E.; González, B.S. Effect of copper sulphate on the lung damage induced by chronic intermittent exposure to ozone. Rev. Med. Chil. 2017, 145, 9–16. [Google Scholar] [CrossRef]
- Knoell, D.L.; Smith, D.A.; Sapkota, M.; Heires, A.J.; Hanson, C.K.; Smith, L.M.; Poole, J.A.; Wyatt, T.A.; Romberger, D.J. Insufficient zinc intake enhances lung inflammation in response to agricultural organic dust exposure. J. Nutr. Biochem. 2019, 70, 56–64. [Google Scholar] [CrossRef]
- Joshi, P.C.; Mehta, A.; Jabber, W.J.; Fan, X.; Guidot, D.M. Zinc deficiency mediates alcohol-induced alveolar epithelial and macrophage dysfunction in rats. Am. J. Respir. Cell Mol. Biol. 2009, 41, 207–216. [Google Scholar] [CrossRef]
- Kim, K.K.; Dotson, M.R.; Agarwal, M.; Yang, J.; Bradley, P.B.; Subbotina, N.; Osterholzer, J.J.; Sisson, T.H. Efferocytosis of apoptotic alveolar epithelial cells is sufficient to initiate lung fibrosis. Cell Death Dis. 2018, 9, 1056. [Google Scholar] [CrossRef]
- Sisson, T.H.; Mendez, M.; Choi, K.; Subbotina, N.; Courey, A.; Cunningham, A.; Dave, A.; Engelhardt, J.F.; Liu, X.; White, E.S.; et al. Targeted injury of type II alveolar epithelial cells induces pulmonary fibrosis. Am. J. Respir. Crit. Care Med. 2010, 181, 254–263. [Google Scholar] [CrossRef]
- Barkauskas, C.E.; Cronce, M.J.; Rackley, C.R.; Bowie, E.J.; Keene, D.R.; Stripp, B.R.; Randell, S.H.; Noble, P.W.; Hogan, B.L.M. Type 2 alveolar cells are stem cells in adult lung. J. Clin. Investig. 2013, 123, 3025–3036. [Google Scholar] [CrossRef]
- Parimon, T.; Yao, C.; Stripp, B.R.; Noble, P.W.; Chen, P. Alveolar Epithelial Type II Cells as Drivers of Lung Fibrosis in Idiopathic Pulmonary Fibrosis. Int. J. Mol. Sci. 2020, 21, 2269. [Google Scholar] [CrossRef] [PubMed]
- Selman, M.; King, T.E.; Pardo, A. Idiopathic pulmonary fibrosis: Prevailing and evolving hypotheses about its pathogenesis and implications for therapy. Ann. Intern. Med. 2001, 134, 136–151. [Google Scholar] [CrossRef]
- Alder, J.K.; Barkauskas, C.E.; Limjunyawong, N.; Stanley, S.E.; Kembou, F.; Tuder, R.M.; Hogan, B.L.M.; Mitzner, W.; Armanios, M. Telomere dysfunction causes alveolar stem cell failure. Proc. Natl. Acad. Sci. USA 2015, 112, 5099–5104. [Google Scholar] [CrossRef]
- Snetselaar, R.; van Batenburg, A.A.; van Oosterhout, M.F.M.; Kazemier, K.M.; Roothaan, S.M.; Peeters, T.; Van Der Vis, J.J.; Goldschmeding, R.; Grutters, J.C.; Van Moorsel, C.H.M. Short telomere length in IPF lung associates with fibrotic lesions and predicts survival. PLoS ONE 2017, 12, e0189467. [Google Scholar] [CrossRef]
- Barbas-Filho, J.V.; Ferreira, M.A.; Sesso, A.; Kairalla, R.A.; Carvalho, C.R.; Capelozzi, V.L. Evidence of type II pneumocyte apoptosis in the pathogenesis of idiopathic pulmonary fibrosis (IFP)/usual interstitial pneumonia (UIP). J. Clin. Pathol. 2001, 54, 132–138. [Google Scholar] [CrossRef]
- Li, X.; Wang, Y.; Liang, J.; Bi, Z.; Ruan, H.; Cui, Y.; Ma, L.; Wei, Y.; Zhou, B.; Zhang, L.; et al. Bergenin attenuates bleomycin-induced pulmonary fibrosis in mice via inhibiting TGF-β1 signaling pathway. Phytother. Res. 2021, 35, 5808–5822. [Google Scholar] [CrossRef] [PubMed]
- Chu, L.; Zhuo, J.; Huang, H.; Chen, W.; Zhong, W.; Zhang, J.; Meng, X.; Zou, F.; Cai, S.; Zou, M.; et al. Tetrandrine alleviates pulmonary fibrosis by inhibiting alveolar epithelial cell senescence through PINK1/Parkin-mediated mitophagy. Eur. J. Pharmacol. 2024, 969, 176459. [Google Scholar] [CrossRef]
- Xiao, H.; Peng, L.; Jiang, D.; Liu, Y.; Zhu, L.; Li, Z.; Geng, J.; Xie, B.; Huang, X.; Wang, J.; et al. IL-17A promotes lung fibrosis through impairing mitochondrial homeostasis in type II alveolar epithelial cells. J. Cell. Mol. Med. 2022, 26, 5728–5741. [Google Scholar] [CrossRef] [PubMed]
- Kasper, M.; Barth, K. Potential contribution of alveolar epithelial type I cells to pulmonary fibrosis. Biosci. Rep. 2017, 37, BSR20171301. [Google Scholar] [CrossRef]
- Shi, X.; Zhu, L.; Wang, S.; Zhu, W.; Li, Q.; Wei, J.; Feng, D.; Liu, M.; Chen, Y.; Sun, X.; et al. Magnesium Hydride Ameliorates Endotoxin-Induced Acute Respiratory Distress Syndrome by Inhibiting Inflammation, Oxidative Stress, and Cell Apoptosis. Oxidative Med. Cell Longev. 2022, 26, 5918954. [Google Scholar] [CrossRef] [PubMed]
- Liang, J.; Huang, G.; Liu, X.; Taghavifar, F.; Liu, N.; Wang, Y.; Deng, N.; Yao, C.; Xie, T.; Kulur, V.; et al. 1ZIP8/SIRT1 axis regulates alveolar progenitor cell renewal in aging and idiopathic pulmonary fibrosis. J. Clin. Investig. 2022, 132, e157338. [Google Scholar] [CrossRef]
- Moschini, E.; Gualtieri, M.; Colombo, M.; Fascio, U.; Camatini, M.; Mantecca, P. The modality of cell-particle interactions drives the toxicity of nanosized CuO and TiO2 in human alveolar epithelial cells. Toxicol. Lett. 2013, 222, 102–116. [Google Scholar] [CrossRef]
- Isler, J.A.; Skalet, A.H.; Alwine, J.C. Human cytomegalovirus infection activates and regulates the unfolded protein response. J. Virol. 2005, 79, 6890–6899. [Google Scholar] [CrossRef]
- Tang, Y.-W.; Johnson, J.E.; Browning, P.J.; Cruz-Gervis, R.A.; Davis, A.; Graham, B.S.; Brigham, K.L.; Oates, J.A., Jr.; Loyd, J.E.; Stecenko, A.A. Herpesvirus DNA is consistently detected in lungs of patients with idiopathic pulmonary fibrosis. J. Clin. Microbiol. 2003, 41, 2633–2640. [Google Scholar] [CrossRef] [PubMed]
- Geng, J.; Liu, Y.Y.; Dai, H.; Wang, C. Fatty Acid Metabolism and Idiopathic Pulmonary fibrosis. Front. Physiol. 2022, 12, 794629. [Google Scholar] [CrossRef]
- Chu, S.G.; Villalba, J.A.; Liang, X.; Xiong, K.; Tsoyi, K.; Ith, B.; Ayaub, E.A.; Tatituri, R.V.; Byers, D.E.; Hsu, F.-F.; et al. Palmitic acid-rich high-fat diet exacerbates experimental pulmonary fibrosis by modulating endoplasmic reticulum stress. Am. J. Respir. Cell Mol. Biol. 2019, 61, 737–746. [Google Scholar] [CrossRef] [PubMed]
- Kim, H.; Yoo, H.J.; Lee, K.M.; Song, H.E.; Kim, S.J.; Lee, J.O.; Hwang, J.J.; Song, J.W. Stearic acid attenuates profibrotic signalling in idiopathic pulmonary fibrosis. Respirology 2021, 26, 255–263. [Google Scholar] [CrossRef]
- Soma, M.; Cunnane, S.C.; Horrobin, D.F.; Manku, M.S.; Honda, M.; Hatano, M. Effects of low magnesium diet on the vascular prostaglandin and fatty acid metabolism in rats. Prostaglandins 1988, 36, 431–441. [Google Scholar] [CrossRef]
- Dieck, H.T.; Döring, F.; Fuchs, D.; Roth, H.P.; Daniel, H. Transcriptome and proteome analysis identifies the pathways that increase hepatic lipid accumulation in zinc-deficient rats. J. Nutr. 2005, 135, 199–205. [Google Scholar] [CrossRef]
- Zhu, D.; Zhang, Y.; Li, S.; Gan, L.; Feng, H.; Nie, W. Enteral omega-3 fatty acid supplementation in adult patients with acute respiratory distress syndrome: A systematic review of randomized controlled trials with meta-analysis and trial sequential analysis. Intensive Care Med. 2014, 40, 504–512. [Google Scholar] [CrossRef]
- Charbeneau, R.P.; Peters-Golden, M. Eicosanoids: Mediators and therapeutic targets in fibrotic lung disease. Clin. Sci. 2005, 108, 479–491. [Google Scholar] [CrossRef] [PubMed]
- Silva, R.C.; Landgraf, M.A.; Hiyane, M.I.; Pacheco-Silva, A.; Câmara, N.O.; Landgraf, R.G. Leukotrienes produced in allergic lung inflammation activate alveolar macrophages. Cell. Physiol. Biochem. 2010, 26, 319–326. [Google Scholar] [CrossRef] [PubMed]
- Wetterholm, A.; Macchia, L.; Haeggström, J.Z. Zinc and other divalent cations inhibit purified leukotriene A4 hydrolase and leukotriene B4 biosynthesis in human polymorphonuclear leukocytes. Arch. Biochem. Biophys. 1994, 311, 263–271. [Google Scholar] [CrossRef]
- Gales, C.; Stoica, B.; Rusu-Zota, G.; Nechifor, M. Montelukast Influence on Lung in Experimental Diabetes. Medicina 2024, 60, 749. [Google Scholar] [CrossRef]
- Jenkins, K.J.; Kramer, J.K. Changes in lipid composition of calf tissues by excess dietary zinc. J. Dairy Sci. 1992, 75, 1313–1319. [Google Scholar] [CrossRef]
- Nechifor, M.; Cuciureanu, M.; Chelarescu, D.; Ciubotariu, D.; Pascu, M. Magnesium and other bivalent cations influence upon sodium montelukast effect in experimental-induced thermoalgesia. Magnes. Res. 2008, 21, 38–42. [Google Scholar]
- Genovese, T.; Cuzzocrea, S.; Di Paola, R.; Mazzon, E.; Mastruzzo, C.; Catalano, P.; Sortino, M.; Crimi, N.; Caputi, A.P.; Thiemermann, C.; et al. Effect of rosiglitazone and 15-deoxy-Delta12, 14-prostaglandin J2 on bleomycin-induced lung injury. Eur. Respir. J. 2005, 25, 225–234. [Google Scholar] [CrossRef] [PubMed]
- Oga, T.; Matsuoka, T.; Yao, C.; Nonomura, K.; Kitaoka, S.; Sakata, D.; Kita, Y.; Tanizawa, K.; Taguchi, Y.; Chin, K.; et al. Prostaglandin F(2α) receptor signaling facilitates bleomycin-induced pulmonary fibrosis independently of transforming growth factor-beta. Nat. Med. 2009, 15, 1426–1430. [Google Scholar] [CrossRef]
- Brennan, E.P.; Cacace, A.; Godson, C. Specialized pro-resolving mediators in renal fibrosis. Mol. Asp. Med. 2017, 58, 102–113. [Google Scholar] [CrossRef]
- Mariqueo, T.A.; Zúñiga-Hernández, J. Omega-3 derivatives, specialized pro-resolving mediators: Promising therapeutic tools for the treatment of pain in chronic liver disease. Prostaglandins Leukot. Essent. Fat. Acids 2020, 158, 102095. [Google Scholar] [CrossRef] [PubMed]
- Serhan, C.N.; Dalli, J.; Karamnov, S.; Choi, A.; Park, C.-K.; Xu, Z.-Z.; Ji, R.-R.; Zhu, M.; Petasis, N.A. Macrophage proresolving mediator maresin 1 stimulates tissue regeneration and controls pain. FASEB J. 2012, 26, 1755–1765. [Google Scholar] [CrossRef]
- Xie, C.; Li, X.; Wu, J.; Liang, Z.; Deng, F.; Xie, W.; Zhu, M.; Zhu, J.; Zhu, W.; Geng, S.; et al. Anti-inflammatory Activity of Magnesium Isoglycyrrhizinate Through Inhibition of Phospholipase A2/Arachidonic Acid Pathway. Inflammation 2015, 38, 1639–1648. [Google Scholar] [CrossRef]
- Ludwig, P.; Petrich, K.; Schewe, T.; Diezel, W. Inhibition of eicosanoid formation in human polymorphonuclear leukocytes by high concentrations of magnesium ions. Biol. Chem. Hoppe Seyler 1995, 376, 739–744. [Google Scholar] [CrossRef]
- Mezna, M.; Ahmad, T.; Chettibi, S.; Drainas, D.; Lawrence, A.J. Zinc and barium inhibit the phospholipase A2 from Naja naja atra by different mechanisms. Biochem. J. 1994, 301, 503–508. [Google Scholar] [CrossRef]
- Nito, C.; Kamada, H.; Endo, H.; Niizuma, K.; Myer, D.J.; Chan, P.H. Role of the p38 mitogen-activated protein kinase/cytosolic phospholipase A2 signaling pathway in blood-brain barrier disruption after focal cerebral ischemia and reperfusion. J. Cereb. Blood Flow. Metab. 2008, 28, 1686–1696. [Google Scholar] [CrossRef]
- Milanino, R.; Passarella, E.; Velo, G.P. Adjuvant arthritis in young copper-deficient rats. Agents Actions 1978, 8, 623–628. [Google Scholar] [CrossRef] [PubMed]
- Ponist, S.; Valentová, J.; Bezáková, L.; Oblozinský, M. Antilipoxygenase activity of copper complexes of aminoalkanoate type. Neuro Endocrinol. Lett. 2006, 27, 180–182. [Google Scholar] [PubMed]
- Li, X.; Xie, M.; Lu, C.; Mao, J.; Cao, Y.; Yang, Y.; Wei, Y.; Liu, X.; Cao, S.; Song, Y.; et al. Design and synthesis of Leukotriene A4 hydrolase inhibitors to alleviate idiopathic pulmonary fibrosis and acute lung injury. Eur. J. Med. Chem. 2020, 203, 112614. [Google Scholar] [CrossRef]
- Khodabakhsh, P.; Khoie, N.; Dehpour, A.R.; Abdollahi, A.; Ghazi-Khansari, M.; Shafaroodi, H. Montelukast suppresses the development of irritable bowel syndrome phenotype possibly through modulating NF-κB signaling in an experimental model. Inflammopharmacology 2022, 30, 313–325. [Google Scholar] [CrossRef]
- Fireman, E.; Schwartz, Y.; Mann, A.; Greif, J. Effect of montelukast, a cysteinyl receptor antagonist, on myofibroblasts in interstitial lung disease. J. Clin. Immunol. 2004, 24, 418–425. [Google Scholar] [CrossRef] [PubMed]
- Shimbori, C.; Shiota, N.; Okunishi, H. Effects of montelukast, a cysteinyl-leukotriene type 1 receptor antagonist, on the pathogenesis of bleomycin-induced pulmonary fibrosis in mice. Eur. J. Pharmacol. 2011, 650, 424–430. [Google Scholar] [CrossRef]
- Ong, T.J.; Kemp, P.J.; Oliver, R.E.; McArdle, H.J. Characterization of zinc uptake and its regulation by arachidonic acid in fetal type II pneumocytes. Am. J. Physiol. 1995, 269, L71–L77. [Google Scholar] [CrossRef]
- Xu, Y.; Mizuno, T.; Sridharan, A.; Du, Y.; Guo, M.; Tang, J.; Wikenheiser-Brokamp, K.A.; Perl, A.-K.T.; Funari, V.A.; Gokey, J.J.; et al. Single-cell RNA sequencing identifies diverse roles of epithelial cells in idiopathic pulmonary fibrosis. JCI Insight 2016, 1, e90558. [Google Scholar] [CrossRef]
- Zhang, K.; Wang, L.; Hong, X.; Chen, H.; Shi, Y.; Liu, Y.; Liu, J.; Liu, J.P. Pulmonary Alveolar Stem Cell Senescence, Apoptosis, and Differentiation by p53-Dependent and -Independent Mechanisms in Telomerase-Deficient Mice. Cells 2021, 10, 2892. [Google Scholar] [CrossRef]
- Takahashi, T.; Munakata, M.; Ohtsuka, Y.; Nisihara, H.; Nasuhara, Y.; Kamachi-Satoh, A.; Dosaka-Akita, H.; Homma, Y.; Kawakami, Y. Expression and alteration of ras and p53 proteins in patients with lung carcinoma accompanied by idiopathic pulmonary fibrosis. Cancer 2002, 95, 624–633. [Google Scholar] [CrossRef] [PubMed]
- Shetty, S.; Idell, S. Caveolin-1-Related Intervention for Fibrotic Lung Diseases. Cells 2023, 12, 554. [Google Scholar] [CrossRef]
- Iezhitsa, I.; Lambuk, L.; Agarwal, R.; Agarwal, P.; Peresypkina, A.; Pobeda, A.; Ismail, N.M. Magnesium acetyltaurate prevents retinal damage and visual impairment in rats through suppression of NMDA-induced upregulation of NF-κB, p53 and AP-1 (c-Jun/c-Fos). Neural Regen. Res. 2021, 16, 2330–2344. [Google Scholar] [CrossRef]
- Chen, P.M.; Wu, T.C.; Wang, Y.C.; Cheng, Y.C.; Sheu, G.T.; Chen, C.Y.; Lee, H. Activation of NF-κB by SOD2 promotes the aggressiveness of lung adenocarcinoma by modulating NKX2-1-mediated IKKβ expression. Carcinogenesis 2013, 34, 2655–2663. [Google Scholar] [CrossRef]
- Inchehsablagh, B.R.; Soufi, F.G.; Koochakkhani, S.; Azarkish, F.; Farshidi, H.; Eslami, M.; Mahmoodi, M.; Soltani, N.; Eftekhar, E. Magnesium Supplementation Affects the Expression of Sirtuin1, Tumor Protein P53 and Endothelial Nitric Oxide Synthase Genes in Patients with Atherosclerosis: A Double-Blind, Randomized, Placebo-Controlled Trial. Indian J. Clin. Biochem. 2023, 38, 59–66. [Google Scholar] [CrossRef] [PubMed]
- Clegg, M.S.; Hanna, L.A.; Niles, B.J.; Momma, T.Y.; Keen, C.L. Zinc deficiency-induced cell death. UBMB Life 2005, 57, 661–669. [Google Scholar] [CrossRef] [PubMed]
- Formigari, A.; Gregianin, E.; Irato, P. The effect of zinc and the role of p53 in copper-induced cellular stress responses. J. Appl. Toxicol. 2013, 33, 527–536. [Google Scholar] [CrossRef]
- Sauve, A.A.; Schramm, V.L. SIR2: The biochemical mechanism of NAD(+)-dependent protein deacetylation and ADP-ribosyl enzyme intermediates. Curr. Med. Chem. 2004, 11, 807–826. [Google Scholar] [CrossRef]
- Zhang, Y.; Huang, W.; Zheng, Z.; Wang, W.; Yuan, Y.; Hong, Q.; Lin, J.; Li, X.; Meng, Y. Cigarette smoke-inactivated SIRT1 promotes autophagy-dependent senescence of alveolar epithelial type 2 cells to induce pulmonary fibrosis. Free Radic. Biol. Med. 2021, 166, 116–127. [Google Scholar] [CrossRef]
- Peng, Z.; Zhang, W.; Qiao, J.; He, B. Melatonin attenuates airway inflammation via SIRT1 dependent inhibition of NLRP3 inflammasome and IL-1β in rats with COPD. Int. Immunopharmacol. 2018, 62, 23–28. [Google Scholar] [CrossRef]
- Nogueiras, R.; Habegger, K.M.; Chaudhary, N.; Finan, B.; Banks, A.S.; Dietrich, M.O.; Horvath, T.L.; Sinclair, D.A.; Pfluger, P.T.; Tschöop, M.H. Sirtuin 1 and sirtuin 3: Physiological modulators of metabolism. Physiol. Rev. 2012, 92, 1479–1514. [Google Scholar] [CrossRef] [PubMed]
- Kobayashi, E.H.; Suzuki, T.; Funayama, R.; Nagashima, T.; Hayashi, M.; Sekine, H.; Tanaka, N.; Moriguchi, T.; Motohashi, H.; Nakayama, K.; et al. Nrf2 suppresses macrophage inflammatory response by blocking proinflammatory cytokine transcription. Nat. Commun. 2016, 7, 11624. [Google Scholar] [CrossRef] [PubMed]
- Foster, P.S.; Tay, H.L.; Oliver, B.G. Deficiency in the zinc transporter ZIP8 impairs epithelia renewal and enhances lung fibrosis. J. Clin. Investig. 2022, 132, e160595. [Google Scholar] [CrossRef]
- Jablonski, R.P.; Kim, S.; Cheresh, P.; Williams, D.B.; Morales-Nebreda, L.; Cheng, Y.; Yeldandi, A.; Bhorade, S.; Pardo, A.; Selman, M.; et al. SIRT3 deficiency promotes lung fibrosis by augmenting alveolar epithelial cell mitochondrial DNA damage and apoptosis. FASEB J. 2017, 31, 2520–2532. [Google Scholar] [CrossRef] [PubMed]
- Ravishankar, S.; Ashraf, Q.M.; Fritz, K.; Mishra, O.P.; Delivoria-Papadopoulos, M. Expression of Bax and Bcl-2 proteins during hypoxia in cerebral cortical neuronal nuclei of newborn piglets: Effect of administration of magnesium sulfate. Brain Res. 2001, 901, 23–29. [Google Scholar] [CrossRef]
- Wei, Z.; Sun, X.; He, Q.; Zhao, Y.; Wu, Y.; Han, X.; Wu, Z.; Chu, X.; Guan, S. Nephroprotective effect of magnesium isoglycyrrhizinate against arsenic trioxide-induced acute kidney damage in mice. Exp. Ther. Med. 2022, 23, 276. [Google Scholar] [CrossRef]
- Larson-Casey, J.L.; Deshane, J.S.; Ryan, A.J.; Thannickal, V.J.; Carter, A.B. Macrophage Akt1 kinase-mediated mitophagy modulates apoptosis resistance and pulmonary fibrosis. Immunity 2016, 44, 582–596. [Google Scholar] [CrossRef]
- Wu, Q.; Zhang, K.-J.; Jiang, S.-M.; Fu, L.; Shi, Y.; Tan, R.-B.; Cui, J.; Zhou, Y. p53: A Key Protein That Regulates Pulmonary Fibrosis. Oxidative Med. Cell Longev. 2020, 6635794. [Google Scholar] [CrossRef]
- Komiya, C.; Tanaka, M.; Tsuchiya, K.; Shimazu, N.; Mori, K.; Furuke, S.; Miyachi, Y.; Shiba, K.; Yamaguchi, S.; Ikeda, K.; et al. Antifibrotic effect of pirfenidone in a mouse model of human nonalcoholic steatohepatitis. Sci. Rep. 2017, 7, 44754. [Google Scholar] [CrossRef]
- Cho, H.-J.; Hwang, J.-A.; Yang, E.J.; Kim, E.-C.; Kim, J.-R.; Kim, S.Y.; Kim, Y.Z.; Park, S.C.; Lee, Y.-S. Nintedanib induces senolytic effect via STAT3 inhibition. Cell Death Dis. 2022, 13, 760. [Google Scholar] [CrossRef]
- Zischka, H.; Kroemer, G. Copper—A novel stimulator of autophagy. Cell Stress 2020, 4, 92–94. [Google Scholar] [CrossRef]
- Xue, Q.; Kang, R.; Klionsky, D.J. Copper metabolism in cell death and autophagy. Autophagy 2023, 19, 2175–2195. [Google Scholar] [CrossRef]
- Jian, Z.; Guo, H.; Liu, H.; Cui, H.; Fang, J.; Zuo, Z.; Deng, J.; Li, Y.; Wang, X.; Zhao, L. Oxidative stress, apoptosis and inflammatory responses involved in copper-induced pulmonary toxicity in mice. Aging 2020, 12, 16867–16886. [Google Scholar] [CrossRef]
- Kang, Z.; Qiao, N.; Liu, G.; Chen, H.; Tang, Z.; Li, Y. Copper-induced apoptosis and autophagy through oxidative stress-mediated mitochondrial dysfunction in male germ cells. Toxicol. Vitr. 2019, 61, 104639. [Google Scholar] [CrossRef] [PubMed]
- Derseh, H.B.; Perera, K.U.E.; Dewage, S.N.V.; Stent, A.; Koumoundouros, E.; Organ, L.; Pagel, C.N.; Snibson, K.J. Tetrathiomolybdate Treatment Attenuates Bleomycin-Induced Angiogenesis and Lung Pathology in a Sheep Model of Pulmonary Fibrosis. Front. Pharmacol. 2021, 12, 700902. [Google Scholar] [CrossRef] [PubMed]
- Plataki, M.; Koutsopoulos, A.V.; Darivianaki, A.V.; Delides, G.; Siafakas, N.M.; Bouros, D. Expression of apoptotic and antiapoptotic markers in epithelial cells in idiopathic pulmonary fibrosis. Chest 2005, 127, 266–274. [Google Scholar] [CrossRef]
- Ronan, N.; Bennett, D.M.; Khan, K.A.; McCarthy, Y.; Dahly, D.; Bourke, L.; Chelliah, A.; Cavazza, A.; O’rEgan, K.; Moloney, F.; et al. Tissue and Bronchoalveolar Lavage Biomarkers in Idiopathic Pulmonary Fibrosis Patients on Pirfenidone. Lung 2018, 196, 543–552. [Google Scholar] [CrossRef] [PubMed]
- Xaubet, A.; Marin-Arguedas, A.; Lario, S.; Ancochea, J.; Morell, F.; Ruiz-Manzano, J.; Rodriguez-Becerra, E.; Rodriguez-Arias, J.M.; Iñigo, P.; Sanz, S.; et al. Transforming growth factor-β1 gene polymorphisms are associated with disease progression in idiopathic pulmonary fibrosis. Am. J. Respir. Crit. Care Med. 2003, 168, 431–435. [Google Scholar] [CrossRef]
- Wang, H.; Xu, H.; Lyu, W.; Xu, Q.; Fan, S.; Chen, H.; Wang, D.; Chen, J.; Dai, J. KLF4 regulates TERT expression in alveolar epithelial cells in pulmonary fibrosis. Cell Death Dis. 2022, 13, 435. [Google Scholar] [CrossRef]
- Demedts, M.; Behr, J.; Buhl, R.; Costabel, U.; Dekhuijzen, R.; Jansen, H.M.; MacNee, W.; Thomeer, M.; Wallaert, B.; Laurent, F.; et al. High-dose acetylcysteine in idiopathic pulmonary fibrosis. N. Engl. J. Med. 2005, 353, 2229–2242. [Google Scholar] [CrossRef]
- Raghu, G.; Selman, M. Nintedanib and pirfenidone. New antifibrotic treatments indicated for idiopathic pulmonary fibrosis offer hopes and raises questions. Am. J. Respir. Crit. Care Med. 2015, 191, 252–254. [Google Scholar] [CrossRef]
- Liu, Y.; Lu, F.; Kang, L.; Wang, Z.; Wang, Y. Pirfenidone attenuates bleomycin-induced pulmonary fibrosis in mice by regulating Nrf2/Bach1 equilibrium. BMC Pulm. Med. 2017, 17, 63. [Google Scholar] [CrossRef]
- Kou, N.; Chen, Y.-B.; Li, X.-W.; Xu, D.; Wang, Y.; Dong, X.-R.; Cui, Y.-L.; Wang, Q. Pulmonary administration of tetrandrine loaded Zinc-Alginate nanogels attenuates pulmonary fibrosis in rats. Int. J. Pharm. 2024, 649, 123625. [Google Scholar] [CrossRef]
- Homma, S.; Azuma, A.; Taniguchi, H.; Ogura, T.; Mochiduki, Y.; Sugiyama, Y.; Nakata, K.; Yoshimura, K.; Takeuchi, M.; Kudoh, S.; et al. Efficacy of inhaled N-acetylcysteine monotherapy in patients with early stage idiopathic pulmonary fibrosis. Respirology 2012, 17, 467–477. [Google Scholar] [CrossRef] [PubMed]
- Misra, H.P.; Rabideau, C. Pirfenidone inhibits NADPH-dependent microsomal lipid peroxidation and scavenges hydroxyl radicals. Mol. Cell. Biochem. 2000, 204, 119–126. [Google Scholar] [CrossRef] [PubMed]
- Leenders, N.H.J.; van Ittersum, F.J.; Hoekstra, T.; Hoenderop, J.G.J.; Vervloet, M.G. Routine hemodialysis induces a decline in plasma magnesium concentration in most patients: A prospective observational cohort study. Sci. Rep. 2018, 8, 10256. [Google Scholar] [CrossRef] [PubMed]
- Rodelo-Haad, C.; Pendón-Ruiz de Mier, M.V.; Díaz-Tocados, J.M.; Martin-Malo, A.; Santamaria, R.; Muñoz-Castañeda, J.R.; Rodriguez, M. The Role of Disturbed Mg Homeostasis in Chronic Kidney Disease Comorbidities. Front. Cell Dev. Biol. 2020, 8, 543099. [Google Scholar] [CrossRef]
- Qu, C.; Xu, Y.; Yang, X.; Lu, X. Magnesium lithospermate B improves pulmonary artery banding induced right ventricular dysfunction by alleviating inflammation via p38MAPK pathway. Pulm. Pharmacol. Ther. 2020, 63, 101935. [Google Scholar] [CrossRef]
- Dos Santos, M.I.S.; Molle, R.D.; Silva, F.M.; Rodrigues, T.W.; Feldmann, M.; Forte, G.C.; Marostica, P.J.C. Antioxidant Micronutrients and Essential Fatty Acids Supplementation on Cystic Fibrosis Outcomes: A Systematic Review. J. Acad. Nutr. Diet. 2020, 120, 1016–1033.e1. [Google Scholar] [CrossRef]
- Wang, D.; Zhu, Z.-L.; Lin, D.-C.; Zheng, S.-Y.; Chuang, K.-H.; Gui, L.-X.; Yao, R.-H.; Zhu, W.-J.; Sham, J.S.; Lin, M.-J. Magnesium Supplementation Attenuates Pulmonary Hypertension via Regulation of Magnesium Transporters. Hypertension 2021, 77, 617–631. [Google Scholar] [CrossRef]
- Bethou, A. Utility of Nebulized Magnesium Sulfate Therapy for Persistent Pulmonary Hypertension of Newborn. Indian J. Pediatr. 2021, 88, 749–750. [Google Scholar] [CrossRef]
- Chen, W.; Chen, A.; Lian, G.; Yan, Y.; Liu, J.; Wu, J.; Gao, G.; Xie, L. Zinc attenuates monocrotaline-induced pulmonary hypertension in rats through upregulation of A20. J. Mol. Cell. Cardiol. 2024, 195, 24–35. [Google Scholar] [CrossRef]
- Li, T.; Luo, X.-J.; Wang, E.-L.; Li, N.-S.; Zhang, X.-J.; Song, F.-L.; Yang, J.-F.; Liu, B.; Peng, J. Magnesium lithospermate B prevents phenotypic transformation of pulmonary arteries in rats with hypoxic pulmonary hypertension through suppression of NADPH oxidase. Eur. J. Pharmacol. 2019, 847, 32–41. [Google Scholar] [CrossRef]
- Zhao, D.; Chen, P.; Chen, M.; Chen, L.; Wang, L. Association of Magnesium Depletion Score with Congestive Heart Failure: Results from the NHANES 2007–2016. Biol. Trace Elem. Res. 2024, 202, 454–465. [Google Scholar] [CrossRef]
- Lin, B.; Alexander, R.; Fritzen, R.; Mills, S.; Stewart, A.J.; McCowan, C. Abnormal Plasma/Serum Magnesium, Copper, and Zinc Concentrations Associate with the Future Development of Cardiovascular Diseases. Nutrients 2025, 17, 1447. [Google Scholar] [CrossRef] [PubMed]
- Wang, W.; Wang, X.; Luo, J.; Chen, X.; Ma, K.; He, H.; Li, W.; Cui, J. Serum Copper Level and the Copper-to-Zinc Ratio Could Be Useful in the Prediction of Lung Cancer and Its Prognosis: A Case-Control Study in Northeast China. Nutr. Cancer 2021, 73, 1908–1915. [Google Scholar] [CrossRef] [PubMed]
- Feng, Y.; Gao, M.; Xu, X.; Liu, H.; Lu, K.; Song, Z.; Yu, J.; Liu, X.; Han, X.; Li, L.; et al. Elevated serum magnesium levels prompt favourable outcomes in cancer patients treated with immune checkpoint blockers. Eur. J. Cancer 2024, 213, 115069. [Google Scholar] [CrossRef] [PubMed]
- Charoenngam, N.; Ponvilawan, B.; Ungprasert, P. Higher zinc intake is associated with decreased risk of lung cancer. J. Evid. Based Med. 2021, 14, 185–187. [Google Scholar] [CrossRef] [PubMed]

| Mg2+ Actions | |
|---|---|
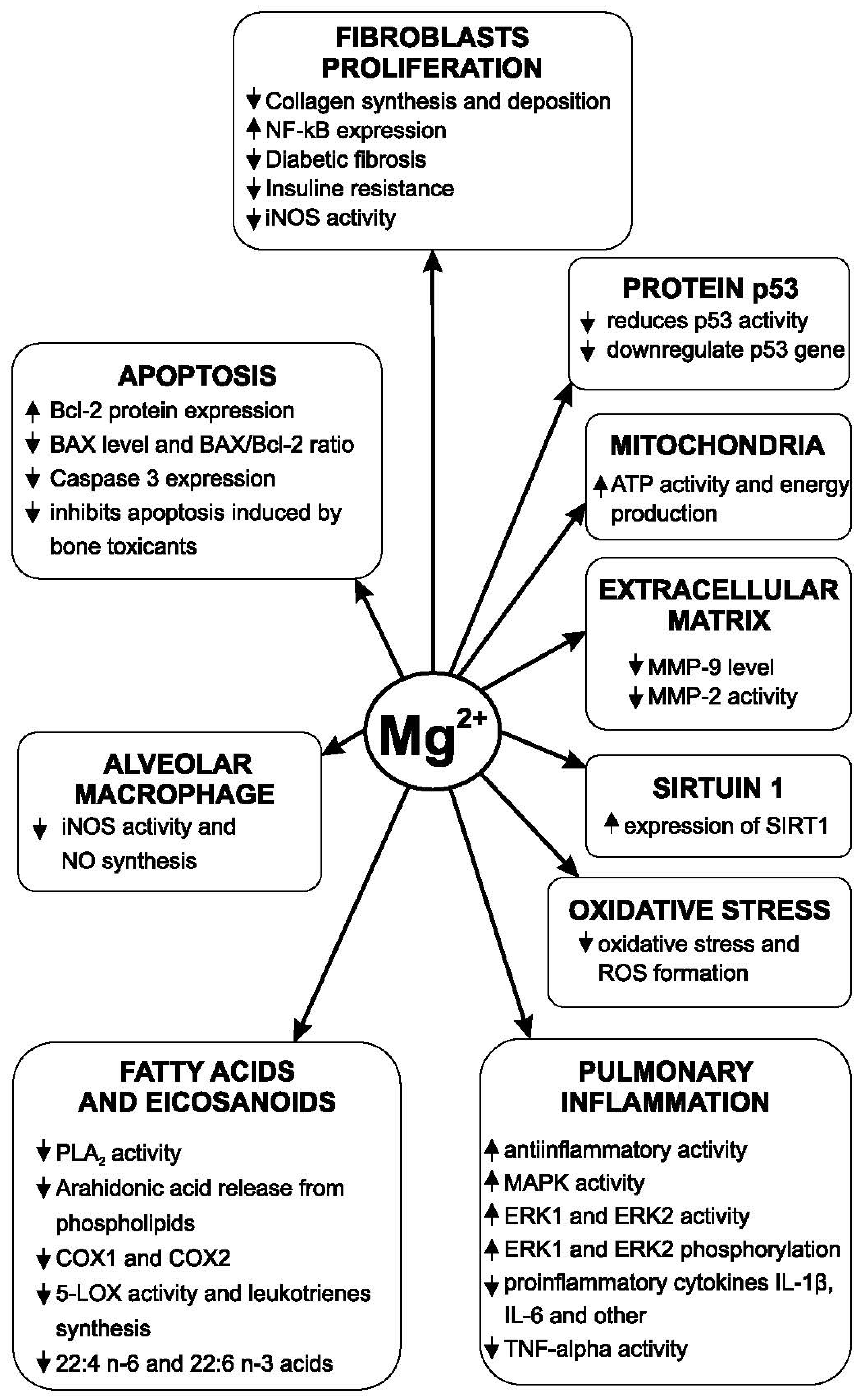
| Oxidative stress | In animal studies, Mg2+ significantly reduced oxidative stress and lung lesions associated with it [39]. Mg2+ inhibits nuclear factor-kappaB (NF-κB) activity [40,41] |
| Inflammation | Magnesium isoglycyrrhizinate (MgIG) reduces the formation of pro-inflammatory factors determined by LPS [51]. MgIG significantly reduced the concentration of IL-6 and TNF-α at the lung and serum levels in rats [58]. Low magnesium concentration causes an increase in the expression of p38-mitogen-activated protein kinase (MAPK) [60] Magnesium citrate 300 mg/day in patients with COPD significantly reduced the level of CRP [73]. Magnesium in cell culture increased the activity of MAPK, ERK 1 and ERK 2 [69]. In a double-blinded, placebo-controlled trial, administration of 250 mg/day magnesium oxide for 6 weeks downregulated gene expression levels of interleukin-8 (c) and TNF-α [61]. |
| Mitochondrial dysfunctions | Mg2+ is essential for the activity of ATP and the production of energy at the mitochondrial level. |
| Excessive extracellular matrix accumulation | Magnesium isoglycyrrhizinate inhibited the activity of MMP-9 in rats with lung injury [82]. In human cell cultures, magnesium concentrations (0–3.0 mmol/L) significantly reduced the production of MMP2 stimulated by homocysteine [83] |
| Fibroblasts and myofibroblasts differentiation and fibrosis | Mg-deficient diet in rats induced a19% increase in collagen synthesis and deposition [96]. MgIG reduced the pulmonary concentration of TGF-1 beta in radiation-induced experimental pulmonary fibrosis and decreased fibrosis progression [99]. Magnesium lithospermate B (50 mg/kg/day for 7 days), in animal studies, had an antifibrotic effect [100]. Magnesium inhibits the differentiation of pulmonary fibroblasts by influencing the MAPK/Akt/Nox4 biological signal transduction pathway [116]. |
| Alveolar macrophage | The decrease in magnesium concentration in the culture medium of the alveolar macrophages determines the increase in the synthesis of nitric oxide through the stimulation of iNOS [130] |
| Alveolar epithelial cells | Magnesium hydride (MgH2) diminishes LPS induced inflammatory reaction, apoptosis, and barrier breakdown in alveolar epithelial cells [100] MgH2 also suppressed barrier breakdown by upregulating the expression of occludin [150]. |
| Some active endogenous substances involved in IPF pathogeny | MgIG inhibits PLA2 and suppresses the stimulation of this enzyme by lipopolysaccharide (LPS). MgIG compound inhibits Cyclooxygenase 1 (COX1) and Cyclooxygenase 2 (COX2) (the main enzymes in the synthesis of pro-inflammatory eicosanoids) [70,172]. In clinical studies, administration of magnesium (300 mg/day magnesium sulfate) for 3 months led to downregulation of p53 gene [189]. Magnesium lithospermate B (25–50 mg/kg/day) in experimental studies in rats increased the expression of SIRT1 [194] |
| Apoptosis | Mg2+ reduced the Bax level (which increases in hypoxia conditions) and normalized the Bax/Bcl ratio [199]. MgIG also inhibited apoptosis increased by some toxicants [200]. |
| Zn2+ and Cu2+ Actions | |
|---|---|
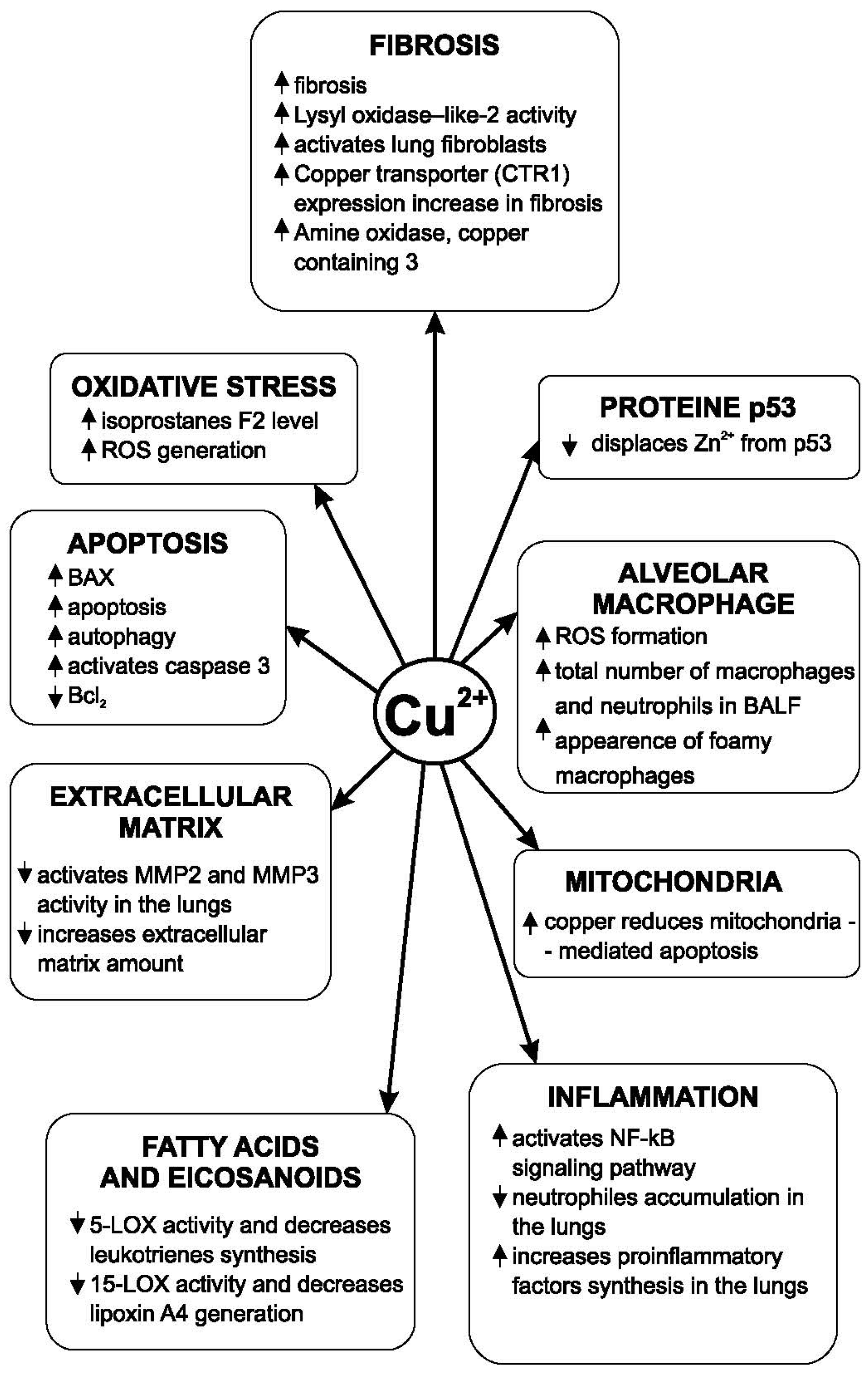
| Oxidative stress | Zinc deficiency exacerbates oxidative stress in the lungs, increases the production of ROS and decreases the reduction in the expression of Nrf2 [38]. Zinc increases the level of GSH [45]. Zinc aspartate in acute lung injury significantly reduces the pulmonary level of malondialdehyde (MDA), nitric oxide, and myeloperoxidase [46]. Zinc sulfate in the case of lung injury produced an increase in SOD levels and alleviated lung injury [49]. The copper(II) catalyzed GSH oxidation [51]. The increase in Cu concentration in the lungs is associated with increased oxidative stress in patients with cystic fibrosis [50]. |
| Inflammation | Zinc has anti-inflammatory actions [55]. Zinc alleviates inflammation induced by lipopolysaccharide (LPS) and other pro-inflammatory factors [56]. The main way through which zinc regulates biological signal transduction mediated by ERK1/2 is the inhibition of phosphatases that determine the dephosphorylation of ERK1 and ERK2 [72]. In animal studies, copper in drinking water for 16 weeks showed an increase in oxidative stress and pro-inflammatory factors at the lung level, simultaneously with an intensification of copper accumulation in the lungs [75]. A copper/zinc ratio higher than normal has a pro-inflammatory action [76]. |
| Mitochondrial dysfunctions | Copper concentrations higher than normal it causes mitochondrial dysfunction. Copper induces an increased mitochondrial deposition of lipids [79]. Copper produces swelling and decreases the mitochondrial membrane potential [80]. |
| Excessive extracellular matrix accumulation | In human clinic, serum zinc levels are negatively correlated with the concentration of MMP-2, MMP-9 [84]. In animal studies, the addition of zinc to the normal diet or to the high-fat diet significantly reduced MMP2 and MMP9’s expressions [85]. Copper-methionine administration in cold-stressed broilers decreased the concentration of MMP-2 [87]. |
| Fibroblasts and myofibroblasts differentiation and fibrosis | Zinc in drinking water reduced collagen accumulation in the lungs of animals experimentally intoxicated with CCl4 by the inhibition of the lung prolyl hydroxylase activity [101]. In animal studies, zinc reduced the deposition of collagen in the lungs [102]. A copper-dependent monoamine oxidase is also involved in the development of fibrosis in various organs [104]. The main mechanism of action of intracellular copper ions is the activation of LOXL(lysyl oxidase-like) [105]. LOXL is an essential enzyme in collagen synthesis and the formation of the extracellular matrix. Amine oxidase copper-containing-3 (AOC3) is an enzyme with a role in the development of pulmonary fibrosis [110]. Exposure to CuSO4 (100 μM concentration) in vitro produces a decrease in the viability of both alveolar cells and bronchoepithelial cells [113]. Copper also increases the autophagy [79] and inhibits the acetylcholinesterase [115]. |
| Alveolar macrophage | Zinc deficiency increased the macrophage infiltration [56]. Exposure of alveolar macrophages to copper oxide increases the generation of ROS in these cells [97]. The copper transporter ATP7A was identified in macrophages [134]. Exposure of animals to CuSO4 in air produces an increase in the plasma concentration of isoprostane F2 and an increase in the total number of neutrophils and macrophages in BALF [135]. |
| Alveolar epithelial cells | Deficiency of a zinc transporter, SLC39A8 (ZIP8), has been identified in AEC2s in patients with IPF [151]. In AECs, copper oxide increases oxidative stress and produces morphological changes. Copper oxide induces mitochondrial damage [152]. |
| Some active endogenous substances involved in IPF pathogeny | Zinc in micromolar concentrations inhibited the activity of 15-lipoxygenase, the essential enzyme in the synthesis of lipoxins, in human polymorphonuclear leukocytes [163]. Ratio between the concentrations of zinc and copper also influences the unsaturated fatty acid composition of the phospholipids of cell membranes [165]. Zinc inhibited the stimulation of PLA2 and the release of arachidonic acid [174]. AECII captures zinc through a process that is stimulated by arachidonic acid [182] CuSO4·5H2O inhibited both the activity of 5-lipooxygenase (5-LOX) and that of 15-LOX, i.e., the synthesis of leukotrienes and lipoxins [177]. CuSO4 and other copper compounds inhibit the lipoxygenases that catalyze the hydroperoxidation of polyunsaturated fatty acids [177]. Cu2+ displaces Zn2+ from p53 protein [191]. Zinc activates the sirtuin signaling pathway [195]. By activating SIRT 1, zinc reduces NF-kB activity [196]. |
| Apoptosis | Increasing intracellular copper concentration induces apoptosis and enhances autophagy [205,206]. Copper activates the caspase pathway. It is an important mechanism by which copper induces apoptosis [208]. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Published by MDPI on behalf of the Lithuanian University of Health Sciences. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license.
Share and Cite
Nechifor, M.; Zamfir, C.L.; Gales, C. Magnesium, Zinc and Copper in Lung Fibrosis: A Narrative Review. Medicina 2026, 62, 10. https://doi.org/10.3390/medicina62010010
Nechifor M, Zamfir CL, Gales C. Magnesium, Zinc and Copper in Lung Fibrosis: A Narrative Review. Medicina. 2026; 62(1):10. https://doi.org/10.3390/medicina62010010
Chicago/Turabian StyleNechifor, Mihai, Carmen Lacramioara Zamfir, and Cristina Gales. 2026. "Magnesium, Zinc and Copper in Lung Fibrosis: A Narrative Review" Medicina 62, no. 1: 10. https://doi.org/10.3390/medicina62010010
APA StyleNechifor, M., Zamfir, C. L., & Gales, C. (2026). Magnesium, Zinc and Copper in Lung Fibrosis: A Narrative Review. Medicina, 62(1), 10. https://doi.org/10.3390/medicina62010010






