Artificial Intelligence and Advanced Digital Health for Hypertension: Evolving Tools for Precision Cardiovascular Care
Abstract
1. Introduction
2. Methods
2.1. Databases and Search Strategy
2.2. Eligibility Criteria
2.3. Synthesis Approach
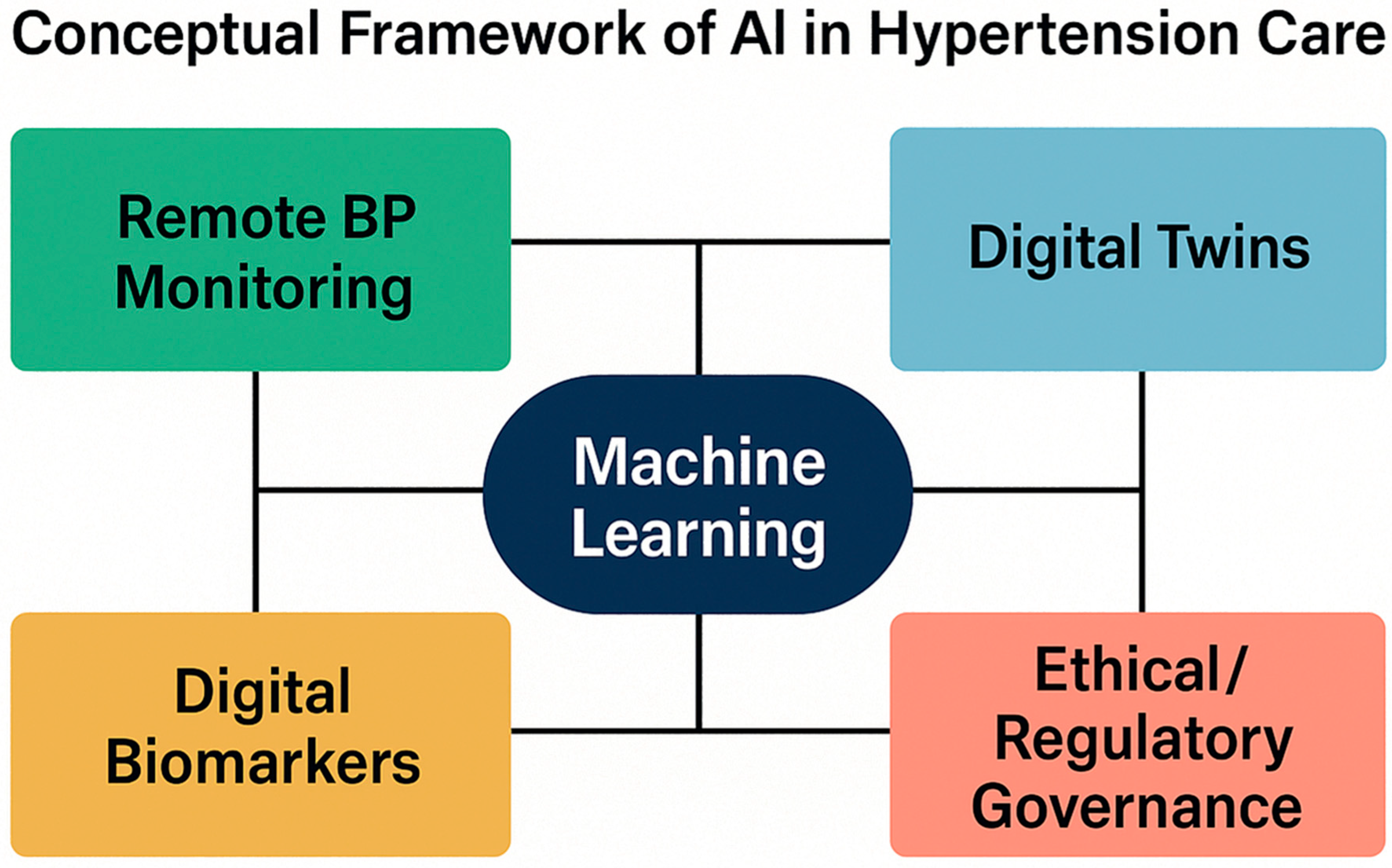
3. AI-Guided Remote Blood Pressure Titration
4. Digital Twin Technologies in Hypertension: Concept and Applications
5. Digital Biomarkers and Remote Blood Pressure Monitoring in Hypertension
6. Clinical Applications and Outcomes of AI-Driven Hypertension Management
7. Implementation, Ethical Governance, and Future Directions in AI-Driven Hypertension Management
8. Limitations and Strengths
9. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| AI | Artificial Intelligence |
| BP | Blood Pressure |
| CDSS | Clinical Decision Support System |
| HBPM | Home Blood Pressure Monitoring |
| LLM | Large Language Model |
| RCT | Randomized Controlled Trial |
References
- GBD 2021 Risk Factors Collaborators. Global burden of 87 risk factors in 204 countries and territories, 1990–2021: A systematic analysis for the Global Burden of Disease Study 2019. Lancet 2020, 396, 1223–1249. [Google Scholar] [CrossRef]
- NCD Risk Factor Collaboration (NCD-RisC). Worldwide trends in hypertension prevalence and progress in treatment and control from 1990 to 2019: A pooled analysis of 1201 population-representative studies with 104 million participants. Lancet 2021, 398, 957–980. [Google Scholar] [CrossRef]
- Whelton, P.K.; Carey, R.M. The 2017 Clinical Practice Guidelines for hypertension: What is new and what do we do? Curr. Cardiol. Rep. 2018, 41, 279–281. [Google Scholar]
- Chow, C.K.; Redfern, J.; Hillis, G.S.; Thakkar, J. A digital health intervention to increase medication adherence in patients with cardiovascular disease: A randomized controlled trial. Eur. Heart J. 2022, 43, 567–575. [Google Scholar]
- Omboni, S.; McManus, R.J.; Bosworth, H.B.; Chappell, L.C.; Green, B.B.; Kario, K.; Logan, A.G.; Magid, D.J.; Mckinstry, B.; Margolis, K.L.; et al. Evidence and recommendations on the use of telemedicine for the management of arterial hypertension. Hypertension 2020, 76, 1368–1383. [Google Scholar] [CrossRef] [PubMed]
- Skalidis, I.; Muller, O.; Fournier, S. CardioVerse: The cardiovascular medicine in the era of Metaverse. Trends Cardiovasc. Med. 2023, 33, 471–476. [Google Scholar] [CrossRef]
- Skalidis, I.; Lu, H.; Maurizi, N.; Fournier, S.; Tsigkas, G.; Apostolos, A.; Cook, S.; Iglesias, J.F.; Garot, P.; Hovasse, T.; et al. Mobile Health Applications for Secondary Prevention After Myocardial Infarction or PCI: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Healthcare 2025, 13, 1881. [Google Scholar] [CrossRef] [PubMed]
- Morawski, K.; Ghazinouri, R.; Krumme, A.; Lauffenburger, J.C.; Lu, Z.; Zhang, F.; Durfee, E.; Oley, L.; Lee, J.; Mohta, N.; et al. Association of a smartphone application with medication adherence and blood pressure control: The MedISAFE-BP randomized clinical trial. JAMA Int. Med. 2018, 178, 802–809. [Google Scholar] [CrossRef]
- Skalidis, I.; Kachrimanidis, I.; Koliastasis, L.; Arangalage, D.; Antiochos, P.; Maurizi, N.; Muller, O.; Fournier, S.; Hamilos, M.; Skalidis, E. Cardiology in the digital era: From artificial intelligence to Metaverse, paving the way for future advancements. Future Cardiol. 2023, 19, 755–758. [Google Scholar] [CrossRef]
- Corral-Acero, J.; Margara, F.; Marciniak, M.; Rodero, C.; Loncaric, F.; Feng, Y.; Gilbert, A.; Fernandes, J.F.; Bukhari, H.A.; Wajdan, A.; et al. The ‘Digital Twin’ to enable the vision of precision cardiology. Eur. Heart J. 2020, 41, 4556–4564. [Google Scholar] [CrossRef]
- Niederer, S.A.; Lumens, J.; Trayanova, N.A. Computational models in cardiology. Nat. Rev. Cardiol. 2019, 16, 100–111. [Google Scholar] [CrossRef]
- McManus, R.J.; Mant, J.; Haque, M.S.; Bray, E.P.; Bryan, S.; Greenfield, S.M.; Jones, M.I.; Jowett, S.; Little, P.; Penaloza, C.; et al. Effect of self-monitoring and medication self-titration on systolic blood pressure in hypertensive patients at high risk of cardiovascular disease: The TASMIN-SR randomized clinical trial. JAMA 2014, 312, 799–808. [Google Scholar] [CrossRef]
- Truong, A.T.L.; Tan, S.B.; Wang, G.Z.; Yip, A.W.J.; Egermark, M.; Yeung, W.; Lee, V.V.; Chan, M.Y.; Kumar, K.S.; Tan, L.W.J.; et al. CURATE.AI-assisted dose titration for anti-hypertensive personalized therapy: Study protocol for a multi-arm, randomized, pilot feasibility trial using CURATE.AI (CURATE.AI ADAPT trial). Eur. Heart J. Digit. Health 2023, 5, 41–49. [Google Scholar] [CrossRef] [PubMed]
- McEvoy, J.W.; McCarthy, C.P.; Bruno, R.M.; Brouwers, S.; Canavan, M.D.; Ceconi, C.; Christodorescu, R.M.; Daskalopoulou, S.S.; Ferro, C.J.; Gerdts, E.; et al. ESCScientific Document Group 2024 ESCGuidelines for the management of elevated blood pressure hypertension. Eur. Heart J. 2024, 45, 3912–4018. [Google Scholar] [CrossRef]
- Kreutz, R.; Brunström, M.; Burnier, M.; Grassi, G.; Januszewicz, A.; Muiesan, M.L.; Tsioufis, K.; de Pinho, R.M.; Albini, F.L.; Boivin, J.M.; et al. 2024 European Society of Hypertension clinical practice guidelines for the management of arterial hypertension. Eur. J. Int. Med. 2024, 126, 1–15. [Google Scholar] [CrossRef]
- Ye, C.; Fu, T.; Hao, S.; Zhang, Y.; Wang, O.; Jin, B.; Xia, M.; Liu, M.; Zhou, X.; Wu, Q.; et al. Prediction of incident hypertension within the next year: Prospective study using statewide electronic health records and machine learning. J. Med. Int. Res. 2018, 20, e22. [Google Scholar] [CrossRef] [PubMed]
- Gu, F.; Meyer, A.J.; Ježek, F.; Zhang, S.; Catalan, T.; Miller, A.; Schenk, N.A.; Sturgess, V.E.; Uceda, D.; Li, R.; et al. Identification of digital twins to guide interpretable AI for diagnosis and prognosis in heart failure. npj Digit. Med. 2025, 8, 110. [Google Scholar] [CrossRef] [PubMed]
- Coorey, G.; Figtree, G.A.; Fletcher, D.F.; Snelson, V.J.; Vernon, S.T.; Winlaw, D.; Grieve, S.M.; McEwan, A.; Yang, J.Y.H.; Qian, P.; et al. The health digital twin to tackle cardiovascular disease-a review of an emerging interdisciplinary field. npj Digit. Med. 2022, 5, 126. [Google Scholar] [CrossRef]
- Sel, K.; Osman, D.; Zare, F.; Masoumi Shahrbabak, S.; Brattain, L.; Hahn, J.O.; Inan, O.T.; Mukkamala, R.; Palmer, J.; Paydarfar, D.; et al. Building Digital Twins for Cardiovascular Health: From Principles to Clinical Impact. J. Am. Heart Assoc. 2024, 13, e031981. [Google Scholar] [CrossRef]
- Naik, A.; Nalepa, J.; Wijata, A.M.; Mahon, J.; Mistry, D.; Knowles, A.T.; Dawson, E.A.; Lip, G.Y.H.; Olier, I.; Ortega-Martorell, S. Artificial intelligence and digital twins for the personalised prediction of hypertension risk. Comput. Biol. Med. 2025, 196, 110718. [Google Scholar] [CrossRef]
- Islam, S.M.S.; Chow, C.K.; Daryabeygikhotbehsara, R.; Subedi, N.; Rawstorn, J.; Tegegne, T.; Karmakar, C.; Siddiqui, M.U.; Lambert, G.; Maddison, R. Wearable cuffless blood pressure monitoring devices: A systematic review and meta-analysis. Eur. Heart J. Digit. Health 2022, 3, 323–337. [Google Scholar] [CrossRef] [PubMed]
- Al-Alusi, M.A.; Friedman, S.F.; Kany, S.; Rämö, J.T.; Pipilas, D.; Singh, P.; Reeder, C.; Khurshid, S.; Pirruccello, J.P.; Maddah, M.; et al. A deep learning digital biomarker to detect hypertension and stratify cardiovascular risk from the electrocardiogram. npj Digit. Med. 2025, 8, 120. [Google Scholar] [CrossRef]
- Coravos, A.; Goldsack, J.C.; Karlin, D.R.; Nebeker, C.; Perakslis, E.; Zimmerman, N.; Erb, M.K. Digital Medicine: A Primer on Measurement. Digit. Biomark. 2019, 3, 31–71. [Google Scholar] [CrossRef]
- Kario, K.; Nomura, A.; Harada, N.; Okura, A.; Nakagawa, K.; Tanigawa, T.; Hida, E. Efficacy of a digital therapeutics system in the management of essential hypertension: The HERB-DH1 pivotal trial. Eur. Heart J. 2021, 42, 4111–4122. [Google Scholar] [CrossRef]
- Meyer, B.; Riepenhausen, A.; Betz, L.T.; Jauch-Chara, K.; Reshetnik, A. Internet-based digital intervention to support the self-management of hypertension compared to usual care: Results of the HALCYON randomized controlled trial. BMC Cardiovasc. Disord. 2025, 25, 256. [Google Scholar] [CrossRef]
- Bhatt, B.J.; Amir, H.M.; Jones, S.; Jamieson, A.; Chaturvedi, N.; Hughes, A.; Orini, M. Validation of a popular consumer-grade cuffless blood pressure device for continuous 24 h monitoring. Eur. Heart. J. Digit. Health 2025, 6, 704–712. [Google Scholar] [CrossRef]
- Derendinger, F.C.; Vischer, A.S.; Krisai, P.; Socrates, T.; Schumacher, C.; Mayr, M.; Burkard, T. Ability of a 24-h ambulatory cuffless blood pressure monitoring device to track blood pressure changes in clinical practice. J. Hypertens. 2024, 42, 662–671. [Google Scholar] [CrossRef]
- Stergiou, G.S.; Avolio, A.P.; Palatini, P.; Kyriakoulis, K.G.; Schutte, A.E.; Mieke, S.; Kollias, A.; Parati, G.; Asmar, R.; Pantazis, N.; et al. European Society of Hypertension recommendations for the validation of cuffless blood pressure measuring devices: European Society of Hypertension Working Group on Blood Pressure Monitoring and Cardiovascular Variability. J. Hypertens. 2023, 41, 2074–2087. [Google Scholar] [CrossRef]
- Hicks, L.S.; Sequist, T.D.; Ayanian, J.Z.; Shaykevich, S.; Fairchild, D.G.; Orav, E.J.; Bates, D.W. Impact of computerized decision support on blood pressure management and control: A randomized controlled trial. J. Gen. Int. Med. 2008, 23, 429-41. [Google Scholar] [CrossRef] [PubMed]
- Leitner, J.; Chiang, P.H.; Agnihotri, P.; Dey, S. The Effect of an AI-Based, Autonomous, Digital Health Intervention Using Precise Lifestyle Guidance on Blood Pressure in Adults With Hypertension: Single-Arm Nonrandomized Trial. JMIR Cardiol. 2024, 8, e51916. [Google Scholar] [CrossRef] [PubMed]
- Garcia, P.; Ma, S.P.; Shah, S.; Smith, M.; Jeong, Y.; Devon-Sand, A.; Tai-Seale, M.; Takazawa, K.; Clutter, D.; Vogt, K.; et al. Artificial Intelligence-Generated Draft Replies to Patient Inbox Messages. JAMA Netw. Open. 2024, 7, e243201. [Google Scholar] [CrossRef]
- Kaboudi, N.; Firouzbakht, S.; Eftekhar, M.S.; Fayazbakhsh, F.; Joharivarnoosfaderani, N.; Ghaderi, S.; Dehdashti, M.; Kia, Y.M.; Afshari, M.; Vasaghi-Gharamaleki, M.; et al. Diagnostic Accuracy of ChatGPT for Patients’ Triage; a Systematic Review and Meta-Analysis. Arch. Acad. Emerg. Med. 2024, 12, e60. [Google Scholar]
- Nascimento, I.J.B.D.; Abdulazeem, H.; Vasanthan, L.T.; Martinez, E.Z.; Zucoloto, M.L.; Østengaard, L.; Azzopardi-Muscat, N.; Zapata, T.; Novillo-Ortiz, D. Barriers and facilitators to utilizing digital health technologies by healthcare professionals: A systematic thematic review of reviews. npj Digit. Med. 2023, 6, 161. [Google Scholar] [CrossRef] [PubMed]
- Katz, M.E.; Mszar, R.; Grimshaw, A.A.; Gunderson, C.G.; Onuma, O.K.; Lu, Y.; Spatz, E.S. Digital Health Interventions for Hypertension Management in US Populations Experiencing Health Disparities: A Systematic Review and Meta-Analysis. JAMA Netw. Open. 2024, 7, e2356070. [Google Scholar] [CrossRef] [PubMed]
- Sadeghi, Z.; Alizadehsani, R.; Cifci, M.A.; Kausar, S.; Rehman, R.; Mahanta, P.; Bora, P.K.; Almasri, A.; Alkhawaldeh, R.S.; Hussain, S.; et al. A review of Explainable Artificial Intelligence in healthcare. Comput. Biol. Med. 2024, 118, 109370. [Google Scholar] [CrossRef]
- Panch, T.; Mattie, H.; Atun, R. Artificial intelligence and algorithmic bias: Implications for health systems. J. Glob. Health 2019, 9, 010318. [Google Scholar] [CrossRef]
- Vayena, E.; Blasimme, A.; Cohen, I.G. Machine learning in medicine: Addressing ethical challenges. PLoS Med. 2018, 15, e1002689. [Google Scholar] [CrossRef]
- US Food and Drug Administration. Proposed Regulatory Framework for Modifications to Artificial Intelligence/Machine Learning-Based Software as a Medical Device; US Food and Drug Administration: Silver Spring, MD, USA, 2019.
- Attia, Z.I.; Kapa, S.; Lopez-Jimenez, F.; McKie, P.M.; Ladewig, D.J.; Satam, G.; Pellikka, P.A.; Enriquez-Sarano, M.; Noseworthy, P.A.; Munger, T.M.; et al. Screening for cardiac contractile dysfunction using an artificial intelligence-enabled electrocardiogram. Nat. Med. 2019, 25, 70–74. [Google Scholar] [CrossRef]
- Gill, S.K.; Karwath, A.; Uh, H.W.; Cardoso, V.R.; Gu, Z.; Barsky, A.; Slater, L.; Acharjee, A.; Duan, J.; Dall’Olio, L.; et al. BigData@Heart Consortium the cardAIc group Artificial intelligence to enhance clinical value across the spectrum of cardiovascular healthcare. Eur. Heart J. 2023, 44, 713–725. [Google Scholar] [CrossRef]
- Cersosimo, A.; Zito, E.; Pierucci, N.; Matteucci, A.; La Fazia, V.M. A Talk with ChatGPT: The Role of Artificial Intelligence in Shaping the Future of Cardiology and Electrophysiology. J. Pers. Med. 2025, 15, 205. [Google Scholar] [CrossRef] [PubMed]
- Skalidis, I.; Fournier, S.; Skalidis, E.; Maurizi, N. Virtual hospitals and digital doctors: How far are we from the CardioVerse? Eur. Heart J. 2022, 44, 7–9. [Google Scholar] [CrossRef]
- Abdalla, M.; Bolen, S.D.; Brettler, J.; Egan, B.M.; Ferdinand, K.C.; Ford, C.D.; Lackland, D.T.; Wall, H.K.; Shimbo, D.; American Heart Association and American Medical Association. Implementation Strategies to Improve Blood Pressure Control in the United States: A Scientific Statement from the American Heart Association and American Medical Association. Hypertension 2023, 80, e143–e157. [Google Scholar] [CrossRef]
- Monahan, M.; Jowett, S.; Nickless, A.; Franssen, M.; Grant, S.; Greenfield, S.; Hobbs, F.D.R.; Hodgkinson, J.; Mant, J.; McManus, R.J. Cost-Effectiveness of Telemonitoring and Self-Monitoring of Blood Pressure for Antihypertensive Titration in Primary Care (TASMINH4). Hypertension 2019, 73, 1231–1239. [Google Scholar] [CrossRef] [PubMed]
- Hayek, M.A.; Giannouchos, T.; Lawley, M.; Kum, H.C. Economic Evaluation of Blood Pressure Monitoring Techniques in Patients with Hypertension: A Systematic Review. JAMA Netw. Open. 2023, 6, e2344372. [Google Scholar] [CrossRef] [PubMed]
- Nomura, A.; Tanigawa, T.; Kario, K.; Igarashi, A. Cost-effectiveness of digital therapeutics for essential hypertension. Hypertens. Res. 2022, 45, 1538–1548. [Google Scholar] [CrossRef] [PubMed]

| Technology | Function | Example Applications | Clinical Outcomes | Level of Evidence |
|---|---|---|---|---|
| Remote BP Monitoring | Continuous or home-based BP tracking | Smartphone apps with Bluetooth cuffs | Improved BP control, enhanced adherence | RCTs, meta-analyses |
| Machine Learning Algorithms | Risk prediction, medication titration | ML models predicting uncontrolled BP or optimizing drug regimens | Increased treatment intensification, reduced variability | Observational + pilot RCTs |
| Digital Twins | Personalized simulations of BP response | Virtual BP phenotype to simulate therapy effects | Theoretical benefit; limited clinical validation | Conceptual/early clinical |
| Explainable AI (XAI) | Transparent decision support | Visual explanations for BP prediction models | Enhanced clinician trust, interpretability | Preclinical and pilot trials |
| Federated Learning | Multi-center model training without data sharing | Cross-hospital AI models for BP titration | Maintains privacy, supports scalability | Early implementation studies |
| Study (First Author, Year) | Intervention | Comparator | Population | BP Reduction (mmHg) | Duration | Key Findings |
|---|---|---|---|---|---|---|
| Chow et al., 2022 [4] | SMS-based reminders | Control | Latin America | −2.2 systolic | 1 year | Modest benefit |
| Omboni et al., 2020 [5] | Team-based digital titration | Office BP follow-up | US primary care | −7.0 systolic | 6 months | Increased treatment intensification |
| Morawski et al., 2018 [8] | Smartphone BP app | Standard care | Chinese adults with hypertension | −5.3 systolic | 12 months | Enhanced self-management |
| Katz et al., 2024 [34] | Tailored mHealth + CHW | Usual care | Underserved US adults | −4.1 systolic | 6 months | Improved equity and control |
| Domain | Barrier | Enabler | Source |
|---|---|---|---|
| Infrastructure | Lack of EHR integration | Interoperable platforms | Nascimento et al., NPJ Digit Med 2023 [33] |
| Clinician Engagement | Low trust in black-box models | Explainable AI frameworks | Sadeghi et al., Comput Biol Med 2024 [35] |
| Equity | Digital literacy gaps, device access | Tailored interfaces, CHW support | Katz et al., JAMA Netw Open 2024 [34] |
| Regulation | Dynamic algorithms hard to audit | FDA SaMD framework, EU AI Act | US FDA 2019; Stergiou et al., J Hypertens 2023 [28,38] |
| Data Privacy | Sharing concerns across institutions | Federated learning architecture | Nascimento et al., NPJ Digit Med 2023 [33] |
| Priority Area | Proposed Direction | Rationale |
|---|---|---|
| Prospective RCTs | Evaluate AI + remote BP tools in diverse settings | Clinical validation, generalizability |
| Health Economic Studies | Assess cost-effectiveness of digital hypertension tools | Reimbursement, policy alignment |
| Implementation Science | Study uptake in low-resource settings | Address global disparities |
| Co-design Strategies | Involve clinicians, patients in model development | Improve trust, usability |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Published by MDPI on behalf of the Lithuanian University of Health Sciences. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Skalidis, I.; Maurizi, N.; Salihu, A.; Fournier, S.; Cook, S.; Iglesias, J.F.; Laforgia, P.; D’Angelo, L.; Garot, P.; Hovasse, T.; et al. Artificial Intelligence and Advanced Digital Health for Hypertension: Evolving Tools for Precision Cardiovascular Care. Medicina 2025, 61, 1597. https://doi.org/10.3390/medicina61091597
Skalidis I, Maurizi N, Salihu A, Fournier S, Cook S, Iglesias JF, Laforgia P, D’Angelo L, Garot P, Hovasse T, et al. Artificial Intelligence and Advanced Digital Health for Hypertension: Evolving Tools for Precision Cardiovascular Care. Medicina. 2025; 61(9):1597. https://doi.org/10.3390/medicina61091597
Chicago/Turabian StyleSkalidis, Ioannis, Niccolo Maurizi, Adil Salihu, Stephane Fournier, Stephane Cook, Juan F. Iglesias, Pietro Laforgia, Livio D’Angelo, Philippe Garot, Thomas Hovasse, and et al. 2025. "Artificial Intelligence and Advanced Digital Health for Hypertension: Evolving Tools for Precision Cardiovascular Care" Medicina 61, no. 9: 1597. https://doi.org/10.3390/medicina61091597
APA StyleSkalidis, I., Maurizi, N., Salihu, A., Fournier, S., Cook, S., Iglesias, J. F., Laforgia, P., D’Angelo, L., Garot, P., Hovasse, T., Neylon, A., Unterseeh, T., Champagne, S., Amabile, N., Sayah, N., Sanguineti, F., Akodad, M., Lu, H., & Antiochos, P. (2025). Artificial Intelligence and Advanced Digital Health for Hypertension: Evolving Tools for Precision Cardiovascular Care. Medicina, 61(9), 1597. https://doi.org/10.3390/medicina61091597






