Improving the Mental Health of Nursing Staff Seen from the Perspective of Staff a Preliminary Study
Abstract
1. Introduction
- What are the main challenges that have affected the mental health of nurses in Albania after the COVID-19 pandemic?
- What are the most common ways of coping with stress used by nurses in Albania?
- What are the suggestions and recommendations of nurses in Albania themselves for improving mental health in the workplace?
2. Materials and Methods
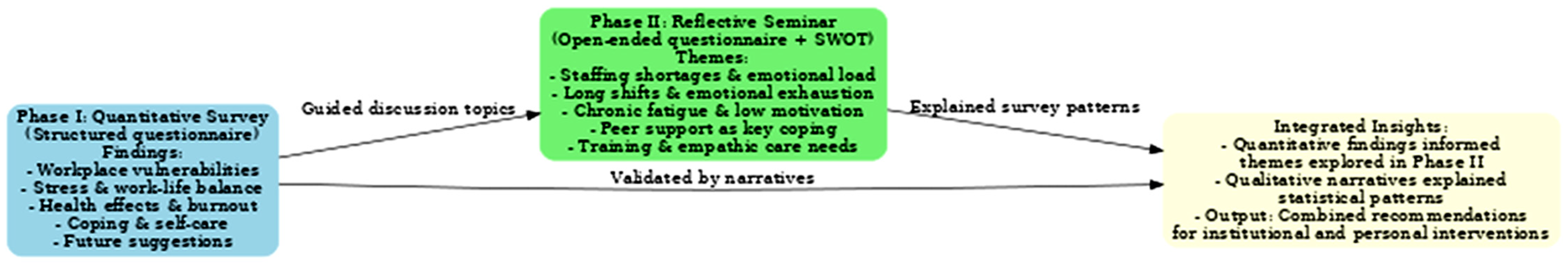
2.1. Study Design
2.2. Study Settings
2.3. Study Sample
- Direct pandemic care experience—nurses had been directly involved in patient care during the COVID-19 pandemic.
- Willingness to engage—expressed readiness to participate in reflective discussions on post-pandemic challenges.
- Significant challenges—had reported substantial professional or psychological challenges in Phase I.
2.4. Data Sources/Measurement
2.4.1. Data Sources During the First Phase
- Vulnerabilities in the workplace.
- Stress and work–life balance.
- Health effects and burnout.
- Coping mechanisms and self-care.
- Views and suggestions for the future.
2.4.2. Data Sources During the Second Phase
- What challenges most affected your mental health after the pandemic?
- What coping mechanisms or strategies helped you the most?
- What support did you expect from the institution but did not receive?
- What concrete recommendations do you have to improve mental well-being?
- What training or programs would be helpful for you?
2.4.3. Questionnaire Distribution and Data Collection
2.4.4. Pilot Study
2.5. Data Collection and Analysis
- A pre- and post-intervention reflective questionnaire with prompts (e.g., main challenges, coping strategies, gaps in institutional support, suggestions for improvement).
- An institutional program evaluation form assessing the availability of 12 potential support interventions.
2.5.1. Measured Variables
- Challenges and difficulties in the workplace—four items (e.g., staff shortages, overload and constant pressure, insufficient communication and support).
- Impact of work on personal life and work–life balance—three items (e.g., continuous stress, deterioration in work–life balance, and need for flexible work policies).
- Effect on physical and mental health—three items (e.g., burnout, insufficient psychological support, and need for workplace wellness programs).
- Coping strategies and self-care—three items (e.g., physical activity and recreation, support from colleagues, and health maintenance through leisure policies).
- Suggestions and improving working conditions and institutional support— three items (improving working conditions, investment in professional training, development of psychological support policies).
- ▪ Key post-pandemic challenges;
- ▪ Effective individual coping strategies;
- ▪ Perceived gaps in institutional support;
- ▪ Concrete suggestions for improvement.
2.5.2. Statistical Methods
- A structured open-ended reflection questionnaire;
- A program evaluation form assessing institutional support and provided training;
- A SWOT analysis worksheet.
2.6. Ethical Considerations
3. Results
3.1. Phase I. Challenges Faced by Nurses After the Pandemic—Coping Mechanisms and Suggestions for the Future
3.2. Phase II. Reflective Training Seminar and Qualitative Analysis
- Group-based reflective seminar activities using a structured open-ended questionnaire, program evaluation form, and SWOT analysis worksheet.
- A pre- and post-seminar closed-ended questionnaire to measure short-term changes in knowledge and awareness.
Interpretation of SWOT Analysis Results
- Understanding of the impacts on mental health (from 27.7% to 70.2% after);
- Identification of practical solutions (from 31.9% to 76.6%);
- Awareness of coping strategies (from 25.5% to 42.6% and from 23.4% to 46.8% for the two related items);
- Recognition of importance of work–life balance (from 27.7% to 53.2%).
4. Discussion
Limitations of the Study
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| COVID-19 | Corona virus Disease 2019 |
| SWOT | Strengths, Weaknesses, Opportunities, Threats |
References
- Hu, D.; Kong, Y.; Li, W.; Han, Q.; Zhang, X.; Zhu, L.X.; Wan, S.W.; Liu, Z.; Shen, Q.; Yang, J.; et al. Frontline nurses’ burnout, anxiety, depression, and fear statuses and their associated factors during the COVID-19 outbreak in Wuhan, China: A large-scale cross-sectional study. eClinicalMedicine 2022, 24, 100424. [Google Scholar] [CrossRef] [PubMed]
- Galanis, P.; Vraka, I.; Fragkou, D.; Bilali, A.; Kaitelidou, D. Nurses’ burnout and associated risk factors during the COVID-19 pandemic: A systematic review and meta-analysis. J. Adv. Nurs. 2021, 77, 3286–3302. [Google Scholar] [CrossRef] [PubMed]
- Villar, R.C.; Nashwan, A.J.; Mathew, R.G.; Mohamed, A.S.; Munirathinam, S.; Abujaber, A.A.; Al-Jabry, M.M.; Shraim, M. The lived experiences of frontline nurses during the coronavirus disease 2019 (COVID-19) pandemic in Qatar: A qualitative study. Nurs. Open 2021, 8, 3516–3526. [Google Scholar] [CrossRef] [PubMed]
- Specht, K.; Primdahl, J.; Jensen, H.I.; Elkjær, M.; Hoffmann, E.; Boye, L.K.; Thude, B.R. Frontline nurses’ experiences of working in a COVID-19 ward—A qualitative study. Nurs. Open 2021, 8, 3006–3015. [Google Scholar] [CrossRef] [PubMed]
- Denning, M.; Goh, E.T.; Tan, B.; Kanneganti, A.; Almonte, M.; Scott, A.; Martin, G.; Clarke, J.; Sounderajah, V.; Markar, S.; et al. Determinants of burnout and other aspects of psychological well-being in healthcare workers during the COVID-19 pandemic: A multinational cross-sectional study. PLoS ONE 2021, 16, e0238666. [Google Scholar] [CrossRef] [PubMed]
- Labrague, L.J.; De los Santos, J.A.A. Fear of COVID-19, Psychological Distress, Work Satisfaction and Turnover Intention among Frontline Nurses. J. Nurs. Manag. 2021, 29, 395–403. [Google Scholar] [CrossRef] [PubMed]
- Kamberi, F. Mental Health Consequences of the COVID-19 Pandemic among Nurses in Albania. Albanian Med. J. 2023, 3, 11–18. [Google Scholar]
- Pollock, A.; Campbell, P.; Cheyne, J.; Cowie, J.; Davis, B.; McCallum, J.; McGill, K.; Elders, A.; Hagen, S.; McClurg, D.; et al. Interventions to Support the Resilience and Mental Health of Frontline Health and Social Care Professionals during and after a Disease Outbreak, Epidemic or Pandemic: A Mixed-Methods Systematic Review. Cochrane Database Syst. Rev. 2020, 11, CD013779. [Google Scholar] [CrossRef] [PubMed]
- Kamberi, F.; Sinaj, E.; Jaho, J.; Subashi, B.; Sinanaj, G.; Jaupaj, K.; Stramarko, Y.; Arapi, P.; Dine, L.; Gurguri, A.; et al. Impact of COVID-19 Pandemic on Mental Health, Risk Perception and Coping Strategies among Health Care Workers in Albania—Evidence That Needs Attention. Clin. Epidemiol. Glob. Health 2021, 12, 100824. [Google Scholar] [CrossRef] [PubMed]
- Pellikka, A.; Junttila, K.; Laukkala, T.; Haapa, T. Nurses’ Perceptions of Desired Support from Their Employer during the COVID-19 Pandemic: A Qualitative Survey Study. BMC Nurs. 2024, 23, 128. [Google Scholar] [CrossRef] [PubMed]
- Luo, Y.; Feng, X.; Wang, D.; Qiao, X.; Xiao, X.; Jia, S.; Zheng, M.; Reinhardt, J.D. Experience of Clinical Nurses Engaged in Caring for Patients with COVID-19: A Qualitative Systematic Review and Meta-Synthesis. J. Clin. Nurs. 2023, 32, 5258–5273. [Google Scholar] [CrossRef] [PubMed]
- Agency for Quality Assurance in Healthcare (ASCK). Calendar of Activities, November 2024. Available online: https://asck.gov.al/kalendari-i-aktiviteteve-nentor-2024/ (accessed on 26 August 2025).
- Greenberg, N.; Docherty, M.; Gnanapragasam, S.; Wessely, S. Managing mental health challenges faced by healthcare workers during COVID-19 pandemic. BMJ 2020, 368, m1211. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization (WHO). Mental Health and COVID-19: Early Evidence of the Pandemic’s Impact. World Health Organization: Geneva, Switzerland, 2022; Available online: https://www.who.int/publications/i/item/WHO-2019-nCoV-Sci_Brief-Mental_health-2022.1 (accessed on 26 August 2025).
- Zarrin, L.; Ghafourifard, M.; Sheikhalipour, Z. Relationship between nurses reflection, self-efficacy, and work engagement. J. Caring Sci. 2023, 12, 155–162. [Google Scholar] [CrossRef]
- Huang, L.; Zhang, X.; Wang, F.; Zhang, S.; Chang, X.; Chu, Y.; Wang, L.; Jia, W.; Zhang, B. Reflection, self-directed learning, and professional identity in nursing. Nurse Educ. Today 2024, 126, 105858. [Google Scholar] [CrossRef]
- Salem, G.M.M.; Hashimi, W.; El-Ashry, A.M. Reflective Mindfulness and Emotional Regulation Training (RMERT) in Nursing Students. BMC Nurs. 2025, 24, 478. [Google Scholar] [CrossRef] [PubMed]
- Barkhordari-Sharifabad, M.; Alipour, Z.; Jahantab, R. Reflective Capacity as a Predictor of Clinical Self-Efficacy in Nursing Students. BMC Med. Educ. 2025, 25, 614. [Google Scholar] [CrossRef] [PubMed]
- Braun, V.; Clarke, V. Using thematic analysis in psychology. Qual. Res. Psychol. 2006, 3, 77–101. [Google Scholar] [CrossRef]
- Yu, F.; Chu, G.; Yeh, T.; Fernandez, R. Enhancing Resilience to Improve Psychological Adaptation in Nurses. Int. J. Nurs. Stud. 2024, 157, 104825. [Google Scholar] [CrossRef] [PubMed]
| Category | Subcategory | Frequency (n) | Percentage (%) |
|---|---|---|---|
| Gender | Male | 52 | 17.9 |
| Female | 236 | 82.1 | |
| Work Experience (Years) | ≤5 years | 74 | 25.7 |
| 6–10 years | 82 | 28.5 | |
| 11–20 years | 57 | 19.8 | |
| >20 years | 75 | 26.0 | |
| Self-Reported Weekly Working Hours During COVID-19 | <40 h | 38 | 13.2 |
| 40 h | 152 | 52.8 | |
| >40 h | 98 | 34.0 | |
| Weekly Working Hours (Current Period) | <40 h | 39 | 13.5 |
| 40 h | 173 | 60.1 | |
| >40 h | 76 | 26.4 | |
| Work Department During COVID-19 | Intensive Care Unit (ICU) | 11 | 3.8 |
| Surgery | 22 | 7.6 | |
| Operating Room | 12 | 4.2 | |
| ENT/Ophthalmology | 15 | 5.2 | |
| Emergency | 38 | 13.2 | |
| Pathology | 24 | 8.3 | |
| COVID-19 Dedicated Ward | 55 | 19.1 | |
| Pediatrics | 41 | 14.2 | |
| Dispensary | 4 | 1.4 | |
| Maternity | 52 | 18.1 | |
| Pediatrics/ICU | 14 | 4.9 | |
| Current Work Department | Intensive Care Unit (ICU) | 12 | 4.2 |
| Surgery | 14 | 4.9 | |
| Infectious Diseases | 26 | 9.0 | |
| Operating Room | 15 | 5.2 | |
| ENT/Ophthalmology | 16 | 5.6 | |
| Emergency | 32 | 11.1 | |
| Pathology | 44 | 15.3 | |
| Pediatrics | 45 | 15.6 | |
| Dispensary | 2 | 0.7 | |
| Maternity | 63 | 21.9 | |
| Imaging | 2 | 0.7 | |
| Pediatrics/ICU | 17 | 5.9 | |
| Received Training During COVID-19 | Yes | 253 | 87.8 |
| No | 35 | 12.2 |
| Challenges Faced After the Pandemic | n | % | ||
|---|---|---|---|---|
| Workplace Weaknesses | Have you identified major weaknesses in the resources and infrastructure available at your workplace since the pandemic? | Rarely | 226 | 78.5 |
| Sometimes | 57 | 19.8 | ||
| Most of the time | 5 | 1.7 | ||
| Are workloads unsustainable due to staff shortages? | Rarely | 193 | 67 | |
| Sometimes | 62 | 21.5 | ||
| Most of the time | 33 | 11.5 | ||
| Has communication and support from your institution been insufficient after the pandemic? | Rarely | 187 | 64.9 | |
| Sometimes | 59 | 20.5 | ||
| Most of the time | 41 | 14.2 | ||
| Does your institution need to improve technological resources and staff training to address post-pandemic challenges? | Rarely | 227 | 78.8 | |
| Sometimes | 45 | 15.6 | ||
| Most of the time | 16 | 5.6 | ||
| Ongoing Work–life Stress | Has continuous stress negatively impacted your physical and mental well-being after the pandemic? | Rarely | 205 | 71.2 |
| Sometimes | 42 | 14.6 | ||
| Most of the time | 41 | 14.2 | ||
| Has your work–life balance worsened since the pandemic? | Rarely | 180 | 62.5 | |
| Sometimes | 63 | 21.9 | ||
| Most of the time | 45 | 15.6 | ||
| Are flexible work policies necessary to reduce stress at work? | Rarely | 168 | 58.3 | |
| Sometimes | 67 | 23.3 | ||
| Most of the time | 53 | 18.4 | ||
| Health Effects and Burnout | Have you experienced burnout or mental health issues as a result of the pandemic? | Rarely | 189 | 65.6 |
| Sometimes | 67 | 23.2 | ||
| Most of the time | 32 | 11.1 | ||
| Has the psychological support provided by your institution been sufficient to address the stress experienced? | Rarely | 202 | 70.1 | |
| Sometimes | 63 | 21.9 | ||
| Most of the time | 23 | 8 | ||
| Are workplace wellness programs necessary to prevent burnout? | Rarely | 211 | 73.3 | |
| Sometimes | 65 | 22.6 | ||
| Most of the time | 12 | 4.2 | ||
| Coping Mechanisms and Suggestions for the Future | n | % | ||
|---|---|---|---|---|
| Coping Mechanisms and Self-Care | Have you used physical exercises and recreational activities to reduce stress after the pandemic? | Rarely | 197 | 68.4 |
| Sometimes | 43 | 14.9 | ||
| Most of the time | 48 | 16.7 | ||
| Has the support group of colleagues helped you cope with daily challenges? | Rarely | 206 | 71.5 | |
| Sometimes | 43 | 14.9 | ||
| Most of the time | 39 | 13.5 | ||
| Have time off and leisure policies improved and maintained your health as a nurse? | Rarely | 226 | 78.5 | |
| Sometimes | 41 | 14.2 | ||
| Most of the time | 21 | 7.3 | ||
| Perspectives and Suggestions for the Future | Has the pandemic highlighted the importance of improving working conditions for nurses? | Rarely | 192 | 66.7 |
| Sometimes | 37 | 12.8 | ||
| Most of the time | 59 | 20.5 | ||
| Do you consider investment in training and professional development essential for the future careers of nurses? | Rarely | 230 | 79.9 | |
| Sometimes | 53 | 18.4 | ||
| Most of the time | 5 | 1.7 | ||
| Has the development of policies for psychological support been a priority in your healthcare institution? | Rarely | 253 | 87.8 | |
| Sometimes | 30 | 10.4 | ||
| Most of the time | 5 | 1.7 | ||
| Category | Subcategory | Frequency (n) | Percentage (%) | Mean (±SD) |
|---|---|---|---|---|
| Gender | Female | 38 | 80.9 | - |
| Male | 9 | 19.1 | - | |
| Age | - | - | 34 (±3.4) | |
| Hospital | Regional Hospital of Vlora | 28 | 59.6 | - |
| Regional Hospital of Fier | 19 | 40.4 | - | |
| Category | Content | Numeric Data |
|---|---|---|
| Strengths | Positive coping mechanisms (self-care, physical activity, family support).
| 23 out of 47 (48.9%) have attended ongoing training. |
| Weaknesses |
| 9 out of 47 (19.1%) had mental health training. Twelve out of 47 (25.5%) participants received resilience training. |
| Opportunities |
| 15 out of 47 (33.3%) reported new healthcare programs. |
| Threats |
| 38 of 47 (80%) had no leadership training. 33 of 47 (70.2%) had no crisis training. |
| Knowledge | Before | After | |
|---|---|---|---|
| 1 | Coping strategies | 12/25.5% | 20/42.6% |
| 2 | Impacts on mental health | 13/27.7% | 33/70.2% |
| 3 | Practical solutions | 15/31.9% | 36/76.6% |
| 4 | Current issues | 14/29.8% | 30/63.8% |
| 5 | Contribution to the profession | 13/27.7% | 35/74.5% |
| 6 | Lack of support | 12/25.5% | 18/38.3% |
| 7 | Work–life balance | 13/27.7% | 25/53.2% |
| 8 | Coping strategies | 11/23.4% | 22/46.8% |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Published by MDPI on behalf of the Lithuanian University of Health Sciences. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Çerçizaj, R.; Kamberi, F.; Kiçaj, E.; Prifti, V.; Qirko, S.; Kokalla, E.; Rogozea, L. Improving the Mental Health of Nursing Staff Seen from the Perspective of Staff a Preliminary Study. Medicina 2025, 61, 1573. https://doi.org/10.3390/medicina61091573
Çerçizaj R, Kamberi F, Kiçaj E, Prifti V, Qirko S, Kokalla E, Rogozea L. Improving the Mental Health of Nursing Staff Seen from the Perspective of Staff a Preliminary Study. Medicina. 2025; 61(9):1573. https://doi.org/10.3390/medicina61091573
Chicago/Turabian StyleÇerçizaj, Rudina, Fatjona Kamberi, Emirjona Kiçaj, Vasilika Prifti, Sonila Qirko, Erlini Kokalla, and Liliana Rogozea. 2025. "Improving the Mental Health of Nursing Staff Seen from the Perspective of Staff a Preliminary Study" Medicina 61, no. 9: 1573. https://doi.org/10.3390/medicina61091573
APA StyleÇerçizaj, R., Kamberi, F., Kiçaj, E., Prifti, V., Qirko, S., Kokalla, E., & Rogozea, L. (2025). Improving the Mental Health of Nursing Staff Seen from the Perspective of Staff a Preliminary Study. Medicina, 61(9), 1573. https://doi.org/10.3390/medicina61091573






