Comparison of Cup Position and Perioperative Characteristics in Total Hip Arthroplasty Following Three Types of Pelvic Osteotomy
Abstract
1. Introduction
2. Materials and Methods
2.1. Patients
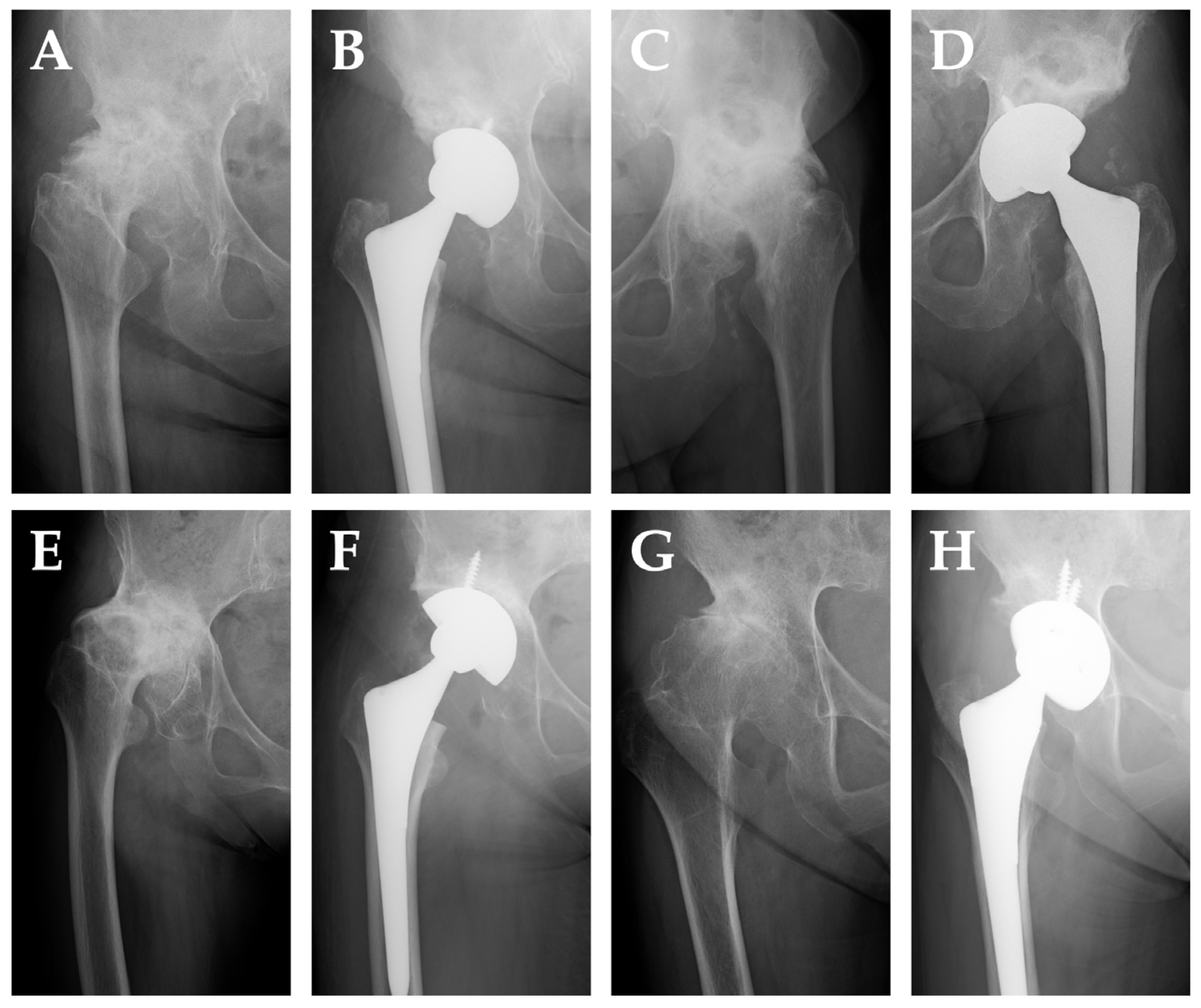
2.2. Radiographic Evaluation
- I.
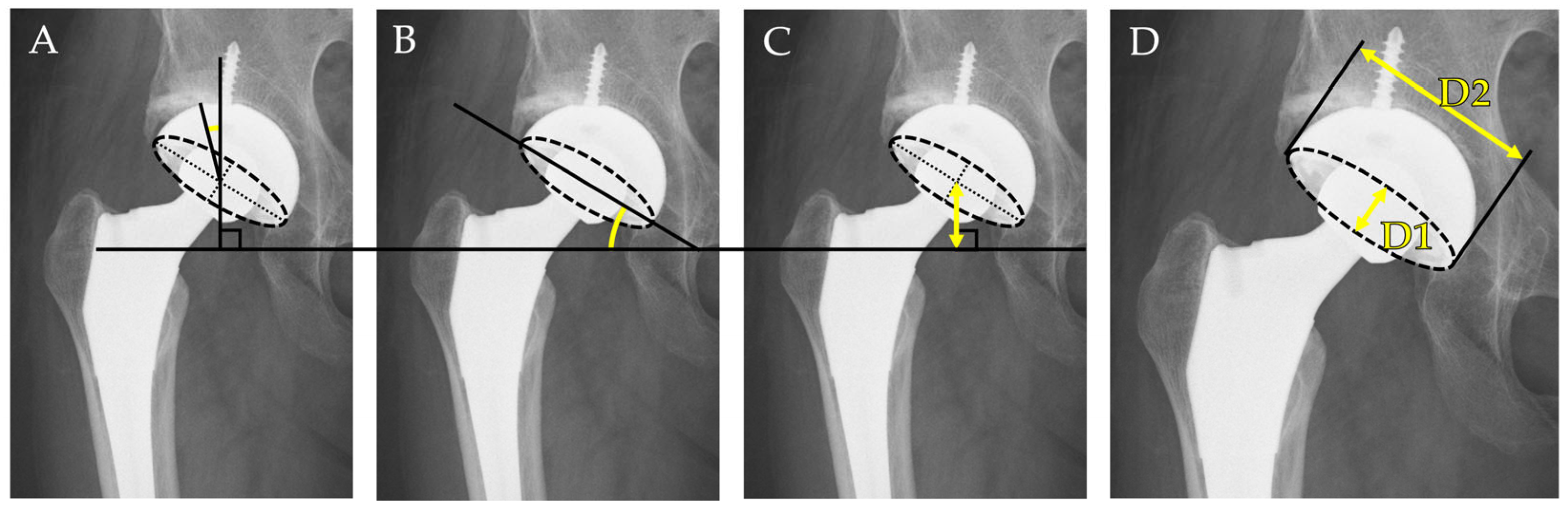
- Cup inclination angle: Defined as the angle between the inter-teardrop line and the opening face of the acetabular component. This reflects the abduction angle of the cup and was measured directly on the AP radiograph.
- II.
- Center-edge (CE) angle: Measured between a vertical line drawn from the center of the femoral head and a line connecting the femoral head center to the lateral edge of the acetabular cup. This parameter was used to evaluate the degree of lateral coverage of the implant.
- III.
- Cup height: Defined as the vertical distance between the center of the femoral head (or the prosthetic head) and the inter-teardrop line. In all cases, the inter-teardrop line was identifiable on standardized supine AP pelvic radiographs. In cases with mild distortion, contralateral bony landmarks and pelvic symmetry were used to confirm the accuracy of reference points.
- IV.
- Radiographic anteversion: Estimated using Lewinnek’s method [25], calculated as the inverse sine of the ratio of the short axis (D1) to the long axis (D2) of the elliptical projection of the cup on the AP radiograph:
2.3. Surgical Characteristics
- I.
- Operative time: Defined as the duration from skin incision to wound closure, recorded in minutes, as documented in the operative records.
- II.
- Estimated blood loss: Determined based on intraoperative suction volume and the weight of surgical sponges, as recorded in the anesthesia chart. This parameter was used to assess intraoperative bleeding associated with anatomical complexity or surgical difficulty.
- III.
- Use of bulk bone grafting or reinforcement devices: These reconstructive measures were employed when acetabular bone stock was insufficient for stable component fixation due to prior osteotomy, dysplasia, or bone defects. Bulk bone grafts consisted of either morselized or structural autografts harvested from the resected femoral head, or in some cases, allografts. Reinforcement devices included acetabular support rings (e.g., KT plates) and cages, selected intraoperatively according to the extent of bone deficiency.
2.4. Statistical Analysis
3. Results
3.1. Patient Background
3.2. Radiographic Measurements
3.3. Surgical Parameters
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| THA | Total hip arthroplasty |
| DDH | Developmental dysplasia of hip |
| PAO | Periacetabular osteotomy |
| CE | Center-edge |
| ICC | Intraclass Correlation Coefficient |
| AP | Anteroposterior |
References
- Jacobsen, S.; Sonne-Holm, S. Hip dysplasia: A significant risk factor for the development of hip osteoarthritis. A cross-sectional survey. Rheumatology 2005, 44, 211–218. [Google Scholar] [CrossRef] [PubMed]
- Reijman, M.; Hazes, J.M.W.; Pols, H.A.P.; Koes, B.W.; Bierma-Zeinstra, S.M.A. Acetabular Dysplasia Predicts Incident Osteoarthritis of the Hip The Rotterdam Study. Arthritis Rheum. 2005, 52, 787–793. [Google Scholar] [CrossRef]
- Sato, T.; Yamate, S.; Utsunomiya, T.; Inaba, Y.; Ike, H.; Kinoshita, K.; Doi, K.; Kawano, T.; Shiomoto, K.; Hara, T.; et al. Life Course Epidemiology of Hip Osteoarthritis in Japan A Multicenter, Cross-Sectional Study. J. Bone Jt. Surg. Am. 2024, 106, 966–975. [Google Scholar] [CrossRef]
- Southam, L.; Rodriguez-Lopez, J.; Wilkins, J.M.; Pombo-Suarez, M.; Snelling, S.; Gomez-Reino, J.J.; Chapman, K.; Gonzalez, A.; Loughlin, J. An SNP in the 5′-UTR of GDF5 is associated with osteoarthritis susceptibility in Europeans and with in vivo differences in allelic expression in articular cartilage. Hum. Mol. Genet. 2007, 16, 2226–2232. [Google Scholar] [CrossRef]
- Masuya, H.; Nishida, K.; Furuichi, T.; Toki, H.; Nishimura, G.; Kawabata, H.; Yokoyama, H.; Yoshida, A.; Tominaga, S.; Nagano, J.; et al. A novel dominant-negative mutation in Gdf5 generated by ENU mutagenesis impairs joint formation and causes osteoarthritis in mice. Hum. Mol. Genet. 2007, 16, 2366–2375. [Google Scholar] [CrossRef]
- Mototani, H.; Mabuchi, A.; Saito, S.; Fujioka, M.; Iida, A.; Takatori, Y.; Kotani, A.; Kubo, T.; Nakamura, K.; Sekine, A.; et al. A functional single nucleotide polymorphism in the core promoter region of CALM1 is associated with hip osteoarthritis in Japanese. Hum. Mol. Genet. 2005, 14, 1009–1017. [Google Scholar] [CrossRef]
- Nakajima, M.; Kizawa, H.; Saitoh, M.; Kou, I.; Miyazono, K.; Ikegawa, S. Mechanisms for asporin function and regulation in articular cartilage. J. Biol. Chem. 2007, 282, 32185–32192. [Google Scholar] [CrossRef]
- Feldman, G.J.; Parvizi, J.; Sawan, H.; Erickson, J.A.; Peters, C.L. Linkage Mapping and Whole Exome Sequencing Identify a Shared Variant in CXCR3 in a Large Multi-Generation Family. J. Arthroplast. 2014, 29, 238–241. [Google Scholar] [CrossRef] [PubMed]
- Mori, Y.; Ueno, K.; Chiba, D.; Hashimoto, K.; Kawai, Y.; Baba, K.; Tanaka, H.; Aki, T.; Ogasawara, M.; Shibasaki, N.; et al. Genome-Wide Association Study and Transcriptome of Japanese Patients with Developmental Dysplasia of the Hip Demonstrates an Association with the Ferroptosis Signaling Pathway. Int. J. Mol. Sci. 2023, 24, 5019. [Google Scholar] [CrossRef]
- Dygut, J.; Piwowar, M. Distinction Between Dysplasia, Malformation, and Deformity-Towards the Proper Diagnosis and Treatment of Hip Development Disorders. Diagnostics 2025, 15, 1547. [Google Scholar] [CrossRef] [PubMed]
- Wen, J.; Ping, H.; Kong, X.; Chai, W. Developmental dysplasia of the hip: A systematic review of susceptibility genes and epigenetics. Gene 2023, 853, 147067. [Google Scholar] [CrossRef]
- Bakarman, K.; Alsiddiky, A.M.; Zamzam, M.; Alzain, K.O.; Alhuzaimi, F.S.; Rafiq, Z. Developmental Dysplasia of the Hip (DDH): Etiology, Diagnosis, and Management. Cureus 2023, 15, e43207. [Google Scholar] [CrossRef]
- Venkatadass, K.; Durga Prasad, V.; Al Ahmadi, N.M.M.; Rajasekaran, S. Pelvic osteotomies in hip dysplasia: Why, when and how? EFORT Open Rev. 2022, 7, 153–163. [Google Scholar] [CrossRef] [PubMed]
- Ganz, R.; Klaue, K.; Vinh, T.S.; Mast, J.W. A new periacetabular osteotomy for the treatment of hip dysplasias. Technique and preliminary results. Clin. Orthop. Relat. Res. 1988, 232, 26–36. [Google Scholar] [CrossRef]
- Cirrincione, P.; Cao, N.; Trotzky, Z.; Nichols, E.; Sink, E. Does Periacetabular Osteotomy Change Sagittal Spinopelvic Alignment? Clin. Orthop. Relat. Res. 2024, 482, 1659–1667. [Google Scholar] [CrossRef] [PubMed]
- Bartonicek, J.; Vavra, J.; Chochola, A. Bosworth hip shelf arthroplasty in adult dysplastic hips: Ten to twenty three year results. Int. Orthop. 2012, 36, 2425–2431. [Google Scholar] [CrossRef][Green Version]
- Tanaka, H.; Chiba, D.; Mori, Y.; Kuwahara, Y.; Baba, K.; Yamada, N.; Fujii, G.; Itoi, E. Long-term results of a modified Spitzy shelf operation for developmental dysplasia of the hip in adults and adolescents. Eur. J. Orthop. Surg. Traumatol. 2018, 28, 1341–1347. [Google Scholar] [CrossRef]
- Chiari, K. Pelvic osteotomy in hip arthroplasty. Wien. Med. Wochenschr. 1953, 103, 707–709. [Google Scholar]
- Kurishima, H.; Chiba, D.; Baba, K.; Hamada, S.; Suzuki, T.; Kanabuchi, R.; Fujii, G.; Oyama, M.; Ochiai, T.; Mori, Y.; et al. Long-term results of Chiari pelvic osteotomy on the preservation of hip function with mean follow-up of more than 30 years and its prognostic factors. J. Orthop. Sci. 2024, 29, 990–994. [Google Scholar] [CrossRef]
- Jawad, M.U.; Scully, S.P. In brief: Crowe’s classification: Arthroplasty in developmental dysplasia of the hip. Clin. Orthop. Relat. Res. 2011, 469, 306–308. [Google Scholar] [CrossRef]
- Huan, S.W.; Wu, W.R.; Peng, S.J.; Zhuang, T.F.; Liu, N. Total hip arthroplasty after pelvic osteotomy: A meta-analysis. Acta Orthop. Belg. 2024, 90, 523–533. [Google Scholar] [CrossRef]
- Shapira, J.; Annin, S.; Rosinsky, P.J.; Maldonado, D.R.; Lall, A.C.; Domb, B.G. Total hip arthroplasty after pelvic osteotomy for acetabular dysplasia: A systematic review. J. Orthop. 2021, 25, 112–119. [Google Scholar] [CrossRef]
- Henderson, E.R.; Marulanda, G.A.; Cheong, D.; Temple, H.T.; Letson, G.D. Hip abductor moment arm--a mathematical analysis for proximal femoral replacement. J. Orthop. Surg. Res. 2011, 6, 6. [Google Scholar] [CrossRef]
- Göktaş, H.; Subaşi, E.; Uzkut, M.; Kara, M.; Biçici, H.; Shirazi, H.; Chethan, K.N.; Mihçin, Ş. Optimization of Hip Implant Designs Based on Its Mechanical Behaviour. In Biomechanics in Medicine, Sport and Biology; Lecture Notes in Networks and Systems: Cham, Switzerland, 2022; pp. 37–43. [Google Scholar]
- Lewinnek, G.E.; Lewis, J.L.; Tarr, R.; Compere, C.L.; Zimmerman, J.R. Dislocations after total hip-replacement arthroplasties. J. Bone Jt. Surg. Am. 1978, 60, 217–220. [Google Scholar] [CrossRef]
- Fukui, K.; Kaneuji, A.; Sugimori, T.; Ichiseki, T.; Matsumoto, T. Does rotational acetabular osteotomy affect subsequent total hip arthroplasty? Arch. Orthop. Trauma. Surg. 2015, 135, 407–415. [Google Scholar] [CrossRef] [PubMed]
- Sarin, V.K.; Pratt, W.R.; Bradley, G.W. Accurate femur repositioning is critical during intraoperative total hip arthroplasty length and offset assessment. J. Arthroplast. 2005, 20, 887–891. [Google Scholar] [CrossRef] [PubMed]
- Tanaka, H.; Yamada, N.; Kurishima, H.; Mori, Y.; Aizawa, T. Association between Hip Center Position and Isokinetic Hip Muscle Performance after Anterolateral Muscle-Sparing Total Hip Arthroplasty. Medicina 2022, 58, 538. [Google Scholar] [CrossRef]
- Wu, C.; Shu, G.; Xie, X.; Yuan, X.; Chen, S. Meta-analysis of the Efficacy of the Anatomical Center and High Hip Center Techniques in the Treatment of Adult Developmental Dysplasia of the Hip. Biomed. Res. Int. 2022, 2022, 7256664. [Google Scholar] [CrossRef]
- Bicanic, G.; Delimar, D.; Delimar, M.; Pecina, M. Influence of the acetabular cup position on hip load during arthroplasty in hip dysplasia. Int. Orthop. 2009, 33, 397–402. [Google Scholar] [CrossRef]
- Hidayat, T.; Ammarullah, M.I.; Saputra, E.; Lamura, M.D.P.; K N, C.; Ismail, R.; Bayuseno, A.P.; Jamari, J. A method for estimating the contact area of a dual-mobility total hip prosthesis. AIP Adv. 2024, 14, 015317. [Google Scholar] [CrossRef]
- Cho, M.R.; Choi, W.K.; Kim, J.J. Current Concepts of Using Large Femoral Heads in Total Hip Arthroplasty. Hip Pelvis 2016, 28, 134–141. [Google Scholar] [CrossRef] [PubMed]
- Kostensalo, I.; Junnila, M.; Virolainen, P.; Remes, V.; Matilainen, M.; Vahlberg, T.; Pulkkinen, P.; Eskelinen, A.; Makela, K.T. Effect of femoral head size on risk of revision for dislocation after total hip arthroplasty: A population-based analysis of 42,379 primary procedures from the Finnish Arthroplasty Register. Acta Orthop. 2013, 84, 342–347. [Google Scholar] [CrossRef] [PubMed]
- Houcke, J.V.; Khanduja, V.; Pattyn, C.; Audenaert, E. The History of Biomechanics in Total Hip Arthroplasty. Indian. J. Orthop. 2017, 51, 359–367. [Google Scholar] [CrossRef]
- Komiyama, K.; Hamai, S.; Motomura, G.; Ikemura, S.; Fujii, M.; Kawahara, S.; Nakashima, Y. Total hip arthroplasty after periacetabular osteotomy versus primary total hip arthroplasty: A propensity-matched cohort study. Arch. Orthop. Trauma. Surg. 2021, 141, 1411–1417. [Google Scholar] [CrossRef]
- Sikov, M.; Sloan, M.; Sheth, N.P. Effect of operative time on complications following primary total hip arthroplasty: Analysis of the NSQIP database. Hip Int. 2021, 31, 231–236. [Google Scholar] [CrossRef]
- Tamaki, T.; Oinuma, K.; Miura, Y.; Shiratsuchi, H. Total Hip Arthroplasty after Previous Acetabular Osteotomy: Comparison of Three Types of Acetabular Osteotomy. J. Arthroplast. 2016, 31, 172–175. [Google Scholar] [CrossRef]
- Parvizi, J.; Burmeister, H.; Ganz, R. Previous Bernese periacetabular osteotomy does not compromise the results of total hip arthroplasty. Clin. Orthop. Relat. Res. 2004, 423, 118–122. [Google Scholar] [CrossRef] [PubMed]
- Yuasa, T.; Maezawa, K.; Nozawa, M.; Kaneko, K. Total hip arthroplasty after previous rotational acetabular osteotomy. Eur. J. Orthop. Surg. Traumatol. 2015, 25, 1057–1060. [Google Scholar] [CrossRef]
- Tokunaga, K.; Aslam, N.; Zdero, R.; Schemitsch, E.H.; Waddell, J.P. Effect of prior Salter or Chiari osteotomy on THA with developmental hip dysplasia. Clin. Orthop. Relat. Res. 2011, 469, 237–243. [Google Scholar] [CrossRef]
- Chiari, C.; Schneider, E.; Stamm, T.; Peloschek, P.; Kotz, R.; Windhager, R. Ultra-long-term results of the Chiari pelvic osteotomy in hip dysplasia patients: A minimum of thirty-five years follow-up. Int. Orthop. 2024, 48, 291–299. [Google Scholar] [CrossRef]
- Minoda, Y.; Kadowaki, T.; Kim, M. Total hip arthroplasty of dysplastic hip after previous Chiari pelvic osteotomy. Arch. Orthop. Trauma. Surg. 2006, 126, 394–400. [Google Scholar] [CrossRef]
- Ikezaki, T.; Kawai, T.; Okuzu, Y.; Goto, K.; Kuroda, Y.; Matsuda, S. Effects of prior shelf procedure on subsequent conversion total hip arthroplasty. BMC Musculoskelet. Disord. 2024, 25, 963. [Google Scholar] [CrossRef]
- Willemsen, K.; Doelman, C.J.; Sam, A.S.Y.; Seevinck, P.R.; Sakkers, R.J.B.; Weinans, H.; van Der Wal, B.C.H. Long-term outcomes of the hip shelf arthroplasty in adolescents and adults with residual hip dysplasia: A systematic review. Acta Orthop. 2020, 91, 383–389. [Google Scholar] [CrossRef] [PubMed]
- Bishi, H.; Smith, J.B.V.; Asopa, V.; Field, R.E.; Wang, C.; Sochart, D.H. Comparison of the accuracy of 2D and 3D templating methods for planning primary total hip replacement: A systematic review and meta-analysis. EFORT Open Rev. 2022, 7, 70–83. [Google Scholar] [CrossRef]
- Shigemura, T.; Yamamoto, Y.; Murata, Y.; Sato, T.; Tsuchiya, R.; Wada, Y. Total hip arthroplasty after a previous pelvic osteotomy: A systematic review and meta-analysis. Orthop. Traumatol. Surg. Res. 2018, 104, 455–463. [Google Scholar] [CrossRef]
- Romanelli, F.; Hong, I.S.; Khan, J.A.; Porter, A.; Jankowski, J.M.; Liporace, F.A.; Yoon, R.S. Intraoperative Fluoroscopy Versus Navigation to Determine Cup Anteversion in Direct Anterior Total Hip Replacement: A Technical Trick for Obtaining “True” Anteversion. Arthroplast. Today 2024, 27, 101426. [Google Scholar] [CrossRef]
- Tanaka, H.; Tarasawa, K.; Mori, Y.; Baba, K.; Kanabuchi, R.; Kuriyama, Y.; Kurishima, H.; Fukuchi, H.; Kawamata, H.; Fushimi, K.; et al. Tranexamic acid in total hip arthroplasty: Nationwide evidence for reducing blood transfusions and post-operative complications. J. Jt. Surg. Res. 2025, 3, 132–137. [Google Scholar] [CrossRef]
- Ghelman, B.; Kepler, C.K.; Lyman, S.; Della Valle, A.G. CT outperforms radiography for determination of acetabular cup version after THA. Clin. Orthop. Relat. Res. 2009, 467, 2362–2370. [Google Scholar] [CrossRef] [PubMed]
- Mori, Y.; Mori, N.; Mori, T.; Nakamura, S.; Ishizuka, M.; Sano, T.; Itoi, E. Risk of acetabular protrusion is low in rheumatoid arthritis patients treated with bipolar hemiarthroplasty for displaced femoral neck fractures without rheumatoid change in hip joints. Eur. J. Orthop. Surg. Traumatol. 2014, 24, 905–909. [Google Scholar] [CrossRef]

| Parameter | PAO Group (n = 12) | Chiari Group (n = 5) | Shelf Group (n = 8) | Control Group (n = 25) | p-Value (vs Control) |
|---|---|---|---|---|---|
| Sex (Male/Female) | 1/11 | 1/4 | 3/5 | 4/21 | 0.52/0.82/0.19 |
| BMI (kg/m2) | 24.1 ± 3.0 | 23.7 ± 1.4 | 23.0 ± 2.5 | 24.7 ± 4.0 | 0.91/0.81/0.61 |
| Age at THA conversion (years) | 57.3 ± 11.3 | 63.0 ± 8.7 | 63.8 ± 8.6 | 63.6 ± 11.8 | 0.27/0.99/0.99 |
| Parameter | PAO Group (n = 12) | Chiari Group (n = 5) | Shelf Group (n = 8) | Control Group (n = 25) | p-Value (vs Control) |
|---|---|---|---|---|---|
| Center-edge angle | 24.4 ± 16.3 | 18.0 ± 12.3 | 28.2 ± 9.2 | 18.1 ± 8.4 | 0.33/0.99/0.21 |
| Inclination angle | 45.2 ± 10.4 | 39.2 ± 5.1 | 47.2 ± 5.0 | 43.7 ± 4.9 | 0.88/0.26/0.63 |
| Anteversion angle | 13.9 ± 5.6 | 9.4 ± 9.5 | 14.4 ± 10.0 | 14.7 ± 6.8 | 0.98/0.16/0.99 |
| Height (mm) | 29.0 ± 8.9 | 27.8 ± 7.5 | 27.2 ± 3.6 | 21.8 ± 5.4 | 0.0075 */0.07/0.21 |
| Parameter | PAO Group (n = 12) | Chiari Group (n = 5) | Shelf Group (n = 8) | Control Group (n = 25) | p-Value (vs Control) |
|---|---|---|---|---|---|
| Operative time (min) | 123.0 ± 58.0 | 97.2 ± 33.9 | 107.2 ± 27.1 | 93.1 ± 24.6 | 0.078/0.99/0.82 |
| Blood loss (cc) | 499.0 ± 472.4 | 329.2 ± 173.6 | 549.3 ± 295.1 | 466.0 ± 311.7 | 0.94/0.68/0.99 |
| Bulk bone graft use | 2 (16.7%) | 1 (12.5%) | 0 (0%) | 0 (0%) | 0.036 */0.07/1.0 |
| Support ring use | 2 (16.7%) | 0 (0%) | 0 (0%) | 0 (0%) | 0.036 */1.0/1.0 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Published by MDPI on behalf of the Lithuanian University of Health Sciences. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kanabuchi, R.; Mori, Y.; Baba, K.; Tanaka, H.; Kurishima, H.; Kuriyama, Y.; Fukuchi, H.; Kawamata, H.; Aizawa, T. Comparison of Cup Position and Perioperative Characteristics in Total Hip Arthroplasty Following Three Types of Pelvic Osteotomy. Medicina 2025, 61, 1407. https://doi.org/10.3390/medicina61081407
Kanabuchi R, Mori Y, Baba K, Tanaka H, Kurishima H, Kuriyama Y, Fukuchi H, Kawamata H, Aizawa T. Comparison of Cup Position and Perioperative Characteristics in Total Hip Arthroplasty Following Three Types of Pelvic Osteotomy. Medicina. 2025; 61(8):1407. https://doi.org/10.3390/medicina61081407
Chicago/Turabian StyleKanabuchi, Ryuichi, Yu Mori, Kazuyoshi Baba, Hidetatsu Tanaka, Hiroaki Kurishima, Yasuaki Kuriyama, Hideki Fukuchi, Hiroki Kawamata, and Toshimi Aizawa. 2025. "Comparison of Cup Position and Perioperative Characteristics in Total Hip Arthroplasty Following Three Types of Pelvic Osteotomy" Medicina 61, no. 8: 1407. https://doi.org/10.3390/medicina61081407
APA StyleKanabuchi, R., Mori, Y., Baba, K., Tanaka, H., Kurishima, H., Kuriyama, Y., Fukuchi, H., Kawamata, H., & Aizawa, T. (2025). Comparison of Cup Position and Perioperative Characteristics in Total Hip Arthroplasty Following Three Types of Pelvic Osteotomy. Medicina, 61(8), 1407. https://doi.org/10.3390/medicina61081407






