The Positional Relationship Between the Mandibular Canal and the Lower Third Molar Determined on Cone-Beam Computed Tomography
Abstract
1. Introduction
2. Materials and Methods
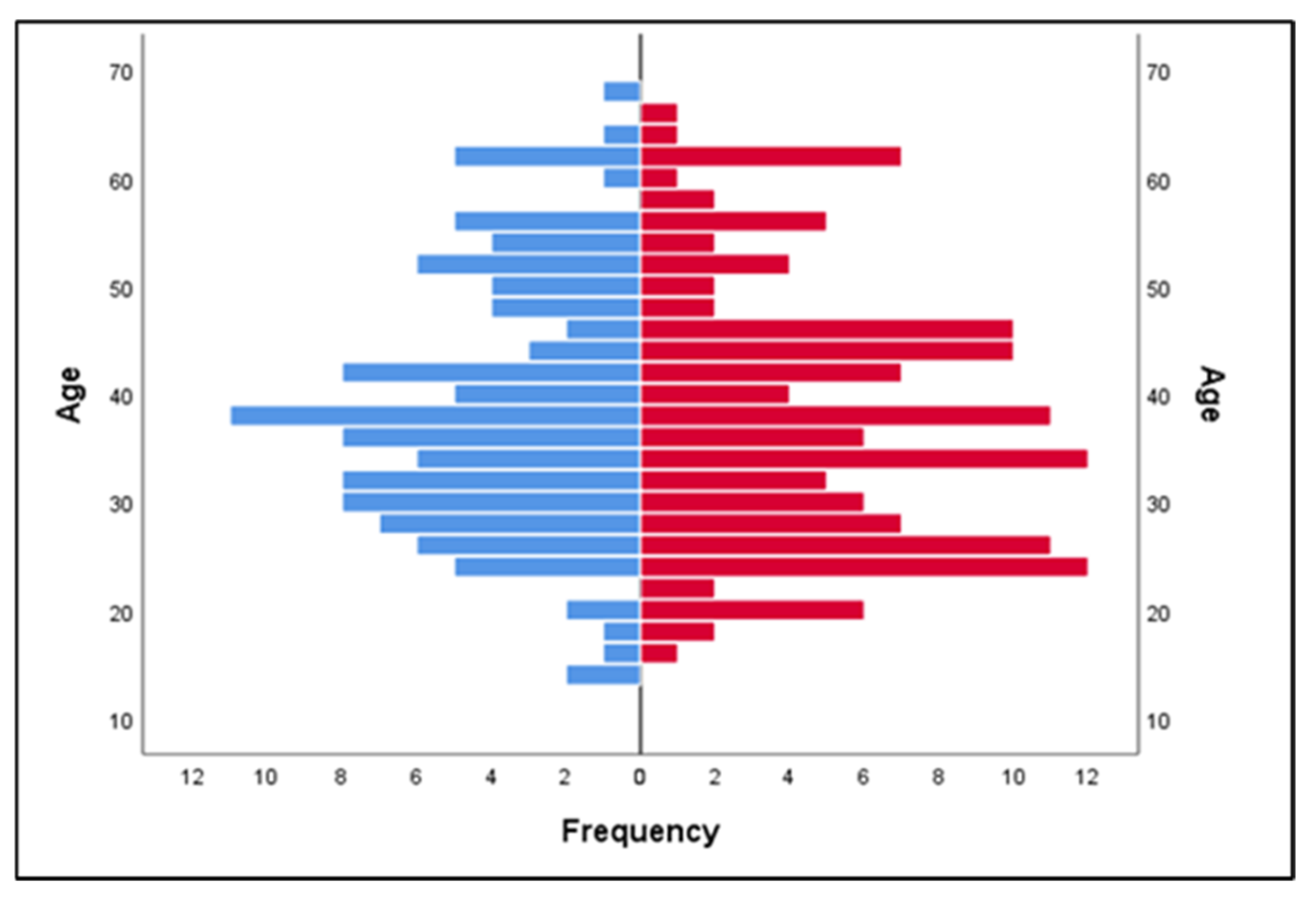
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| IAN | Inferior alveolar nerve |
| CBCT | Cone-beam computed tomography |
| OPG | Orthopantomograph |
| AR | Adjusted residuals |
References
- Liu, Z.L.; Jiang, E.S.; Cui, L.Y.; Li, J.X. Cone-Beam Computed Tomography Analysis on the Relationship between the Mandibular Third Molar and the Position of the Mandibular Canal in Koreans from the Yanbian Area and the Han People. Int. J. Clin. Pract. 2023, 2023, 9563476. [Google Scholar] [CrossRef]
- Mugnier, A. Embriologie et Développement Buco-Facial; J. Prelat: Paris, France, 1964. [Google Scholar]
- Almendros-Marqués, N.; Berini-Aytés, L.; Gay-Escoda, C. Influence of Lower Third Molar Position on the Incidence of Preoperative Complications. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2006, 102, 725–732. [Google Scholar] [CrossRef] [PubMed]
- Tuteja, M.; Bahirwani, S.; Balaji, P. An Evaluation of Third Molar Eruption for Assessment of Chronologic Age: A Panoramic Study. J. Forensic Dent. Sci. 2012, 4, 13–18. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Trakinienė, G.; Smailienė, D.; Lopatienė, K.; Trakinis, T.; Šidlauskas, A. Effect of Genetic and Environmental Factors on the Impaction of Lower Third Molars. Appl. Sci. 2021, 11, 1824. [Google Scholar] [CrossRef]
- Tsai, H.H. Factors Associated with Mandibular Third Molar Eruption and Impaction. J. Clin. Pediatr. Dent. 2005, 30, 109–113. [Google Scholar] [CrossRef] [PubMed]
- Jeevitha, J.Y.; Thiagarajan, A.; Sivalingam, B. Influence and Impact of Mandibular Ramal Dimensions on the Incidence of Lower Third Molar Impaction: A Prospective Study. J. Pharm. Bioallied Sci. 2022, 14 (Suppl. S1), S364–S368. [Google Scholar] [CrossRef]
- Barone, S.; Antonelli, A.; Averta, F.; Diodati, F.; Muraca, D.; Bennardo, F.; Giudice, A. Does Mandibular Gonial Angle Influence the Eruption Pattern of the Lower Third Molar? A Three-Dimensional Study. J. Clin. Med. 2021, 10, 4057. [Google Scholar] [CrossRef]
- Ghaeminia, H.; Meijer, G.J.; Soehardi, A.; Borstlap, W.A.; Mulder, J.; Bergé, S.J. Position of the Impacted Third Molar in Relation to the Mandibular Canal. Diagnostic Accuracy of Cone Beam Computed Tomography Compared with Panoramic Radiography. Int. J. Oral Maxillofac. Surg. 2009, 38, 964–971. [Google Scholar] [CrossRef]
- Zhu, T.; Chen, D.; Wu, F.; Zhu, F.; Zhu, H. Artificial Intelligence Model to Detect Real Contact Relationship between Mandibular Third Molars and Inferior Alveolar Nerve Based on Panoramic Radiographs. Diagnostics 2021, 11, 1664. [Google Scholar] [CrossRef]
- Patel, P.S.; Shah, J.S.; Dudhia, B.B.; Butala, P.B.; Jani, Y.V.; Macwan, R.S. Comparison of Panoramic Radiograph and Cone Beam Computed Tomography Findings for Impacted Mandibular Third Molar Root and Inferior Alveolar Nerve Canal Relation. Indian J. Dent. Res. 2020, 31, 91–102. [Google Scholar] [CrossRef]
- Leung, Y.Y.; Hung, K.F.; Li, D.T.S.; Yeung, A.W.K. Application of Cone Beam Computed Tomography in Risk Assessment of Lower Third Molar Surgery. Diagnostics 2023, 13, 919. [Google Scholar] [CrossRef]
- Kiencało, A.; Jamka-Kasprzyk, M.; Panaś, M.; Wyszyńska-Pawelec, G. Analysis of Complications after the Removal of 339 Third Molars. Dent. Med. Probl. 2021, 58, 75–80. [Google Scholar] [CrossRef]
- Sayed, N.; Bakathir, A.; Pasha, M.; Al-Sudairy, S. Complications of Third Molar Extraction: A Retrospective Study from a Tertiary Healthcare Centre in Oman. Sultan Qaboos Univ. Med. J. 2019, 19, e230–e235. [Google Scholar] [CrossRef]
- Sukegawa, S.; Yokota, K.; Kanno, T.; Manabe, Y.; Sukegawa-Takahashi, Y.; Masui, M.; Furuki, Y. What are the risk factors for postoperative infections of third molar extraction surgery: A retrospective clinical study? Med. Oral Patol. Oral Cir. Bucal 2019, 24, e123–e129. [Google Scholar] [CrossRef]
- Candotto, V.; Oberti, L.; Gabrione, F.; Scarano, A.; Rossi, D.; Romano, M. Complication in Third Molar Extractions. J. Biol. Regul. Homeost. Agents 2019, 33 (Suppl. S1), 169–172. [Google Scholar] [PubMed]
- Miclotte, I.; Agbaje, J.O.; Spaey, Y.; Legrand, P.; Politis, C. Incidence and Treatment of Complications in Patients Who Had Third Molars or Other Teeth Extracted. Br. J. Oral Maxillofac. Surg. 2018, 56, 388–393. [Google Scholar] [CrossRef] [PubMed]
- Shintani, Y.; Nakanishi, T.; Ueda, M.; Mizobata, N.; Tojyo, I.; Fujita, S. Comparison of Subjective and Objective Assessments of Neurosensory Function after Lingual Nerve Repair. Med. Princ. Pract. 2019, 28, 231–235. [Google Scholar] [CrossRef] [PubMed]
- Brauer, H.U. Unusual Complications Associated with Third Molar Surgery: A Systematic Review. Quintessence Int. 2009, 40, 565–572. [Google Scholar]
- Azenha, M.R.; Kato, R.B.; Bueno, R.B.; Neto, P.J.; Ribeiro, M.C. Accidents and Complications Associated to Third Molar Surgeries Performed by Dentistry Students. Oral Maxillofac. Surg. 2014, 18, 459–464. [Google Scholar] [CrossRef]
- Bouloux, G.F.; Steed, M.B.; Perciaccante, V.J. Complications of Third Molar Surgery. Oral Maxillofac. Surg. Clin. N. Am. 2007, 19, 117–128. [Google Scholar] [CrossRef]
- Jerjes, W.; Upile, T.; Shah, P.; Nhembe, F.; Gudka, D.; Kafas, P.; McCarthy, E.; Abbas, S.; Patel, S.; Hamdoon, Z.; et al. Risk Factors Associated with Injury to the Inferior Alveolar and Lingual Nerves Following Third Molar Surgery—Revisited. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2010, 109, 335–345. [Google Scholar] [CrossRef]
- Brann, C.R.; Brickley, M.R.; Shepherd, J.P. Factors Influencing Nerve Damage during Lower Third Molar Surgery. Br. Dent. J. 1999, 186, 514–516. [Google Scholar] [CrossRef]
- Costantinides, F.; Biasotto, M.; Maglione, M.; Di Lenarda, R. Local vs General Anaesthesia in the Development of Neurosensory Disturbances after Mandibular Third Molars Extraction: A Retrospective Study of 534 Cases. Med. Oral Patol. Oral Cir. Bucal 2016, 21, e724–e730. [Google Scholar] [CrossRef] [PubMed]
- Robinson, P.P. Observations on the Recovery of Sensation Following Inferior Alveolar Nerve Injuries. Br. J. Oral Maxillofac. Surg. 1988, 26, 177–189. [Google Scholar] [CrossRef] [PubMed]
- Hartman, B.; Adlesic, E.C. Evaluation and Management of Impacted Teeth in the Adolescent Patient. Dent. Clin. N. Am. 2021, 65, 805–814. [Google Scholar] [CrossRef] [PubMed]
- De Sousa, A.S.; Neto, J.V.; Normando, D. The Prediction of Impacted Versus Spontaneously Erupted Mandibular Third Molars. Prog. Orthod. 2021, 22, 29. [Google Scholar] [CrossRef]
- Céspedes-Sánchez, J.M.; Ayuso-Montero, R.; Marí-Roig, A.; Arranz-Obispo, C.; López-López, J. The Importance of a Good Evaluation in Order to Prevent Oral Nerve Injuries: A Review. Acta Odontol. Scand. 2014, 72, 161–167. [Google Scholar] [CrossRef]
- Ghaeminia, H.; Gerlach, N.L.; Hoppenreijs, T.J.; Kicken, M.; Dings, J.P.; Borstlap, W.A.; de Haan, T.; Bergé, S.J.; Meijer, G.J.; Maal, T.J. Clinical Relevance of Cone Beam Computed Tomography in Mandibular Third Molar Removal: A Multicentre, Randomised, Controlled Trial. J. Craniomaxillofac. Surg. 2015, 43, 2158–2167. [Google Scholar] [CrossRef]
- Ghaeminia, H.; Meijer, G.J.; Soehardi, A.; Borstlap, W.A.; Mulder, J.; Vlijmen, O.J.; Bergé, S.J.; Maal, T.J.J. The Use of Cone Beam CT for the Removal of Wisdom Teeth Changes the Surgical Approach Compared with Panoramic Radiography: A Pilot Study. Int. J. Oral Maxillofac. Surg. 2011, 40, 834–839. [Google Scholar] [CrossRef]
- Guerrero, M.E.; Botetano, R.; Beltran, J.; Horner, K.; Jacobs, R. Can Preoperative Imaging Help to Predict Postoperative Outcome after Wisdom Tooth Removal? A Randomized Controlled Trial Using Panoramic Radiography Versus Cone-Beam CT. Clin. Oral Investig. 2014, 18, 335–342. [Google Scholar] [CrossRef]
- Guerrero, M.E.; Nackaerts, O.; Beinsberger, J.; Horner, K.; Schoenaers, J.; Jacobs, R.; SEDENTEXCT Project Consortium. Inferior Alveolar Nerve Sensory Disturbance after Impacted Mandibular Third Molar Evaluation Using Cone Beam Computed Tomography and Panoramic Radiography: A Pilot Study. J. Oral Maxillofac. Surg. 2012, 70, 2264–2270. [Google Scholar] [CrossRef]
- Gu, L.; Zhu, C.; Chen, K.; Liu, X.; Tang, Z. Anatomic Study of the Position of the Mandibular Canal and Corresponding Mandibular Third Molar on Cone-Beam Computed Tomography Images. Surg. Radiol. Anat. 2018, 40, 609–614. [Google Scholar] [CrossRef]
- Chaudhary, B.; Joshi, U.; Dahal, S.; Sagtani, A.; Khanal, P.; Bhattarai, N. Anatomical Position of Lower Third Molar in Relation to Mandibular Canal on Cone-Beam Computed Tomography Images in A Tertiary Care Hospital: A Descriptive Cross-sectional Study. JNMA J. Nepal Med. Assoc. 2020, 58, 879–883. [Google Scholar] [CrossRef]
- Ge, J.; Zheng, J.W.; Yang, C.; Qian, W.T. Variations in the Buccal-Lingual Alveolar Bone Thickness of Impacted Mandibular Third Molar: Our Classification and Treatment Perspectives. Sci. Rep. 2016, 6, 16375. [Google Scholar] [CrossRef]




| Frequency (no.) | Percentage (%) | |
|---|---|---|
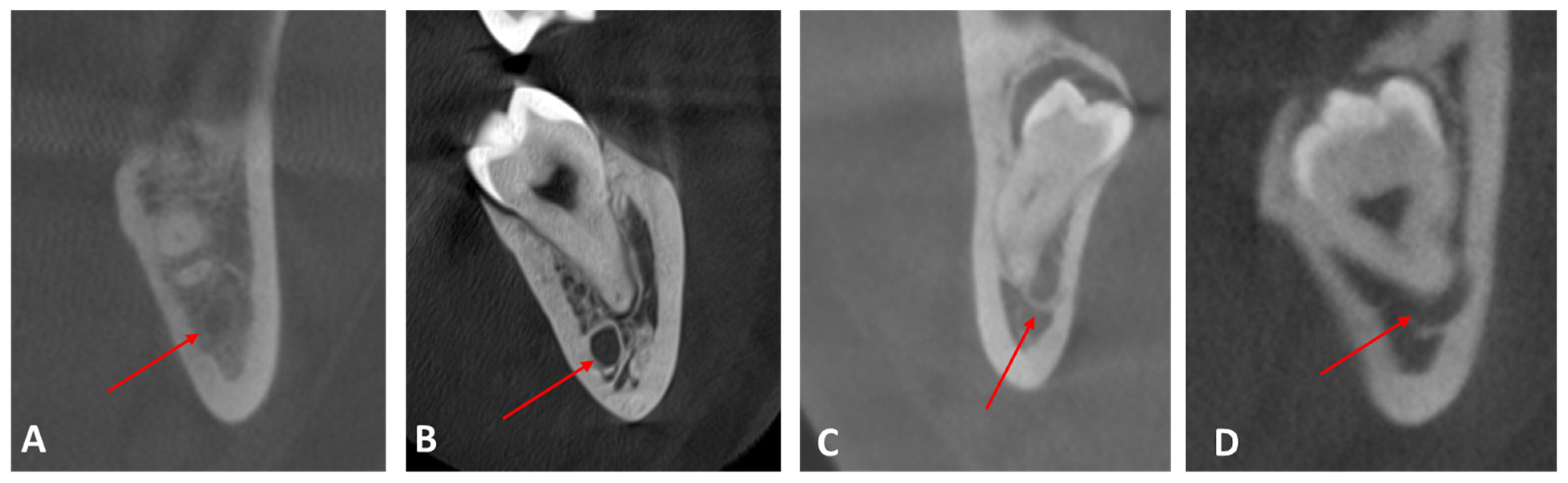
| Class I: the mandibular canal locates on the apical side | 179 | 70.8 |
| Class II: the mandibular canal locates on the buccal side | 44 | 17.4 |
| Class III: the mandibular canal locates on the lingual side | 21 | 8.3 |
| Class IV: the mandibular canal locates between the roots | 9 | 3.6 |
| Total | 253 | 100.0 |
| Frequency | Percent | |
|---|---|---|
| No contact | 167 | 66.0 |
| Contact with complete white line | 27 | 10.7 |
| Contact with a defective white line | 56 | 22.1 |
| Penetration of the mandibular canal | 3 | 1.2 |
| Total | 253 | 100.0 |
| Frequency | Percent | ||
|---|---|---|---|
| Valid | 0–2 mm | 25 | 9.9 |
| 2–4 mm | 50 | 19.8 | |
| 4–6 mm | 39 | 15.4 | |
| 6–8 mm | 32 | 12.6 | |
| 8–10 mm | 16 | 6.3 | |
| over 10 mm | 5 | 2.0 | |
| Total | 167 | 66.0 | |
| Missing | System | 86 | 34.0 |
| Total | 253 | 100.0 | |
| Contact | Total | ||||||
|---|---|---|---|---|---|---|---|
| No Contact | Contact with Complete White Line | Contact with a Defective White Line | Penetration of the Mandibular Canal | ||||
| Position of the mandibular canal | Class I: the mandibular canal is located on the apical side | Count | 135 | 20 | 23 | 1 | 179 |
| Expected count | 118.2 | 19.1 | 39.6 | 2.1 | 179.0 | ||
| % within position of the mandibular canal | 75.4% | 11.2% | 12.8% | 0.6% | 100.0% | ||
| % within contact | 80.8% | 74.1% | 41.1% | 33.3% | 70.8% | ||
| Adjusted residual | 4.9 | 0.4 | −5.5 | −1.4 | |||
| Class II: the mandibular canal is located on the buccal side | Count | 29 | 4 | 11 | 0 | 44 | |
| Expected count | 29.0 | 4.7 | 9.7 | 0.5 | 44.0 | ||
| % within position of the mandibular canal | 65.9% | 9.1% | 25.0% | 0.0% | 100.0% | ||
| % within contact | 17.4% | 14.8% | 19.6% | 0.0% | 17.4% | ||
| Adjusted residual | 0.0 | −0.4 | 0.5 | −0.8 | |||
| Class III: the mandibular canal is located on the lingual side | Count | 3 | 3 | 14 | 1 | 21 | |
| Expected count | 13.9 | 2.2 | 4.6 | 0.2 | 21.0 | ||
| % within position of the mandibular canal | 14.3% | 14.3% | 66.7% | 4.8% | 100.0% | ||
| % within contact | 1.8% | 11.1% | 25.0% | 33.3% | 8.3% | ||
| Adjusted residual | −5.2 | 0.6 | 5.1 | 1.6 | |||
| Class IV: the mandibular canal is located between the roots | Count | 0 | 0 | 8 | 1 | 9 | |
| Expected count | 5.9 | 1.0 | 2.0 | 0.1 | 9.0 | ||
| % within position of the mandibular canal | 0.0% | 0.0% | 88.9% | 11.1% | 100.0% | ||
| % within contact | 0.0% | 0.0% | 14.3% | 33.3% | 3.6% | ||
| Adjusted residual | −4.3 | −1.1 | 4.9 | 2.8 | |||
| Total | Count | 167 | 27 | 56 | 3 | 253 | |
| Expected count | 167.0 | 27.0 | 56.0 | 3.0 | 253.0 | ||
| % within position of the mandibular canal | 66.0% | 10.7% | 22.1% | 1.2% | 100.0% | ||
| % within contact | 100.0% | 100.0% | 100.0% | 100.0% | 100.0% | ||
| Distance | Total | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| 0–2 mm | 2–4 mm | 4–6 mm | 6–8 mm | 8–10 mm | Over 10 mm | ||||
| Position of the mandibular canal | Class I | Count | 18 | 35 | 31 | 31 | 15 | 5 | 135 |
| Expected count | 20.2 | 40.4 | 31.5 | 25.9 | 12.9 | 4.0 | 135.0 | ||
| % within position of the mandibular canal | 13.3% | 25.9% | 23.0% | 23.0% | 11.1% | 3.7% | 100.0% | ||
| % within distance (mm) | 72.0% | 70.0% | 79.5% | 96.9% | 93.8% | 100.0% | 80.8% | ||
| Adjusted residual | −1.2 | −2.3 | −0.2 | 2.6 | 1.4 | 1.1 | |||
| Class II | Count | 7 | 13 | 7 | 1 | 1 | 0 | 29 | |
| Expected count | 4.3 | 8.7 | 6.8 | 5.6 | 2.8 | 0.9 | 29.0 | ||
| % within position of the mandibular canal | 24.1% | 44.8% | 24.1% | 3.4% | 3.4% | 0.0% | 100.0% | ||
| % within distance (mm) | 28.0% | 26.0% | 17.9% | 3.1% | 6.3% | 0.0% | 17.4% | ||
| Adjusted residual | 1.5 | 1.9 | 0.1 | −2.4 | −1.2 | −1.0 | |||
| Class III | Count | 0 | 2 | 1 | 0 | 0 | 0 | 3 | |
| Expected count | 0.4 | 0.9 | 0.7 | 0.6 | 0.3 | 0.1 | 3.0 | ||
| % within position of the mandibular canal | 0.0% | 66.7% | 33.3% | 0.0% | 0.0% | 0.0% | 100.0% | ||
| % within distance (mm) | 0.0% | 4.0% | 2.6% | 0.0% | 0.0% | 0.0% | 1.8% | ||
| Adjusted residual | −0.7 | 1.4 | 0.4 | −0.9 | −0.6 | −0.3 | |||
| Total | Count | 25 | 50 | 39 | 32 | 16 | 5 | 167 | |
| Expected count | 25.0 | 50.0 | 39.0 | 32.0 | 16.0 | 5.0 | 167.0 | ||
| % within position of the mandibular canal | 15.0% | 29.9% | 23.4% | 19.2% | 9.6% | 3.0% | 100.0% | ||
| % within distance (mm) | 100.0% | 100.0% | 100.0% | 100.0% | 100.0% | 100.0% | 100.0% | ||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Published by MDPI on behalf of the Lithuanian University of Health Sciences. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Urechescu, H.; Banu, A.; Pricop, M.; Streian, F.; Pricop, A.; Cuzic, C. The Positional Relationship Between the Mandibular Canal and the Lower Third Molar Determined on Cone-Beam Computed Tomography. Medicina 2025, 61, 1291. https://doi.org/10.3390/medicina61071291
Urechescu H, Banu A, Pricop M, Streian F, Pricop A, Cuzic C. The Positional Relationship Between the Mandibular Canal and the Lower Third Molar Determined on Cone-Beam Computed Tomography. Medicina. 2025; 61(7):1291. https://doi.org/10.3390/medicina61071291
Chicago/Turabian StyleUrechescu, Horatiu, Ancuta Banu, Marius Pricop, Felicia Streian, Alisia Pricop, and Cristiana Cuzic. 2025. "The Positional Relationship Between the Mandibular Canal and the Lower Third Molar Determined on Cone-Beam Computed Tomography" Medicina 61, no. 7: 1291. https://doi.org/10.3390/medicina61071291
APA StyleUrechescu, H., Banu, A., Pricop, M., Streian, F., Pricop, A., & Cuzic, C. (2025). The Positional Relationship Between the Mandibular Canal and the Lower Third Molar Determined on Cone-Beam Computed Tomography. Medicina, 61(7), 1291. https://doi.org/10.3390/medicina61071291







