Study on Quality of Life of Patients with Obstructive Sleep Apnea—Pilot Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Patient Selection
2.2. Quality of Life Measurement
2.3. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Ahmed, A.; Husain, A.; Love, T.E.; Gambassi, G.; Dell’Italia, L.J.; Francis, G.S.; Gheorghiade, M.; Allman, R.M.; Meleth, S.; Bourge, R.C. Heart failure, chronic diuretic use, and increase in mortality and hospitalization: An observational study using propensity score methods. Eur. Heart J. 2006, 27, 1431–1439. [Google Scholar] [CrossRef]
- Akashiba, T.; Kawahara, S.; Akahosni, T.; Chiharu, O.; Saito, O.; Majima, T.; Horie, T. Relationship between quality of life and mood or depression in patients with severe obstructive sleep apnea syndrome. Chest 2002, 122, 861–865. [Google Scholar] [CrossRef] [PubMed]
- Rohra, A.K.; Demko, C.A.; Hans, M.G.; Rosen, C.; Palomoc, J.M. Sleep disordered breathing in children seeking orthodontic care. Am. J. Orthod. Dentofac. Orthop. 2018, 154, 65–71. [Google Scholar] [CrossRef] [PubMed]
- Minagi, H.O.; Okuno, K.; Nohara, K.; Sakai, T. Predictors of Side Effects with Long-Term Oral Appliance Therapy for Obstructive Sleep Apnea. J. Clin. Sleep Med. 2018, 14, 119–125. [Google Scholar] [CrossRef] [PubMed]
- Fransson, A.M.C.; Benavente-Lundahl, C.; Isacsson, G. A prospective 10-year cephalometric follow-up study of patients with obstructive sleep apnea and snoring who used a mandibular protruding device. Am. J. Orthod. Dentofac. Orthop. 2020, 157, 91–97. [Google Scholar] [CrossRef]
- He, J.; Wang, Y.; Hu, H.; Liao, Q.; Zhang, W.; Xiang, X.; Fan, X. Impact on the upper airway space of different types of orthognathic surgery for the correction of skeletal class III malocclusion: A systematic review and meta-analysis. Int. J. Surg. 2017, 38, 31–40. [Google Scholar] [CrossRef]
- Williams, S.K.; Ravenell, J.; Girardin, J.L.; Zizi, F.; Underberg, J.A.; McFarlane, S.I.; Ogedegbe, G. Resistant Hypertension and Sleep Apnea: Pathophysiologic Insights and Strategic Management. Curr. Diab. Rep. 2011, 11, 64–69. [Google Scholar] [CrossRef]
- Arnardottir, E.S.; Janson, C.; Bjornsdotttir, E.; Benediktsdottir, B.; Juliusson, S.; Kuna, S.T.; Pack, A.I.; Gislason, T. Nocturnal sweating–a common symptom of obstructive sleep apnoea: The Icelandic sleep apnoea cohort. BMJ Open 2013, 3, e002795. [Google Scholar] [CrossRef]
- Avlonitou, E.; Kapsimalis, F.; Varouchakis, G.; Vardavas, C.; Behrakis, P. Adherence to CPAP therapy improves quality of life and reduces symptoms among obstructive sleep apnea syndrome patients. Sleep Breath. 2012, 16, 563–569. [Google Scholar] [CrossRef]
- Juniper, E.F.; Guyatt, G.H.; Epstein, R.S.; Ferrie, P.J.; Jaeschke, R.; Hiller, T.K. Evaluation of impairment of health-related quality of life in asthma: Development of a questionnaire for use in clinical trials. Thorax 1992, 47, 76–83. [Google Scholar] [CrossRef]
- Arnardottir, E.S.; Maislin, G.; Schwab, R.J.; Staley, B.; Benediktsdottir, B.; Olafsson, I.; Juliusson, S.; Romer, M.; Gislason, T.; Pack, A.I. The interaction of obstructive sleep apnea and obesity on the inflammatory markers C-reactive protein and interleukin-6: The Icelandic Sleep Apnea Cohort. Sleep 2012, 35, 921–932. [Google Scholar] [CrossRef] [PubMed]
- Behrents, R.G.; Valanju Shelgikar, A.; Conley, R.S.; Flores-Mir, C.; Hans, M.; Levine, M.; McNamara, J.A.; Palomo, J.M.; Pliska, B.; Stockstill, J.W.; et al. Obstructive sleep apnea and orthodontics: An American Association of Orthodontists White Paper. Am. J. Orthod. Dentofac. Orthop. 2019, 156, 13–28. [Google Scholar] [CrossRef] [PubMed]
- Flemons, W.W.; Reimer, M.A. Development of a disease-specific health-related quality of life questionnaire for sleep apnea. Am. J. Respir. Crit. Care Med. 1998, 158, 494–503. [Google Scholar] [CrossRef] [PubMed]
- Buist, A.S.; McBurnie, M.A.; Vollmer, W.M.; Gillespie, S.; Burney, P.; Mannino, D.M.; Menezes, A.M.B.; Sullivan, S.D.; Lee, T.A.; Weiss, K.B.; et al. International variation in the prevalence of COPD (the BOLD Study): A population-based prevalence study. Lancet 2007, 370, 741–775. [Google Scholar] [CrossRef]
- Strohl, K.P.; Redline, S. Recognition of obstructive sleep apnea. Am. J. Respir. Crit. Care Med. 1996, 154, 279–289. [Google Scholar] [CrossRef]
- Ringler, J.; Basner, R.C.; Shannon, R.; Schwartzstein, R.; Manning, H.; Weinberger, S.E.; Weiss, J.W. Hypoxemia alone does not explain blood pressure elevations after obstructive apneas. J. Appl.Physiol. 1990, 69, 2143–2148. [Google Scholar] [CrossRef]
- Cheshire, K.; Deary, H.E.I.; Shapiro, C.; Douglas, N.J. Factors impairing daytime performance in patients with sleep apnea/hypopnea syndrome. Arch. Intern. Med. 1992, 152, 538–541. [Google Scholar] [CrossRef]
- Fransson, A.M.C.; Isacsson, G.; Nohlert, E. The outcome of oral appliance therapy on position-dependent obstructive sleep apnea: A multicenter randomized controlled trial. Am. J. Orthod. Dentofac. Orthop. 2022, 162, 386–393. [Google Scholar] [CrossRef]
- Hudgel, D.W. Neuropsychiatric manifestations of obstructive sleep apnea: A review. Int. J. Psychiatry Med. 1989, 19, 11–22. [Google Scholar] [CrossRef]
- Tanellari, O.; Murariu, A.; Roșu, S.; Savin, C.; Romanec, C.; Armencia, A.; Balcoș, C.; Haddad, C.D.; Zetu, I.N. Validation of the Romanian version of the “Calgary Sleep Apnea Quality Of Life Index (SAQLI)”. Rom. J. Med. Dent. Educ. 2022, 11, 22–27. [Google Scholar]
- Tanellari, O.; Bamboi, I.; Toader, B.; Armencia, A.; Balcoș, C.; Panaite, T. Validation of the albanian version of the “Calgary Sleep Apnea Quality Of Life Index (SAQLI)”. Rom. J. Med. Dent. Educ. 2025, 14, 30–35. [Google Scholar]
- Flemons, W.W.; Reimer, M.A. Measurement properties of the Calgary Sleep Apnea Quality of Life Index. Am. J. Respir. Crit. Care Med. 2002, 165, 159–164. [Google Scholar] [CrossRef] [PubMed]
- Adenekan, B.; Spurr, K.F.; Olafiranye, O. Measuring quality of life in patients with obstructive sleep apnea: Usefulness of the SAQLI. J. Clin. Sleep. Med. 2019, 15, 405–412. [Google Scholar]
- Weaver, T.E.; Maislin, G.; Dinges, D.F.; Bloxham, T.; George, C.F.; Greenberg, H.; Kader, G.; Mahowald, M.; Younger, J.; Pack, A.I. Relationship between hours of CPAP use and achieving normal levels of sleepiness and daily functioning. Sleep 2007, 30, 711–719. [Google Scholar] [CrossRef] [PubMed]
- Karkala, A.; Baxevanidis, A.; Chasiotou, A.; Siopi, D.; Mameletzi, D.; Kouidi, E.; Chloros, D.; Pitsiou, G.; Boutou, A.K. Comparison of physical activity and quality of life between obese individuals with obstructive sleep apnea syndrome and individuals with obesity hypoventilation syndrome. Sleep Breath. 2024, 28, 2683–2691. [Google Scholar] [CrossRef]
- Mendelson, M.; Marillier, M.; Bailly, S.; Flore, P.; Borel, J.C.; Vivodtzev, I.; Doutreleau, S.; Tamisier, R.; Pépin, J.L.; Verges, S. Maximal exercise capacity in patients with obstructive sleep apnoea syndrome: A systematic review and meta-analysis. Eur. Respir. J. 2018, 51, 1702697. [Google Scholar] [CrossRef] [PubMed]
- Luyster, F.S.; Dunbar-Jacob, J.; Aloia, M.S.; Martire, L.M.; Buysse, D.J.; Strollo, P.J. Patient and partner experiences with obstructive sleep apnea and CPAP treatment: A qualitative analysis. Behav. Sleep Med. 2016, 14, 67–84. [Google Scholar] [CrossRef]
- Garbarino, S.; Bardwell, W.A.; Guglielmi, O.; Chiorri, C.; Bonanni, E.; Magnavita, N. Association of Anxiety and Depression in Obstructive Sleep Apnea Patients: A Systematic Review and Meta-Analysis. Behav. Sleep Med. 2020, 18, 35–57. [Google Scholar] [CrossRef]
- Bjorvatn, B.; Rajakulendren, N.; Lehmann, S.; Pallesen, S. Symptoms of anxiety and depression are related to sleep apnea severity in outpatients with suspected obstructive sleep apnea. Front. Psychol. 2015, 6, 1322. [Google Scholar]
- Chervin, R.D. Sleepiness, fatigue, tiredness, and lack of energy in obstructive sleep apnea. Chest 2000, 118, 372–379. [Google Scholar] [CrossRef]
- Yaggi, H.K.; Concato, J.; Kernan, W.N.; Lichtman, J.H.; Brass, L.M.; Mohsenin, V. Obstructive Sleep Apnea as a Risk Factor for Stroke and Death. N. Engl. J. Med. 2005, 353, 2034–2041. [Google Scholar] [CrossRef] [PubMed]
- Bjornsdottir, E.; Keenan, B.T.; Eysteinsdottir, B.; Arnardottir, E.S.; Janson, C.; Gislason, T.; Sigurdsson, J.F.; Kuna, S.T.; Pack, A.I.; Benediktsdottir, B. Quality of life among untreated sleep apnea patients compared with the general population and changes after treatment with positive airway pressure. J. Sleep Res. 2015, 24, 328–338. [Google Scholar] [CrossRef] [PubMed]
- Jordan, A.S.; McSharry, D.G.; Malhotra, A. Adult obstructive sleep apnoea. Lancet 2014, 383, 736–747. [Google Scholar] [CrossRef] [PubMed]
- Patel, S.R. Obstructive Sleep Apnea. Ann. Intern. Med. 2019, 171, ITC81–ITC96. [Google Scholar] [CrossRef]
- Kapur, V.K.; Auckley, D.H.; Chowdhuri, S.; Kuhlmann, D.C.; Mehra, R.; Ramar, K.; Harrod, C.G. Clinical practice guideline for diagnostic testing for adult obstructive sleep apnea. J. Clin. Sleep Med. 2017, 13, 479–504. [Google Scholar] [CrossRef]
- Punjabi, N.M. Sleep-disordered breathing: A major risk factor for hypertension and cardiovascular disease. Curr. Opin. Cardiol. 2020, 35, 598–603. [Google Scholar]
- Benjafield, A.V.; Najib, T.A.; Eastwood, P.R.; Heinzer, R.; Mary, S.M.I.; Morrell, M.J.; Nunez, C.M.; Patel, S.R.; Penzel, T.; Pépin, J.L.; et al. Estimation of the global prevalence and burden of obstructive sleep apnoea: A literature-based analysis. Lancet Respir. Med. 2019, 7, 687–698. [Google Scholar] [CrossRef]
- Weaver, T.E.; Grunstein, R.R. Adherence to continuous positive airway pressure therapy: The challenge to effective treatment of obstructive sleep apnea. Proc. Am. Thorac. Soc. 2021, 18, 80–90. [Google Scholar]
- Harding, S.M. Cpap-related aerophagia: Awareness first! J. Clin. Sleep Med. 2013, 9, 19–20. [Google Scholar] [CrossRef][Green Version]
- Heinzer, R.; Vat, S.; Marques-Vidal, P.; Marti-Soler, H.; Andries, D.; Tobback, N.; Mooser, V.; Preisig, M.; Malhotra, A.; Waeber, G.; et al. Prevalence of sleep-disordered breathing in the general population: The HypnoLaus study. Lancet Respir. Med. 2015, 3, 310–318. [Google Scholar] [CrossRef]
- Tsolakis, I.A.; Kolokitha, O.E. Comparing Airway Analysis in Two-Time Points after Rapid Palatal Expansion: A CBCT Study. J. Clin. Med. 2023, 12, 4686. [Google Scholar] [CrossRef] [PubMed]
- Tsolakis, I.A.; Palomo, J.M.; Matthaios, S.; Tsolakis, A.I. Dental and Skeletal Side Effects of Oral Appliances Used for the Treatment of Obstructive Sleep Apnea and Snoring in Adult Patients—A Systematic Review and Meta-Analysis. J. Pers. Med. 2022, 12, 483. [Google Scholar] [CrossRef] [PubMed]


| No | % | |
|---|---|---|
| Age | 56.54 ± 11.06 years old (minimum age 33 years old–maximum age 77 years old) | |
| Gender | ||
| Female | 11 | 39.3 |
| Male | 17 | 60.7 |
| Residence | ||
| Urban | 18 | 64.3 |
| Rural | 10 | 35.7 |
| Social status | ||
| Employed | 21 | 75.0 |
| Unemployed | 2 | 7.1 |
| Retiree | 5 | 17.9 |
| OSA severity | ||
| Severe obstructive sleep apnea | 15 | 53.6 |
| Moderate obstructive sleep apnea | 9 | 32.1 |
| Mild obstructive sleep apnea | 4 | 14.3 |
| AHI | ||
| AHI > 30/h | 15 | 53.6 |
| AHI 16–30/h | 9 | 32.1 |
| AHI < 15/h | 4 | 14.3 |
| BMI | ||
| Obese (>30 kg/m2) | 12 | 42.9 |
| Overweight (28–30 kg/m2) | 11 | 39.3 |
| Normal weight (<25 kg/m2) | 5 | 17.9 |
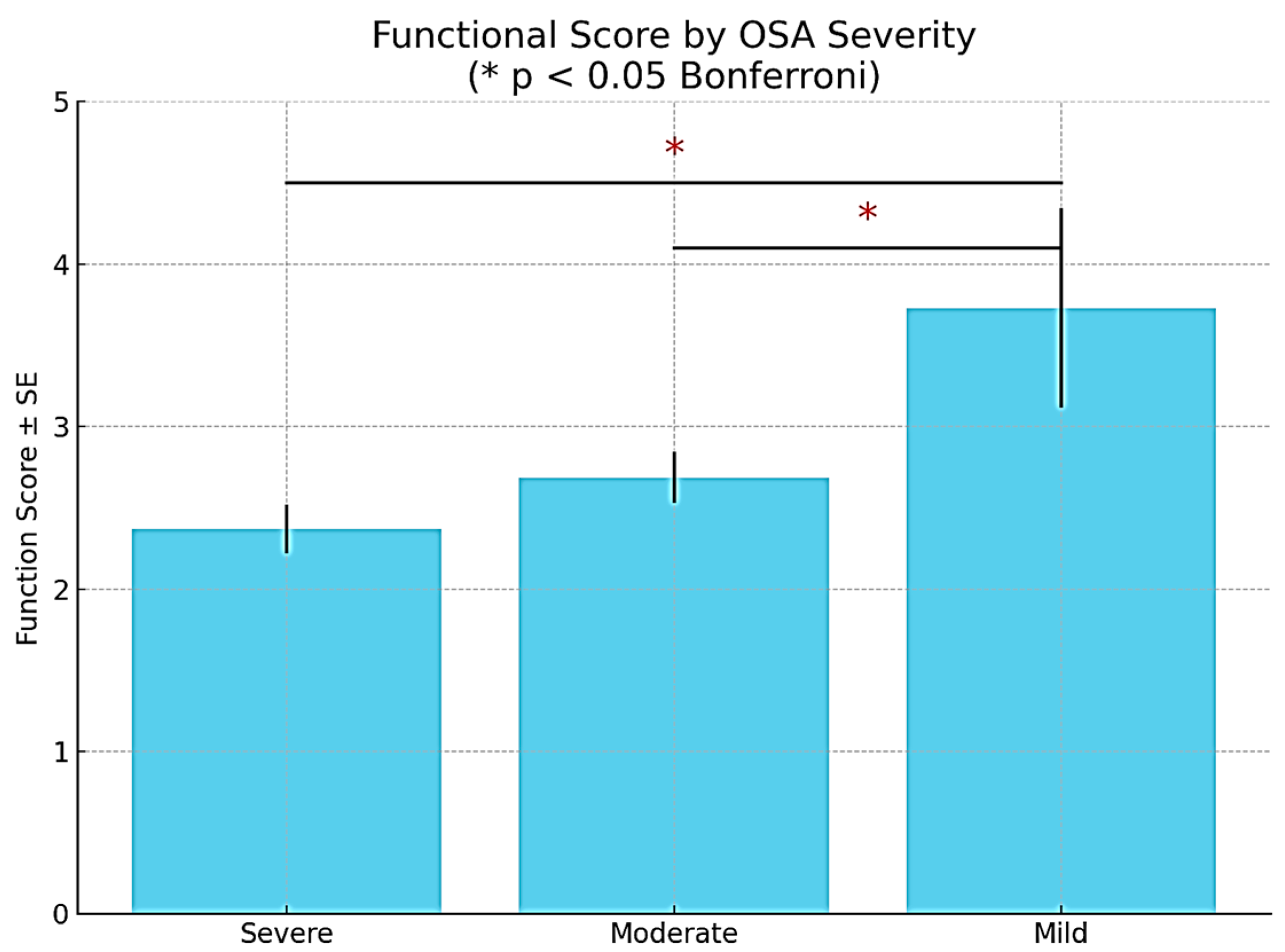
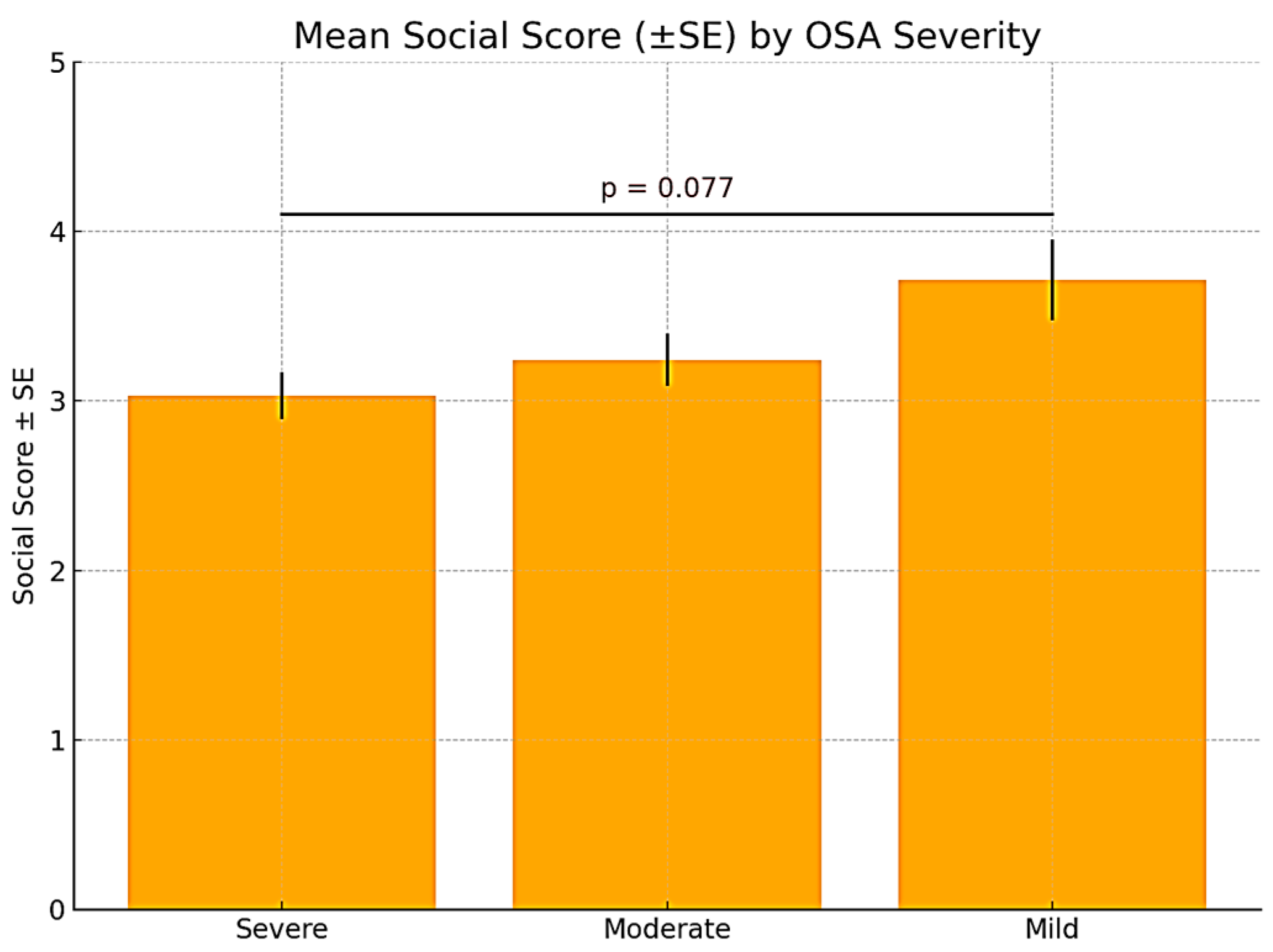
| Field | OSA Severity | Mean | Std. Deviation | Minimum | Maximum | F * | Sig. * |
|---|---|---|---|---|---|---|---|
| Functional | Severe OSA | 2.3700 | 0.58329 | 1.36 | 3.36 | 6.603 | 0.005 |
| Moderate OSA | 2.6867 | 0.47429 | 2.00 | 3.36 | |||
| Mild OSA | 3.7300 | 1.22553 | 2.55 | 5.00 | |||
| Social | Severe OSA | 3.0313 | 0.53954 | 2.23 | 3.77 | 2.866 | 0.076 |
| Moderate OSA | 3.2422 | 0.46711 | 2.62 | 3.85 | |||
| Mild OSA | 3.7125 | 0.48023 | 3.00 | 4.00 | |||
| Emotional Status | Severe OSA | 3.4380 | 0.43486 | 2.55 | 3.82 | 3.753 | 0.038 |
| Moderate OSA | 3.1933 | 0.92480 | 2.00 | 4.82 | |||
| Mild OSA | 4.2975 | 0.80946 | 3.09 | 4.82 | |||
| Symptoms | Severe OSA | 2.9887 | 0.79750 | 1.96 | 4.22 | 13.434 | 0.000 |
| Moderate OSA | 4.0744 | 0.69757 | 3.22 | 5.74 | |||
| Mild OSA | 5.0850 | 0.90850 | 3.74 | 5.74 |
| Model | Unstandardized Coefficients | Standardized Coefficients | t | Sig. | ||
|---|---|---|---|---|---|---|
| B | Std. Error | Beta | ||||
| Daily function domain (constant) | 1.052 | 0.284 | 3.703 | 0.001 | ||
| Sex | −0.408 | 0.223 | −0.256 | −1.827 | 0.081 | |
| Age | 1.056 | 0.271 | 0.557 | 3.901 | 0.001 | |
| AHI | 0.459 | 0.207 | 0.428 | 2.215 | 0.037 | |
| BMI | 0.168 | 0.196 | 0.159 | 0.855 | 0.401 | |
| Social interaction domain (constant) | 2.309 | 0.248 | 9.294 | 0.000 | ||
| Sex | 0.351 | 0.195 | 0.321 | 1.801 | 0.085 | |
| Age | 0.023 | 0.237 | 0.018 | 0.098 | 0.923 | |
| AHI | 0.197 | 0.181 | 0.266 | 1.085 | 0.289 | |
| BMI | 0.194 | 0.172 | 0.268 | 1.129 | 0.270 | |
| Emotional status domain (constant) | 2.541 | 0.385 | 6.606 | 0.000 | ||
| Sex | −0.318 | 0.302 | −0.213 | −1.053 | 0.303 | |
| Age | 0.486 | 0.366 | 0.273 | 1.326 | 0.198 | |
| AHI | 0.401 | 0.281 | 0.398 | 1.430 | 0.166 | |
| BMI | 0.062 | 0.266 | 0.062 | 0.231 | 0.819 | |
| Symptoms domain (constant) | 1.577 | 0.423 | 3.726 | 0.001 | ||
| Sex | 0.039 | 0.332 | 0.018 | 0.117 | 0.908 | |
| Age | 0.059 | 0.403 | 0.023 | 0.147 | 0.884 | |
| AHI | 0.368 | 0.309 | 0.250 | 1.191 | 0.246 | |
| BMI | 0.799 | 0.293 | 0.554 | 2.731 | 0.012 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Published by MDPI on behalf of the Lithuanian University of Health Sciences. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tanellari, O.; Koci, B.; Baruti Papa, E.; Balcos, C.; Armencia, A.O.; Panaite, T.; Zetu, I. Study on Quality of Life of Patients with Obstructive Sleep Apnea—Pilot Study. Medicina 2025, 61, 1234. https://doi.org/10.3390/medicina61071234
Tanellari O, Koci B, Baruti Papa E, Balcos C, Armencia AO, Panaite T, Zetu I. Study on Quality of Life of Patients with Obstructive Sleep Apnea—Pilot Study. Medicina. 2025; 61(7):1234. https://doi.org/10.3390/medicina61071234
Chicago/Turabian StyleTanellari, Olja, Brunilda Koci, Edlira Baruti Papa, Carina Balcos, Adina Oana Armencia, Tinela Panaite, and Irina Zetu. 2025. "Study on Quality of Life of Patients with Obstructive Sleep Apnea—Pilot Study" Medicina 61, no. 7: 1234. https://doi.org/10.3390/medicina61071234
APA StyleTanellari, O., Koci, B., Baruti Papa, E., Balcos, C., Armencia, A. O., Panaite, T., & Zetu, I. (2025). Study on Quality of Life of Patients with Obstructive Sleep Apnea—Pilot Study. Medicina, 61(7), 1234. https://doi.org/10.3390/medicina61071234










