Pre-Exercise Ingestion of Hydrogen-Rich Cold Water Enhances Endurance Performance and Lactate Response in Heat
Abstract
1. Introduction
2. Materials and Methods
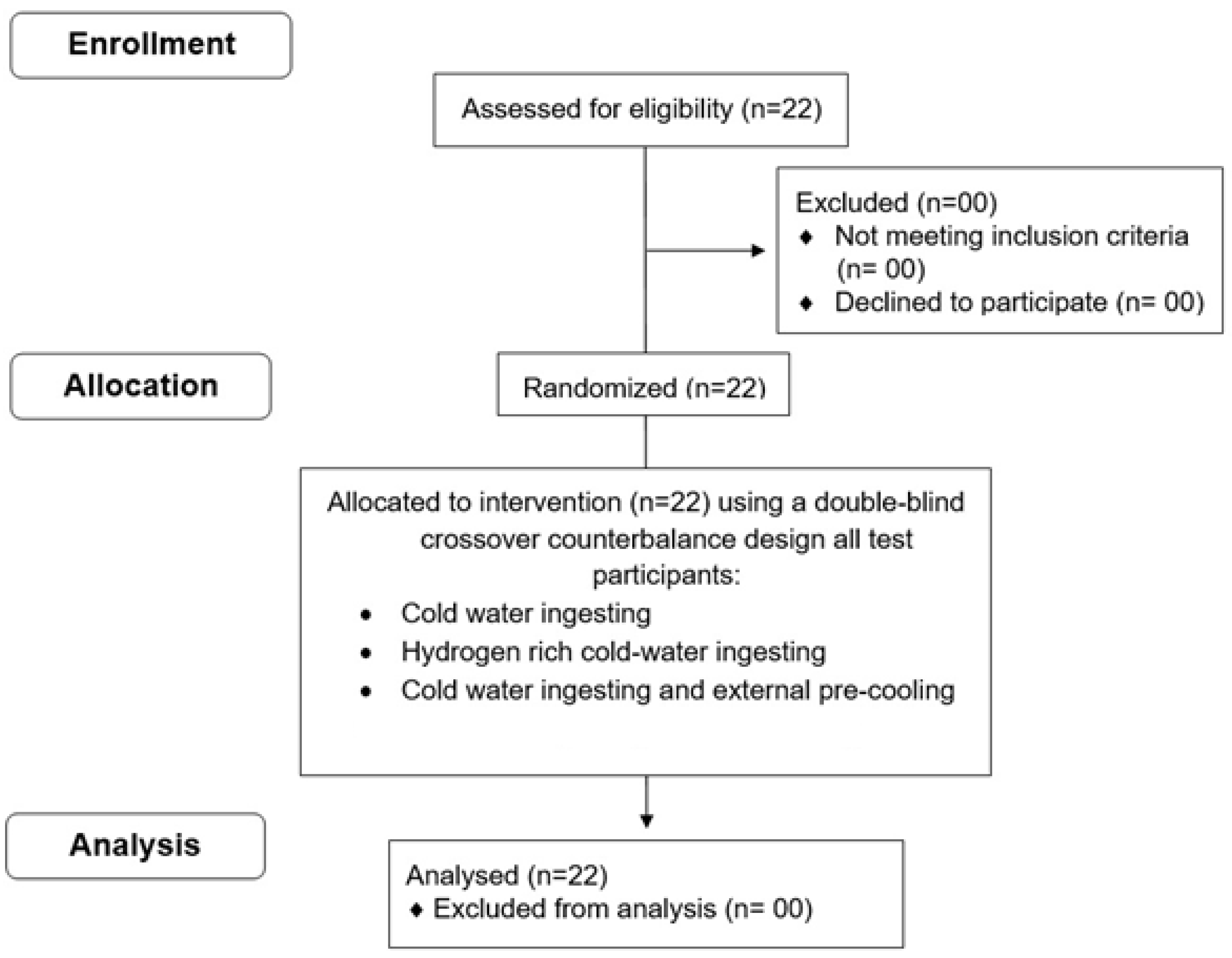
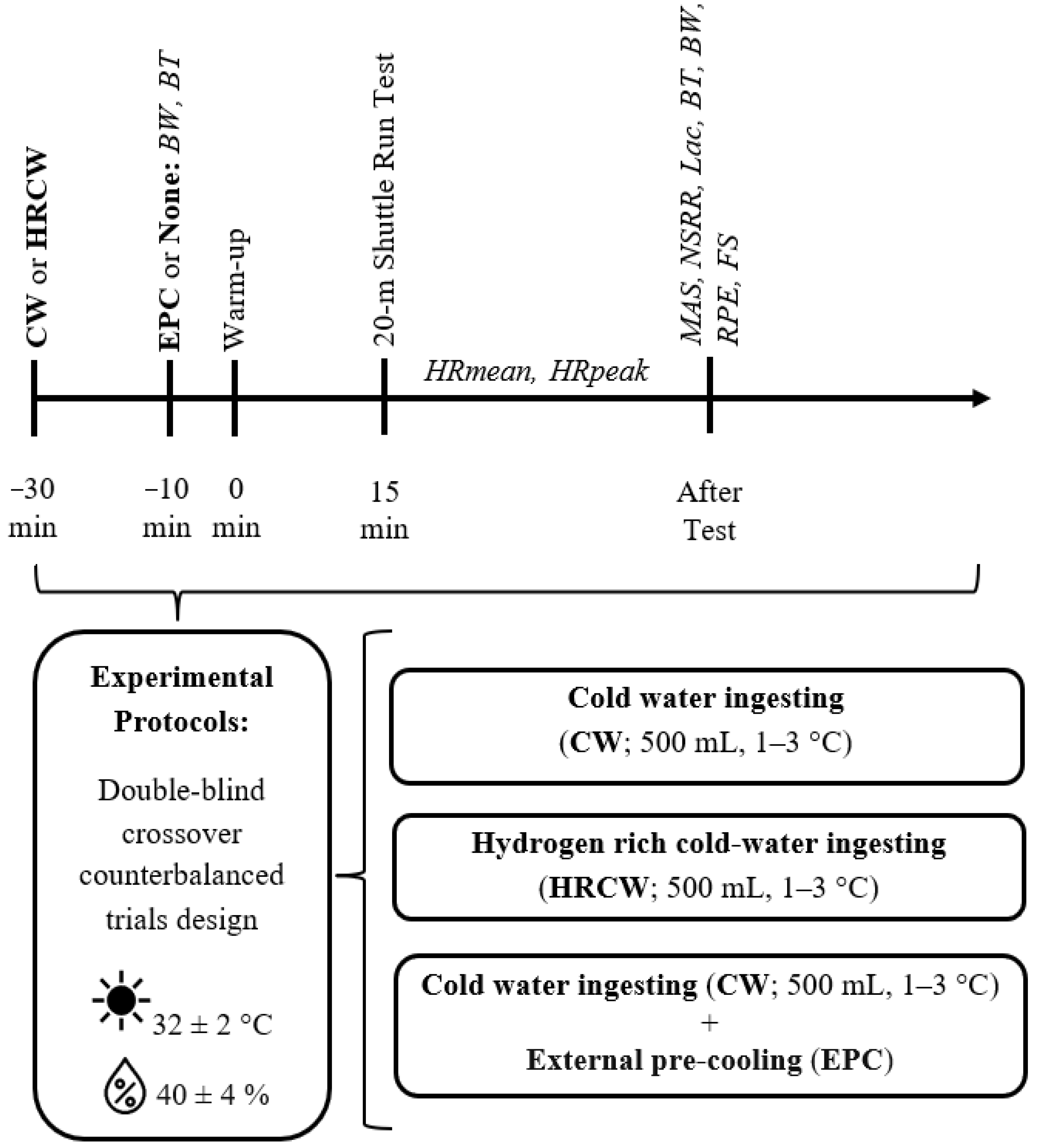
2.1. Study Design
2.2. Participant
2.3. Experimental Procedure
2.3.1. Protocols
Internal and External Pre-Cooling
Hydrogen-Rich Cold Water
2.3.2. Measurements
Anthropometric Measurements and Percentage of Dehydration
Shuttle Run Test
Infrared Tympanic Temperature and Ambient Temperature
Heart Rate and Bood Lactate
Feeling Scale
Rating of Perceived Exertion
2.4. Statistical Analysis
3. Results
3.1. Physical Performance and Heart Rate
3.2. Dehydration
3.3. Blood Lactate
3.4. RPE and Feeling Scale
3.5. Body Temperature
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Racinais, S.; Alonso, J.-M.; Coutts, A.J.; Flouris, A.D.; Girard, O.; González-Alonso, J.; Hausswirth, C.; Jay, O.; Lee, J.K.; Mitchell, N. Consensus recommendations on training and competing in the heat. Scand. J. Med. Sci. Sports 2015, 25, 6–19. [Google Scholar] [CrossRef] [PubMed]
- Gibson, O.R.; James, C.A.; Mee, J.A.; Willmott, A.G.; Turner, G.; Hayes, M.; Maxwell, N.S. Heat alleviation strategies for athletic performance: A review and practitioner guidelines. Temperature 2020, 7, 3–36. [Google Scholar] [CrossRef] [PubMed]
- Périard, J.D.; Racinais, S.; Sawka, M.N. Adaptations and mechanisms of human heat acclimation: Applications for competitive athletes and sports. Scand. J. Med. Sci. Sports 2015, 25, 20–38. [Google Scholar] [CrossRef]
- Bongers, C.C.; de Korte, J.Q.; Eijsvogels, T. Infographic. Keep it cool and beat the heat: Cooling strategies for exercise in hot and humid conditions. Br. J. Sports Med. 2021, 55, 643–644. [Google Scholar] [CrossRef]
- Nybo, L.; Rasmussen, P.; Sawka, M.N. Performance in the heat-physiological factors of importance for hyperthermia-induced fatigue. Compr. Physiol. 2014, 4, 657–689. [Google Scholar] [CrossRef] [PubMed]
- Tucker, R.; Rauch, L.; Harley, Y.X.; Noakes, T.D. Impaired exercise performance in the heat is associated with an anticipatory reduction in skeletal muscle recruitment. Pflügers Arch. 2004, 448, 422–430. [Google Scholar] [CrossRef]
- Flouris, A.; Schlader, Z. Human behavioral thermoregulation during exercise in the heat. Scand. J. Med. Sci. Sports 2015, 25, 52–64. [Google Scholar] [CrossRef]
- Périard, J.D.; Travers, G.J.; Racinais, S.; Sawka, M.N. Cardiovascular adaptations supporting human exercise-heat acclimation. Auton. Neurosci. Basic Clin. 2016, 196, 52–62. [Google Scholar] [CrossRef]
- Heydenreich, J.; Koehler, K.; Braun, H.; Grosshauser, M.; Heseker, H.; Koenig, D.; Lampen, A.; Mosler, S.; Niess, A.; Schek, A. Effects of internal cooling on physical performance, physiological and perceptional parameters when exercising in the heat: A systematic review with meta-analyses. Front. Physiol. 2023, 14, 1125969. [Google Scholar] [CrossRef]
- Hohenauer, E.; Stoop, R.; Clarys, P.; Clijsen, R.; Deliens, T.; Taeymans, J. The effect of pre-exercise cooling on performance characteristics: A systematic review and meta-analysis. Int. J. Clin. Med. 2018, 9, 117–141. [Google Scholar] [CrossRef]
- Ihsan, M.; Landers, G.; Brearley, M.; Peeling, P. Beneficial effects of ice ingestion as a precooling strategy on 40-km cycling time-trial performance. Int. J. Sports Physiol. Perform. 2010, 5, 140–151. [Google Scholar] [CrossRef] [PubMed]
- Ross, M.; Abbiss, C.; Laursen, P.; Martin, D.; Burke, L. Precooling methods and their effects on athletic performance: A systematic review and practical applications. Sports Med. 2013, 43, 207–225. [Google Scholar] [CrossRef] [PubMed]
- Rodríguez, M.Á.; Piedra, J.V.; Sánchez-Fernández, M.; Del Valle, M.; Crespo, I.; Olmedillas, H. A matter of degrees: A systematic review of the ergogenic effect of pre-cooling in highly trained athletes. Int. J. Environ. Res. Public Health 2020, 17, 2952. [Google Scholar] [CrossRef] [PubMed]
- Naito, T.; Iribe, Y.; Ogaki, T. Ice ingestion with a long rest interval increases the endurance exercise capacity and reduces the core temperature in the heat. J. Physiol. Anthropol. 2017, 36, 9. [Google Scholar] [CrossRef]
- Roriz, M.; Brito, P.; Teixeira, F.J.; Brito, J.; Teixeira, V.H. Performance effects of internal pre-and per-cooling across different exercise and environmental conditions: A systematic review. Front. Nutr. 2022, 9, 959516. [Google Scholar] [CrossRef]
- Xu, M.; Wu, Z.; Dong, Y.; Qu, C.; Xu, Y.; Qin, F.; Wang, Z.; Nassis, G.P.; Zhao, J. A mixed-method approach of pre-cooling enhances high-intensity running performance in the heat. J. Sports Sci. Med. 2021, 20, 26. [Google Scholar] [CrossRef]
- Zhou, Q.; Li, H.; Zhang, Y.; Zhao, Y.; Wang, C.; Liu, C. Hydrogen-Rich Water to Enhance Exercise Performance: A Review of Effects and Mechanisms. Metabolites 2024, 14, 537. [Google Scholar] [CrossRef]
- Ostojic, S.M. Hydrogen-rich water as a modulator of gut microbiota? J. Funct. Foods 2021, 78, 104360. [Google Scholar] [CrossRef]
- Dohi, K.; Satoh, K.; Miyamoto, K.; Momma, S.; Fukuda, K.; Higuchi, R.; Ohtaki, H.; Banks, W.A. Molecular hydrogen in the treatment of acute and chronic neurological conditions: Mechanisms of protection and routes of administration. J. Clin. Biochem. Nutr. 2017, 61, 1–5. [Google Scholar] [CrossRef]
- Ohta, S. Recent progress toward hydrogen medicine: Potential of molecular hydrogen for preventive and therapeutic applications. Curr. Pharm. Des. 2011, 17, 2241–2252. [Google Scholar] [CrossRef]
- Jebabli, N.; Ouerghi, N.; Abassi, W.; Yagin, F.H.; Khlifi, M.; Boujabli, M.; Bouassida, A.; Ben Abderrahman, A.; Ardigò, L.P. Acute effect of hydrogen-rich water on physical, perceptual and cardiac responses during aerobic and anaerobic exercises: A randomized, placebo-controlled, double-blinded cross-over trial. Front. Physiol. 2023, 14, 1240871. [Google Scholar] [CrossRef]
- Da Ponte, A.; Giovanelli, N.; Nigris, D.; Lazzer, S. Effects of hydrogen rich water on prolonged intermittent exercise. J. Sports Med. Phys. Fit. 2018, 58, 612–621. [Google Scholar] [CrossRef] [PubMed]
- Aoki, K.; Nakao, A.; Adachi, T.; Matsui, Y.; Miyakawa, S. Pilot study: Effects of drinking hydrogen-rich water on muscle fatigue caused by acute exercise in elite athletes. Med. Gas Res. 2012, 2, 12. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.; Shen, L.; Zhang, Y.; Shen, B. Circadian rhythm and personalized exercise. In Translational Informatics: Sports and Exercise Medicine; Springer: Berlin/Heidelberg, Germany, 2022; pp. 99–122. [Google Scholar]
- Byrne, P.; Miriel, J.; Lenat, Y. Experimental study of an air-source heat pump for simultaneous heating and cooling–part 2: Dynamic behaviour and two-phase thermosiphon defrosting technique. Appl. Energy 2011, 88, 3072–3078. [Google Scholar] [CrossRef]
- Lamarche, D.T.; Meade, R.D.; Mcginn, R.; Poirier, M.P.; Friesen, B.J.; Kenny, G.P. Temperature of ingested water during exercise does not affect body heat storage. Med. Sci. Sports Exerc. 2015, 47, 1272–1280. [Google Scholar] [CrossRef] [PubMed]
- Valenta, M.; Botek, M.; Krejčí, J.; McKune, A.; Sládečková, B.; Neuls, F.; Bajgar, R.; Klimešová, I. Acute pre-exercise hydrogen rich water intake does not improve running performance at maximal aerobic speed in trained track and field runners: A randomized, double-blind, placebo-controlled crossover study. PLoS ONE 2022, 17, e0279307. [Google Scholar] [CrossRef]
- Botek, M.; Sládečková, B.; Krejčí, J.; Pluháček, F.; Najmanová, E. Acute hydrogen-rich water ingestion stimulates cardiac autonomic activity in healthy females. Acta Gymnica 2021, 51, e2021.009. [Google Scholar] [CrossRef]
- Timón, R.; Olcina, G.; González-Custodio, A.; Camacho-Cardenosa, M.; Camacho-Cardenosa, A.; Guardado, I. Effects of 7-day intake of hydrogen-rich water on physical performance of trained and untrained subjects. Biol. Sport 2021, 38, 269–275. [Google Scholar] [CrossRef]
- Harvey, G.; Meir, R.; Brooks, L.; Holloway, K. The use of body mass changes as a practical measure of dehydration in team sports. J. Sci. Med. Sport 2008, 11, 600–603. [Google Scholar] [CrossRef]
- Leger, L.A.; Mercier, D.; Gadoury, C.; Lambert, J. The multistage 20 metre shuttle run test for aerobic fitness. J. Sports Sci. 1988, 6, 93–101. [Google Scholar] [CrossRef]
- Morán-Navarro, R.; Courel-Ibáñez, J.; Martínez-Cava, A.; Conesa-Ros, E.; Sánchez-Pay, A.; Mora-Rodriguez, R.; Pallarés, J.G. Validity of skin, oral and tympanic temperatures during exercise in the heat: Effects of wind and sweat. Ann. Biomed. Eng. 2019, 47, 317–331. [Google Scholar] [CrossRef] [PubMed]
- Chen, H.-Y.; Chen, A.; Chen, C. Investigation of the impact of infrared sensors on core body temperature monitoring by comparing measurement sites. Sensors 2020, 20, 2885. [Google Scholar] [CrossRef]
- Hardy, C.J.; Rejeski, W.J. Not what, but how one feels: The measurement of affect during exercise. J. Sport Exerc. Psychol. 1989, 11, 304–317. [Google Scholar] [CrossRef]
- Borg, G.A. Psychophysical bases of perceived exertion. Med. Sci. Sports Exerc. 1982, 14, 377–381. [Google Scholar] [CrossRef]
- Koo, T.K.; Li, M.Y. A guideline of selecting and reporting intraclass correlation coefficients for reliability research. J. Chiropr. Med. 2016, 15, 155–163. [Google Scholar] [CrossRef]
- Richardson, J.T. Eta squared and partial eta squared as measures of effect size in educational research. Educ. Res. Rev. 2011, 6, 135–147. [Google Scholar] [CrossRef]
- Cohen, J. Statistical Power Analysis for the Behavioral Sciences; Routledge: New York, NY, USA, 2013. [Google Scholar]
- Hopkins, W.G.; Marshall, S.W.; Quarrie, K.L.; Hume, P.A. Risk factors and risk statistics for sports injuries. Clin. J. Sport Med. 2007, 17, 208–210. [Google Scholar] [PubMed]
- Mikami, T.; Tano, K.; Lee, H.; Lee, H.; Park, J.; Ohta, F.; LeBaron, T.W.; Ohta, S. Drinking hydrogen water enhances endurance and relieves psychometric fatigue: A randomized, double-blind, placebo-controlled study. Can. J. Physiol. Pharmacol. 2019, 97, 857–862. [Google Scholar] [CrossRef]
- Alharbi, A.A.D.; Ebine, N.; Nakae, S.; Hojo, T.; Fukuoka, Y. Application of molecular hydrogen as an antioxidant in responses to ventilatory and ergogenic adjustments during incremental exercise in humans. Nutrients 2021, 13, 459. [Google Scholar] [CrossRef]
- Nogueira, J.E.; Amorim, M.R.; Pinto, A.P.; da Rocha, A.L.; da Silva, A.S.; Branco, L.G. Molecular hydrogen downregulates acute exhaustive exercise-induced skeletal muscle damage. Can. J. Physiol. Pharmacol. 2021, 99, 812–820. [Google Scholar] [CrossRef]
- Yoshimura, M.; Nakamura, M.; Kasahara, K.; Yoshida, R.; Murakami, Y.; Hojo, T.; Inoue, G.; Makihira, N.; Fukuoka, Y. Effect of CO2 and H2 gas mixture in cold water immersion on recovery after eccentric loading. Heliyon 2023, 9, e20288. [Google Scholar] [CrossRef] [PubMed]
- Slezák, J.; Kura, B.; Frimmel, K.; Zálešák, M.; Ravingerová, T.; Viczenczová, C.; Okruhlicova, L.; Tribulová, N. Preventive and therapeutic application of molecular hydrogen in situations with excessive production of free radicals. Physiol. Res. 2016, 65, S11–S28. [Google Scholar] [CrossRef] [PubMed]
- LeBaron, T.W.; Kura, B.; Kalocayova, B.; Tribulova, N.; Slezak, J. A new approach for the prevention and treatment of cardiovascular disorders. Molecular hydrogen significantly reduces the effects of oxidative stress. Molecules 2019, 24, 2076. [Google Scholar] [CrossRef]
- Jay, O.; Morris, N.B. Does cold water or ice slurry ingestion during exercise elicit a net body cooling effect in the heat? Sports Med. 2018, 48, 17–29. [Google Scholar] [CrossRef]
- Schmit, C.; Hausswirth, C.; Le Meur, Y.; Duffield, R. Cognitive functioning and heat strain: Performance responses and protective strategies. Sports Med. 2017, 47, 1289–1302. [Google Scholar] [CrossRef] [PubMed]
- Tyler, C.J.; Sunderland, C.; Cheung, S.S. The effect of cooling prior to and during exercise on exercise performance and capacity in the heat: A meta-analysis. Br. J. Sports Med. 2015, 49, 7–13. [Google Scholar] [CrossRef]
- Siegel, R.; Laursen, P.B. Keeping your cool: Possible mechanisms for enhanced exercise performance in the heat with internal cooling methods. Sports Med. 2012, 42, 89–98. [Google Scholar] [CrossRef]
- Moss, J.N.; Trangmar, S.J.; Mackenzie, R.W.; Tyler, C.J. The effects of pre-and per-cooling interventions used in isolation and combination on subsequent 15-minute time-trial cycling performance in the heat. J. Sci. Med. Sport 2021, 24, 800–805. [Google Scholar] [CrossRef]
- Rinaldi, C.; Landre, C.B.; Volpe, M.I.; Gonçalves, R.G.; Nunes, L.d.S.; Darienso, D.; Cruz, A.V.; Oliveira, J.D.; Rinaldi, S.; Fontani, V. Improving functional capacity and quality of life in parkinson’s disease patients through reac neuromodulation treatments for mood and behavioral disorders. J. Pers. Med. 2023, 13, 937. [Google Scholar] [CrossRef]
- Rollo, I.; Williams, C.; Gant, N.; Nute, M. The influence of carbohydrate mouth rinse on self-selected speeds during a 30-min treadmill run. Int. J. Sport Nutr. Exerc. Metab. 2008, 18, 585–600. [Google Scholar] [CrossRef]
- Yanovich, R.; Ketko, I.; Charkoudian, N. Sex differences in human thermoregulation: Relevance for 2020 and beyond. Physiology 2020, 35, 177–184. [Google Scholar] [CrossRef] [PubMed]

| Participants | N | Age (Years) | Body Weight (kg) | Body Height (m) | BMI (kg.m−2) | Training (h wk−1) |
|---|---|---|---|---|---|---|
| Male sports science students | 22 | 19.32 ± 0.84 | 59.82 ± 10.41 | 1.70 ± 0.11 | 20.59 ± 1.98 | 16 |
| Control | HRCW | IEPC | p | η2p | Power | |
|---|---|---|---|---|---|---|
| MAS (Km/h) | 12.24 ± 1.80 | 12.83 ± 1.78 ǂ | 12.71 ± 1.83 | 0.009 | 0.464 | 0.857 |
| Number of shuttle run repetitions | 91.62 ± 45.19 | 110.29 ± 48.49 ǂ | 104 ± 47.95 | 0.004 | 0.447 | 0.908 |
| HRmean (beat/min) | 168.90 ± 10.20 | 167.89 ± 10.38 | 165.91 ± 10.03 | 0.716 | 0.071 | 0.124 |
| HRpeak (beat/min) | 181.29 ± 9.65 | 181.38 ± 8.48 | 180.48 ± 7.19 | 0.222 | 0.211 | 0.351 |
| Dehydration (%) | −0.27 ± 0.27 | −0.44 ± 0.26 ǂ | −0.44 ± 0.19 * | 0.016 | 0.429 | 0.799 |
| Lac.post.test (mmol/L) | 10.62 ± 0.82 | 9.98 ± 0.76 ǂ | 10.01 ± 0.73 * | <0.001 | 0.771 | 1 |
| RPEpost-test (AU) | 9.67 ± 0.48 | 9.38 ± 0.50 ǂ | 9.19 ± 0.60 * | 0.036 | 0.370 | 0.685 |
| FSpost-test (AU) | 1.14 ± 1.56 | 2.38 ± 0.80 ǂ | 2.24 ± 1.04 * | 0.014 | 0.439 | 0.816 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Published by MDPI on behalf of the Lithuanian University of Health Sciences. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Khlifi, M.; Jebabli, N.; Ouerghi, N.; Yagin, F.H.; Dutta, A.K.; Alwhaibi, R.; Bouassida, A. Pre-Exercise Ingestion of Hydrogen-Rich Cold Water Enhances Endurance Performance and Lactate Response in Heat. Medicina 2025, 61, 1173. https://doi.org/10.3390/medicina61071173
Khlifi M, Jebabli N, Ouerghi N, Yagin FH, Dutta AK, Alwhaibi R, Bouassida A. Pre-Exercise Ingestion of Hydrogen-Rich Cold Water Enhances Endurance Performance and Lactate Response in Heat. Medicina. 2025; 61(7):1173. https://doi.org/10.3390/medicina61071173
Chicago/Turabian StyleKhlifi, Mariem, Nidhal Jebabli, Nejmeddine Ouerghi, Fatma Hilal Yagin, Ashit Kumar Dutta, Reem Alwhaibi, and Anissa Bouassida. 2025. "Pre-Exercise Ingestion of Hydrogen-Rich Cold Water Enhances Endurance Performance and Lactate Response in Heat" Medicina 61, no. 7: 1173. https://doi.org/10.3390/medicina61071173
APA StyleKhlifi, M., Jebabli, N., Ouerghi, N., Yagin, F. H., Dutta, A. K., Alwhaibi, R., & Bouassida, A. (2025). Pre-Exercise Ingestion of Hydrogen-Rich Cold Water Enhances Endurance Performance and Lactate Response in Heat. Medicina, 61(7), 1173. https://doi.org/10.3390/medicina61071173









