An Evaluation of Turkish Dentists’ Approach to Indirect Pulp Capping and Material Preferences: A Questionnaire-Based Survey
Abstract
1. Introduction
2. Materials and Methods
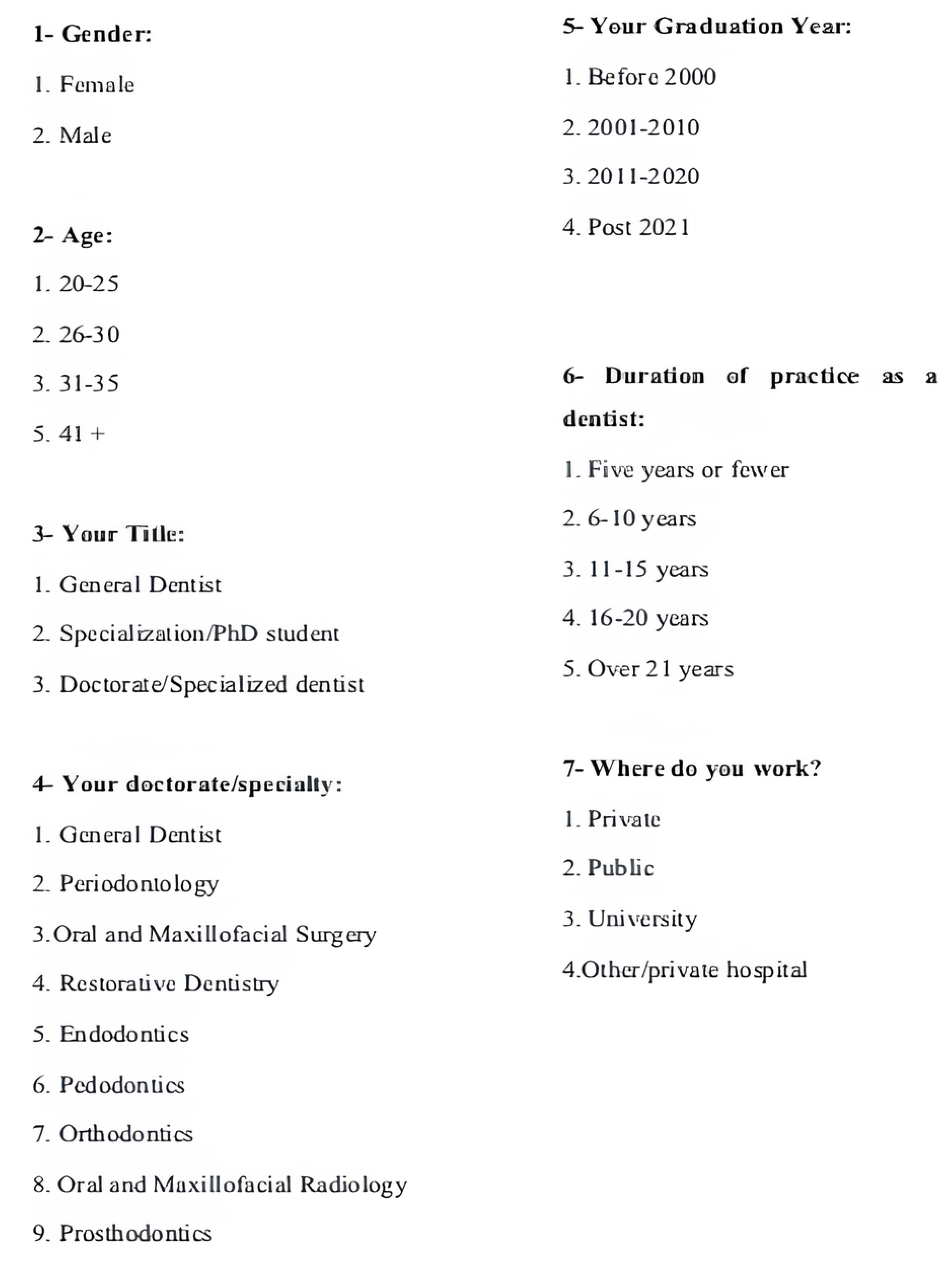
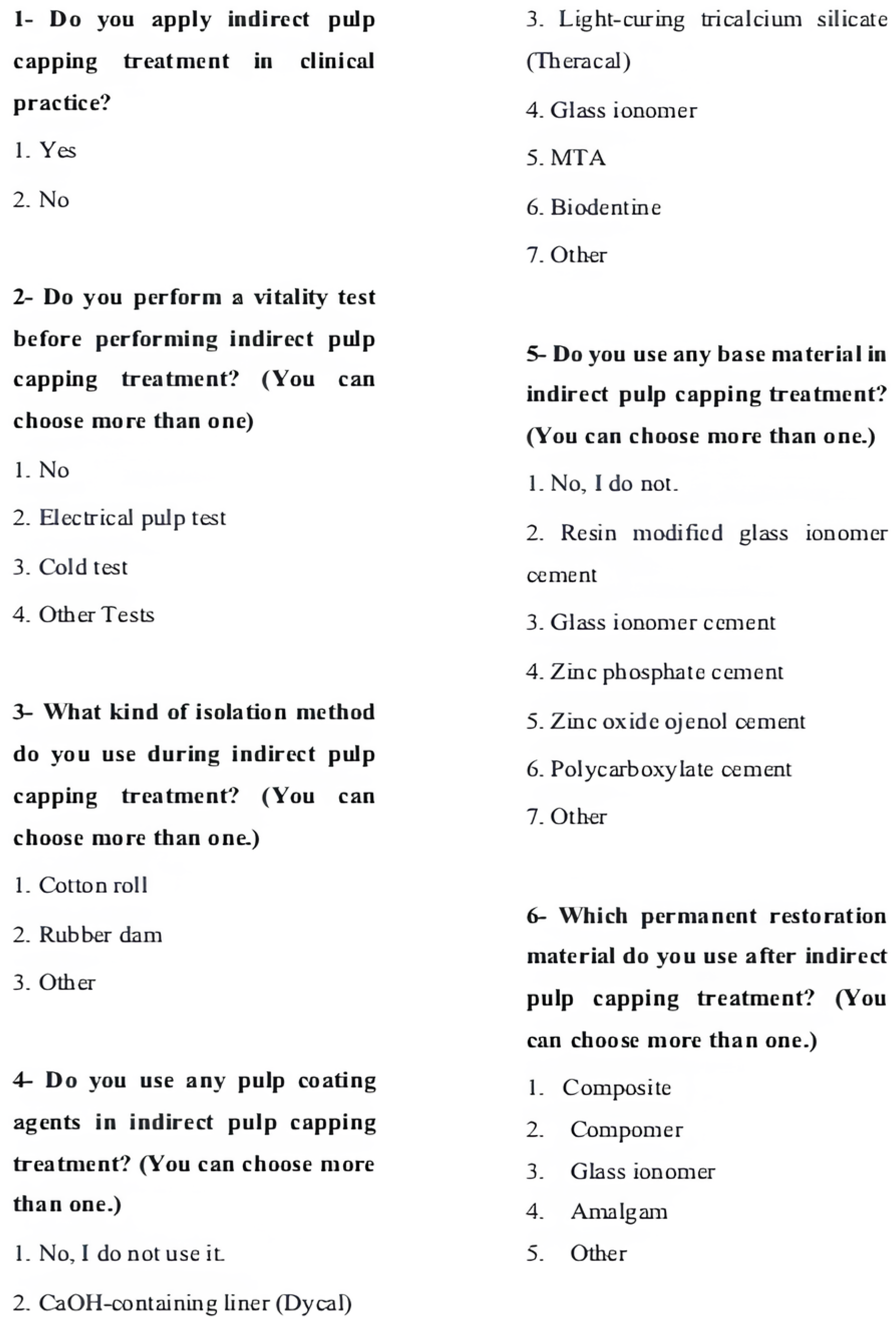
2.1. The Survey
2.2. Inclusion Criteria
2.3. Exclusion Criteria
2.4. The Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Kunert, M.; Lukomska-Szymanska, M. Bio-Inductive Materials in Direct and Indirect Pulp Capping-A Review Article. Materials 2020, 13, 1204. [Google Scholar] [CrossRef] [PubMed]
- Tong, H.J.; Seremidi, K.; Stratigaki, E.; Kloukos, D.; Duggal, M.; Gizani, S. Deep dentine caries management of immature permanent posterior teeth with vital pulp: A systematic review and meta-analysis. J. Dent. 2022, 124, 104214. [Google Scholar] [CrossRef]
- Sahin, N.; Saygili, S.; Akcay, M. Clinical, radiographic, and histological evaluation of three different pulp-capping materials in indirect pulp treatment of primary teeth: A randomized clinical trial. Clin. Oral Investig. 2021, 25, 3945–3955. [Google Scholar] [CrossRef] [PubMed]
- Hamama, H.; Yiu, C.; Burrow, M. Current update of chemomechanical caries removal methods. Aust. Dent. J. 2014, 59, 446–456. [Google Scholar] [CrossRef]
- Duncan, H.F. Present status and future directions-Vital pulp treatment and pulp preservation strategies. Int. Endod. J. 2022, 55 (Suppl. 3), 497–511. [Google Scholar] [CrossRef]
- Sruthi, M.A.; Subramanian, E.; Ravindran, V. Dentists’ preference of pulp capping agent for indirect pulp capping in primary and permanent molars-an observational study. Indian J. Forensic Med. Toxicol. 2020, 14, 5601–5610. [Google Scholar]
- Tucker, R.L.; Ha, W.N. A Systematic Review Comparing Mineral Trioxide Aggregate to Other Commercially Available Direct Pulp Capping Agents in Dogs. J. Vet. Dent. 2021, 38, 34–45. [Google Scholar] [CrossRef]
- Davaie, S.; Hooshmand, T.; Ansarifard, S. Different types of bioceramics as dental pulp capping materials: A systematic review. Ceram. Int. 2021, 47, 20781–20792. [Google Scholar] [CrossRef]
- Arandi, N.Z.; Thabet, M. Minimal Intervention in Dentistry: A Literature Review on Biodentine as a Bioactive Pulp Capping Material. Biomed. Res. Int. 2021, 2021, 5569313. [Google Scholar] [CrossRef]
- Alzraikat, H.; Taha, N.A.; Qasrawi, D.; Burrow, M.F. Shear bond strength of a novel light cured calcium silicate based-cement to resin composite using different adhesive systems. Dent. Mater. J. 2016, 35, 881–887. [Google Scholar] [CrossRef]
- Alovisi, M.; Baldi, A.; Comba, A.; Gamerro, R.; Paolone, G.; Mandurino, M.; Dioguardi, M.; Roggia, A.; Scotti, N. Long-Term Evaluation of Pulp Vitality Preservation in Direct and Indirect Pulp Capping: A Retrospective Clinical Study. J. Clin. Med. 2024, 13, 3962. [Google Scholar] [CrossRef] [PubMed]
- Öz, E.; Kırzıoğlu, Z. Mezuniyet Sonrasi Diş Hekimlerinin Pedodontik Tedavilere Yaklaşimlari. Balıkesir Sağlık Bilimleri Dergisi 2018, 7, 23–33. [Google Scholar]
- Chisini, L.A.; Conde, M.C.; Correa, M.B.; Dantas, R.V.; Silva, A.F.; Pappen, F.G.; Demarco, F.F. Vital Pulp Therapies in Clinical Practice: Findings from a Survey with Dentist in Southern Brazil. Braz. Dent. J. 2015, 26, 566–571. [Google Scholar] [CrossRef] [PubMed]
- Yi, J.K.; Kim, A.N.; Kwon, K.H. Evaluation of the reasons for preferring root canal treatment in mature permanent teeth potentially indicated for pulp preservation: A clinical case/photo-based questionnaire study. BMC Oral Health 2023, 23, 1003. [Google Scholar] [CrossRef]
- Li, M.; Hu, X.; Li, X.; Lei, S.; Cai, M.; Wei, X.; Deng, D. Dentist-related factors influencing the use of vital pulp therapy: A survey among dental practitioners in China. J. Int. Med. Res. 2019, 47, 2381–2393. [Google Scholar] [CrossRef]
- Alfaisal, Y.; Idris, G.; Peters, O.A.; Zafar, S.; Nagendrababu, V.; Peters, C.I. Vital pulp therapy-Factors influencing decision-making for permanent mature teeth with irreversible pulpitis: A systematic review. Int. Endod. J. 2024, 57, 505–519. [Google Scholar] [CrossRef]
- Igna, A.; Mircioagă, D.; Boariu, M.; Stratul, Ș.I. A Diagnostic Insight of Dental Pulp Testing Methods in Pediatric Dentistry. Medicina 2022, 58, 665. [Google Scholar] [CrossRef]
- Edwards, D.; Bailey, O.; Stone, S.; Duncan, H. The management of deep caries in UK primary care: A nationwide questionnaire-based study. Int. Endod. J. 2021, 54, 1804–1818. [Google Scholar] [CrossRef]
- Madarati, A.A. Why dentists don’t use rubber dam during endodontics and how to promote its usage? BMC Oral Health 2016, 16, 24. [Google Scholar] [CrossRef]
- Abuzenada, B.M. Attitude of Dental Students towards the Rubber Dam Use in Operative Dentistry. J. Pharm. Bioallied Sci. 2021, 13 (Suppl. 1), S637–S641. [Google Scholar] [CrossRef]
- Akgül, N.; Yilmaz, E.; Akkurt, O.; Yenidünya, Ö.G. Turkish dentist practice and opinions on diagnosing and treating deep caries lesions: A web-based survey. BMC Oral Health 2025, 25, 200. [Google Scholar] [CrossRef] [PubMed]
- Vadhera, N.; Makkar, S.; Kumar, R.; Aggarwal, A.; Pasricha, S. Practice profile among endodontists in India: A nationwide questionnaire survey. Indian. J. Oral Sci. 2012, 3, 90. [Google Scholar] [CrossRef]
- Zou, H.; Li, Y.; Lian, X.; Yan, Y.; Dai, X.; Wang, G. Frequency and Influencing Factors of Rubber Dam Usage in Tianjin: A Questionnaire Survey. Int. J. Dent. 2016, 2016, 7383212. [Google Scholar] [CrossRef]
- Palmer, N.O.; Ahmed, M.; Grieveson, B. An investigation of current endodontic practice and training needs in primary care in the north west of England. Br. Dent. J. 2009, 206, E22, discussion 584–585. [Google Scholar] [CrossRef][Green Version]
- Chin, J.S.; Thomas, M.B.; Locke, M.; Dummer, P.M. A survey of dental practitioners in Wales to evaluate the management of deep carious lesions with vital pulp therapy in permanent teeth. Br. Dent. J. 2016, 221, 331–338. [Google Scholar] [CrossRef]
- Monteiro, J.; Ní Chaollaí, A.; Duggal, M. The teaching of management of the pulp in primary molars across Europe. Eur. Arch. Paediatr. Dent. 2017, 18, 203–208. [Google Scholar] [CrossRef]
- Alzahrani, A.Y.; Al Tuwirqi, A.A.; Bamashmous, N.O.; Bakhsh, T.A.; El Ashiry, E.A. Non-Destructive In Vitro Evaluation of an Internal Adaptation of Recent Pulp-Capping Materials in Permanent Teeth Using OCT and Micro-CT. Children 2023, 10, 1318. [Google Scholar] [CrossRef]
- Laurent, P.; Camps, J.; De Méo, M.; Déjou, J.; About, I. Induction of specific cell responses to a Ca3SiO5-based posterior restorative material. Dent. Mater. 2008, 24, 1486–1494. [Google Scholar] [CrossRef] [PubMed]
- Luo, Z.; Li, D.; Kohli, M.R.; Yu, Q.; Kim, S.; He, W.X. Effect of Biodentine™ on the proliferation, migration and adhesion of human dental pulp stem cells. J. Dent. 2014, 42, 490–497. [Google Scholar] [CrossRef]
- Lakhotia, R.; Urs, P.; Jenny, A.; Raghunath, V.N.; Nagar, P.; Ninawe, N. Survey on Primary and Young Permanent Tooth Pulp Therapy as Practiced by Pediatric Dentists in Karnataka. Dent. J. Adv. Stud. 2022, 10, 032–037. [Google Scholar] [CrossRef]
- Sidhu, S.K.; Watson, T.F. Resin-modified glass ionomer materials. A status report for the American Journal of Dentistry. Am. J. Dent. 1995, 8, 59–67. [Google Scholar] [PubMed]
- Elmacı, İ.; Tunçdemir, M.T. Restoratif Diş Hekimliğinde Cam Iyonomer Simanlar ve Yeni Gelişmeler. Necmettin Erbakan Üniv. Diş Hekimliği Dergisi 2020, 2, 69–75. [Google Scholar]
- Mohanty, D.; Miglani, D.; Patro, D. Vital Pulp Ther Apy: A Literature Review Of The Material Aspect. Eur. J. Mol. Clin. Med. 2021, 7, 849–856. [Google Scholar]
- Pinto, K.T.; Stanislawczuk, R.; Loguercio, A.D.; Grande, R.H.M.; Bauer, J. Effect of exposure time of zinc oxide eugenol restoration on microtensile bond strength of adhesives to dentin. Rev. Port. Estomatol. Med. Dent. Cir. Maxilofac. 2014, 55, 83–88. [Google Scholar] [CrossRef]
- Drachev, S.N.; Galieva, A.S.; Yushmanova, T.N.; Polivanaya, E.A.; Stangvaltaite-Mouhat, L.; Al-Mahdi, R.; Leinonen, J.; Stein, L.M.; Davidova, N.G.; Al-Haroni, M. Restorative treatment decisions for carious lesions: Do Russian dentists and dental students apply minimal intervention dentistry? BMC Oral Health 2021, 21, 638. [Google Scholar] [CrossRef] [PubMed]
- Alkhudhairy, F. Attitudes of dentists and interns in Riyadh to the use of dental amalgam. BMC Res. Notes 2016, 9, 488. [Google Scholar] [CrossRef]
- Zabrovsky, A.; Mahmoud, R.; Beyth, N.; Ben-Gal, G. Direct Posterior Restorations: A 13-Year Survey of Teaching Trends and Use of Materials. Oper. Dent. 2018, 43, E273–E279. [Google Scholar] [CrossRef]
| Do You Use Indirect Pulp Capping in Clinical Practice? | p | |||
|---|---|---|---|---|
| Yes | No | |||
| n (%) | n (%) | |||
| Gender | Female | 227 (85.3) | 39 (14.7) | 0.027 |
| Male | 104 (76.5) | 32 (23.5) | ||
| Age | 20–25 | 72 (83.7) | 14 (16.3) | 0.211 |
| 26–30 | 172 (82.3) | 37 (17.7) | ||
| 31–35 | 51 (89.5) | 6 (10.5) | ||
| 36–40 | 14 (73.7) | 5 (26.3) | ||
| 41+ | 22 (71) | 9 (29) | ||
| Title | General dentist | 190 (85.6) a | 32 (14.4) | 0.013 |
| Specialization/PhD student | 91 (74) | 32 (26) | ||
| Doctorate/specialized dentist | 50 (87.7) ab | 7 (12.3) | ||
| PhD/specialization branch | General dentistry | 190 (86.4) a | 30 (13.6) a | <0.001 |
| Periodontology | 3 (33.3) bc | 6 (66.7) bc | ||
| Oral and maxillofacial surgery | 4 (26.7) bc | 11 (73.3) bc | ||
| Restorative dentistry | 62 (91.2) a | 6 (8.8) | ||
| Endodontics | 24 (100) | 0 (0) | ||
| Pedodontics | 32 (100) | 0 (0) | ||
| Orthodontics | 1 (10) | 9 (90) | ||
| Prosthodontics | 15 (68.2) ac | 7 (31.8) ac | ||
| Graduation year | Before 2000 | 14 (77.8) | 4 (22.2) | 0.759 |
| 2001–2010 | 27 (77.1) | 8 (22.9) | ||
| 2011–2020 | 218 (83.5) | 43 (16.5) | ||
| Post 2021 | 72 (81.8) | 16 (18.2) | ||
| Years of professional experience | 5 years or fewer | 223 (83.5) | 44 (16.5) | 0.110 |
| 6–10 years | 68 (86.1) | 11 (13.9) | ||
| 11–15 years | 17 (77.3) | 5 (22.7) | ||
| 16–20 years | 14 (73.7) | 5 (26.3) | ||
| Over 21 years | 9 (60) | 6 (40) | ||
| Employed institution | Private | 48 (92.3) | 4 (7.7) | 0.051 |
| Public | 89 (81.7) | 20 (18.3) | ||
| University | 126 (76.4) | 39 (23.6) | ||
| Other/private hospital | 66 (89.2) | 8 (10.8) | ||
| General Dentist | Periodontology | Oral and Maxillofacial Surgery | Restorative Dentistry | Endodontics | Pedodontics | Orthodontics | Prosthodontics | p | ||
|---|---|---|---|---|---|---|---|---|---|---|
| n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | <0.001 | ||
| Do you perform a vitality test before performing indirect pulp capping treatment? | No | 135 (71.1) a | 3 (100) | 2 (50) ab | 39 (63.9) a | 6 (25) b | 23 (71.9) a | 1 (100) | 13 (86.7) a | |
| Electrical pulp test | 25 (13.2) a | 0 (0) | 2 (50) ab | 22 (36.1) bd | 12 (50) bc | 4 (12.5) ad | 0 (0) | 1 (6.7) ab | ||
| Cold test | 42 (22.1) | 0 (0) | 1 (25) | 10 (16.4) | 11 (45.8) | 9 (28.1) | 0 (0) | 2 (13.3) | ||
| Other tests | 2 (1.1) a | 0 (0) | 0 (0) | 1 (1.6) ab | 3 (12.5) b | 0 (0) | 0 (0) | 0 (0) |
| Private | Public | University | Other/Private Hospitals | p | ||
|---|---|---|---|---|---|---|
| n (%) | n (%) | n (%) | n (%) | <0.001 | ||
| What kind of isolation method do you use during indirect pulp capping treatment? | Cotton roll | 41 (85.4) a | 88 (98.9) b | 113 (89.7) a | 57 (86.4) a | |
| Rubber dam | 11 (22.9) a | 3 (3.4) b | 39 (31) a | 18 (27.3) a | ||
| Other | 0 (0) | 0 (0) | 1 (0.8) | 1 (1.5) | ||
| General dentist | Periodontology | Oral and Maxillofacial Surgery | Restorative Dentistry | Endodontics | Pedodontics | Orthodontics | Prosthodontics | p | ||
|---|---|---|---|---|---|---|---|---|---|---|
| n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | <0.001 | ||
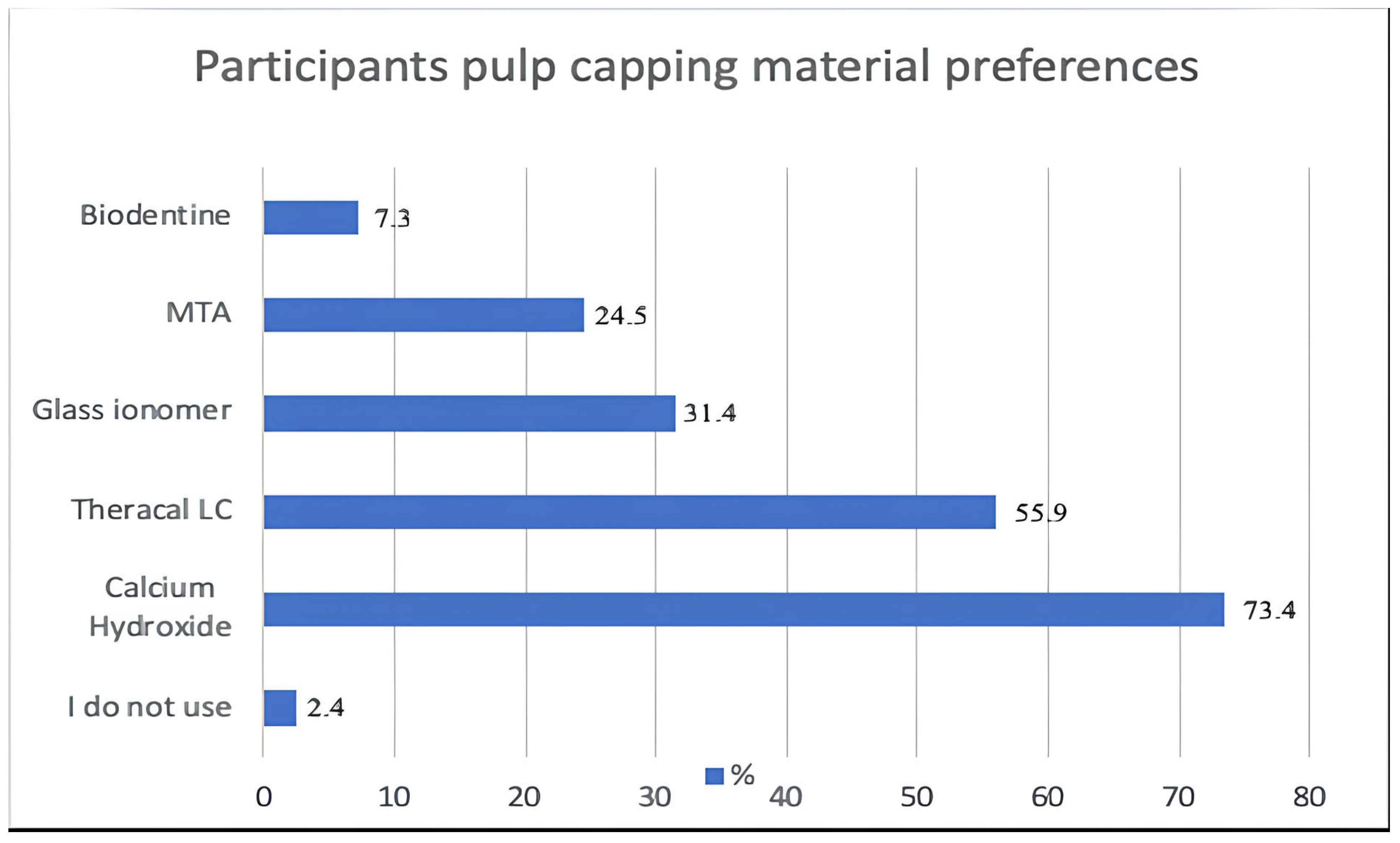
| Do you use any pulp coating agents in indirect pulp capping treatment? | No | 4 (2.1) | 0 (0) | 0 (0) | 1 (1.6) | 2 (8.3) | 1 (3.1) | 0 (0) | 0 (0) | |
| Ca(OH)2 | 143 (75.3) | 3 (100) | 4 (100) | 41 (66.1) | 16 (66.7) | 24 (75) | 0 (0) | 12 (80) | ||
| Theracal LC | 95 (50) a | 2 (66.7) | 2 (50) ab | 50 (80.6) b | 12 (50) ab | 13 (40.6) a | 1 (100) | 10 (66.7) ab | ||
| Glass ionomer | 65 (34.2) | 2 (66.7) ab | 0 (0) | 16 (25.8) | 3 (12.5) | 11 (34.4) | 0 (0) | 7 (46.7) | ||
| MTA | 29 (15.3) a | 0 (0) | 3 (75) bcd | 18 (29) ab | 8 (33.3) abc | 21 (65.6) c | 0 (0) | 2 (13.3) ad | ||
| Biodentine | 10 (5.3) | 0 (0) | 1 (25) | 7 (11.3) | 3 (12.5) | 3 (9.4) | 0 (0) | 0 (0) | ||
| Private | Public | University | Other/Private Hospitals | p | ||
|---|---|---|---|---|---|---|
| n (%) | n (%) | n (%) | n (%) | <0.001 | ||
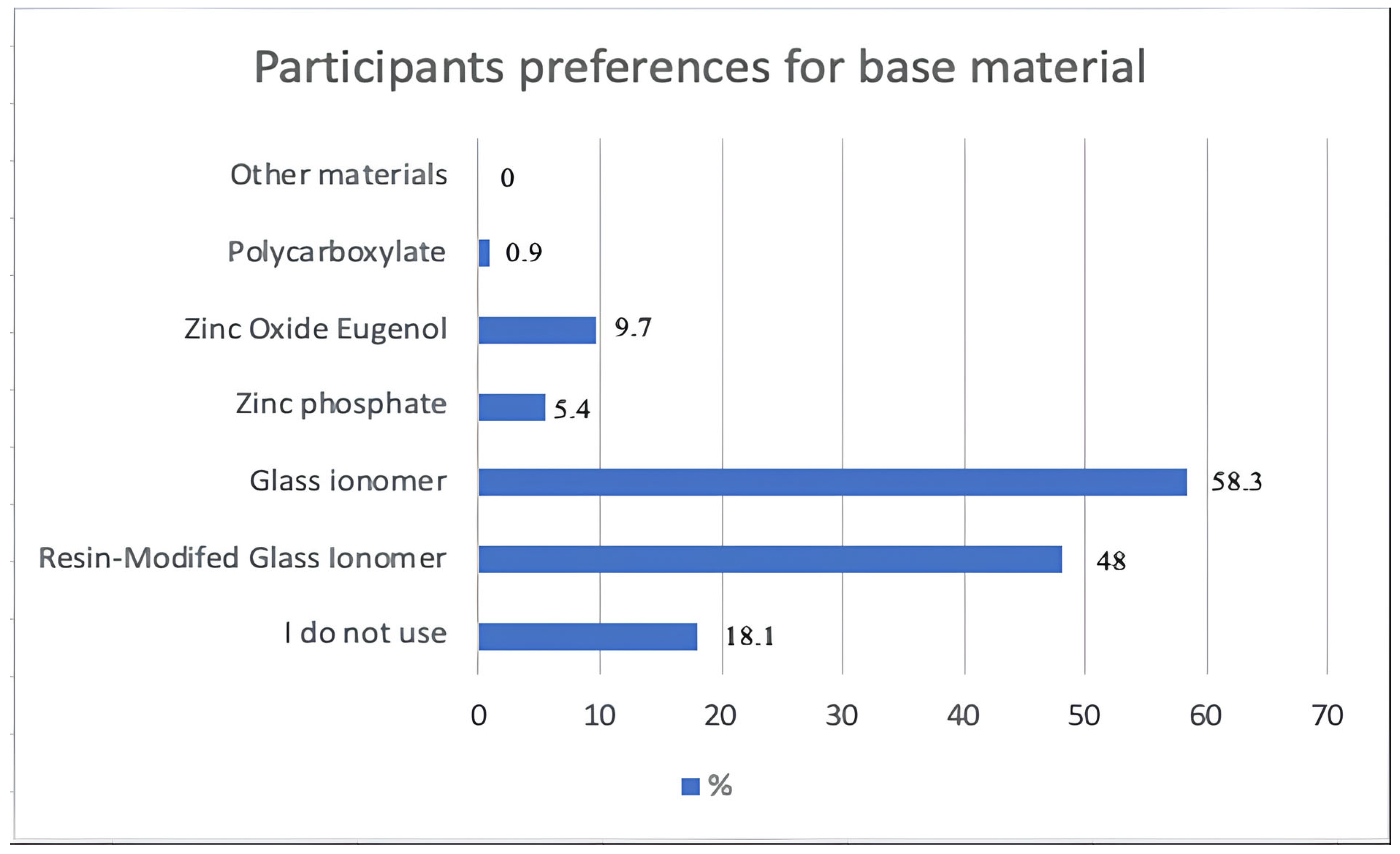
| Do you use any pulp coating agents in indirect pulp capping treatment? | No | 1 (2.1) | 2 (2.2) | 3 (2.4) | 2 (3) | |
| Ca(OH)2 | 29 (60.4) a | 76 (85.4) b | 101 (80.2) b | 35 (53) a | ||
| Theracal LC | 30 (62.5) a | 29 (32.6) b | 74 (58.7) a | 50 (75.8) a | ||
| Glass ionomer | 15 (31.3) | 28 (31.5) | 38 (30.2) | 21 (31.8) | ||
| MTA | 13 (27.1) ab | 11 (12.4) a | 37 (29.4) b | 19 (28.8) ab | ||
| Biodentine | 5 (10.4) | 3 (3.4) | 12 (9.5) | 3 (4.5) | ||
| Private | Public | University | Other Institutions | p | ||
|---|---|---|---|---|---|---|
| n (%) | n (%) | n (%) | n (%) | |||
| Which permanent restoration material do you use after indirect pulp capping treatment? | Composite | 48 (100) | 84 (94.4) | 123 (97.6) | 66 (100) | <0.001 |
| Compomer | 3 (6.3) | 5 (5.6) | 15 (11.9) | 7 (10.6) | ||
| Glass ionomer | 7 (14.6) | 12 (13.5) | 24 (19) | 5 (7.6) | ||
| Amalgam | 0 (0) | 45 (50.6) a | 8 (6.3) b | 2 (3) b |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Published by MDPI on behalf of the Lithuanian University of Health Sciences. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Arslan, B.; Yaman, B.C.; Çeliksöz, Ö.; Can Aydın, H. An Evaluation of Turkish Dentists’ Approach to Indirect Pulp Capping and Material Preferences: A Questionnaire-Based Survey. Medicina 2025, 61, 1120. https://doi.org/10.3390/medicina61071120
Arslan B, Yaman BC, Çeliksöz Ö, Can Aydın H. An Evaluation of Turkish Dentists’ Approach to Indirect Pulp Capping and Material Preferences: A Questionnaire-Based Survey. Medicina. 2025; 61(7):1120. https://doi.org/10.3390/medicina61071120
Chicago/Turabian StyleArslan, Baturalp, Batu Can Yaman, Özge Çeliksöz, and Havva Can Aydın. 2025. "An Evaluation of Turkish Dentists’ Approach to Indirect Pulp Capping and Material Preferences: A Questionnaire-Based Survey" Medicina 61, no. 7: 1120. https://doi.org/10.3390/medicina61071120
APA StyleArslan, B., Yaman, B. C., Çeliksöz, Ö., & Can Aydın, H. (2025). An Evaluation of Turkish Dentists’ Approach to Indirect Pulp Capping and Material Preferences: A Questionnaire-Based Survey. Medicina, 61(7), 1120. https://doi.org/10.3390/medicina61071120






