Mpox Infection and Endocrine Health: Bridging the Knowledge Gap
Abstract
1. Introduction
2. MPX and Thyroid Function
3. MPX and the Adrenals/Other Endocrine Glands
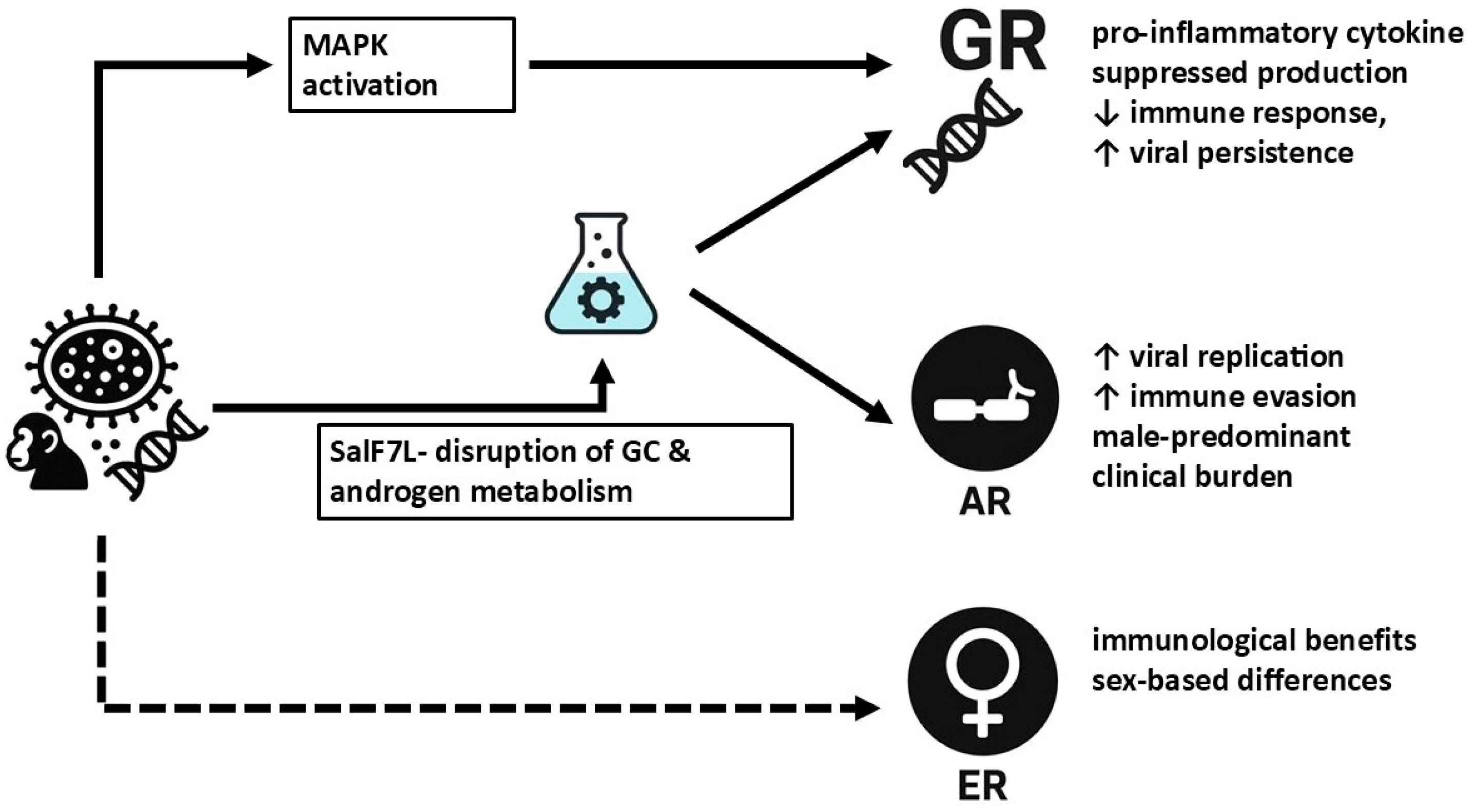
4. MPX and the Gonads: Clinical and Pathophysiological Considerations
5. Interaction of MPX with Hormonal Receptors and Hormonal Metabolism
6. Clinical Implications and Risks of Steroid Therapy in MPX
7. Conclusions
8. Limitations and Future Directions
8.1. Limitations
8.2. Future Research Directions
Author Contributions
Funding
Conflicts of Interest
Abbreviations
| MPX | Mpox |
| MPXV | Monkeypox virus |
| HPA | Hypothalamic–pituitary–adrenal |
| TSH | Thyrotropin |
| T3 | Triiodothyronine |
| T4 | Thyroxine |
| AI | Adrenal insufficiency |
| 11β-HSD | 11β-hydroxysteroid dehydrogenase |
| HPG | Hypothalamic-pituitary-gonadal |
| MSM | Men who have sex with men |
| GRs | Glucocorticoid receptors |
| ARs | Androgen receptors |
| ERs | Estrogen receptors |
| GCs | Glucocorticoids |
| 3β-HSD | 3β-hydroxysteroid dehydrogenase |
| STI | Sexually transmitted infection |
| SGRMs | Selective glucocorticoid receptor modulators |
References
- Gessain, A.; Nakoune, E.; Yazdanpanah, Y. Monkeypox. N. Engl. J. Med. 2022, 387, 1783–1793. [Google Scholar] [CrossRef] [PubMed]
- Jezek, Z.; Szczeniowski, M.; Paluku, K.M.; Mutombo, M. Human monkeypox: Clinical features of 282 patients. J. Infect. Dis. 1987, 156, 293–298. [Google Scholar] [CrossRef]
- Li, L.; Xu, C.; Guo, Y.; Wang, H. Screening potential treatments for mpox from Traditional Chinese Medicine by using a data-driven approach. Medicine 2023, 102, e35116. [Google Scholar] [CrossRef]
- Jadhav, V.; Paul, A.; Trivedi, V.; Bhatnagar, R.; Bhalsinge, R.; Jadhav, S.V. Global epidemiology, viral evolution, and public health responses: A systematic review on Mpox (1958–2024). J. Glob. Health 2025, 15, 04061. [Google Scholar] [CrossRef]
- Maluquer de Motes, C.; Ulaeto, D.O. Mpox poses an ever-increasing epidemic and pandemic risk. Nat. Med. 2025. [Google Scholar] [CrossRef]
- Adebiyi, B.O. Mpox alert: COVID-19’s hard-earned lessons put to the test. One Health 2025, 20, 101003. [Google Scholar] [CrossRef] [PubMed]
- Son, B.W.K. Ending the Mpox Endemic: Beyond Declaring a Public Health Emergency. Integr. J. Vet. Biosci. 2025, 9, 1–3. [Google Scholar] [CrossRef]
- Alshahrani, A. The expected economic burden on the healthcare system because of quarantining patients with monkeypox virus. Saudi Med. J. 2023, 44, 231–236. [Google Scholar] [CrossRef] [PubMed]
- Desailloud, R.; Hober, D. Viruses and thyroiditis: An update. Virol. J. 2009, 6, 5. [Google Scholar] [CrossRef]
- Ssemmondo, E.; Idris, M.A.; Mawer, D.; Easom, N.; Thow, J. Subacute thyroiditis following Mpox infection in a patient with human immunodeficiency virus. Endocrinol. Diabetes Metab. Case Rep. 2023, 2023, 23-0034. [Google Scholar] [CrossRef]
- Zaucha, G.M.; Jahrling, P.B.; Geisbert, T.W.; Swearengen, J.R.; Hensley, L. The pathology of experimental aerosolized monkeypox virus infection in cynomolgus monkeys (Macaca fascicularis). Lab. Investig. 2001, 81, 1581–1600. [Google Scholar] [CrossRef]
- Joob, B.; Wiwanitkit, V. Thyroid Disorder: A Possible Forgotten Clinical Feature of Monkeypox. Endocrinol. Metab. 2023, 38, 285–286. [Google Scholar] [CrossRef] [PubMed]
- Feghali, K.; Atallah, J.; Norman, C. Manifestations of thyroid disease post COVID-19 illness: Report of Hashimoto thyroiditis, Graves' disease, and subacute thyroiditis. J. Clin. Transl. Endocrinol. Case Rep. 2021, 22, 100094. [Google Scholar] [CrossRef] [PubMed]
- Huhn, G.D.; Bauer, A.M.; Yorita, K.; Graham, M.B.; Sejvar, J.; Likos, A.; Damon, I.K.; Reynolds, M.G.; Kuehnert, M.J. Clinical characteristics of human monkeypox, and risk factors for severe disease. Clin. Infect. Dis. 2005, 41, 1742–1751. [Google Scholar] [CrossRef] [PubMed]
- Murugan, A.K.; Alzahrani, A.S. SARS-CoV-2: Emerging Role in the Pathogenesis of Various Thyroid Diseases. J. Inflamm. Res. 2021, 14, 6191–6221. [Google Scholar] [CrossRef] [PubMed]
- Thornhill, J.P.; Barkati, S.; Walmsley, S.; Rockstroh, J.; Antinori, A.; Harrison, L.B.; Palich, R.; Nori, A.; Reeves, I.; Habibi, M.S.; et al. Monkeypox Virus Infection in Humans across 16 Countries—April–June 2022. N. Engl. J. Med. 2022, 387, 679–691. [Google Scholar] [CrossRef]
- Dineen, R.A.; Martin-Grace, J.; Ahmed, K.M.S.; Taylor, A.E.; Shaheen, F.; Schiffer, L.; Gilligan, L.C.; Lavery, G.G.; Frizelle, I.; Gunness, A.; et al. Tissue Glucocorticoid Metabolism in Adrenal Insufficiency: A Prospective Study of Dual-release Hydrocortisone Therapy. J. Clin. Endocrinol. Metab. 2023, 108, 3178–3189. [Google Scholar] [CrossRef]
- Johannsson, G.; Ragnarsson, O. Cardiovascular and metabolic impact of glucocorticoid replacement therapy. Front. Horm. Res. 2014, 43, 33–44. [Google Scholar] [CrossRef]
- Ross, I.L.; Bergthorsdottir, R.; Levitt, N.; Dave, J.A.; Schatz, D.; Marais, D.; Johannsson, G. Cardiovascular risk factors in patients with Addison's disease: A comparative study of South African and Swedish patients. PLoS ONE 2014, 9, e90768. [Google Scholar] [CrossRef]
- Gathercole, L.L.; Lavery, G.G.; Morgan, S.A.; Cooper, M.S.; Sinclair, A.J.; Tomlinson, J.W.; Stewart, P.M. 11β-Hydroxysteroid dehydrogenase 1: Translational and therapeutic aspects. Endocr. Rev. 2013, 34, 525–555. [Google Scholar] [CrossRef]
- Morgan, S.A.; McCabe, E.L.; Gathercole, L.L.; Hassan-Smith, Z.K.; Larner, D.P.; Bujalska, I.J.; Stewart, P.M.; Tomlinson, J.W.; Lavery, G.G. 11β-HSD1 is the major regulator of the tissue-specific effects of circulating glucocorticoid excess. Proc. Natl. Acad. Sci. USA 2014, 111, E2482–E2491. [Google Scholar] [CrossRef]
- Adler, H.; Gould, S.; Hine, P.; Snell, L.B.; Wong, W.; Houlihan, C.F.; Osborne, J.C.; Rampling, T.; Beadsworth, M.B.; Duncan, C.J.; et al. Clinical features and management of human monkeypox: A retrospective observational study in the UK. Lancet Infect. Dis. 2022, 22, 1153–1162. [Google Scholar] [CrossRef] [PubMed]
- Sagmeister, M.S.; Taylor, A.E.; Fenton, A.; Wall, N.A.; Chanouzas, D.; Nightingale, P.G.; Ferro, C.J.; Arlt, W.; Cockwell, P.; Hardy, R.S.; et al. Glucocorticoid activation by 11β-hydroxysteroid dehydrogenase enzymes in relation to inflammation and glycaemic control in chronic kidney disease: A cross-sectional study. Clin. Endocrinol. 2019, 90, 241–249. [Google Scholar] [CrossRef]
- Patel, A.; Bilinska, J.; Tam, J.C.H.; Da Silva Fontoura, D.; Mason, C.Y.; Daunt, A.; Snell, L.B.; Murphy, J.; Potter, J.; Tuudah, C.; et al. Clinical features and novel presentations of human monkeypox in a central London centre during the 2022 outbreak: Descriptive case series. BMJ 2022, 378, e072410. [Google Scholar] [CrossRef]
- Acharya, A.; Kumar, N.; Singh, K.; Byrareddy, S.N. Mpox in MSM: Tackling stigma, minimizing risk factors, exploring pathogenesis, and treatment approaches. Biomed. J. 2024, 48, 100746. [Google Scholar] [CrossRef]
- Liu, J.; Mucker, E.M.; Chapman, J.L.; Babka, A.M.; Gordon, J.M.; Bryan, A.V.; Raymond, J.L.W.; Bell, T.M.; Facemire, P.R.; Goff, A.J.; et al. Retrospective detection of monkeypox virus in the testes of nonhuman primate survivors. Nat. Microbiol. 2022, 7, 1980–1986. [Google Scholar] [CrossRef]
- Liu, Q.; Fu, L.; Wang, B.; Sun, Y.; Wu, X.; Peng, X.; Li, Y.; Lin, Y.F.; Fitzpatrick, T.; Vermund, S.H.; et al. Clinical Characteristics of Human Mpox (Monkeypox) in 2022: A Systematic Review and Meta-Analysis. Pathogens 2023, 12, 146. [Google Scholar] [CrossRef] [PubMed]
- Malone, S.M.; Mitra, A.K.; Onumah, N.A.; Brown, A.; Jones, L.M.; Tresvant, D.; Brown, C.S.; Onyia, A.U.; Iseguede, F.O. Safety and Efficacy of Post-Eradication Smallpox Vaccine as an Mpox Vaccine: A Systematic Review with Meta-Analysis. Int. J. Environ. Res. Public Health 2023, 20, 2963. [Google Scholar] [CrossRef] [PubMed]
- Fine, P.E.; Jezek, Z.; Grab, B.; Dixon, H. The transmission potential of monkeypox virus in human populations. Int. J. Epidemiol. 1988, 17, 643–650. [Google Scholar] [CrossRef]
- Orassay, A.; Diassova, A.; Berdigaliyev, A.; Liu, D.; Makhmutova, Z.; Amin, A.; Xie, Y. Gender trend of monkeypox virus infection. Expert Rev. Anti. Infect. Ther. 2023, 21, 571–576. [Google Scholar] [CrossRef]
- Yon, H.; Shin, H.; Shin, J.I.; Shin, J.U.; Shin, Y.H.; Lee, J.; Rhee, S.Y.; Koyanagi, A.; Jacob, L.; Smith, L.; et al. Clinical manifestations of human Mpox infection: A systematic review and meta-analysis. Rev. Med. Virol. 2023, 33, e2446. [Google Scholar] [CrossRef] [PubMed]
- Babkin, I.V.; Babkina, I.N.; Tikunova, N.V. An Update of Orthopoxvirus Molecular Evolution. Viruses 2022, 14, 388. [Google Scholar] [CrossRef]
- Chang, C.; Greenspan, A.; Gershwin, M.E. The pathogenesis, diagnosis and clinical manifestations of steroid-induced osteonecrosis. J. Autoimmun. 2020, 110, 102460. [Google Scholar] [CrossRef] [PubMed]
- Moore, J.B.; Smith, G.L. Steroid hormone synthesis by a vaccinia enzyme: A new type of virus virulence factor. EMBO J. 1992, 11, 1973–1980. [Google Scholar] [CrossRef] [PubMed]
- Weinstein, R.S. Glucocorticoid-induced osteonecrosis. Endocrine 2012, 41, 183–190. [Google Scholar] [CrossRef] [PubMed]
- Cui, Q.; Jo, W.L.; Koo, K.H.; Cheng, E.Y.; Drescher, W.; Goodman, S.B.; Ha, Y.C.; Hernigou, P.; Jones, L.C.; Kim, S.Y.; et al. ARCO Consensus on the Pathogenesis of Non-traumatic Osteonecrosis of the Femoral Head. J. Korean Med. Sci. 2021, 36, e65. [Google Scholar] [CrossRef]
- Kerachian, M.A.; Séguin, C.; Harvey, E.J. Glucocorticoids in osteonecrosis of the femoral head: A new understanding of the mechanisms of action. J. Steroid Biochem. Mol. Biol. 2009, 114, 121–128. [Google Scholar] [CrossRef]
- Chan, M.H.; Chan, P.K.; Griffith, J.F.; Chan, I.H.; Lit, L.C.; Wong, C.K.; Antonio, G.E.; Liu, E.Y.; Hui, D.S.; Suen, M.W.; et al. Steroid-induced osteonecrosis in severe acute respiratory syndrome: A retrospective analysis of biochemical markers of bone metabolism and corticosteroid therapy. Pathology 2006, 38, 229–235. [Google Scholar] [CrossRef]
| Impact | Findings | Mechanisms | Clinical Implications |
|---|---|---|---|
| Thyroid | MPX linked to subacute thyroiditis, leading to thyrotoxicosis or hypothyroidism | Viral infiltration; immune-mediated damage | Symptoms: fever, weight loss, neck pain Treatment: corticosteroids, levothyroxine |
| Adrenal | Viral infections have been implicated in adrenal insufficiency | Viral invasion; HPA axis dysregulation | Possible risk of adrenal insufficiency, requiring glucocorticoid therapy |
| Reproductive (Men) | MPXV persistence in testes; may affect fertility, hormone production | Testicular inflammation; necrosis | Potential sperm quality reduction, hormonal imbalances Further research needed |
| Hormonal Receptors | MPXV may alter steroid receptor activity | Modulation of glucocorticoid, androgen, and estrogen signaling/metabolism pathways | Possible sex-based differences in severity of MPX |
| Steroid Therapy | Steroids help inflammation but may prolong MPXV viremia | Interaction with glucocorticoid receptors | Need for balance between benefit and harm needed; selective glucocorticoid receptor modulators (SGRMs) may help |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Published by MDPI on behalf of the Lithuanian University of Health Sciences. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Savvidis, C.; Rizzo, M.; Ilias, I. Mpox Infection and Endocrine Health: Bridging the Knowledge Gap. Medicina 2025, 61, 899. https://doi.org/10.3390/medicina61050899
Savvidis C, Rizzo M, Ilias I. Mpox Infection and Endocrine Health: Bridging the Knowledge Gap. Medicina. 2025; 61(5):899. https://doi.org/10.3390/medicina61050899
Chicago/Turabian StyleSavvidis, Christos, Manfredi Rizzo, and Ioannis Ilias. 2025. "Mpox Infection and Endocrine Health: Bridging the Knowledge Gap" Medicina 61, no. 5: 899. https://doi.org/10.3390/medicina61050899
APA StyleSavvidis, C., Rizzo, M., & Ilias, I. (2025). Mpox Infection and Endocrine Health: Bridging the Knowledge Gap. Medicina, 61(5), 899. https://doi.org/10.3390/medicina61050899








