Assessing Nasal Nitric Oxide in Allergic Rhinitis: A Controversial Biomarker
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Population
2.2. Assessment of Allergy
2.3. Measurement of Nasal NO
2.4. Statistical Analysis
3. Results
3.1. Study Groups
3.2. Diagnostic Accuracy of nNO for AR
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Savouré, M.; Bousquet, J.; Jaakkola, J.J.K.; Jaakkola, M.S.; Jacquemin, B.; Nadif, R. Worldwide prevalence of rhinitis in adults: A review of definitions and temporal evolution. Clin. Transl. Allergy 2022, 12, e12130. [Google Scholar] [CrossRef]
- Bousquet, J.; Melén, E.; Haahtela, T.; Koppelman, G.H.; Togias, A.; Valenta, R.; Akdis, C.A.; Czarlewski, W.; Rothenberg, M.; Valiulis, A.; et al. Rhinitis associated with asthma is distinct from rhinitis alone: The ARIA-MeDALL hypothesis. Allergy 2023, 78, 1169–1203. [Google Scholar] [CrossRef] [PubMed]
- Papadopoulos, N.G.; Bernstein, J.A.; Demoly, P.; Dykewicz, M.; Fokkens, W.; Hellings, P.W.; Peters, A.T.; Rondon, C.; Togias, A.; Cox, L.S. Phenotypes and endotypes of rhinitis and their impact on management: A PRACTALL report. Allergy 2015, 70, 474–494. [Google Scholar] [CrossRef] [PubMed]
- Rachelefsky, G.S. National guidelines needed to manage rhinitis and prevent complications. Ann. Allergy Asthma Immunol. 1999, 82, 296–305. [Google Scholar] [CrossRef] [PubMed]
- Forstermann, U.; Sessa, W.C. Nitric oxide synthases: Regulation and function. Eur. Heart J. 2011, 33, 829–837. [Google Scholar] [CrossRef]
- Cinelli, M.A.; Do, H.T.; Miley, G.P.; Silverman, R.B. Inducible nitric oxide synthase: Regulation, structure, and inhibition. Med. Res. Rev. 2019, 40, 158–189. [Google Scholar] [CrossRef]
- Marcos, M.C.; Cisneros Serrano, C. What is the added value of FeNO as T2 biomarker? Front. Allergy 2022, 3, 957106. [Google Scholar] [CrossRef]
- Kouis, P.; Papatheodorou, S.I.; Yiallouros, P.K. Diagnostic accuracy of nasal nitric oxide for establishing diagnosis of primary ciliary dyskinesia: A meta-analysis. BMC Pulm. Med. 2015, 15, 153. [Google Scholar] [CrossRef]
- Beydon, N.; Kouis, P.; Marthin, J.K.; Latzin, P.; Colas, M.; Davis, S.D.; Haarman, E.; Harris, A.L.; Hogg, C.; Kilbride, E.; et al. Nasal nitric oxide measurement in children for the diagnosis of primary ciliary dyskinesia: European Respiratory Society technical standard. Eur. Respir. J. 2023, 61, 2202031. [Google Scholar] [CrossRef]
- Benedict, J.J.; Lelegren, M.; Han, J.K.; Lam, K. Nasal Nitric Oxide as a Biomarker in the Diagnosis and Treatment of Sinonasal Inflammatory Diseases: A Review of the Literature. Ann. Otol. Rhinol. Laryngol. 2022, 132, 460–469. [Google Scholar] [CrossRef]
- Wise, S.K.; Damask, C.; Roland, L.T.; Ebert, C.; Levy, J.M.; Lin, S.; Luong, A.; Rodriguez, K.; Sedaghat, A.R.; Toskala, E.; et al. International consensus statement on allergy and rhinology: Allergic Rhinitis—2023. Int. Forum Allergy Rhinol. 2023, 13, 293–859. [Google Scholar] [CrossRef] [PubMed]
- Suojalehto, H.; Vehmas, T.; Lindström, I.; Kennedy, D.W.; Kilpeläinen, M.; Plosila, T.; Savukoski, S.; Sipilä, J.; Varpula, M.; Wolff, H.; et al. Nasal nitric oxide is dependent on sinus obstruction in allergic rhinitis. Laryngoscope 2014, 124, E213–E218. [Google Scholar] [CrossRef] [PubMed]
- Liu, C.; Zheng, K.; Liu, X.; Zheng, M.; Liu, Z.; Wang, X.; Zhang, L. Use of Nasal Nitric Oxide in the Diagnosis of Allergic Rhinitis and Nonallergic Rhinitis in Patients with and without Sinus Inflammation. J. Allergy Clin. Immunol. Pract. 2020, 8, 1574–1581.e4. [Google Scholar] [CrossRef]
- Baraldi, E.; Azzolin, N.M.; Carra, S.; Dario, C.; Marchesini, L.; Zacchello, F. Effect of topical steroids on nasal nitric oxide production in children with perennial allergic rhinitis: A pilot study. Respir. Med. 1998, 92, 558–561. [Google Scholar] [CrossRef]
- Kharitonov, S.A.; Rajakulasingam, K.; O’Connor, B.; Durham, S.R.; Barnes, P.J. Nasal nitric oxide is increased in patients with asthma and allergic rhinitis and may be modulated by nasal glucocorticoids. J. Allergy Clin. Immunol. 1997, 99, 58–64. [Google Scholar] [CrossRef]
- Antosova, M.; Bencova, A.; Mokra, D.; Plevkova, J.; Pepucha, L.; Buday, T. Exhaled and Nasal Nitric Oxide—Impact for Allergic Rhinitis. Physiol. Res. 2020, 69 (Suppl. S1), S123–S130. [Google Scholar] [CrossRef]
- ATS/ERS Recommendations for Standardized Procedures for the Online and Offline Measurement of Exhaled Lower Respiratory Nitric Oxide and Nasal Nitric Oxide, 2005. Am. J. Respir. Crit. Care Med. 2005, 171, 912–930. [CrossRef]
- Wedbäck, A.; Enbom, H.; Erisksson, N.E.; Movérare, R.; Malcus, I. Seasonal non-allergic rhinitis (SNAR)—A new disease entity? A clinical and immunological comparison between SNAR, seasonal allergic rhinitis and persistent non-allergic rhinitis. Rhinology 2005, 43, 86–92. [Google Scholar] [PubMed]
- Rondón, C.; Doña, I.; López, S.; Campo, P.; Romero, J.J.; Torres, M.J.; Mayorga, C.; Blanca, M. Seasonal idiopathic rhinitis with local inflammatory response and specific IgE in absence of systemic response. Allergy 2008, 63, 1352–1358. [Google Scholar] [CrossRef]
- Gustafsson, L.E.; Leone, A.M.; Persson, M.G.; Wiklund, N.P.; Moncada, S. Endogenous nitric oxide is present in the exhaled air of rabbits, guinea pigs and humans. Biochem. Biophys. Res. Commun. 1991, 181, 852–857. [Google Scholar] [CrossRef]
- Alving, K.; Weitzberg, E.; Lundberg, J. Increased amount of nitric oxide in exhaled air of asthmatics. Eur. Respir. J. 1993, 6, 1368–1370. [Google Scholar] [CrossRef] [PubMed]
- Bousquet, J.; van Cauwenberge, P.; Khaltaev, N. Executive Summary of the Workshop Report 7–10 December 1999, Geneva, Switzerland. Allergy 2002, 57, 841–855. [Google Scholar] [CrossRef] [PubMed]
- Williamson, P.A.; Vaidyanathan, S.; Clearie, K.; Stewart, M.; Lipworth, B.J. Relationship between fractional exhaled nitric oxide and nasal nitric oxide in airways disease. Ann. Allergy Asthma Immunol. 2010, 105, 162–167. [Google Scholar] [CrossRef] [PubMed]
- Arnal, J.F.; Didier, A.; Rami, J.; M’Rini, C.; Charlet, J.P.; Serrano, E.; Besombes, J.P. Nasal nitric oxide is increased in allergic rhinitis. Clin. Exp. Allergy 1997, 27, 358–362. [Google Scholar] [CrossRef]
- Lee, K.J.; Cho, S.H.; Lee, S.H.; Tae, K.; Yoon, H.J.; Kim, S.H.; Jeong, J.H. Nasal and Exhaled Nitric Oxide in Allergic Rhinitis. Clin. Exp. Otorhinolaryngol. 2012, 5, 228–233. [Google Scholar] [CrossRef]
- Nesic, V.S.; Djordjevic, V.Z.; Tomic-Spiric, V.; Dudvarski, Z.R.; Soldatovic, I.A.; Arsovic, N.A. Measuring nasal nitric oxide in allergic rhinitis patients. J. Laryngol. Otol. 2016, 130, 1064–1071. [Google Scholar] [CrossRef]
- Ambrosino, P.; Parrella, P.; Formisano, R.; Papa, A.; Spedicato, G.A.; Di Minno, M.N.; Motta, A.; Maniscalco, M. Clinical application of nasal nitric oxide measurement in allergic rhinitis. Ann. Allergy Asthma Immunol. 2020, 125, 447–459.e5. [Google Scholar] [CrossRef]
- Henriksen, A.H.; Sue-Chu, M.; Lingaas Holmen, T.; Langhammer, A.; Bjermer, L. Exhaled and nasal NO levels in allergic rhinitis: Relation to sensitization, pollen season and bronchial hyperresponsiveness. Eur. Respir. J. 1999, 13, 301–306. [Google Scholar] [CrossRef]
- Palm, J.P.; Alving, K.; Lundberg, J.O. Characterization of airway nitric oxide in allergic rhinitis: The effect of intranasal administration of L-NAME. Allergy 2003, 58, 885–892. [Google Scholar] [CrossRef]
- Maniscalco, M.; Sofia, M.; Carratù, L.; Higenbottam, T. Effect of nitric oxide inhibition on nasal airway resistance after nasal allergen challenge in allergic rhinitis. Eur. J. Clin. Investig. 2001, 31, 462–466. [Google Scholar] [CrossRef]
- Kalpaklioglu, A.F.; Baccioglu, A.; Yalim, S.A. Can nasal nitric oxide be a biomarker to differentiate allergic and non-allergic rhinitis? Egypt. J. Otolaryngol. 2021, 37, 91. [Google Scholar] [CrossRef]
- Moody, A.; Fergusson, W.; Wells, A.; Bartley, J.; Kolbe, J. Nasal Levels of Nitric Oxide as an Outcome Variable in Allergic Upper Respiratory Tract Disease: Influence of Atopy and Hayfever on nNO. Am. J. Rhinol. 2006, 20, 425–429. [Google Scholar] [CrossRef] [PubMed]
- Gucel, S.; Guvensen, A.; Ozturk, M.; Celik, A. Analysis of airborne pollen fall in Nicosia (Cyprus). Environ. Monit. Assess. 2012, 185, 157–169. [Google Scholar] [CrossRef] [PubMed]
- Ge, C.; Zhuang, H.; Yo, H.; Zhang, C. Correlation between peripheral blood iNKT cell levels and exhaled NO in patients with allergic rhinitis. Hum Immunol 2025, 2, 1112555. [Google Scholar] [CrossRef]

| Sensitization Status | Summary Statistics |
|---|---|
| Seasonal allergens, N (% with a positive test) | |
| Olea europea | 14 (35.9) |
| Cupressus sempervirens | 7 (17.9) |
| Phleum pratense | 8 (20.5) |
| Triticum sativa | 6 (15.4) |
| Zea mais | 8 (20.5) |
| Parietaria judaica | 4 (10.2) |
| Artemisia vulgaris | 6 (15.4) |
| Plantago lanceolata | 6 (15.4) |
| Chenopodium album | 3 (7.7) |
| Salsola kali | 5 (12.8) |
| Alternaria alternata | 4 (10.2) |
| Perennial allergens, N (% with a positive test) | |
| Cat | 8 (20.5) |
| Dog | 1 (2.5) |
| Dermatophagoides pteronyssinus | 18 (46.1) |
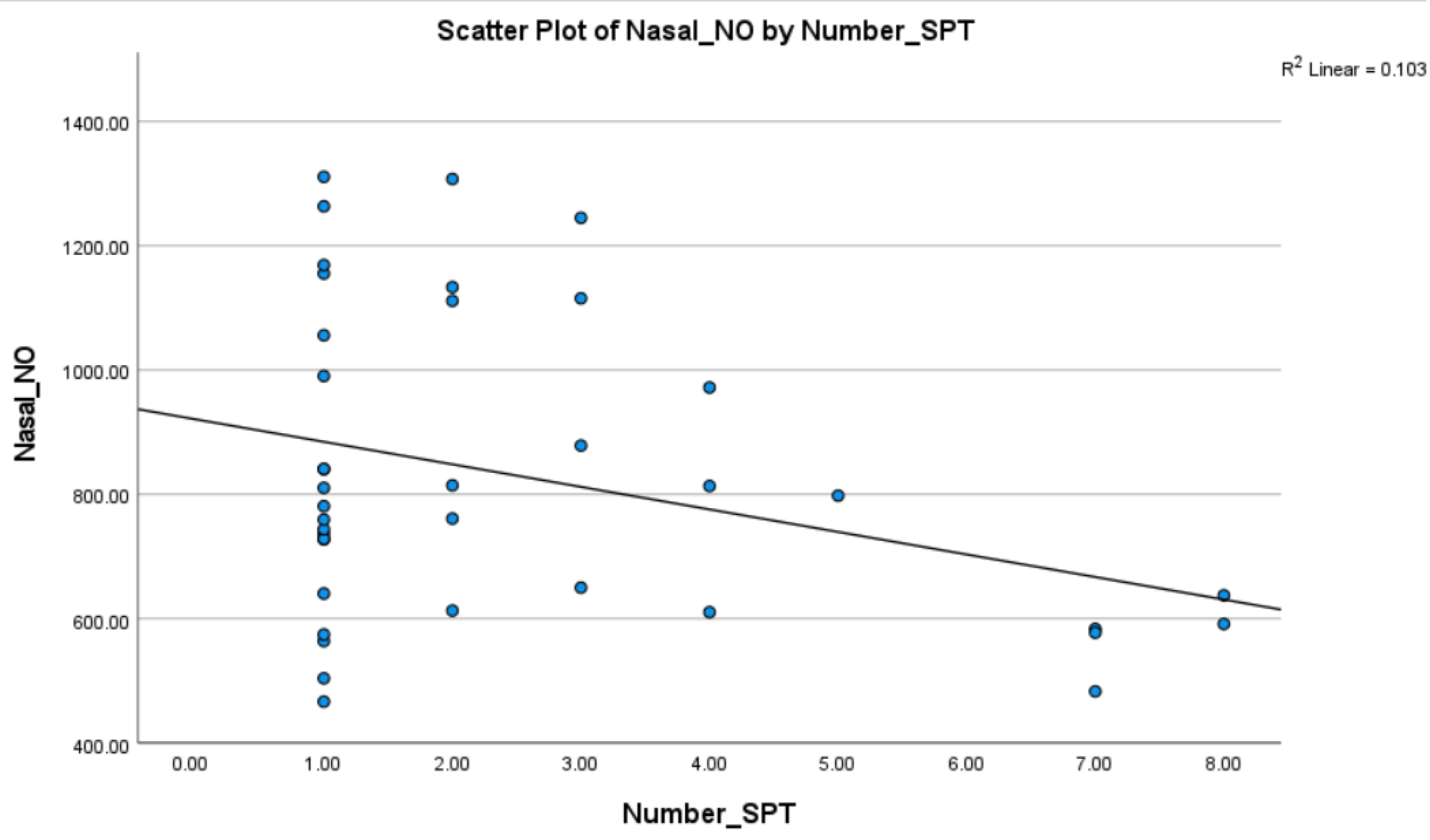
| Number of sensitizations; median (range) | 2 (1-8) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Published by MDPI on behalf of the Lithuanian University of Health Sciences. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Louca, N.; Damianou, D.; Kostea, N.; Kouis, P.; Yiallouros, P.; Pitsios, C. Assessing Nasal Nitric Oxide in Allergic Rhinitis: A Controversial Biomarker. Medicina 2025, 61, 516. https://doi.org/10.3390/medicina61030516
Louca N, Damianou D, Kostea N, Kouis P, Yiallouros P, Pitsios C. Assessing Nasal Nitric Oxide in Allergic Rhinitis: A Controversial Biomarker. Medicina. 2025; 61(3):516. https://doi.org/10.3390/medicina61030516
Chicago/Turabian StyleLouca, Natalia, Despina Damianou, Nektaria Kostea, Panayiotis Kouis, Panayiotis Yiallouros, and Constantinos Pitsios. 2025. "Assessing Nasal Nitric Oxide in Allergic Rhinitis: A Controversial Biomarker" Medicina 61, no. 3: 516. https://doi.org/10.3390/medicina61030516
APA StyleLouca, N., Damianou, D., Kostea, N., Kouis, P., Yiallouros, P., & Pitsios, C. (2025). Assessing Nasal Nitric Oxide in Allergic Rhinitis: A Controversial Biomarker. Medicina, 61(3), 516. https://doi.org/10.3390/medicina61030516








