Echocardiographic Left Ventricular Function in the Third Year After COVID-19 Hospitalization: A Follow-Up Pilot Study in South-East of Romania
Abstract
1. Introduction
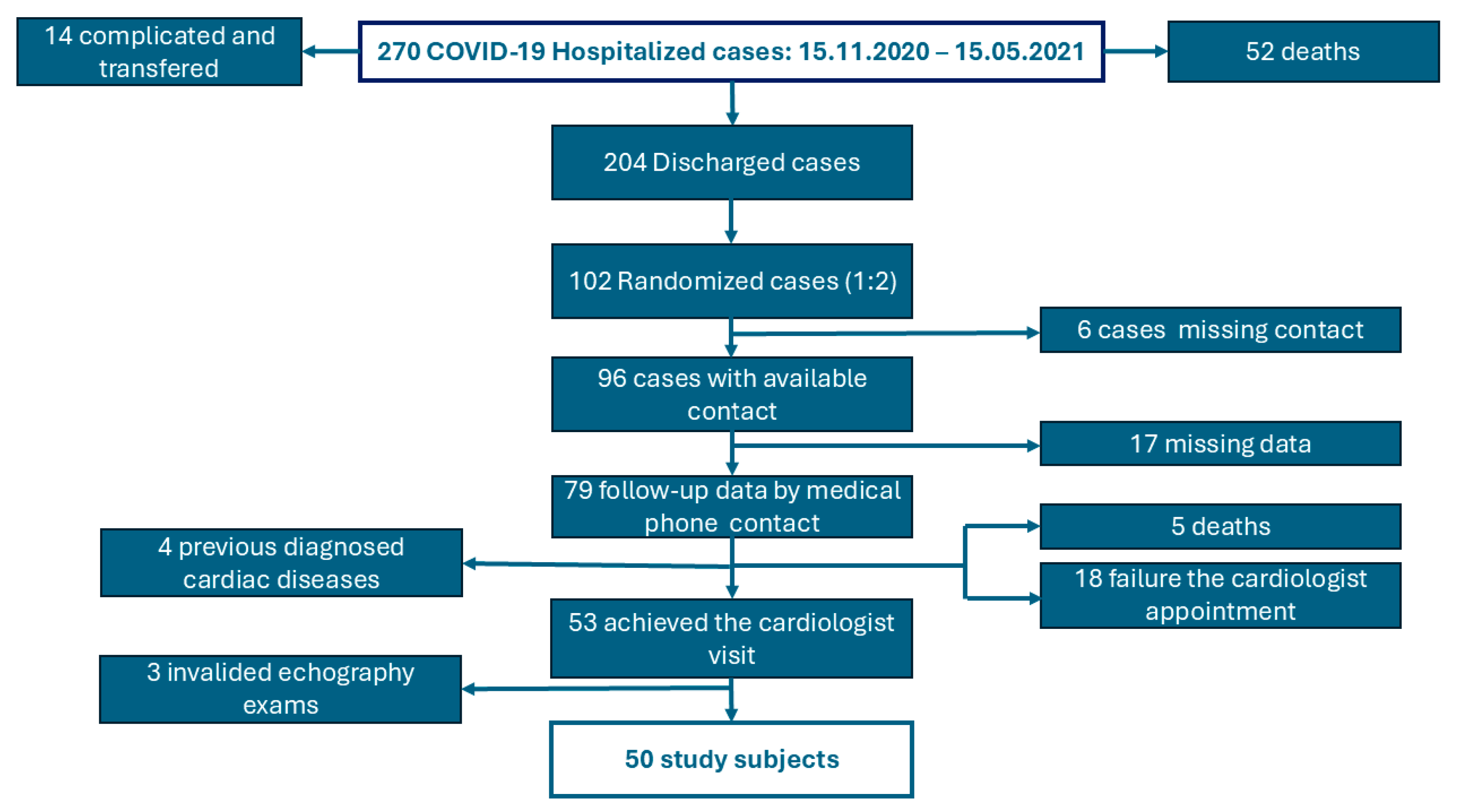
2. Materials and Methods
3. Results
3.1. Epidemiological and Clinical Characteristics of the COVID-19 Hospitalized Patients
3.2. Imaging and Biological Markers of Severity/Prognosis of the COVID-19 Episode
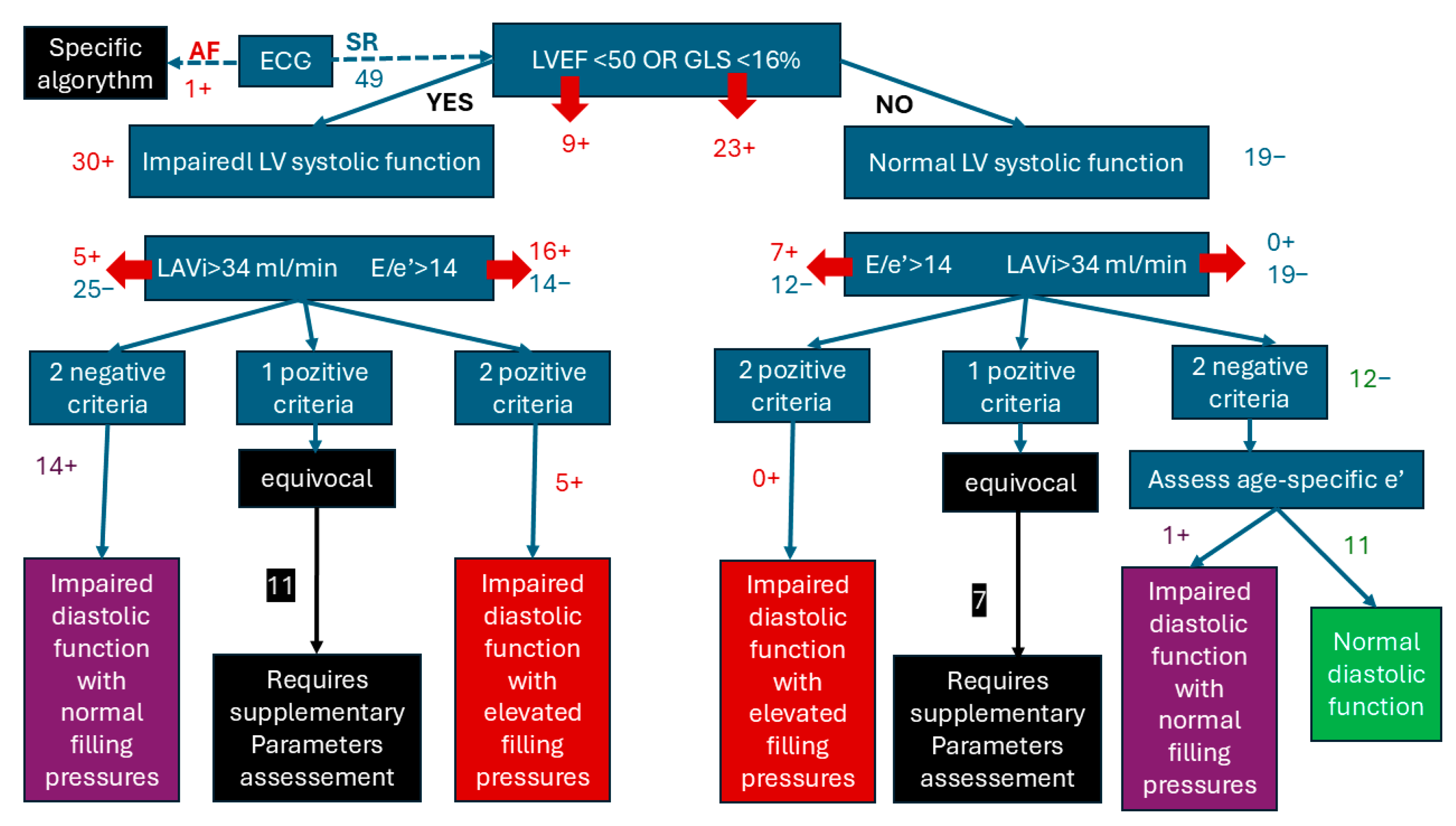
3.3. Echocardiographic Characteristics After COVID-19
3.4. Comparation of LV Dysfunction and Normal LV Function Related to COVID-19 Severity
4. Discussion
The Limits of the Study
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
| LVEF | Sex | |
|---|---|---|
| Male | Female | |
| Normal | 52–72% | 54–74% |
| Mild decreased | 41–51% | 41–53% |
| Middle decreased | 30–40% | 30–40% |
| Severe decreased | <30% | <30% |
| Age (Years Old) | <40 | 40–49 | 50–59 | 60–69 | ≥70 | ||
|---|---|---|---|---|---|---|---|
| GLS-2D | Male | Range | [−16; −23.5] | [−16.5; −23.7] | [−15.8; −23.1] | [−15.3; −22.6] | [−14.3; −22.7] |
| Average | −19.8 | −20.1 | −19.5 | −18.9 | −18.5 | ||
| Female | Range | [−17.8; −24.9] | [−16.7; −25.3] | [−17; −24] | [−15.7; −23.7] | [−15; −22.9] | |
| Average | −21.3 | −21 | −20.5 | −19.7 | −19 | ||
| Age | 18–40 y | 41–65 y | >65 y | |
|---|---|---|---|---|
| Sex | Male | Female | All | All |
| E/A ratio | <0.9 | <1.1 | <0.7 | <0.5 |
| E velocity (m/s) | <0.5 | <0.6 | <0.5 | <0.4 |
| Septal e′ (cm/s) | <7.0 | <8.0 | <5.0 | <4.0 |
| Lateral e′ (cm/s) | <9.0 | <11.0 | <6.0 | <5.0 |
| Severe (n1) | Middle (n2) | OR | p (χ2) | CI 0.95 | ||
|---|---|---|---|---|---|---|
| Gender | F M | 4 10 | 16 20 | 2.00 | 0.303 | 0.5330; 7.491 |
| Age | >65 <65 | 5 9 | 18 18 | 0.555 | 0.362 | 0.156; 1.970 |
| Smoking | YES NO | 3 11 | 8 28 | 0.954 | 0.951 | 0.213; 4.273 |
| Hypertension | YES NO | 6 8 | 15 21 | 1.05 | 0.938 | 0.301; 3.660 |
| Obesity | YES NO | 5 9 | 13 23 | 0.982 | 0.979 | 0.271; 3.561 |
| Diabetes | YES NO | 2 12 | 7 29 | 0.690 | 0.669 | 0.125; 3.790 |
| CT Score > 50% | YES NO | 13 1 | 1 35 | 455 | <0.001 | 69.202; 2991.581 |
| NLR > 6 | YES NO | 10 4 | 9 27 | 7.5 | 0.002 | 2.043; 27.53 |
| CRP > 75 | YES NO | 8 6 | 10 26 | 3.466 | 0.050 | 0.988; 12.15 |
| D-Dimers > 1000 | YES NO | 5 9 | 8 28 | 1.94 | 0.328 | 0.511; 7.385 |
References
- Flores, R.; Pires, O.; Alves, J.; Pereira, V.H. An Echocardiographic Insight into Post-COVID-19 Symptoms. Cureus 2023, 15, e38039. [Google Scholar] [CrossRef] [PubMed]
- Giustino, G.; Croft, L.B.; Stefanini, G.G.; Bragato, R.; Silbiger, J.J.; Vicenzi, M.; Danilov, T.; Kukar, N.; Shaban, N.; Kini, A.; et al. Characterization of Myocardial Injury in Patients With COVID-19. J. Am. Coll. Cardiol. 2020, 76, 2043–2055. [Google Scholar] [CrossRef]
- DePace, N.L.; Colombo, J. Long-COVID Syndrome and the Cardiovascular System: A Review of Neurocardiologic Effects on Multiple Systems. Curr. Cardiol. Rep. 2022, 24, 1711–1726. [Google Scholar] [CrossRef] [PubMed]
- Arbune, M.; Iancu, A.V.; Lupasteanu, G.; Vasile, M.C.; Stefanescu, V. A Challenge of COVID-19: Associated Infective Endocarditis with. Medicina 2021, 57, 1298. [Google Scholar] [CrossRef] [PubMed]
- Tsampasian, V.; Bäck, M.; Bernardi, M.; Cavarretta, E.; Dębski, M.; Gati, S.; Hansen, D.; Kränkel, N.; Koskinas, K.; Niebauer, J.; et al. Cardiovascular disease as part of Long COVID: A systematic review. Eur. J. Prev. Cardiol. 2024, 1–14. [Google Scholar] [CrossRef]
- Popovici, G.C.; Georgescu, C.V.; Vasile, M.C.; Vlase, C.M.; Arbune, A.A.; Arbune, M. Obstructive Sleep Apnea after COVID-19: An Observational Study. Life 2024, 14, 1052. [Google Scholar] [CrossRef] [PubMed]
- Soriano, J.B.; Murthy, S.; Marshall, J.C.; Relan, P.; Diaz, J.V. A clinical case definition of post-COVID-19 condition by a Delphi consensus. Lancet Infect. Dis. 2022, 22, e102–e107. [Google Scholar] [CrossRef]
- Peter, R.S.; Nieters, A.; Kräusslich, H.G.; Brockmann, S.O.; Göpel, S.; Kindle, G.; Merle, U.; Steinacker, J.M.; Rothenbacher, D.; Kern, W.V.; et al. Post-acute sequelae of covid-19 six to 12 months after infection: Population based study. BMJ 2022, 379, e071050. [Google Scholar] [CrossRef] [PubMed]
- Goerlich, E.; Chung, T.H.; Hong, G.H.; Metkus, T.S.; Gilotra, N.A.; Post, W.S.; Hays, A.G. Cardiovascular effects of the post-COVID-19 condition. Nat. Cardiovasc. Res. 2024, 3, 118–129. [Google Scholar] [CrossRef] [PubMed]
- Adeghate, E.A.; Eid, N.; Singh, J. Mechanisms of COVID-19-induced heart failure: A short review. Heart Fail. Rev. 2021, 26, 363–369. [Google Scholar] [CrossRef]
- Zeng, J.H.; Wu, W.B.; Qu, J.X.; Wang, Y.; Dong, C.F.; Luo, Y.F.; Zhou, D.; Feng, W.X.; Feng, C. Cardiac manifestations of COVID-19 in Shenzhen, China. Infection 2020, 48, 861–870. [Google Scholar] [CrossRef]
- Puntmann, V.O.; Carerj, M.L.; Wieters, I.; Fahim, M.; Arendt, C.; Hoffmann, J.; Shchendrygina, A.; Escher, F.; Vasa-Nicotera, M.; Zeiher, A.M.; et al. Outcomes of Cardiovascular Magnetic Resonance Imaging in Patients Recently Recovered From Coronavirus Disease 2019 (COVID-19). JAMA Cardiol. 2020, 5, 1265–1273. [Google Scholar] [CrossRef]
- Kersten, J.; Schellenberg, J.; Jerg, A.; Kirsten, J.; Persch, H.; Liu, Y.; Steinacker, J.M. Strain Echocardiography in Acute COVID-19 and Post-COVID Syndrome: More than Just a Snapshot. Biomedicines 2023, 11, 1236. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Clinical Management of COVID-19: Interim Guidance, 27 May 2020; World Health Organization: Geneva, Switzerland, 2020; Available online: https://iris.who.int/handle/10665/332196 (accessed on 14 December 2021).
- Russell, F.M.; Reyburn, R.; Chan, J.; Tuivaga, E.; Lim, R.; Lai, J.; Van, H.M.T.; Choummanivong, M.; Sychareun, V.; Khanh, D.K.T.; et al. Impact of the change in WHO’s severe pneumonia case definition on hospitalized pneumonia epidemiology: Case studies from six countries. Bull. World Health Organ. 2019, 97, 386–393. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. COVID-19 Clinical Management: Living Guidance, 25 January 2021; World Health Organization: Geneva, Switzerland, 2021; Available online: https://iris.who.int/handle/10665/338882 (accessed on 12 November 2022).
- World Health Organization. International Statistical Classification of Diseases and Related Health Problems 10th Revision. Available online: https://icd.who.int/browse10/2019/en (accessed on 12 September 2024).
- Pan, F.; Ye, T.; Sun, P.; Gui, S.; Liang, B.; Li, L.; Zheng, D.; Wang, J.; Hesketh, R.L.; Yang, L.; et al. Time Course of Lung Changes at Chest CT during Recovery from Coronavirus Disease 2019 (COVID-19). Radiology 2020, 295, 715–721. [Google Scholar] [CrossRef] [PubMed]
- Francone, M.; Iafrate, F.; Masci, G.M.; Coco, S.; Cilia, F.; Manganaro, L.; Panebianco, V.; Andreoli, C.; Colaiacomo, M.C.; Zingaropoli, M.A.; et al. Chest CT score in COVID-19 patients: Correlation with disease severity and short-term prognosis. Eur. Radiol. 2020, 30, 6808–6817. [Google Scholar] [CrossRef]
- Mruk, B.; Plucińska, D.; Walecki, J.; Półtorak-Szymczak, G.; Sklinda, K. Chest Computed Tomography (CT) Severity Scales in COVID-19 Disease: A Validation Study. Med. Sci. Monit. 2021, 27, e931283. [Google Scholar] [CrossRef]
- Kwee, T.C.; Kwee, R.M. Chest CT in COVID-19: What the Radiologist Needs to Know. Radiographics 2020, 40, 1848–1865, Erratum in: Radiographics 2022, 42, E32. [Google Scholar] [CrossRef]
- Liu, Y.; Du, X.; Chen, J.; Jin, Y.; Peng, L.; Wang, H.H.X.; Luo, M.; Chen, L.; Zhao, Y. Neutrophil-to-lymphocyte ratio as an independent risk factor for mortality in hospitalized patients with COVID-19. J. Infect. 2020, 81, e6–e12. [Google Scholar] [CrossRef] [PubMed]
- Forget, P.; Khalifa, C.; Defour, J.P.; Latinne, D.; Van Pel, M.C.; De Kock, M. What is the normal value of the neutrophil-to-lymphocyte ratio? BMC Res. Notes 2017, 10, 12. [Google Scholar] [CrossRef]
- La Torre, G.; Marte, M.; Massetti, A.P.; Carli, S.M.; Romano, F.; Mastroianni, C.M.; Minorenti, M.; Alessandri, F.; Ajassa, C.; Fusconi, M.; et al. The neutrophil/lymphocyte ratio as a prognostic factor in COVID-19 patients: A case-control study. Eur. Rev. Med. Pharmacol. Sci. 2022, 26, 1056–1064. [Google Scholar] [CrossRef]
- Sattar, Y.; Chhabra, L. Electrocardiogram. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2023. [Google Scholar] [PubMed]
- Van Gelder, I.C.; Rienstra, M.; Bunting, K.V.; Casado-Arroyo, R.; Caso, V.; Crijns, H.J.G.M.; De Potter, T.J.R.; Dwight, J.; Guasti, L.; Hanke, T.; et al. 2024 ESC Guidelines for the management of atrial fibrillation developed in collaboration with the European Association for Cardio-Thoracic Surgery (EACTS). Eur. Heart J. 2024, 45, 3314–3414. [Google Scholar] [CrossRef]
- Robinson, S.; Rana, B.; Oxborough, D.; Steeds, R.; Monaghan, M.; Stout, M.; Pearce, K.; Harkness, A.; Ring, L.; Paton, M.; et al. A practical guideline for performing a comprehensive transthoracic echocardiogram in adults: The British Society of Echocardiography minimum dataset. Echo Res. Pract. 2020, 7, G59–G93. [Google Scholar] [CrossRef]
- Smiseth, O.A.; Morris, D.A.; Cardim, N.; Cikes, M.; Delgado, V.; Donal, E.; Flachskampf, F.A.; Galderisi, M.; Gerber, B.L.; Gimelli, A.; et al. Multimodality imaging in patients with heart failure and preserved ejection fraction: An expert consensus document of the European Association of Cardiovascular Imaging. Eur. Heart J. Cardiovasc. Imaging 2022, 23, e34–e61. [Google Scholar] [CrossRef] [PubMed]
- Singh, A.; Carvalho Singulane, C.; Miyoshi, T.; Prado, A.D.; Addetia, K.; Bellino, M.; Daimon, M.; Gutierrez Fajardo, P.; Kasliwal, R.R.; Kirkpatrick, J.N.; et al. Normal Values of Left Atrial Size and Function and the Impact of Age: Results of the World Alliance Societies of Echocardiography Study. J. Am. Soc. Echocardiogr. 2022, 35, 154–164.e153. [Google Scholar] [CrossRef] [PubMed]
- Mangia, M.; D’Andrea, E.; Cecchetto, A.; Beccari, R.; Mele, D.; Nistri, S. Current and Clinically Relevant Echocardiographic Parameters to Analyze Left Atrial Function. J. Cardiovasc. Dev. Dis. 2024, 11, 241. [Google Scholar] [CrossRef]
- Kosaraju, A.; Goyal, A.; Grigorova, Y.; Makaryus, A.N. Left Ventricular Ejection Fraction. 24 April 2023. In StatPearls [Internet]; StatPearls Publishing: Treasure Island, FL, USA, 2024. [Google Scholar] [PubMed]
- Mitter, S.S.; Shah, S.J.; Thomas, J.D. A Test in Context: E/A and E/e’ to Assess Diastolic Dysfunction and LV Filling Pressure. J. Am. Coll. Cardiol. 2017, 69, 1451–1464. [Google Scholar] [CrossRef] [PubMed]
- Sartorio, A.; Cristin, L.; Pont, C.D.; Farzaneh-Far, A.; Romano, S. Global longitudinal strain as an early marker of cardiac damage after cardiotoxic medications, a state of the art review. Prog. Cardiovasc. Dis. 2025, in press. [CrossRef]
- Nyberg, J.; Jakobsen, E.O.; Østvik, A.; Holte, E.; Stølen, S.; Lovstakken, L.; Grenne, B.; Dalen, H. Echocardiographic Reference Ranges of Global Longitudinal Strain for All Cardiac Chambers Using Guideline-Directed Dedicated Views. JACC Cardiovasc. Imaging 2023, 16, 1516–1531. [Google Scholar] [CrossRef]
- Khan, F.H.; Zhao, D.; Ha, J.W.; Nagueh, S.F.; Voigt, J.U.; Klein, A.L.; Gude, E.; Broch, K.; Chan, N.; Quill, G.M.; et al. Evaluation of left ventricular filling pressure by echocardiography in patients with atrial fibrillation. Echo Res. Pract. 2024, 11, 14. [Google Scholar] [CrossRef] [PubMed]
- Stefani, L.; Brown, P.; Gerges, M.; Emerson, P.; Ferkh, A.; Kairaitis, K.; Gilroy, N.; Altman, M.; Thomas, L. Echocardiographic Assessment in Patients Recovered from Acute COVID-19 Illness. J. Cardiovasc. Dev. Dis. 2023, 10, 349. [Google Scholar] [CrossRef] [PubMed]
- Vera-Pineda, R.; Carrizales-Sepúlveda, E.F.; Morales-Rendón, E.J.; Ordaz-Farías, A.; Solís, J.G.; Benavides-González, M.A.; Flores-Ramírez, R. Echocardiographic manifestations during the first 3 months after an episode of COVID-19 and their relationship with disease severity and persistence of symptoms. Am. J. Med. Sci. 2023, 366, 32–37. [Google Scholar] [CrossRef] [PubMed]
- Shafi, A.M.A.; Shaikh, S.A.; Shirke, M.M.; Iddawela, S.; Harky, A. Cardiac manifestations in COVID-19 patients-A systematic review. J. Card. Surg. 2020, 35, 1988–2008. [Google Scholar] [CrossRef] [PubMed]
- Matejova, G.; Radvan, M.; Bartecku, E.; Kamenik, M.; Koc, L.; Horinkova, J.; Sykorova, L.; Stepanova, R.; Kala, P. Cardiac sequelae after COVID-19: Results of a 1-year follow-up study with echocardiography and biomarkers. Front. Cardiovasc. Med. 2022, 9, 1067943. [Google Scholar] [CrossRef] [PubMed]
- Garcia-Zamora, S.; Picco, J.M.; Lepori, A.J.; Galello, M.I.; Saad, A.K.; Ayón, M.; Monga-Aguilar, N.; Shehadeh, I.; Manganiello, C.F.; Izaguirre, C.; et al. Abnormal echocardiographic findings after COVID-19 infection: A multicenter registry. Int. J. Cardiovasc. Imaging 2023, 39, 77–85. [Google Scholar] [CrossRef] [PubMed]
- Olszanecka, A.; Wojciechowska, W.; Bednarek, A.; Kusak, P.; Wizner, B.; Terlecki, M.; Stolarz-Skrzypek, K.; Klocek, M.; Drożdż, T.; Sładek, K.; et al. Serial echocardiographic evaluation of COVID-19 patients without prior history of structural heart disease: A 1-year follow-up CRACoV-HHS study. Front. Cardiovasc. Med. 2023, 10, 1230669. [Google Scholar] [CrossRef]
- Tamariz, L.; Ryan, M.; Marzouka, G.R.; Bast, E.; Klimas, N.; Palacio, A. Cardiovascular risk factors predictwho should have echocardiographic evaluation in long COVID. Echocardiography 2024, 41, e15745. [Google Scholar] [CrossRef]
- Brady, B.; King, G.; Murphy, R.T.; Walsh, D. Myocardial strain: A clinical review. Ir. J. Med. Sci. 2023, 192, 1649–1656. [Google Scholar] [CrossRef]
- Henein, M.Y.; Pilebro, B.; Lindqvist, P. Echocardiographic red flags of ATTR cardiomyopathy a single centre validation. Eur. Heart J. Imaging Methods Pract. 2024, 2, qyae105. [Google Scholar] [CrossRef] [PubMed]
- Negishi, T.; Thavendiranathan, P.; Negishi, K.; Marwick, T.H. Rationale and Design of the Strain Surveillance of Chemotherapy for Improving Cardiovascular Outcomes: The SUCCOUR Trial. JACC Cardiovasc. Imaging 2018, 11, 1098–1105. [Google Scholar] [CrossRef] [PubMed]
- Wibowo, A.; Pranata, R.; Astuti, A.; Tiksnadi, B.B.; Martanto, E.; Martha, J.W.; Purnomowati, A.; Akbar, M.R. Left and right ventricular longitudinal strains are associated with poor outcome in COVID-19: A systematic review and meta-analysis. J. Intensive Care 2021, 9, 9. [Google Scholar] [CrossRef] [PubMed]
- Huang, L.; Zhao, P.; Tang, D.; Zhu, T.; Han, R.; Zhan, C.; Liu, W.; Zeng, H.; Tao, Q.; Xia, L. Cardiac Involvement in Patients Recovered From COVID-2019 Identified Using Magnetic Resonance Imaging. JACC Cardiovasc. Imaging 2020, 13, 2330–2339. [Google Scholar] [CrossRef] [PubMed]
- Miyoshi, T.; Addetia, K.; Citro, R.; Daimon, M.; Desale, S.; Fajardo, P.G.; Kasliwal, R.R.; Kirkpatrick, J.N.; Monaghan, M.J.; Muraru, D.; et al. Left Ventricular Diastolic Function in Healthy Adult Individuals: Results of the World Alliance Societies of Echocardiography Normal Values Study. J. Am. Soc. Echocardiogr. 2020, 33, 1223–1233. [Google Scholar] [CrossRef]
| N = 50 | Option | n | % | p | CI 0.95 |
|---|---|---|---|---|---|
| Sex | Male Female | 30 20 | 60% 40% | 0.202 | 0.264; 0.549 |
| Age | >65 years old <65 years old | 23 27 | 46% 54% | 0.671 | 0.393; 0.682 |
| Living area | Rural Urban | 2 48 | 4% 96% | <0.001 | 0.862; 0.995 |
| Education level | 2nd Education Upper 2nd Education High Education | 13 26 11 | 26% 52% 22% | 0.887 | 0.374; 0.664 |
| Professional status | Retired Employed Unemployed | 25 20 5 | 50% 40% 10% | <0.001 | 0.033; 0.219 |
| Smoking | Yes No | 11 39 | 22% 78% | <0.001 | 0.64; 0.884 |
| Hypertension | Yes No | 21 29 | 42% 58% | 0.322 | 0.281; 0.568 |
| Obesity | Yes No | 18 32 | 36% 64% | 0.064 | 0.491; 0.771 |
| Diabetes | Yes No | 9 41 | 18% 82% | <0.001 | 0.685; 0.914 |
| CVD | Yes No | 4 46 | 8% 92% | <0.001 | 0.842; 0.997 |
| CLD | Yes No | 3 47 | 6% 94% | <0.001 | 0.872; 1.007 |
| CKD | Yes No | 1 49 | 2% 98% | <0.001 | 0.893; 0.999 |
| COPD | Yes No | 1 49 | 2% 98% | <0.001 | 0.893; 0.999 |
| Other CID | Yes No | 8 42 | 16% 84% | <0.001 | 0.017; 0.292 |
| NV | Hospitalized Patients with COVID-19 | ||||
|---|---|---|---|---|---|
| No | Average ± SD | Median | Min; Max | ||
| WBC [/µL] | 4–10 × 103/µL | 49 | 6.798 ± 3.25 | 6.2 | 1.5; 16.1 |
| NLR | <3.5 | 48 | 6.51 ± 4.79 | 5.49 | 1.15; 24.97 |
| CRP [mg/dL] | <0.1 | 41 | 75.67 ± 58.36 | 56.6 | 3.4; 186.1 |
| ESR [mm/h] | 0–10 | 36 | 77.75 ± 34.80 | 75.5 | 12; 140 |
| D-DIMERS [ng/mL] | 0–200 | 21 | 939.49 ± 687.72 | 785.72 | 97.25; 3290 |
| FERITINE [µg/L] | <300 (♂) <150 (♀) | 35 | 666.18 ± 377.97 | 696.56 | 58.8; 1200 |
| CREATININE [mg/dL] | 0.5–1.1 (♂) 0.6–1.2 (♀) | 47 | 0.90 ± 0.40 | 0.84 | 0.44; 3.28 |
| N = 50 | Normal | Low | High | p * | CI |
|---|---|---|---|---|---|
| LAVi | 43 (86%) | - | 7 (14%) | <0.001 | 0.761; 0.958 |
| E/A | 23 (46%) | - | 27 (54%) | 0.571 | 0.398; 0.681 |
| E/e’ | 29 (38%) | - | 21 (42%) | 0.257 | 0.279; 0.560 |
| e’ | 43 (86%) | 7 (14%) | <0.001 | 0.761; 0.958 | |
| S | 23 (46%) | 27 (54%) | - | 0.571 | 0.398; 0.681 |
| LVEF | 41 (82%) | 9 (18%) | - | <0.001 | 0.710; 0.929 |
| GLS | 27 (54%) | 23 (46%) | - | 0.571 | 0.398; 0.681 |
| N = 49 | Impaired LVF | Normal LVF | OR | p | CI 0.95 | |
|---|---|---|---|---|---|---|
| LVSF | CT-score > 50 | 7 | 7 | 0.521 | 0.307 | 0.149; 1.821 |
| N/Ly > 6 | 11 | 9 | 0.796 | 0.703 | 0.246; 2.575 | |
| CRP > 75 | 8 | 9 | 0.404 | 0.137 | 0.122; 1.338 | |
| Impaired diastolic filling pressure | CT-score > 50 | 4 | 6 | 0.25 | 0.076 | 0.053; 1.157 |
| N/Ly > 6 | 8 | 6 | 0.666 | 0.580 | 0.158; 2.812 | |
| CRP > 75 | 6 | 5 | 0.600 | 0.501 | 0.135; 2.657 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Published by MDPI on behalf of the Lithuanian University of Health Sciences. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Vlase, C.-M.; Gutu, C.; Bogdan Goroftei, R.E.; Boghean, A.; Iordachi, T.F.D.; Arbune, A.-A.; Arbune, M. Echocardiographic Left Ventricular Function in the Third Year After COVID-19 Hospitalization: A Follow-Up Pilot Study in South-East of Romania. Medicina 2025, 61, 333. https://doi.org/10.3390/medicina61020333
Vlase C-M, Gutu C, Bogdan Goroftei RE, Boghean A, Iordachi TFD, Arbune A-A, Arbune M. Echocardiographic Left Ventricular Function in the Third Year After COVID-19 Hospitalization: A Follow-Up Pilot Study in South-East of Romania. Medicina. 2025; 61(2):333. https://doi.org/10.3390/medicina61020333
Chicago/Turabian StyleVlase, Constantin-Marinel, Cristian Gutu, Roxana Elena Bogdan Goroftei, Andreea Boghean, Traian Florin Daniel Iordachi, Anca-Adriana Arbune, and Manuela Arbune. 2025. "Echocardiographic Left Ventricular Function in the Third Year After COVID-19 Hospitalization: A Follow-Up Pilot Study in South-East of Romania" Medicina 61, no. 2: 333. https://doi.org/10.3390/medicina61020333
APA StyleVlase, C.-M., Gutu, C., Bogdan Goroftei, R. E., Boghean, A., Iordachi, T. F. D., Arbune, A.-A., & Arbune, M. (2025). Echocardiographic Left Ventricular Function in the Third Year After COVID-19 Hospitalization: A Follow-Up Pilot Study in South-East of Romania. Medicina, 61(2), 333. https://doi.org/10.3390/medicina61020333








