A Meta-Analysis to Assess the Probable Association of Hypertension During Pregnancy and Placenta Accreta
Abstract
1. Background
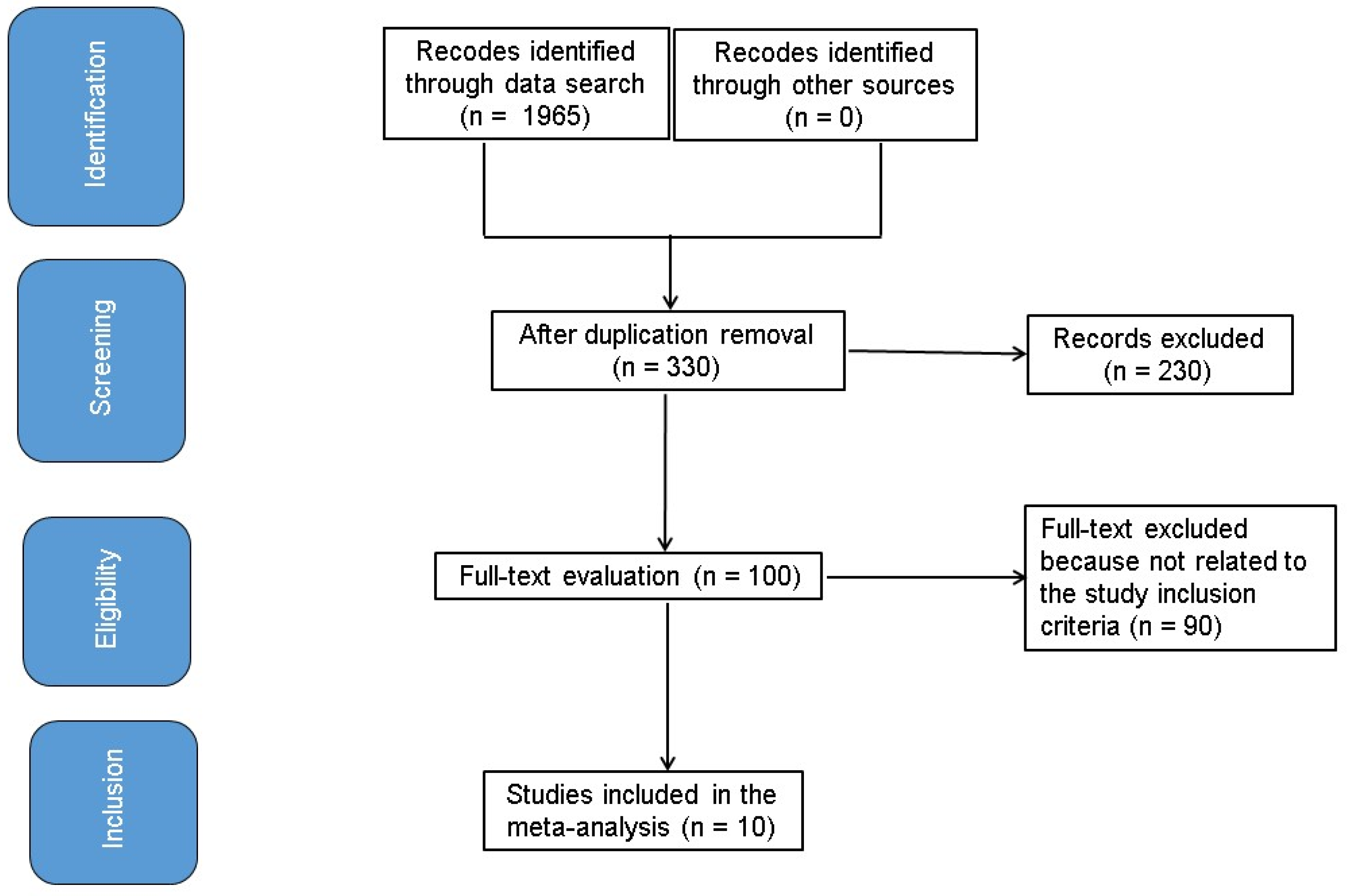
2. Methods
2.1. Eligibility Criteria
2.2. Information Sources
- The research was retrospective study.
- The focus of the populace was pregnant women.
- The study examined hypertension during pregnancy.
- The study provided the probable association between hypertension during pregnancy and PA.
- Research that did not involve a comparison between hypertensive pregnant women and a control group.
- Studies concerning conditions unrelated to PA.
- Research that did not emphasize the impact of comparative findings.
2.3. Search Strategy
2.4. Selection Process
2.5. Data Collection Process
2.6. Data Items
2.7. Study Risk of Bias Assessment
2.8. Effect Estimates
2.9. Synthesis Methods
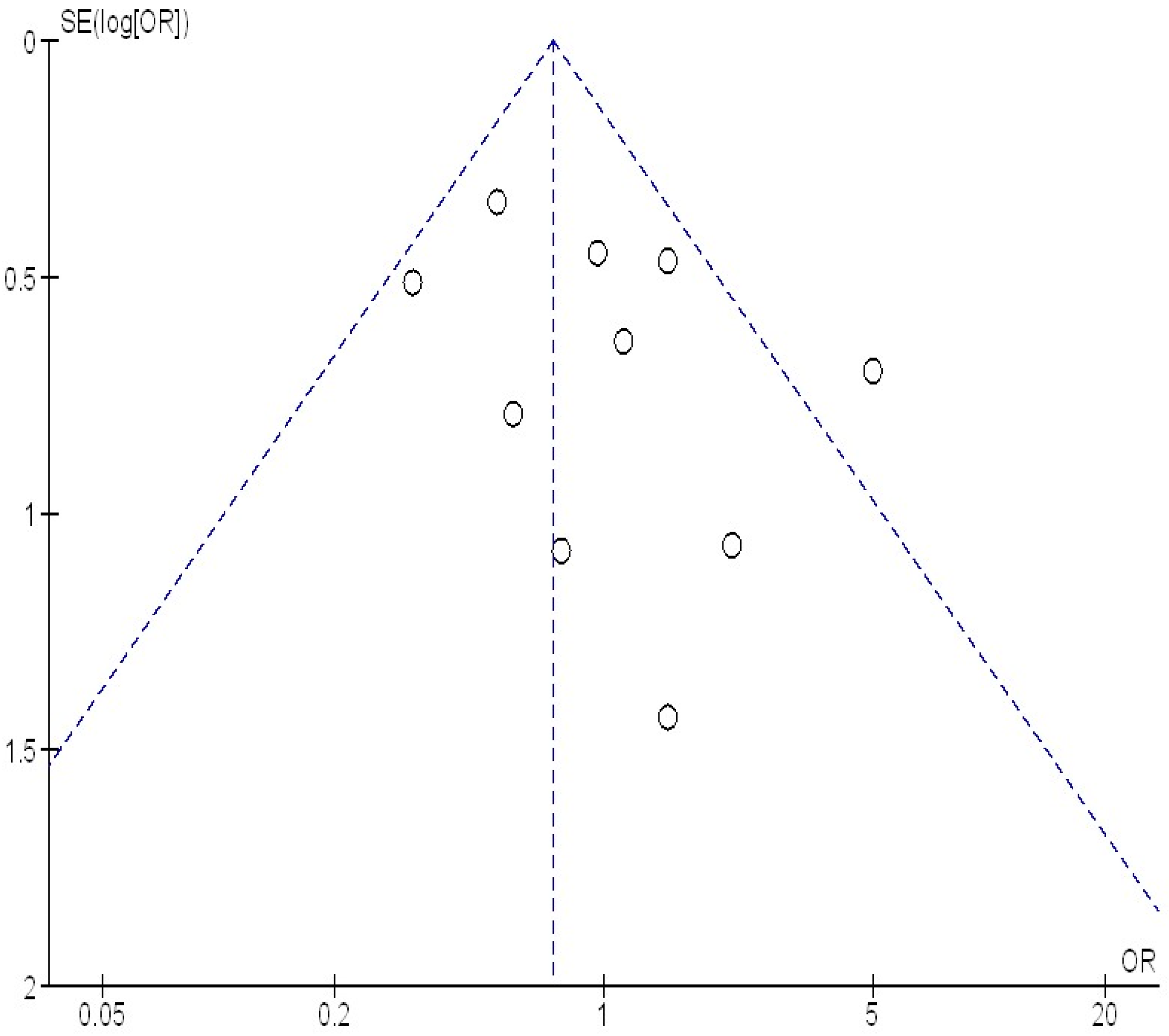
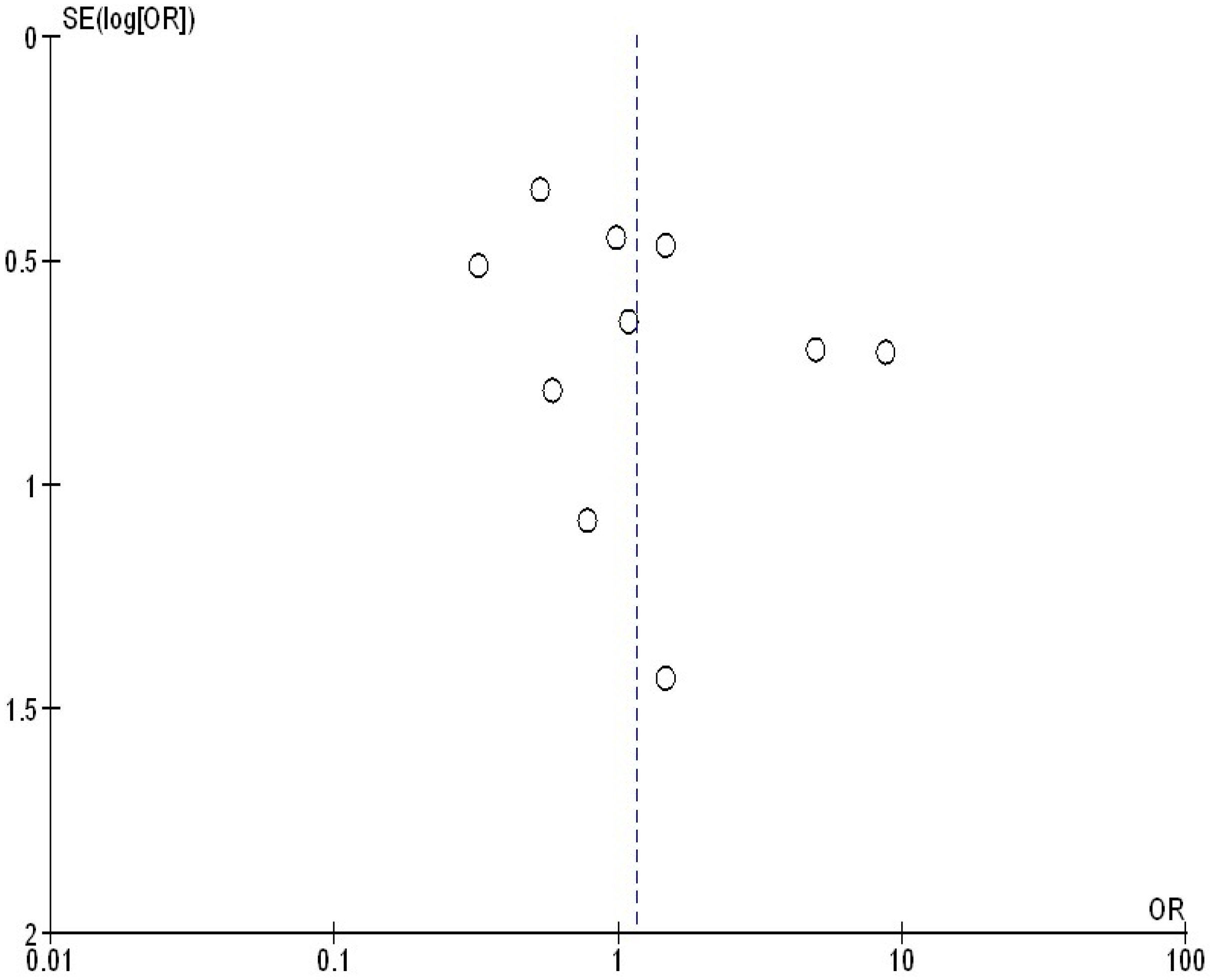
2.10. Reporting Bias Assessment
2.11. Certainty Assessment
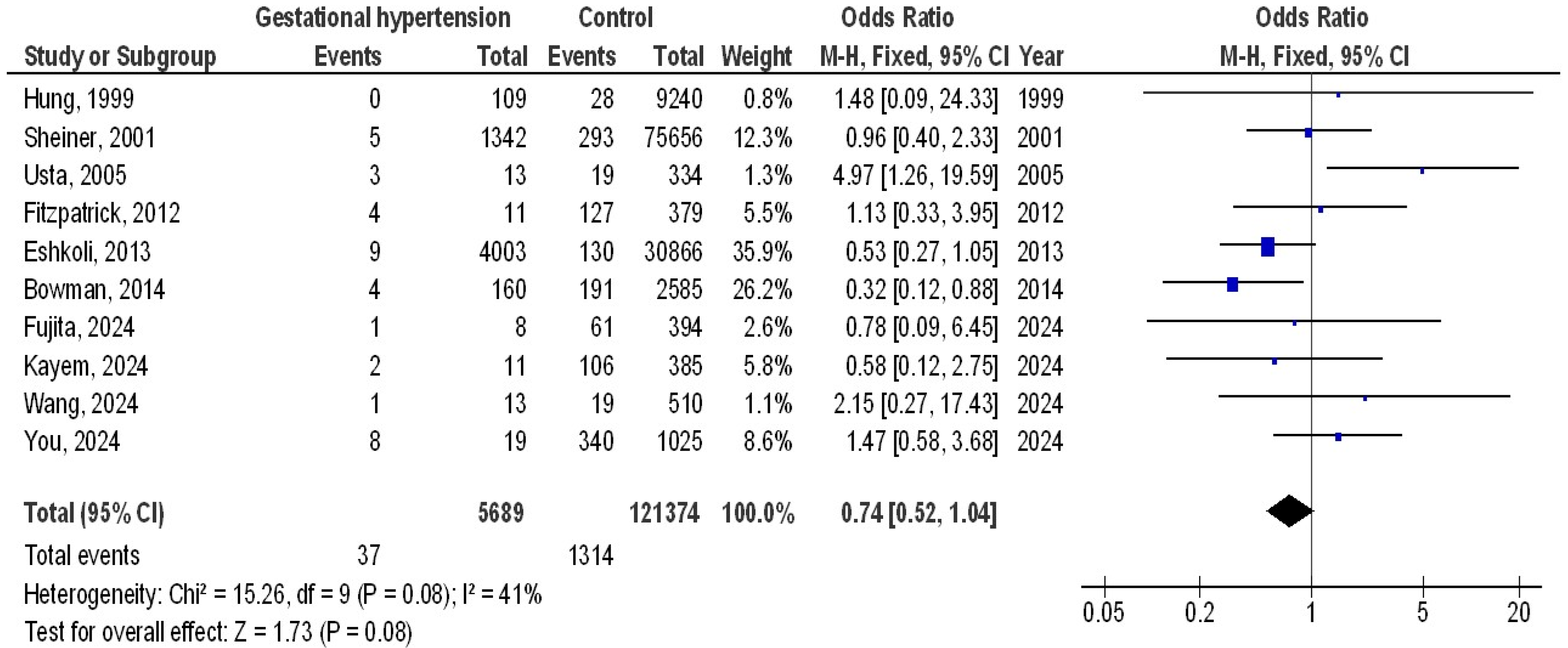
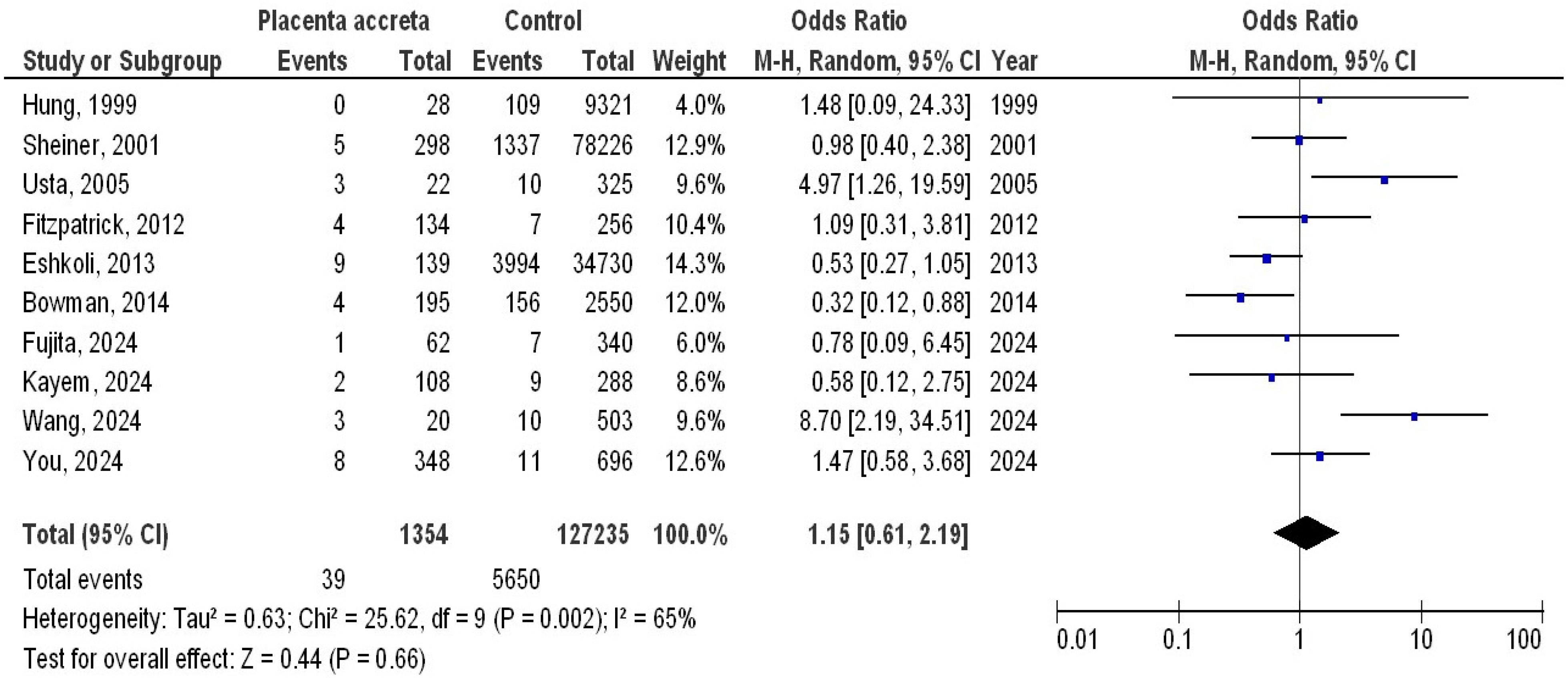
3. Results
4. Discussion
5. Limitations
6. Conclusions
Funding
Conflicts of Interest
References
- Dreux, S.; Salomon, L.J.; Muller, F.; Goffinet, F.; Oury, J.-F.; Sentilhes, L.; Group, A.S. Second-trimester maternal serum markers and placenta accreta. Prenat. Diagn. 2012, 32, 1010–1012. [Google Scholar] [CrossRef] [PubMed]
- Garmi, G.; Salim, R. Epidemiology, etiology, diagnosis, and management of placenta accreta. Obstet. Gynecol. Int. 2012, 2012, 873929. [Google Scholar] [CrossRef]
- Wu, S.; Kocherginsky, M.; Hibbard, J.U. Abnormal placentation: Twenty-year analysis. Am. J. Obstet. Gynecol. 2005, 192, 1458–1461. [Google Scholar] [CrossRef] [PubMed]
- Khong, T.; Staples, A.; Chan, A.; Keane, R.; Wilkinson, C. Pregnancies complicated by retained placenta: Sex ratio and relation to pre-eclampsia. Placenta 1998, 19, 577–580. [Google Scholar] [CrossRef]
- Gielchinsky, Y.; Rojansky, N.; Fasouliotis, S.; Ezra, Y. Placenta accreta—Summary of 10 years: A survey of 310 cases. Placenta 2002, 23, 210–214. [Google Scholar] [CrossRef]
- Usta, I.M.; Hobeika, E.M.; Musa, A.A.A.; Gabriel, G.E.; Nassar, A.H. Placenta previa-accreta: Risk factors and complications. Am. J. Obstet. Gynecol. 2005, 193, 1045–1049. [Google Scholar] [CrossRef]
- Fitzpatrick, K.E.; Sellers, S.; Spark, P.; Kurinczuk, J.J.; Brocklehurst, P.; Knight, M. Incidence and risk factors for placenta accreta/increta/percreta in the UK: A national case-control study. PLoS ONE 2012, 7, e52893. [Google Scholar] [CrossRef] [PubMed]
- Bowman, Z.S.; Eller, A.G.; Bardsley, T.R.; Greene, T.; Varner, M.W.; Silver, R.M. Risk factors for placenta accreta: A large prospective cohort. Am. J. Perinatol. 2014, 31, 799–804. [Google Scholar]
- Eshkoli, T.; Weintraub, A.Y.; Sergienko, R.; Sheiner, E. Placenta accreta: Risk factors, perinatal outcomes, and consequences for subsequent births. Am. J. Obstet. Gynecol. 2013, 208, 219.e1–219.e7. [Google Scholar] [CrossRef] [PubMed]
- Stroup, D.F.; Berlin, J.A.; Morton, S.C.; Olkin, I.; Williamson, G.D.; Rennie, D.; Moher, D.; Becker, B.J.; Sipe, T.A.; Thacker, S.B. Meta-analysis of observational studies in epidemiology: A proposal for reporting. JAMA 2000, 283, 2008–2012. [Google Scholar] [CrossRef]
- Higgins, J.P.; Thompson, S.G.; Deeks, J.J.; Altman, D.G. Measuring inconsistency in meta-analyses. Bmj 2003, 327, 557–560. [Google Scholar] [CrossRef]
- Liberati, A.; Altman, D.G.; Tetzlaff, J.; Mulrow, C.; Gøtzsche, P.C.; Ioannidis, J.P.; Clarke, M.; Devereaux, P.J.; Kleijnen, J.; Moher, D. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: Explanation and elaboration. J. Clin. Epidemiol. 2009, 62, e1–e34. [Google Scholar] [CrossRef]
- Collaboration, C. RoB 2: A Revised Cochrane Risk-of-Bias Tool for Randomized Trials. 2020. Available online: https://methods.cochrane.org/bias/resources/rob-2-revised-cochrane-risk-bias-tool-randomized-trials (accessed on 6 December 2019).
- Gupta, A.; Das, A.; Majumder, K.; Arora, N.; Mayo, H.G.; Singh, P.P.; Beg, M.S.; Singh, S. Obesity is Independently Associated With Increased Risk of Hepatocellular Cancer–related Mortality. Am. J. Clin. Oncol. 2018, 41, 874–881. [Google Scholar] [CrossRef]
- Hung, T.-H.; Shau, W.-Y.; Hsieh, C.-C.; Chiu, T.-H.; Hsu, J.-J. Risk factors for placenta accreta. Obstet. Gynecol. 1999, 93, 545–550. [Google Scholar] [PubMed]
- Sheiner, E.; Shoham-Vardi, I.; Hallak, M.; Hershkowitz, R.; Katz, M.; Mazor, M. Placenta previa: Obstetric risk factors and pregnancy outcome. J. Matern.-Fetal Med. 2001, 10, 414–419. [Google Scholar] [CrossRef] [PubMed]
- Kayem, G.; Seco, A.; Vendittelli, F.; Crenn Hebert, C.; Dupont, C.; Branger, B.; Huissoud, C.; Fresson, J.; Winer, N.; Langer, B.; et al. Risk factors for placenta accreta spectrum disorders in women with any prior cesarean and a placenta previa or low lying: A prospective population-based study. Sci. Rep. 2024, 14, 6564. [Google Scholar] [CrossRef]
- You, H.; Wang, Y.; Han, R.; Gu, J.; Zeng, L.; Zhao, Y. Risk factors for placenta accreta spectrum without prior cesarean section: A case–control study in China. Int. J. Gynecol. Obstet. 2024, 166, 1092–1099. [Google Scholar] [CrossRef]
- Wang, L.; Liu, T.; Yang, Y.; Li, Y.; Xiao, L.; Li, X.; Wei, S. Risk Factors for Peripartum Hysterectomy Among Pregnancies with Suspected Placenta Accreta Spectrum in Preoperative Obstetric Imaging Screening: A Retrospective Cohort Study. BMC Pregnancy Childbirth 2024, Preprints. [Google Scholar] [CrossRef]
- Fujita, T.; Yoshizato, T.; Mitao, H.; Shimomura, T.; Kuramoto, T.; Obara, H.; Ide, H.; Koga, F.; Kojima, K.; Nomiyama, M.; et al. Risk factors for placenta accreta spectrum in pregnancies conceived after frozen–thawed embryo transfer in a hormone replacement cycle. Eur. J. Obstet. Gynecol. Reprod. Biol. 2024, 296, 194–199. [Google Scholar] [CrossRef]
- Alves, E.; Azevedo, A.; Rodrigues, T.; Santos, A.C.; Barros, H. Impact of risk factors on hypertensive disorders in pregnancy, in primiparae and multiparae. Ann. Hum. Biol. 2013, 40, 377–384. [Google Scholar] [CrossRef]
- Lindheimer, M.D.; Taler, S.J.; Cunningham, F.G. Hypertension in pregnancy. J. Am. Soc. Hypertens. 2008, 2, 484–494. [Google Scholar] [CrossRef] [PubMed]
- Tantbirojn, P.; Crum, C.; Parast, M. Pathophysiology of placenta creta: The role of decidua and extravillous trophoblast. Placenta 2008, 29, 639–645. [Google Scholar] [CrossRef] [PubMed]
- Fan, D.; Li, S.; Wu, S.; Wang, W.; Ye, S.; Xia, Q.; Liu, L.; Feng, J.; Wu, S.; Guo, X. Prevalence of abnormally invasive placenta among deliveries in mainland China: A PRISMA-compliant Systematic Review and Meta-analysis. Medicine 2017, 96, e6636. [Google Scholar] [CrossRef]
- Basta, P.; Majka, M.; Jozwicki, W.; Lukaszewska, E.; Knafel, A.; Grabiec, M.; Stasienko, E.; Wicherek, L. The frequency of CD25+ CD4+ and FOXP3+ regulatory T cells in ectopic endometrium and ectopic decidua. Reprod. Biol. Endocrinol. 2010, 8, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Schwede, S.; Alfer, J.; Von Rango, U. Differences in regulatory T-cell and dendritic cell pattern in decidual tissue of placenta accreta/increta cases. Placenta 2014, 35, 378–385. [Google Scholar] [CrossRef] [PubMed]
- Yliniemi, A.; Makikallio, K.; Korpimaki, T.; Kouru, H.; Marttala, J.; Ryynanen, M. Combination of PAPPA, fhCGβ, AFP, PIGF, sTNFR1, and maternal characteristics in prediction of early-onset preeclampsia. Clin. Med. Insights Reprod. Health 2015, 9, CMRH. S21865. [Google Scholar] [CrossRef]
- Desai, N.; Krantz, D.; Roman, A.; Fleischer, A.; Boulis, S.; Rochelson, B. Elevated first trimester PAPP-A is associated with increased risk of placenta accreta. Prenat. Diagn. 2014, 34, 159–162. [Google Scholar] [CrossRef] [PubMed]
- Lash, G.E.; Ernerudh, J. Decidual cytokines and pregnancy complications: Focus on spontaneous miscarriage. J. Reprod. Immunol. 2015, 108, 83–89. [Google Scholar] [CrossRef]
- Feldman, D.R.; Baum, M.S.; Ginsberg, M.S.; Hassoun, H.; Flombaum, C.D.; Velasco, S.; Fischer, P.; Ronnen, E.; Ishill, N.; Patil, S. Phase I trial of bevacizumab plus escalated doses of sunitinib in patients with metastatic renal cell carcinoma. J. Clin. Oncol. 2009, 27, 1432. [Google Scholar] [CrossRef]
- McMahon, K.; Karumanchi, S.A.; Stillman, I.E.; Cummings, P.; Patton, D.; Easterling, T. Does soluble fms-like tyrosine kinase-1 regulate placental invasion? Insight from the invasive placenta. Am. J. Obstet. Gynecol. 2014, 210, 68.e1–68.e4. [Google Scholar] [CrossRef]
- Wang, W.; Fan, D.; Wang, J.; Wu, S.; Lu, Y.; He, Y.; Liu, Z. Association between hypertensive disorders complicating pregnancy and risk of placenta accreta: A meta-analysis and systematic review. Hypertens. Pregnancy 2018, 37, 168–174. [Google Scholar] [CrossRef]
- Szymusik, I.; Kosinska-Kaczynska, K.; Krowicka, M.; Sep, M.; Marianowski, P.; Wielgos, M. Perinatal outcome of in vitro fertilization singletons—10 years’ experience of one center. Arch. Med. Sci. 2019, 15, 666–672. [Google Scholar] [CrossRef]
- Li, Y.; Meng, X.; Zhou, C.; Zhou, X. Pregnancy-associated plasma protein A as a predictor of all-cause mortality and cardiovascular events in patients with chronic kidney disease: A meta-analysis of prospective studies. Arch. Med. Sci. 2020, 16, 8–15. [Google Scholar] [CrossRef]
- Fijałkowska, A.; Szczerba, E.; Szewczyk, G.; Budaj-Fidecka, A.; Burakowski, J.; Sobkowicz, B.; Nowowiejska-Wiewióra, A.; Opolski, G.; Torbicki, A.; Kurzyna, M.; et al. Pregnancy as a predictor of deviations from the recommended diagnostic pathway in women with suspected pulmonary embolism: ZATPOL registry data. Arch. Med. Sci. 2018, 14, 838–845. [Google Scholar] [CrossRef] [PubMed]
- Hao, Y.; Sun, X.; Wen, N.; Song, D.; Li, H. Effects of n-3 polyunsaturated fatty acid supplementation on pregnancy outcomes: A systematic review and meta-analysis. Arch. Med. Sci. 2021, 18, 890. [Google Scholar] [CrossRef]
| Database | Search Strategy |
|---|---|
| Pubmed | #1 “placenta accreta” [MeSH Terms] OR “preeclampsia” [All Fields] OR “hypertension” [All Fields] #2 “pregnancy” [MeSH Terms] OR “placenta accreta” [All Fields] OR “morbidly adherent placenta” [All Fields] OR “gestation” [All Fields] #3 #1 AND #2 |
| Embase | ‘placenta accreta’/exp OR ‘preeclampsia’/exp OR ‘hypertension’/exp #2 ‘pregnancy’/exp OR ‘ICBG’/exp OR ‘morbidly adherent placenta’ OR ‘gestation’ #3 #1 AND #2 |
| Cochrane Library | #1 (placenta accreta): ti,ab,kw OR (preeclampsia): ti,ab,kw OR (hypertension):ti, ab,kw (word variations were searched) #2 (pregnancy): ti,ab,kw OR (morbidly adherent placenta):ti,ab,kw OR (gestation):ti,ab,kw (word variations were searched) #3 #1 AND #2 |
| Study | Country | Total | Placenta Accreta | Hypertension |
|---|---|---|---|---|
| Hung, 1999 [15] | Taiwan | 9349 | 28 | 109 |
| Sheiner, 2001 [16] | Palestine | 78,524 | 298 | 1342 |
| Usta, 2005 [6] | Lebanon | 347 | 22 | 13 |
| Fitzpatrick, 2012 [7] | UK | 390 | 134 | 11 |
| Eshkoli, 2013 [9] | Palestine | 34,869 | 139 | 4003 |
| Bowman, 2014 [8] | USA | 2745 | 195 | 160 |
| Kayem, 2024 [17] | France | 396 | 108 | 11 |
| You, 2024 [18] | China | 1044 | 348 | 19 |
| Wang, 2024 [19] | China | 523 | 20 | 13 |
| Fujita, 2024 [20] | Japan | 402 | 62 | 8 |
| Total | 128,589 | 1354 | 4225 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Published by MDPI on behalf of the Lithuanian University of Health Sciences. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Imam, M.S.; Meshari Abdularhman Alnaim, D.; Khalid Abdullah Alaraifi, R.; Salah Saleh Alabduljabbar, J.; Abdulrahman Mohammed Alhamed, A.; Mohammed Fayadh Alansari, A.; Ali Alqarni, R.A.; Fahad Saleh Alotaibi, S.; Zuwayyid Aali Alsufyani, D.; Mohammed Abdullah Alzaidi, R.; et al. A Meta-Analysis to Assess the Probable Association of Hypertension During Pregnancy and Placenta Accreta. Medicina 2025, 61, 297. https://doi.org/10.3390/medicina61020297
Imam MS, Meshari Abdularhman Alnaim D, Khalid Abdullah Alaraifi R, Salah Saleh Alabduljabbar J, Abdulrahman Mohammed Alhamed A, Mohammed Fayadh Alansari A, Ali Alqarni RA, Fahad Saleh Alotaibi S, Zuwayyid Aali Alsufyani D, Mohammed Abdullah Alzaidi R, et al. A Meta-Analysis to Assess the Probable Association of Hypertension During Pregnancy and Placenta Accreta. Medicina. 2025; 61(2):297. https://doi.org/10.3390/medicina61020297
Chicago/Turabian StyleImam, Mohamed S., Dina Meshari Abdularhman Alnaim, Renad Khalid Abdullah Alaraifi, Juman Salah Saleh Alabduljabbar, Alanoud Abdulrahman Mohammed Alhamed, Asalah Mohammed Fayadh Alansari, Raghad Abdullah Ali Alqarni, Shouq Fahad Saleh Alotaibi, Dimah Zuwayyid Aali Alsufyani, Rana Mohammed Abdullah Alzaidi, and et al. 2025. "A Meta-Analysis to Assess the Probable Association of Hypertension During Pregnancy and Placenta Accreta" Medicina 61, no. 2: 297. https://doi.org/10.3390/medicina61020297
APA StyleImam, M. S., Meshari Abdularhman Alnaim, D., Khalid Abdullah Alaraifi, R., Salah Saleh Alabduljabbar, J., Abdulrahman Mohammed Alhamed, A., Mohammed Fayadh Alansari, A., Ali Alqarni, R. A., Fahad Saleh Alotaibi, S., Zuwayyid Aali Alsufyani, D., Mohammed Abdullah Alzaidi, R., Ali Hussain Mathkoor, S., Hameed Hamde Alotaibi, R., Abdelrahim, M. E. A., & Mohamed, B. M. E. (2025). A Meta-Analysis to Assess the Probable Association of Hypertension During Pregnancy and Placenta Accreta. Medicina, 61(2), 297. https://doi.org/10.3390/medicina61020297





