Quality of Life Following Vancouver Type B Periprosthetic Femoral Fractures: A Cross-Sectional Study
Abstract
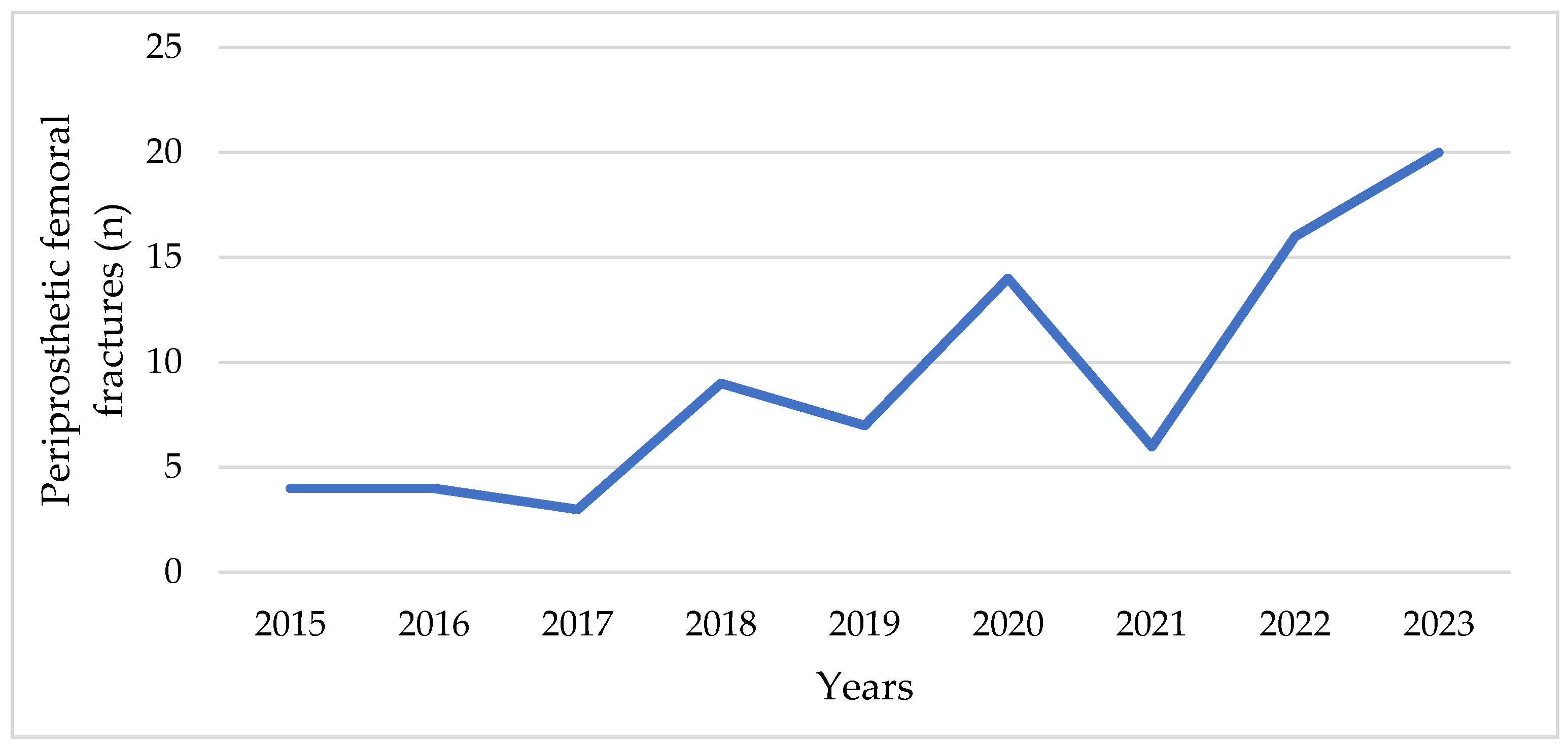
1. Introduction
The 36-Item Short Form Survey (SF-36)
2. Materials and Methods
2.1. Study Design and Eligibility Criteria
- Age ≥ 65 years
- Vancouver type B proximal PFF
- Surgical treatment at our clinic between January 2016 and December 2022
- Voluntary consent to participate
- Age < 65 years
- Death prior to follow-up
- Intraoperative fractures
- Cognitive impairment preventing independent survey completion
2.2. Quality of Life Assessment and Data Collection
2.3. Statistical Data Analysis
3. Results
3.1. Age and Quality of Life
3.2. Sex Differences
3.3. Differences in Quality of Life According to Operated Leg
3.4. Quality of Life and the Type of PFF Revision
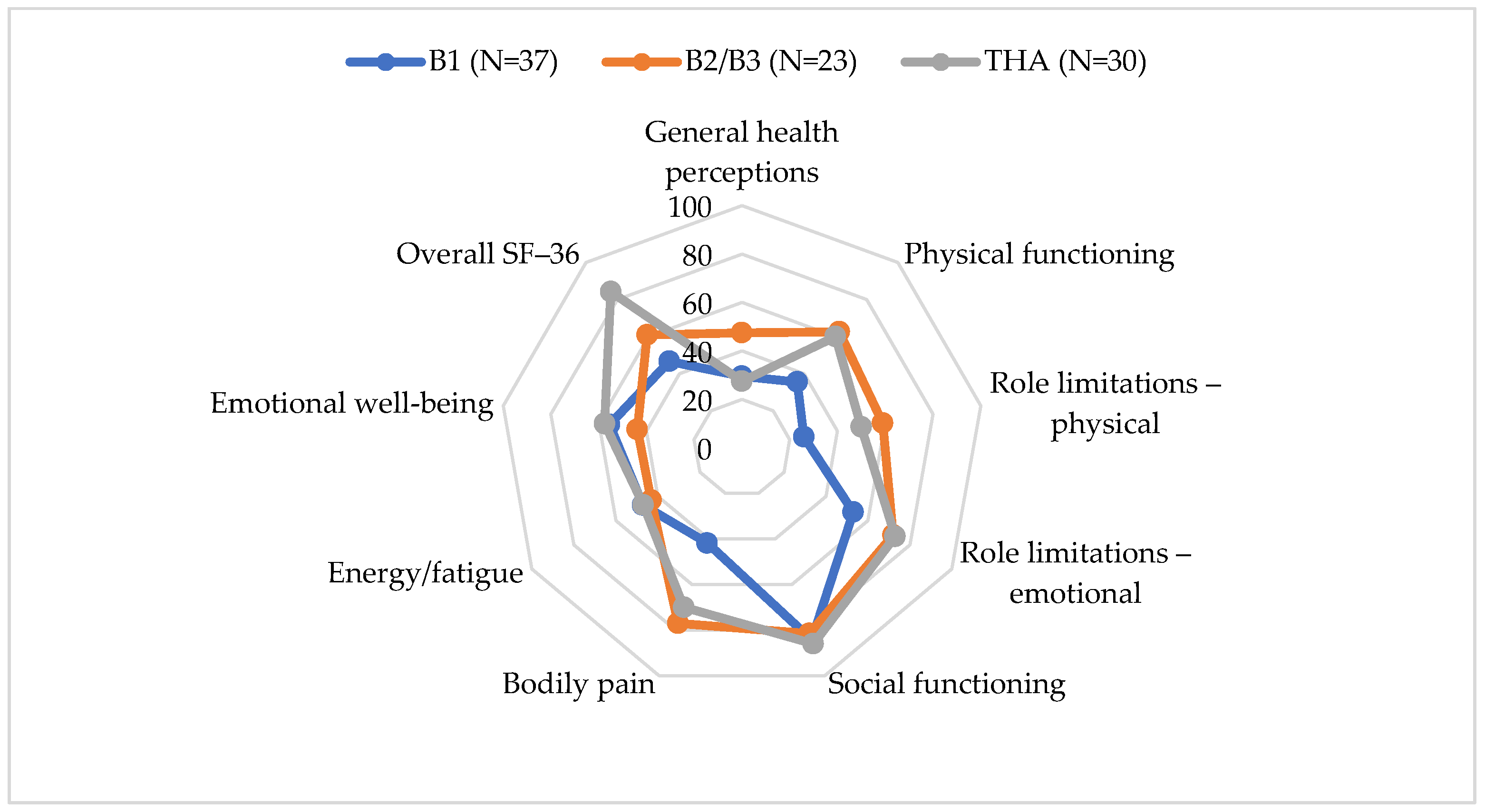
3.5. Comparison with Primary THA
4. Discussion
4.1. Clinical Implications
4.2. Study Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Garofalo, S.; Morano, C.; Bruno, L.; Pagnotta, L. A Comprehensive Literature Review for Total Hip Arthroplasty (THA): Part 2—Material Selection Criteria and Methods. J. Funct. Biomater. 2025, 16, 184. [Google Scholar] [CrossRef] [PubMed]
- Patel, I.; Nham, F.; Zalikha, A.K.; El-Othmani, M.M. Epidemiology of Total Hip Arthroplasty: Demographics, Comorbidities and Outcomes. Arthroplasty 2023, 5, 2. [Google Scholar] [CrossRef] [PubMed]
- Zhao, W.-Q.; Li, X.-S.; Fan, M.-Q.; Yao, Z.-Y.; Song, Z.-F.; Tong, P.-J.; Huang, J.-F. Surgical Treatment of Specific Unified Classification System B Fractures: Potentially Destabilising Lesser Trochanter Periprosthetic Fractures. Sci. Rep. 2023, 13, 14330. [Google Scholar] [CrossRef] [PubMed]
- Aprato, A.; Tosto, F.; Comba, A.; Mellano, D.; Piccato, A.; Daghino, W.; Massè, A. The Clinical and Economic Burden of Proximal Femur Periprosthetic Fractures. Musculoskelet. Surg. 2022, 106, 201–206. [Google Scholar] [CrossRef]
- Islam, R.; Lanting, B.; Somerville, L.; Hunter, S.W. Evaluating the Functional and Psychological Outcomes Following Periprosthetic Femoral Fracture After Total Hip Arthroplasty. Arthroplast. Today 2022, 18, 57–62. [Google Scholar] [CrossRef]
- Ben-Shlomo, Y.; Blom, A.; Boulton, C.; Brittain, R.; Clark, E.; Craig, R.; Dawson-Bowling, S.; Deere, K.; Esler, C. The National Joint Registry 16th Annual Report 2019; National Joint Registry: London, UK, 2019. [Google Scholar]
- Jones, C.M.; Acuña, A.J.; Jan, K.; Forlenza, E.M.; Della Valle, C.J. Trends and Epidemiology in Revision Total Hip Arthroplasty: A Large Database Study. J. Arthroplast. 2025, 40, S255–S261.e1. [Google Scholar] [CrossRef]
- Ding, X.; Liu, B.; Huo, J.; Liu, S.; Wu, T.; Ma, W.; Li, M.; Han, Y. Risk Factors Affecting the Incidence of Postoperative Periprosthetic Femoral Fracture in Primary Hip Arthroplasty Patients: A Retrospective Study. Am. J. Transl. Med. 2023, 15, 1374–1385. [Google Scholar]
- Lindberg-Larsen, M.; Jørgensen, C.C.; Solgaard, S.; Kjersgaard, A.G.; Kehlet, H. Increased Risk of Intraoperative and Early Postoperative Periprosthetic Femoral Fracture with Uncemented Stems. Acta Orthop. 2017, 88, 390–394. [Google Scholar] [CrossRef]
- Ramavath, A.; Lamb, J.N.; Palan, J.; Pandit, H.G.; Jain, S. Postoperative Periprosthetic Femoral Fracture around Total Hip Replacements: Current Concepts and Clinical Outcomes. EFORT Open Rev. 2020, 5, 558–567. [Google Scholar] [CrossRef]
- Olivo-Rodríguez, A.; Tapia-Pérez, H.; Jiménez-Ávila, J. Quality of Life of Patients after Periprosthetic Hip Fracture Surgery. Acta Ortop. Mex. 2012, 26, 174–179. [Google Scholar]
- Jaatinen, R.; Luukkaala, T.; Helminen, H.; Hongisto, M.T.; Viitanen, M.; Nuotio, M.S. Prevalence and Prognostic Significance of Depressive Symptoms in a Geriatric Post-Hip Fracture Assessment. Aging Ment. Health 2022, 26, 1837–1844. [Google Scholar] [CrossRef] [PubMed]
- Schapira, B.; Madanipour, S.; Subramanian, P. Vancouver B2 Periprosthetic Femoral Fractures around Cemented Polished Taper-Slip Stems—How Should We Treat These? A Systematic Scoping Review and Algorithm for Management. Orthop. Traumatol. Surg. Res. 2025, 111, 104110. [Google Scholar] [CrossRef] [PubMed]
- Brady, O.H.; Garbuz, D.S.; Masri, B.A.; Duncan, C.P. CLASSIFICATION OF THE HIP. Orthop. Clin. N. Am. 1999, 30, 215–220. [Google Scholar] [CrossRef] [PubMed]
- Brady, O.H.; Garbuz, D.S.; Masri, B.A.; Duncan, C.P. The Reliability of Validity of the Vancouver Classification of Femoral Fractures after Hip Replacement. J. Arthroplast. 2000, 15, 59–62. [Google Scholar] [CrossRef]
- Lindahl, H.; Malchau, H.; Herberts, P.; Garellick, G. Periprosthetic Femoral Fractures. J. Arthroplast. 2005, 20, 857–865. [Google Scholar] [CrossRef]
- Luzzi, A.; Lakra, A.; Murtaugh, T.; Shah, R.P.; Cooper, H.J.; Geller, J.A. The Effect of Periprosthetic Fractures Following Total Hip and Knee Arthroplasty on Long-Term Functional Outcomes and Quality of Life. Arthroplast. Today 2024, 29, 101418. [Google Scholar] [CrossRef]
- Nieboer, M.F.; van der Jagt, O.P.; de Munter, L.; de Jongh, M.A.C.; van de Ree, C.L.P. Health Status after Periprosthetic Proximal Femoral Fractures. Bone Jt. J. 2024, 106, 442–449. [Google Scholar] [CrossRef]
- Märdian, S.; Schaser, K.-D.; Gruner, J.; Scheel, F.; Perka, C.; Schwabe, P. Adequate Surgical Treatment of Periprosthetic Femoral Fractures Following Hip Arthroplasty Does Not Correlate with Functional Outcome and Quality of Life. Int. Orthop. 2015, 39, 1701–1708. [Google Scholar] [CrossRef]
- Kinov, P.; Volpin, G.; Sevi, R.; Tanchev, P.P.; Antonov, B.; Hakim, G. Surgical Treatment of Periprosthetic Femoral Fractures Following Hip Arthroplasty: Our Institutional Experience. Injury 2015, 46, 1945–1950. [Google Scholar] [CrossRef]
- Risager, S.K.; Pedersen, T.A.; Viberg, B.; Odgaard, A.; Lindberg-Larsen, M.; Abrahamsen, C. Patient Experiences after Surgically Treated Periprosthetic Knee Fracture in the Distal Femur—An Explorative Qualitative Study. Int. J. Orthop. Trauma Nurs. 2025, 58, 101194. [Google Scholar] [CrossRef]
- Finlayson, G.; Tucker, A.; Black, N.D.; McDonald, S.; Molloy, M.; Wilson, D. Outcomes and Predictors of Mortality Following Periprosthethic Proximal Femoral Fractures. Injury 2019, 50, 438–443. [Google Scholar] [CrossRef] [PubMed]
- Smolle, M.A.; Hörlesberger, N.; Maurer-Ertl, W.; Puchwein, P.; Seibert, F.-J.; Leithner, A. Periprosthetic Fractures of Hip and Knee–A Morbidity and Mortality Analysis. Injury 2021, 52, 3483–3488. [Google Scholar] [CrossRef] [PubMed]
- Demnati, B.; Chabihi, Z.; Boumediane, E.M.; Dkhissi, S.; Idarrha, F.; Fath Elkhir, Y.; Benhima, M.A.; Abkari, I.; Rafai, M.; Ibn moussa, S.; et al. Psychological Impact of Peri-Implant Fractures: A Cross-Sectional Study. Tunis. Med. 2024, 102, 708–714. [Google Scholar] [CrossRef] [PubMed]
- Pavlović, M.; Bliemel, C.; Ketter, V.; Lenz, J.; Ruchholtz, S.; Eschbach, D. Health-Related Quality of Life (EQ-5D) after Revision Arthroplasty Following Periprosthetic Femoral Fractures Vancouver B2 and B3 in Geriatric Trauma Patients. Arch. Orthop. Trauma Surg. 2024, 144, 2141–2148. [Google Scholar] [CrossRef]
- Ware, J., Jr.; Sherbourne, C. The MOS 36-Item Short-Form Health Survey (SF-36). I. Conceptual Framework and Item Selection. Med. Care 1992, 30, 473–483. [Google Scholar] [CrossRef]
- Kulić, L.; Vujović, M. Examination of the Impact of Characteristics of the Health Issues, Length of Time since Themyocardial Infarction and Comorbidity to the Quality of Life of Diseased of Myocardial Infarction. Prax. Medica 2019, 48, 25–32. [Google Scholar] [CrossRef]
- Laucis, N.C.; Hays, R.D.; Bhattacharyya, T. Scoring the SF-36 in Orthopaedics: A Brief Guide. J. Bone Jt. Surg. 2015, 97, 1628–1634. [Google Scholar] [CrossRef]
- Kwan, Y.H.; Fong, W.W.S.; Lui, N.L.; Yong, S.T.; Cheung, Y.B.; Malhotra, R.; Østbye, T.; Thumboo, J. Validity and Reliability of the Short Form 36 Health Surveys (SF-36) among Patients with Spondyloarthritis in Singapore. Rheumatol. Int. 2016, 36, 1759–1765. [Google Scholar] [CrossRef]
- Wu, Q.; Chen, Y.; Zhou, Y.; Zhang, X.; Huang, Y.; Liu, R. Reliability, Validity, and Sensitivity of Short-Form 36 Health Survey (SF-36) in Patients with Sick Sinus Syndrome. Medicine 2023, 102, e33979. [Google Scholar] [CrossRef]
- American Society of Anesthesiologists Statement on ASA Physical Status Classification System. Available online: https://www.asahq.org/standards-and-practice-parameters/statement-on-asa-physical-status-classification-system (accessed on 25 November 2025).
- Nikolic, A.; Biocanin, V.; Rancic, N.; Duspara, M.; Djuric, D. Serbian Translation and Validation of the SF-36 for the Assessment of Quality of Life in Patients with Diagnosed Arterial Hypertension. Exp. Appl. Biomed. Res. (EABR) 2023, 24, 227–234. [Google Scholar] [CrossRef]
- Benyamini, Y.; Burns, E. Views on Aging: Older Adults’ Self-Perceptions of Age and of Health. Eur. J. Ageing 2020, 17, 477–487. [Google Scholar] [CrossRef] [PubMed]
- Ortega-Gómez, E.; Vicente-Galindo, P.; Martín-Rodero, H.; Galindo-Villardón, P. Detection of Response Shift in Health-Related Quality of Life Studies: A Systematic Review. Health Qual. Life Outcomes 2022, 20, 20. [Google Scholar] [CrossRef] [PubMed]
- Sawatzky, R.; Kwon, J.-Y.; Barclay, R.; Chauhan, C.; Frank, L.; van den Hout, W.B.; Nielsen, L.K.; Nolte, S.; Sprangers, M.A.G. Implications of Response Shift for Micro-, Meso-, and Macro-Level Healthcare Decision-Making Using Results of Patient-Reported Outcome Measures. Qual. Life Res. 2021, 30, 3343–3357. [Google Scholar] [CrossRef] [PubMed]
- Sidler-Maier, C.C.; Waddell, J.P. Incidence and Predisposing Factors of Periprosthetic Proximal Femoral Fractures: A Literature Review. Int. Orthop. 2015, 39, 1673–1682. [Google Scholar] [CrossRef]
- Lewis, G.S.; Caroom, C.T.; Wee, H.; Jurgensmeier, D.; Rothermel, S.D.; Bramer, M.A.; Reid, J.S. Tangential Bicortical Locked Fixation Improves Stability in Vancouver B1 Periprosthetic Femur Fractures. J. Orthop. Trauma 2015, 29, e364–e370. [Google Scholar] [CrossRef]
- Solomon, L.B.; Hussenbocus, S.M.; Carbone, T.A.; Callary, S.A.; Howie, D.W. Is Internal Fixation Alone Advantageous in Selected B2 Periprosthetic Fractures? ANZ J. Surg. 2015, 85, 169–173. [Google Scholar] [CrossRef]
- Kanakaris, N.K.; Obakponovwe, O.; Krkovic, M.; Costa, M.L.; Shaw, D.; Mohanty, K.R.; West, R.M.; Giannoudis, P.V. Fixation of Periprosthetic or Osteoporotic Distal Femoral Fractures with Locking Plates: A Pilot Randomised Controlled Trial. Int. Orthop. 2019, 43, 1193–1204. [Google Scholar] [CrossRef]
- Farrow, L.; Ablett, A.D.; Sargeant, H.W.; Smith, T.O.; Johnston, A.T. Does Early Surgery Improve Outcomes for Periprosthetic Fractures of the Hip and Knee? A Systematic Review and Meta-Analysis. Arch. Orthop. Trauma Surg. 2021, 141, 1393–1400. [Google Scholar] [CrossRef]
- Pavlou, G.; Panteliadis, P.; Macdonald, D.; Timperley, J.A.; Gie, G.; Bancroft, G.; Tsiridis, E. A Review of 202 Periprosthetic Fractures—Stem Revision and Allograft Improves Outcome for Type B Fractures. HIP Int. 2011, 21, 021–029. [Google Scholar] [CrossRef]
- Gitajn, I.L.; Heng, M.; Weaver, M.J.; Casemyr, N.; May, C.; Vrahas, M.S.; Harris, M.B. Mortality Following Surgical Management of Vancouver B Periprosthetic Fractures. J. Orthop. Trauma 2017, 31, 9–14. [Google Scholar] [CrossRef]
- Antoniadis, A.; Camenzind, R.; Schelling, G.; Helmy, N. Is Primary Osteosynthesis the Better Treatment of Periprosthetic Fémur Fractures Vancouver Type B2? Br. J. Surg. 2017, 104, 17. [Google Scholar]
- Joestl, J.; Hofbauer, M.; Lang, N.; Tiefenboeck, T.; Hajdu, S. Locking Compression Plate versus Revision-Prosthesis for Vancouver Type B2 Periprosthetic Femoral Fractures after Total Hip Arthroplasty. Injury 2016, 47, 939–943. [Google Scholar] [CrossRef] [PubMed]
- Poulsen, N.R.; Mechlenburg, I.; Søballe, K.; Lange, J. Patient-Reported Quality of Life and Hip Function after 2-Stage Revision of Chronic Periprosthetic Hip Joint Infection: A Cross-Sectional Study. HIP Int. 2018, 28, 407–414. [Google Scholar] [CrossRef] [PubMed]
- Thien, T.M.; Chatziagorou, G.; Garellick, G.; Furnes, O.; Havelin, L.I.; Mäkelä, K.; Overgaard, S.; Pedersen, A.; Eskelinen, A.; Pulkkinen, P.; et al. Periprosthetic Femoral Fracture within Two Years After Total Hip Replacement. J. Bone Jt. Surg. 2014, 96, e167. [Google Scholar] [CrossRef]
- Milenkovic, S.; Stanojlovic, M.; Mitkovic, M.; Radenkovic, M. Dynamic Internal Fixation of the Periprosthetic Femoral Fractures after Total Hip Arthroplasty. Acta Chir. Iugosl. 2004, 51, 93–96. [Google Scholar] [CrossRef]
- Şenel, A.; Çirci, E.; Kalyenci, A.S.; Barış, A.; Öztürkmen, Y. Evaluation of Variables Influencing Mortality in Periprosthetic Femur Fractures: Do Fracture Type and Surgical Method Affect Mortality? Istanb. Med. J. 2024, 25, 311–317. [Google Scholar] [CrossRef]
- Tachi, H.; Takegami, Y.; Okura, T.; Tokutake, K.; Nakashima, H.; Mishima, K.; Kasai, T.; Imagama, S. Comparison of Clinical Outcomes of Periprosthetic Fractures Between Cemented vs. Cementless Stem Methods After Initial Total Hip Arthroplasty or Bipolar Hemiarthroplasty: A Multicenter Analysis (TRON Study). Arthroplast. Today 2025, 33, 101699. [Google Scholar] [CrossRef]
- Elashmawy, M.I.; Mostafa, M.A.R. Use of Cemented Standard Stem Arthroplasty for Unstable Intertrochanteric Fractures in Elderly Patients: A Pilot Study. J. Musculoskelet. Surg. Res. 2025, 9, 244–250. [Google Scholar] [CrossRef]
- Khan, T.; Grindlay, D.; Ollivere, B.J.; Scammell, B.E.; Manktelow, A.R.J.; Pearson, R.G. A Systematic Review of Vancouver B2 and B3 Periprosthetic Femoral Fractures. Bone Jt. J. 2017, 99, 17–25. [Google Scholar] [CrossRef]
- Ricci, W.M. Periprosthetic Femur Fractures. J. Orthop. Trauma 2015, 29, 130–137. [Google Scholar] [CrossRef]
- Zampelis, V.; Ornstein, E.; Franzén, H.; Atroshi, I. A Simple Visual Analog Scale for Pain is as Responsive as the WOMAC, the SF-36, and the EQ-5D in Measuring Outcomes of Revision Hip Arthroplasty. Acta Orthop. 2014, 85, 128–132. [Google Scholar] [CrossRef]
- Märdian, S.; Schaser, K.; Scheel, F.; Gruner, J.; Schwabe, P. Quality of Life and Functional Outcome of Periprosthetic Fractures around the Knee Following Knee Arthroplasty. Acta Chir. Orthop. Traumatol. Cech. 2015, 82, 113–118. [Google Scholar] [CrossRef]
- Stoffel, K.; Blauth, M.; Joeris, A.; Blumenthal, A.; Rometsch, E. Fracture Fixation versus Revision Arthroplasty in Vancouver Type B2 and B3 Periprosthetic Femoral Fractures: A Systematic Review. Arch. Orthop. Trauma Surg. 2020, 140, 1381–1394. [Google Scholar] [CrossRef]
- Buijs, M.A.S.; Haidari, S.; IJpma, F.F.A.; Hietbrink, F.; Govaert, G.A.M. What Can They Expect? Decreased Quality of Life and Increased Postoperative Complication Rate in Patients with a Fracture-Related Infection. Injury 2024, 55, 111425. [Google Scholar] [CrossRef]
- Cursaru, A.; Popa, M.; Cretu, B.; Iordache, S.; Iacobescu, G.L.; Spiridonica, R.; Rascu, A.; Serban, B.; Cirstoiu, C. Exploring Individualized Approaches to Managing Vancouver B Periprosthetic Femoral Fractures: Insights from a Comprehensive Case Series Analysis. Cureus 2024, 16, e53269. [Google Scholar] [CrossRef]
- de Sire, A.; Invernizzi, M.; Baricich, A.; Lippi, L.; Ammendolia, A.; Grassi, F.A.; Leigheb, M. Optimization of Transdisciplinary Management of Elderly with Femur Proximal Extremity Fracture: A Patient-Tailored Plan from Orthopaedics to Rehabilitation. World J. Orthop. 2021, 12, 456–466. [Google Scholar] [CrossRef] [PubMed]
- Cohen, J.S.; Agarwal, A.R.; Kinnard, M.J.; Thakkar, S.C.; Golladay, G.J. The Association of Postoperative Osteoporosis Therapy With Periprosthetic Fracture Risk in Patients Undergoing Arthroplasty for Femoral Neck Fractures. J. Arthroplast. 2023, 38, 726–731. [Google Scholar] [CrossRef]
- Lee, K.-J.; Um, S.-H.; Kim, Y.-H. Postoperative Rehabilitation after Hip Fracture: A Literature Review. Hip Pelvis 2020, 32, 125–131. [Google Scholar] [CrossRef] [PubMed]

| Type | Description | Example |
|---|---|---|
| A | Involving apophysis, e.g., avulsion | Greater or lesser trochanter |
| B | Directly adjacent to implant | Femoral shaft fracture around stem |
| B1 | Well-fixed implant | |
| B2 | Loose implant and good bone stock | |
| B3 | Loose implant and poor bone stock | |
| C | Distant to implant but within same bone | Distal femur fracture below stem |
| D | Interprosthetic—between two joint replacements at either end of long bone | Femoral shaft fracture between a hip and knee replacement |
| E | Involves two bones supporting one joint replacement | Combined acetabular and femur fracture around THR |
| F | At native joint surface which directly articulates with an implant | Acetabular fracture next to hip hemiarthroplasty |
| Parameter | PFF Group (n = 60) | THA Control (n = 30) |
|---|---|---|
| Sex (F/M) n (%) | 32/28 (53.3/46.7) | 17/13 (56.7/43.3) |
| Age (years), mean ± SD | 73.02 ± 8.97 | 71.36 ± 8.53 |
| Time to surgery (days), mean ± SD | 3.2 ± 1.4 | 2.7 ± 1.2 |
| Vancouver type (B1/B2/B3) | 37/19/4 | - |
| Surgical treatment | ORIF (B1), Revision + ORIF (B2/B3) | Primary THA |
| ASA status (II/III), n (%) | 24/36 (40.0/60.0) | 13/17 (43.3/56.7) |
| Follow-up (months), mean ± SD | 25.1 ± 7.2 | 23.4 ± 5.1 |
| Domain | r | 95% CI (Lower) | 95% CI (Upper) |
|---|---|---|---|
| General health perceptions | 0.768 ** | 0.646 | 0.851 |
| Physical functioning | −0.806 ** | −0.877 | −0.702 |
| Role limitations—physical | −0.731 ** | −0.817 | −0.607 |
| Role limitations—emotional | −0.687 ** | −0.782 | −0.557 |
| Social functioning | −0.687 ** | −0.782 | −0.557 |
| Bodily pain | 0.735 * | 0.615 | 0.829 |
| Energy/fatigue | −0.762 ** | −0.842 | −0.660 |
| Emotional well-being | −0.827 ** | −0.888 | −0.738 |
| Overall SF-36 | −0.619 ** | −0.730 | −0.471 |
| Domain | Male ± SD | Female ± SD | t | p | Cohen’s d | 95% CI (d) |
|---|---|---|---|---|---|---|
| General health perceptions | 42.0 ± 31.0 | 39.5 ± 32.0 | −0.306 | 0.760 | −0.079 | −0.587 to 0.428 |
| Physical functioning | 54.0 ± 42.0 | 50.5 ± 43.0 | 0.317 | 0.752 | 0.082 | −0.425 to 0.589 |
| Role limitations—physical | 46.0 ± 50.0 | 46.0 ± 50.0 | −0.034 | 0.973 | −0.009 | −0.516 to 0.498 |
| Role limitations—emotional | 67.0 ± 44.0 | 63.0 ± 45.0 | 0.367 | 0.715 | 0.095 | −0.412 to 0.602 |
| Social functioning | 83.25 ± 44.0 | 84.25 ± 42.0 | 0.367 | 0.715 | 0.095 | −0.412 to 0.602 |
| Bodily pain | 72.6 ± 68.0 | 70.6 ± 70.0 | −0.436 | 0.665 | −0.113 | −0.620 to 0.394 |
| Energy/fatigue | 45.0 ± 30.0 | 44.4 ± 26.0 | −0.422 | 0.674 | −0.110 | −0.617 to 0.397 |
| Emotional well-being | 50.4 ± 32.0 | 50.8 ± 32.0 | 0.040 | 0.968 | 0.010 | −0.497 to 0.517 |
| Overall SF-36 | 68.64 ± 15.28 | 64.96 ± 15.91 | 0.909 | 0.367 | 0.236 | −0.254 to 0.726 |
| Domain | Left ± SD | Right ± SD | t | p | Cohen’s d | 95% CI (d) |
|---|---|---|---|---|---|---|
| General health perceptions | 49.0 ± 36.0 | 52.5 ± 34.0 | 0.519 | 0.605 | 0.142 | −0.400 to 0.685 |
| Physical functioning | 54.0 ± 42.0 | 60.0 ± 41.0 | −0.686 | 0.494 | −0.187 | −0.728 to 0.354 |
| Role limitations—physical | 41.0 ± 49.0 | 54.0 ± 50.0 | −1.254 | 0.213 | −0.341 | −0.882 to 0.201 |
| Role limitations—emotional | 61.0 ± 47.0 | 75.0 ± 41.0 | −1.423 | 0.158 | −0.386 | −0.928 to 0.157 |
| Social functioning | 84.5 ± 48.0 | 81.5 ± 42.0 | −1.426 | 0.157 | −0.387 | −0.929 to 0.156 |
| Bodily pain | 72.0 ± 61.0 | 72.6 ± 62.0 | 0.104 | 0.917 | 0.028 | −0.513 to 0.569 |
| Energy/fatigue | 45.4 ± 23.0 | 44.8 ± 24.0 | −0.213 | 0.832 | −0.058 | −0.599 to 0.484 |
| Emotional well-being | 50.8 ± 32.0 | 46.6 ± 34.0 | −0.609 | 0.544 | −0.165 | −0.706 to 0.377 |
| Overall SF-36 | 72.67 ± 17.49 | 72.29 ± 17.30 | 0.103 | 0.918 | 0.028 | −0.513 to 0.569 |
| Domain | B2 and B3 (Osteosynthesis in Conjunction with a Stem Replacement) (n = 23) ± SD | B1 (Osteosynthesis) (n = 37) ± SD | t | p | Cohen’s d | 95% CI (d) |
|---|---|---|---|---|---|---|
| General health perceptions | 47.5 ± 31.0 | 29.5 ± 28.5 | −2.266 | 0.027 * | −0.501 | −0.936 to −0.067 |
| Physical functioning | 62.5 ± 42.0 | 35.5 ± 37.5 | 2.526 | 0.014 * | 0.599 | 0.128 to 1.070 |
| Role limitations—physical | 59.0 ± 49.0 | 26.0 ± 44.0 | 2.684 | 0.010 * | 0.636 | 0.161 to 1.111 |
| Role limitations—emotional | 72.0 ± 42.0 | 53.0 ± 46.0 | 1.639 | 0.107 | 0.389 | −0.101 to 0.879 |
| Social functioning | 81.5 ± 42.0 | 84.25 ± 46.0 | 1.639 | 0.107 | 0.389 | −0.101 to 0.879 |
| Bodily pain | 77.0 ± 69.5 | 41.8 ± 62.0 | −2.074 | 0.042 * | −0.486 | −0.923 to −0.049 |
| Energy/fatigue | 43.2 ± 28.0 | 47.2 ± 23.0 | 2.839 | 0.006 * | 0.672 | 0.199 to 1.146 |
| Emotional well-being | 43.8 ± 32.0 | 55.4 ± 30.0 | 2.797 | 0.007 * | 0.662 | 0.191 to 1.132 |
| Overall SF-36 | 60.8 ± 41.8 | 46.6 ± 39.8 | 1.22 | 0.227 | 0.287 | −0.167 to 0.741 |
| Domain | PFF ± SD | THA ± SD | t | p | Cohen’s d | 95% CI (d) |
|---|---|---|---|---|---|---|
| General health perceptions | 42.4 ± 31.3 | 27.5 ± 29.5 | 4.717 | <0.0005 * | 0.972 | 0.621 to 1.323 |
| Physical functioning | 54.0 ± 42.0 | 60.0 ± 37.5 | −1.557 | 0.123 | −0.331 | −0.733 to 0.072 |
| Role limitations—physical | 46.0 ± 50.0 | 50.0 ± 50.0 | −0.295 | 0.768 | −0.063 | −0.466 to 0.339 |
| Role limitations—emotional | 65.0 ± 45.0 | 73.0 ± 44.0 | −0.772 | 0.442 | −0.164 | −0.566 to 0.239 |
| Social functioning | 83.0 ± 45.0 | 86.0 ± 43.0 | −0.770 | 0.445 | −0.163 | −0.566 to 0.239 |
| Bodily pain | 72.5 ± 68.5 | 70.0 ± 43.0 | 0.875 | 0.384 | 0.185 | −0.226 to 0.596 |
| Energy/fatigue | 45.0 ± 28.0 | 47.0 ± 8.0 | 1.874 | 0.065 | 0.345 | −0.043 to 0.733 |
| Emotional well-being | 50.5 ± 32.0 | 57.5 ± 32.0 | −1.630 | 0.107 | −0.300 | −0.701 to 0.101 |
| Overall SF-36 | 66.68 ± 15.60 | 84.10 ± 14.65 | −5.092 | <0.0005 * | −1.031 | −1.372 to −0.690 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Published by MDPI on behalf of the Lithuanian University of Health Sciences. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gvozdenović, N.; Vranješ, M.; Lekić, I.; Bjelan, S.; Ćorić, A. Quality of Life Following Vancouver Type B Periprosthetic Femoral Fractures: A Cross-Sectional Study. Medicina 2025, 61, 2159. https://doi.org/10.3390/medicina61122159
Gvozdenović N, Vranješ M, Lekić I, Bjelan S, Ćorić A. Quality of Life Following Vancouver Type B Periprosthetic Femoral Fractures: A Cross-Sectional Study. Medicina. 2025; 61(12):2159. https://doi.org/10.3390/medicina61122159
Chicago/Turabian StyleGvozdenović, Nemanja, Miodrag Vranješ, Igor Lekić, Sveto Bjelan, and Andrijana Ćorić. 2025. "Quality of Life Following Vancouver Type B Periprosthetic Femoral Fractures: A Cross-Sectional Study" Medicina 61, no. 12: 2159. https://doi.org/10.3390/medicina61122159
APA StyleGvozdenović, N., Vranješ, M., Lekić, I., Bjelan, S., & Ćorić, A. (2025). Quality of Life Following Vancouver Type B Periprosthetic Femoral Fractures: A Cross-Sectional Study. Medicina, 61(12), 2159. https://doi.org/10.3390/medicina61122159







