Evaluation of Risk Factors for Revision Surgery After Proximal Femoral Nailing for Intertrochanteric Fractures
Abstract
1. Introduction
2. Materials and Methods
2.1. Patient Selection
2.2. Data Collection and Outcome Assessment
2.3. Statistical Analysis
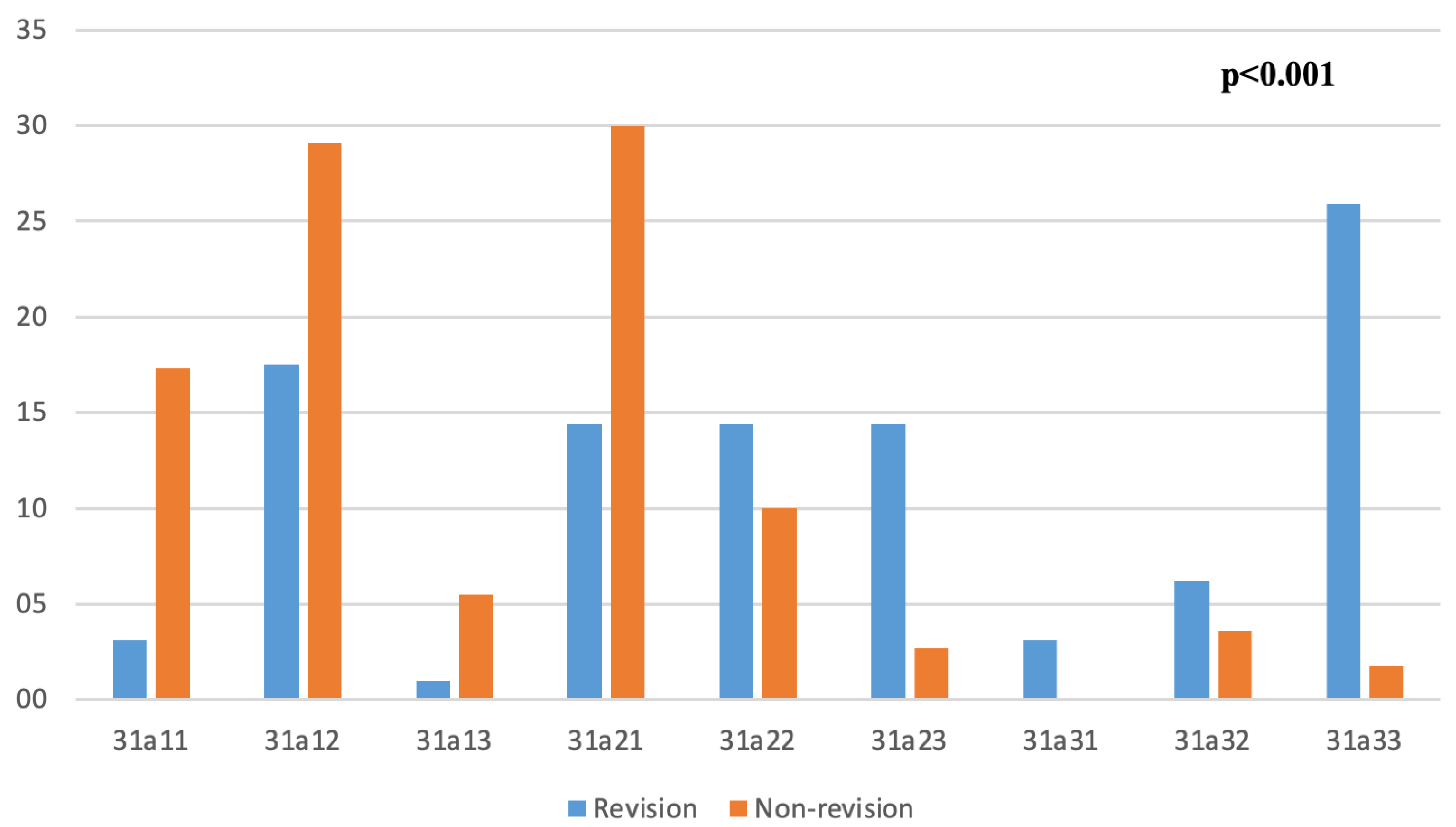
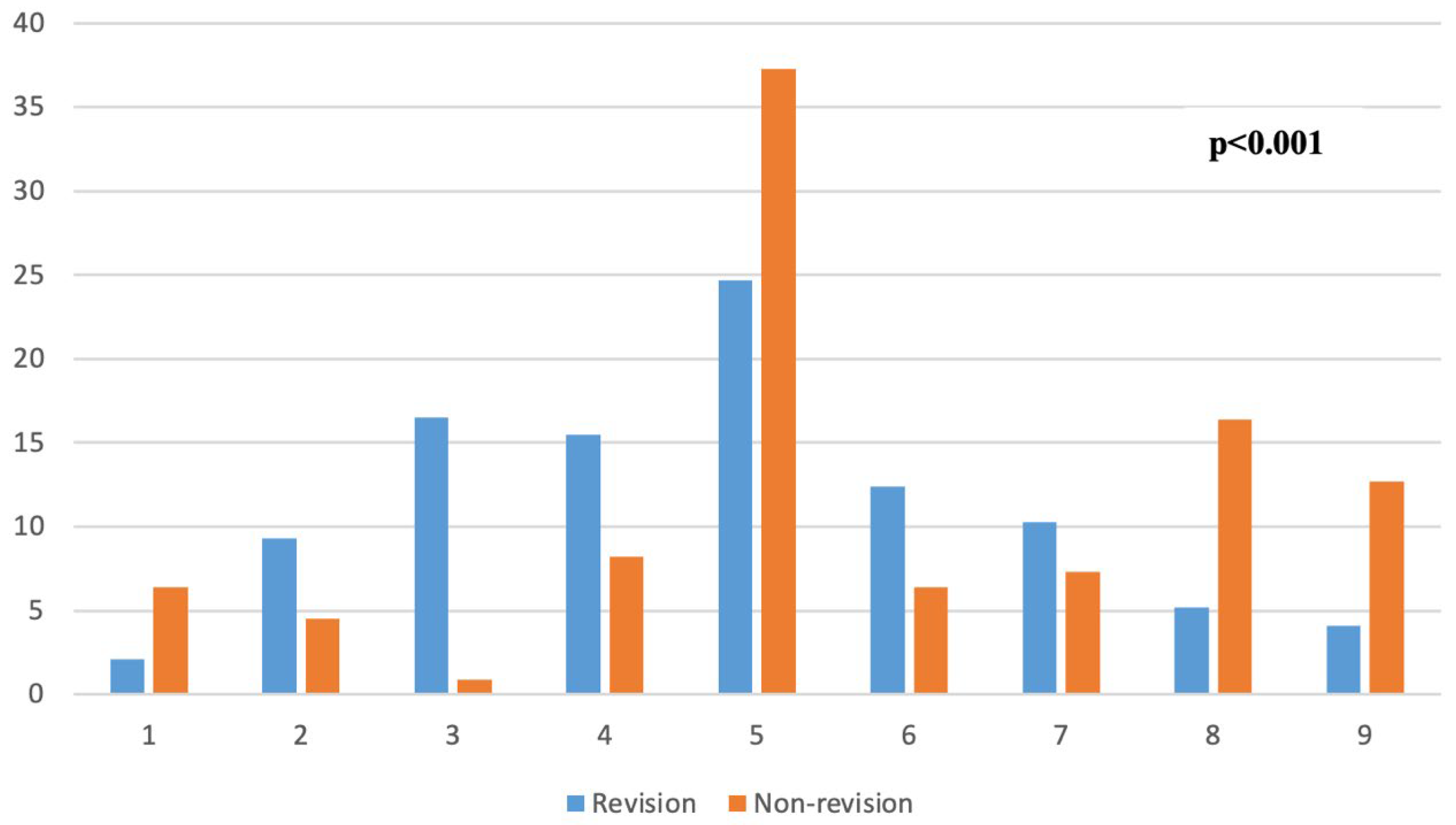
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| PFN | Proximal femoral nail |
| SHS | Sliding hip screw |
| TAD | Tip-apex distance |
| Cal TAD | Calcar-referenced tip-apex distance |
| IQR | Interquartile range |
| SD | Standard deviation |
| CI | Confidence interval |
| OR | Odds ratio |
References
- Veronese, N.; Maggi, S. Epidemiology and social costs of hip fracture. Injury 2018, 49, 1458–1460. [Google Scholar] [CrossRef]
- The REFReSH Study Group; Leal, J.; Gray, A.M.; Prieto-Alhambra, D.; Arden, N.K.; Cooper, C.; Javaid, M.K.; Judge, A. Impact of hip fracture on hospital care costs: A population-based study. Osteoporos. Int. 2016, 27, 549–558. [Google Scholar] [CrossRef]
- Parker, M.J.; Handoll, H.H. Gamma and other cephalocondylic intramedullary nails versus extramedullary implants for extracapsular hip fractures in adults. Cochrane Database Syst. Rev. 2010, CD000093. [Google Scholar] [CrossRef]
- Niu, E.; Yang, A.; Harris, A.H.S.; Bishop, J. Which Fixation Device is Preferred for Surgical Treatment of Intertrochanteric Hip Fractures in the United States? A Survey of Orthopaedic Surgeons. Clin. Orthop. Relat. Res. 2015, 473, 3647–3655. [Google Scholar] [CrossRef]
- Haidukewych, G.J. Intertrochanteric fractures: Ten tips to improve results. J. Bone Jt. Surg. 2009, 91, 712–719. [Google Scholar]
- Uzun, M.; Ertürer, E.; Ozturk, I.; Akman, S.; Seckin, F.; Ozcelik, I.B. Long-term radiographic complications following treatment of unstable intertrochanteric femoral fractures with the proximal femoral nail and effects on functional results. Acta Orthop. Traumatol. Turc. 2009, 43, 457–463. [Google Scholar] [CrossRef]
- Morgan, S.; Bourget-Murray, J.; Garceau, S.; Grammatopoulos, G. Revision total hip arthroplasty for periprosthetic fracture: Epidemiology, outcomes, and factors associated with success. Ann. Jt. 2023, 8, 30. [Google Scholar] [CrossRef]
- Cleveland, M.; Bosworth, D.M.; Thompson, F.R.; Wilson, H.J.; Ishizuka, T. A ten-year analysis of intertrochanteric fractures of the femur. J. Bone Jt. Surg. Am. 1959, 41, 1399–1408. [Google Scholar] [CrossRef]
- Charlson, M.E.; Carrozzino, D.; Guidi, J.; Patierno, C. Charlson Comorbidity Index: A Critical Review of Clinimetric Properties. Psychother. Psychosom. 2022, 91, 8–35. [Google Scholar] [CrossRef] [PubMed]
- Carr, J.B.; Williams, D.; Richards, M. Lateral decubitus positioning for intramedullary nailing of the femur without the use of a fracture table. Orthopedics 2009, 32, 721–724. [Google Scholar] [CrossRef] [PubMed]
- Daher, M.; Nassar, J.E.; Liu, J.; Daniels, A.H.; El-Othmani, M.M. Is lateral decubitus positioning without a traction table a safe option for unstable intertrochanteric fractures? A meta-analysis of randomized controlled trials. Eur. J. Orthop. Surg. Traumatol. 2025, 35, 232. [Google Scholar] [CrossRef]
- Kakumanu, R.K.; Kunadharaju, R.T.; Beesetty, M.; Golla, D. Ease of doing proximal femoral nailing in lateral position in the management of peri-trochanteric femoral fractures in adults: A prospective study. Int. J. Orthop. 2019, 5, 39–46. [Google Scholar] [CrossRef]
- Xue, L.; Zha, L.; Chen, Q.; Liang, Y.-J.; Li, K.-R.; Zhou, Z.; Guan, J.-L.; Qin, H.; Li, Y.-P. Randomized controlled trials of proximal femoral nail antirotation in lateral decubitus and supine position on treatment of intertrochanteric fractures. Sci. World J. 2013, 2013, 276015. [Google Scholar] [CrossRef]
- Korytkowski, P.D.; Panzone, J.M.; Aldahamsheh, O.; Alkhayarin, M.M.; Almohamad, H.O.; Alhammoud, A. Open and closed reduction methods for intramedullary nailing of femoral shaft fractures: A systematic review and meta-analysis of comparative studies. J. Clin. Orthop. Trauma. 2023, 44, 102256. [Google Scholar] [CrossRef]
- Díaz, V.J.; Cañizares, A.C.P.; Martín, I.A.; Peinado, M.A.; Doussoux, P.C. Predictive variables of open reduction in intertrochanteric fracture nailing: A report of 210 cases. Injury 2016, 47 (Suppl. S3), S51–S55. [Google Scholar] [CrossRef]
- Berk, T.; Halvachizadeh, S.; Martin, D.P.; Hierholzer, C.; Müller, D.; Pfeifer, R.; Jukema, G.N.; Gueorguiev, B.; Pape, H.-C. Trochanteric fracture pattern is associated with increased risk for nonunion independent of open or closed reduction technique. BMC Geriatr. 2022, 22, 990. [Google Scholar] [CrossRef]
- Baer, M.; Neuhaus, V.; Pape, H.C.; Ciritsis, B. Influence of mobilization and weight bearing on in-hospital outcome in geriatric patients with hip fractures. SICOT J. 2019, 5, 4. [Google Scholar] [CrossRef] [PubMed]
- Tarrant, S.M.; Attia, J.; Balogh, Z.J. The influence of weight-bearing status on post-operative mobility and outcomes in geriatric hip fracture. Eur. J. Trauma. Emerg. Surg. 2022, 48, 4093–4103. [Google Scholar] [CrossRef] [PubMed]
- Geller, J.A.; Saifi, C.; Morrison, T.A.; Macaulay, W. Tip-apex distance of intramedullary devices as a predictor of cut-out failure in the treatment of peritrochanteric elderly hip fractures. Int. Orthop. 2010, 34, 719–722. [Google Scholar] [CrossRef]
- Li, S.; Chang, S.-M.; Jin, Y.-M.; Zhang, Y.-Q.; Niu, W.-X.; Du, S.-C.; Zhang, L.-Z.; Ma, H. A mathematical simulation of the tip-apex distance and the calcar-referenced tip-apex distance for intertrochanteric fractures reduced with lag screws. Injury 2016, 47, 1302–1308. [Google Scholar] [CrossRef]
- Lopes-Coutinho, L.; Dias-Carvalho, A.; Esteves, N.; Sousa, R. Traditional distance “tip-apex” vs. new calcar referenced “tip-apex”-which one is the best peritrochanteric osteosynthesis failure predictor? Injury 2020, 51, 674–677. [Google Scholar] [CrossRef]
- Kulakoglu, B.; Ozdemir, G.; Bingol, O.; Karlidag, T.; Keskin, O.H.; Durgal, A. A new scoring system for predicting cut-out risk in patients with intertrochanteric femur fractures treated with proximal femoral nail anti-rotation. Acta Orthop. Traumatol. Turc. 2023, 57, 258–266. [Google Scholar] [CrossRef]
- Chang, S.-M.; Zhang, Y.-Q.; Ma, Z.; Li, Q.; Dargel, J.; Eysel, P. Fracture reduction with positive medial cortical support: A key element in stability reconstruction for the unstable pertrochanteric hip fractures. Arch. Orthop. Trauma Surg. 2015, 135, 811–818. [Google Scholar] [CrossRef]
- Shao, Q.; Zhang, Y.; Sun, G.-X.; Yang, C.-S.; Liu, N.; Chen, D.-W.; Cheng, B. Positive or negative anteromedial cortical support of unstable pertrochanteric femoral fractures: A finite element analysis study. Biomed. Pharmacother. 2021, 138, 111473. [Google Scholar] [CrossRef] [PubMed]
- Zhao, K.; Zhang, J.; Li, J.; Meng, H.; Wang, Z.; Zhu, Y.; Hou, Z.; Zhang, Y. Incidence and risk factors of surgical site infection after intertrochanteric fracture surgery: A prospective cohort study. Int. Wound J. 2020, 17, 1871–1880. [Google Scholar] [CrossRef] [PubMed]
- Harrison, T.; Robinson, P.; Cook, A.; Parker, M.J. Factors affecting the incidence of deep wound infection after hip fracture surgery. J. Bone Jt. Surg. Br. 2012, 94, 237–240. [Google Scholar] [CrossRef] [PubMed]
- Bohl, D.D.; Shen, M.R.; Hannon, C.P.; Fillingham, Y.A.; Darrith, B.; Della Valle, C.J. Serum Albumin Predicts Survival and Postoperative Course Following Surgery for Geriatric Hip Fracture. J. Bone Jt. Surg. Am. 2017, 99, 2110–2118. [Google Scholar] [CrossRef] [PubMed]
- Scotcher, M.; Uren, N.; Qureshi, A.; Hancock, N.; Round, J. Fracture-related infection in revision proximal femoral intramedullary nails. Injury 2024, 55, 111338. [Google Scholar] [CrossRef]
- Xie, W.; Shi, L.; Zhang, C.; Cui, X.; Chen, X.; Xie, T.; Zhang, S.; Chen, H.; Rui, Y. Anteromedial cortical support reduction of intertrochanteric fractures–A review. Injury 2024, 111926. [Google Scholar] [CrossRef]
- Marmor, M.; Liddle, K.; Pekmezci, M.; Buckley, J.; Matityahu, A. The effect of fracture pattern stability on implant loading in OTA type 31-A2 proximal femur fractures. J. Orthop. Trauma 2013, 27, 683–689. [Google Scholar] [CrossRef]
- Liu, C.-C.; Xing, W.-Z.; Zhang, Y.-X.; Pan, Z.-H.; Feng, W.-L. Three-dimensional finite element analysis and comparison of a new intramedullary fixation with interlocking intramedullary nail. Cell Biochem. Biophys. 2015, 71, 717–724. [Google Scholar] [CrossRef] [PubMed]
- Horwitz, D.S.; Tawari, A.; Suk, M. Nail Length in the Management of Intertrochanteric Fracture of the Femur. JAAOS-J. Am. Acad. Orthop. Surg. 2016, 24, e50–e58. [Google Scholar] [CrossRef]
- Cinque, M.E.; Goodnough, L.H.; Schultz, B.J.; Fithian, A.T.; DeBaun, M.; Lucas, J.F.; Gardner, M.J.; Bishop, J.A. Short versus long cephalomedullary nailing of intertrochanteric fractures: A meta-analysis of 3208 patients. Arch. Orthop. Trauma Surg. 2022, 142, 1367–1374. [Google Scholar] [CrossRef] [PubMed]
- Rinehart, D.B.; O’NEill, D.E.; Liu, J.W.B.; Sanders, D.T. Does Size Matter for Cephalomedullary Nails in Geriatric Intertrochanteric Fractures? J. Orthop. Trauma 2021, 35, 329–332. [Google Scholar] [CrossRef] [PubMed]
| Total (n = 207) | Revision (n = 97) | Non-Revision (n = 110) | p | |
|---|---|---|---|---|
| Age, years, median (IQR) | 81 (74–87) | 82 (75.5–87) | 78.5 (71–87) | 0.095 ¥ |
| Gender, n (%) | 0.004 a | |||
| Female | 137 (66.2) | 74 (76.3) | 63 (57.3) | |
| Male | 70 (33.8) | 23 (23.7) | 47 (42.7) | |
| Fracture side, n (%) | 0.738 a | |||
| Left | 105 (50.7) | 48 (49.5) | 57 (51.8) | |
| Right | 102 (49.3) | 49 (50.5) | 53 (48.2) | |
| Dorr classification, n (%) | <0.001 a | |||
| Type A | 23 (11.1) | 23 (23.7) | 0 (0) | |
| Type B | 74 (35.8) | 24 (24.7) | 50 (45.5) | |
| Type C | 110 (53.1) | 50 (51.6) | 60 (54.5) | |
| Posteromedial comminution, n (%) | 85 (41.1) | 53 (54.6) | 32 (29.1) | <0.001 a |
| Anesthesia type, n (%) | 0.021 a | |||
| Spinal | 165 (79.7) | 84 (86.6) | 81 (73.6) | |
| General | 42 (20.3) | 13 (13.4) | 29 (26.4) | |
| Patient’s position, n (%) | <0.001 a | |||
| Lateral decubitus | 130 (62.8) | 41 (42.3) | 89 (80.9) | |
| Supine | 77 (37.2) | 56 (57.7) | 21 (19.1) | |
| Reduction, n (%) | <0.001 a | |||
| Closed | 170 (82.1) | 65 (67) | 105 (95.5) | |
| Open | 37 (17.9) | 32 (33) | 5 (4.5) | |
| Infection, n (%) | 16 (7.7) | 15 (15.5) | 1 (0.9) | <0.001 a |
| Medial cortical support variance, n (%) | <0.001 a | |||
| Neutral | 65 (31.4) | 31 (32.0) | 34 (30.9) | |
| Positive | 95 (45.9) | 31 (32.0) | 64 (58.2) | |
| Negative | 47 (22.7) | 35 (36.0) | 12 (10.9) | |
| Trochanter minor fracture size, cm, median (IQR) | 4 (3–5.4) | 3.85 (2.9–5.1) | 4 (3.1–5.5) | 0.486 ¥ |
| Calcar-referenced tip-apex distance, mm, median (IQR) | 28 (23–35) | 32 (25–37) | 26 (23–31) | <0.001 ¥ |
| Classical tip-apex distance, mm, median (IQR) | 24 (18–30) | 25 (19–31) | 22 (17–29) | 0.168 ¥ |
| Lateral cortical thickness, mm, median (IQR) | 22 (14–29) | 21 (13.8–29) | 22.5 (14.8–29) | 0.746 ¥ |
| Charlson comorbidity index, mean ± SD | 5.7 ± 1.7 | 6.3 ± 1.5 | 5.2 ± 1.7 | <0.001 b |
| Bivariate Analysis OR (95% CI) | p | Multivariate Analysis OR (95% CI) | p | |
|---|---|---|---|---|
| Gender | 0.004 | 0.066 | ||
| Male | Ref | Ref | ||
| Female | 2.40 (1.31–4.38) | 0.36 (0.12–1.06) | ||
| Presence of posteromedial comminution | <0.001 | 0.666 | ||
| No | Ref | Ref | ||
| Yes | 2.93 (1.66–5.21) | 1.27 (0.42–3.85) | ||
| Anesthesia type | 0.023 | 0.112 | ||
| General | Ref | Ref | ||
| Spinal | 2.31 (1.12–4.76) | 3.16 (0.76–13.08) | ||
| Patient’s position | <0.001 | <0.001 | ||
| Lateral decubitis | Ref | Ref | ||
| Supine | 5.78 (3.10–10.79) | 9.13 (3.73–22.32) | ||
| Reduction | <0.001 | <0.001 | ||
| Open | Ref | Ref | ||
| Closed | 10.33 (3.83–27.87) | 24.98 (5.48–113.76) | ||
| Surgical site infection | 0.004 | 0.029 | ||
| No | Ref | Ref | ||
| Yes | 19.93 (2.58–154.02) | 14.48 (1.29–126.35) | ||
| Medial cortical support | <0.001 | 0.630 | ||
| Negative | Ref | Ref | ||
| Neutral | 0.16 (0.76–0.36) | 0.32 (0.10–1.02) | ||
| Positive | 0.31 (0.13–0.70) | 0.74 (0.22–2.43) | ||
| Calcar-referenced tip-apex distance | 1.01 (0.98–1.05) | 0.292 | 1.08 (0.98–1.13) | 0.225 |
| Charlson comorbidity index | 1.52 (1.24–1.86) | <0.001 | 2.19 (1.60–3.00) | <0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Published by MDPI on behalf of the Lithuanian University of Health Sciences. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Duman, E.; Torun, Ö.; Girgin, A.B.; Özçelik, M.A.; Acar, A.; Çevik, H.B. Evaluation of Risk Factors for Revision Surgery After Proximal Femoral Nailing for Intertrochanteric Fractures. Medicina 2025, 61, 2085. https://doi.org/10.3390/medicina61122085
Duman E, Torun Ö, Girgin AB, Özçelik MA, Acar A, Çevik HB. Evaluation of Risk Factors for Revision Surgery After Proximal Femoral Nailing for Intertrochanteric Fractures. Medicina. 2025; 61(12):2085. https://doi.org/10.3390/medicina61122085
Chicago/Turabian StyleDuman, Evrim, Ömer Torun, Ahmet Berkay Girgin, Mehmet Alperen Özçelik, Ahmet Acar, and Hüseyin Bilgehan Çevik. 2025. "Evaluation of Risk Factors for Revision Surgery After Proximal Femoral Nailing for Intertrochanteric Fractures" Medicina 61, no. 12: 2085. https://doi.org/10.3390/medicina61122085
APA StyleDuman, E., Torun, Ö., Girgin, A. B., Özçelik, M. A., Acar, A., & Çevik, H. B. (2025). Evaluation of Risk Factors for Revision Surgery After Proximal Femoral Nailing for Intertrochanteric Fractures. Medicina, 61(12), 2085. https://doi.org/10.3390/medicina61122085






