Elderly Men with De Novo Metastatic Castration-Sensitive Prostate Cancer: Therapy and Does Comorbidity Matter
Abstract
1. Introduction
2. Methods
Statistical Analyses
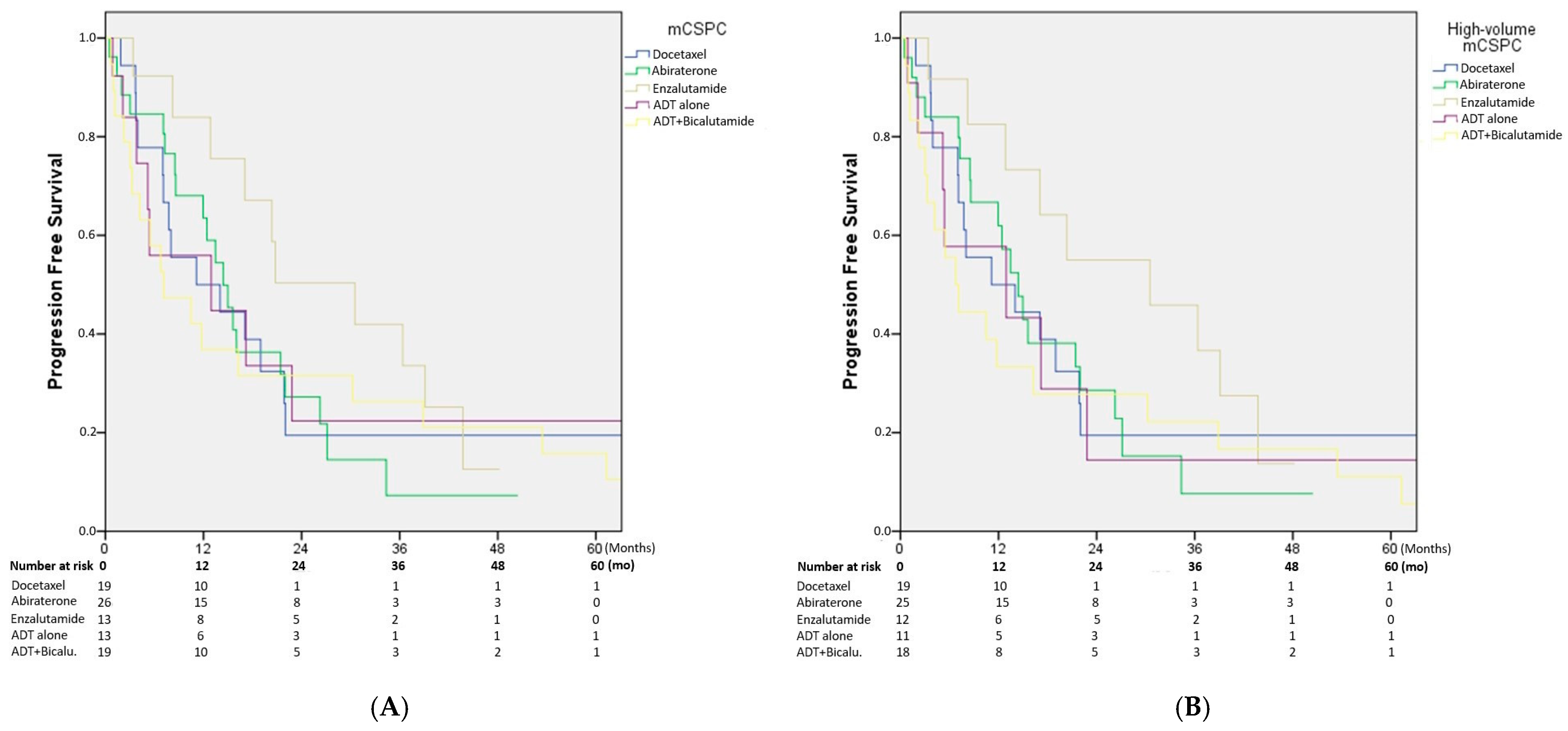
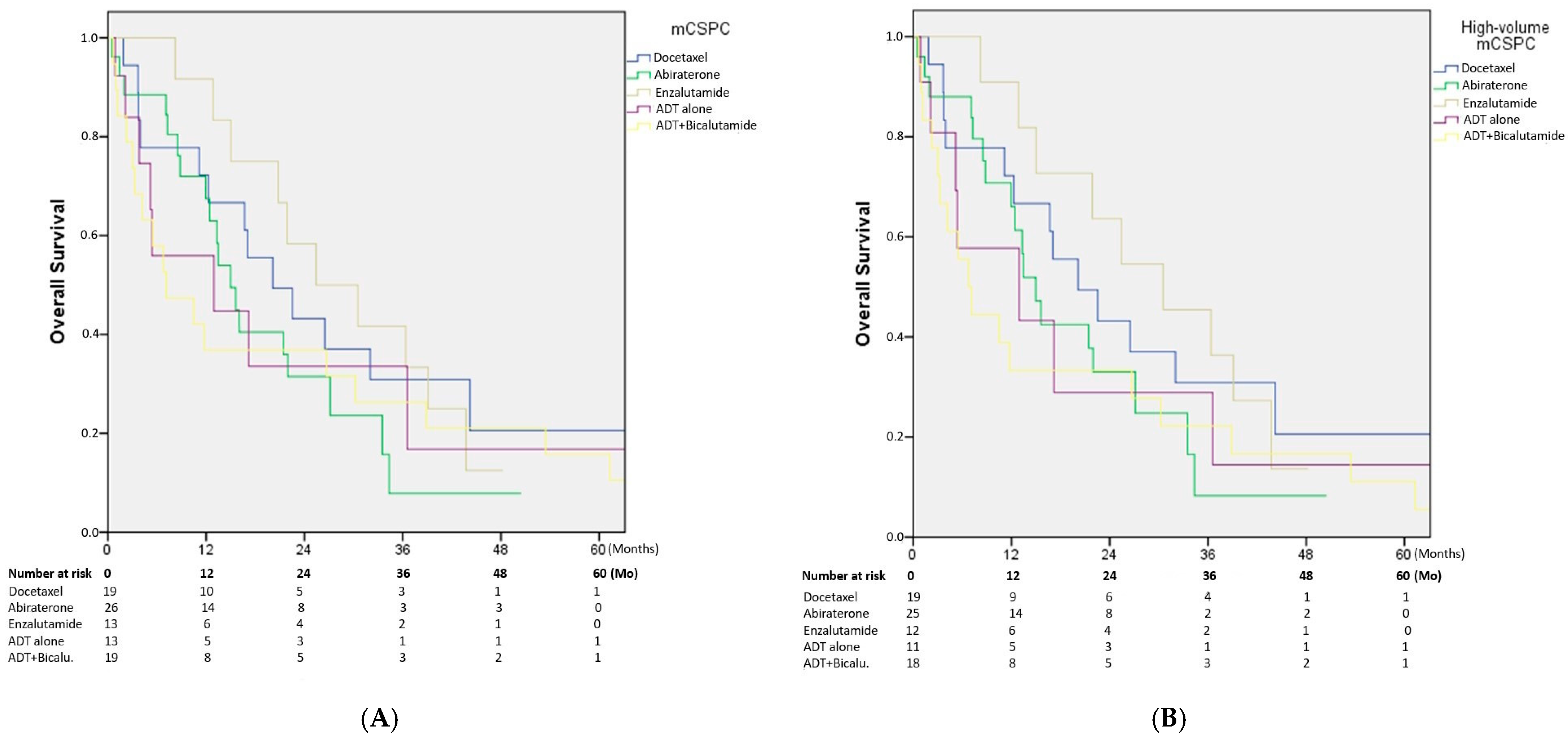
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Devasia, T.P.; Mariotto, A.B.; Nyame, Y.A.; Etzioni, R. Estimating the Number of Men Living with Metastatic Prostate Cancer in the United States. Cancer Epidemiol. Biomark. Prev. 2023, 32, 659–665. [Google Scholar] [CrossRef]
- Desai, M.M.; Cacciamani, G.E.; Gill, K.; Zhang, J.; Liu, L.; Abreu, A.; Gill, I.S. Trends in Incidence of Metastatic Prostate Cancer in the US. JAMA Netw. Open 2022, 5, e222246. [Google Scholar] [CrossRef]
- Huggins, C.; Hodges, C.V. Studies on prostatic cancer: I. The effect of castration, of estrogen and of androgen injection on serum phosphatases in metastatic carcinoma of the prostate. J. Urol. 2002, 168, 9–12. [Google Scholar] [CrossRef] [PubMed]
- Huggins, C.; Stevens, R.E., Jr.; Hodges, C.V. Studies on prostatic cancer: II. The effects of castration on advanced carcinoma of the prostate gland. Arch. Surg. 1941, 43, 209–223. [Google Scholar] [CrossRef]
- Riaz, I.B.; Islam, M.; Ikram, W.; Naqvi, S.A.A.; Maqsood, H.; Saleem, Y.; Riaz, A.; Ravi, P.; Wang, Z.; Hussain, S.A.; et al. Disparities in the Inclusion of Racial and Ethnic Minority Groups and Older Adults in Prostate Cancer Clinical Trials: A Meta-analysis. JAMA Oncol. 2023, 9, 180–187. [Google Scholar] [CrossRef]
- Scher, K.S.; Hurria, A. Under-representation of older adults in cancer registration trials: Known problem, little progress. J. Clin. Oncol. 2012, 30, 2036–2038. [Google Scholar] [CrossRef]
- Sweeney, C.J.; Chen, Y.H.; Carducci, M.; Liu, G.; Jarrard, D.F.; Eisenberger, M.; Wong, Y.N.; Hahn, N.; Kohli, M.; Cooney, M.M.; et al. Chemohormonal Therapy in Metastatic Hormone-Sensitive Prostate Cancer. N. Engl. J. Med. 2015, 373, 737–746. [Google Scholar] [CrossRef] [PubMed]
- Fizazi, K.; Tran, N.; Fein, L.; Matsubara, N.; Rodriguez-Antolin, A.; Alekseev, B.Y.; Ozguroglu, M.; Ye, D.; Feyerabend, S.; Protheroe, A.; et al. Abiraterone plus Prednisone in Metastatic, Castration-Sensitive Prostate Cancer. N. Engl. J. Med. 2017, 377, 352–360. [Google Scholar] [CrossRef]
- Hammarsten, J.; Hogstedt, B. Calculated fast-growing benign prostatic hyperplasia—A risk factor for developing clinical prostate cancer. Scand. J. Urol. Nephrol. 2002, 36, 330–338. [Google Scholar] [CrossRef] [PubMed]
- Grossman, E.; Messerli, F.H.; Boyko, V.; Goldbourt, U. Is there an association between hypertension and cancer mortality? Am. J. Med. 2002, 112, 479–486. [Google Scholar] [CrossRef]
- Kouvaris, J.; Kouloulias, V.; Loghis, C.; Sykiotis, C.; Balafouta, M.; Vlahos, L. Prognostic factors for survival in invasive squamous cell vulvar carcinoma: A univariate analysis. Gynecol. Obs. Obstet. Investig. 2001, 51, 262–265. [Google Scholar] [CrossRef] [PubMed]
- Carrizo, P.H.; Dubin, M.; Stoppani, A.O. Physiopathologic effects of nitric oxide and their relationship with oxidative stress. Medicina 1998, 58, 367–373. [Google Scholar] [PubMed]
- Egami, K.; Murohara, T.; Shimada, T.; Sasaki, K.; Shintani, S.; Sugaya, T.; Ishii, M.; Akagi, T.; Ikeda, H.; Matsuishi, T.; et al. Role of host angiotensin II type 1 receptor in tumor angiogenesis and growth. J. Clin. Investig. 2003, 112, 67–75. [Google Scholar] [CrossRef]
- Yoshiji, H.; Yoshii, J.; Ikenaka, Y.; Noguchi, R.; Yanase, K.; Tsujinoue, H.; Imazu, H.; Fukui, H. Suppression of the renin-angiotensin system attenuates vascular endothelial growth factor-mediated tumor development and angiogenesis in murine hepatocellular carcinoma cells. Int. J. Oncol. 2002, 20, 1227–1231. [Google Scholar] [CrossRef]
- Grossman, E.; Messerli, F.H.; Goldbourt, U. Carcinogenicity of antihypertensive therapy. Curr. Hypertens. Rep. 2002, 4, 195–201. [Google Scholar] [CrossRef]
- Santala, E.E.; Rannikko, A.; Murtola, T.J. Antihypertensive drugs and prostate cancer survival after radical prostatectomy in Finland-A nationwide cohort study. Int. J. Cancer 2019, 144, 440–447. [Google Scholar] [CrossRef]
- Haggstrom, C.; Stocks, T.; Nagel, G.; Manjer, J.; Bjorge, T.; Hallmans, G.; Engeland, A.; Ulmer, H.; Lindkvist, B.; Selmer, R.; et al. Prostate cancer, prostate cancer death, and death from other causes, among men with metabolic aberrations. Epidemiology 2014, 25, 823–828. [Google Scholar] [CrossRef]
- Scosyrev, E.; Messing, E.M.; Mohile, S.; Golijanin, D.; Wu, G. Prostate cancer in the elderly: Frequency of advanced disease at presentation and disease-specific mortality. Cancer 2012, 118, 3062–3070. [Google Scholar] [CrossRef]
- Bian, S.X.; Hoffman, K.E. Management of prostate cancer in elderly men. Semin. Radiat. Oncol. 2013, 23, 198–205. [Google Scholar] [CrossRef] [PubMed]
- Fane, M.; Weeraratna, A.T. How the ageing microenvironment influences tumour progression. Nat. Rev. Cancer 2020, 20, 89–106. [Google Scholar] [CrossRef] [PubMed]
- Dyche, D.J.; Ness, J.; West, M.; Allareddy, V.; Konety, B.R. Prevalence of prostate specific antigen testing for prostate cancer in elderly men. J. Urol. 2006, 175, 2078–2082. [Google Scholar] [CrossRef] [PubMed]
- Graham, L.S.; Lin, J.K.; Lage, D.E.; Kessler, E.R.; Parikh, R.B.; Morgans, A.K. Management of Prostate Cancer in Older Adults. Am. Soc. Clin. Oncol. Educ. Book 2023, 43, e390396. [Google Scholar] [CrossRef] [PubMed]
- Schaeffer, E.M.; Srinivas, S.; Adra, N.; An, Y.; Barocas, D.; Bitting, R.; Bryce, A.; Chapin, B.; Cheng, H.H.; D’Amico, A.V.; et al. Prostate Cancer, Version 4.2023, NCCN Clinical Practice Guidelines in Oncology. J. Natl. Compr. Cancer Netw. 2023, 21, 1067–1096. [Google Scholar] [CrossRef] [PubMed]
| Age at Diagnosis (Year) | 81 (75–93) |
| Comorbidities (n, %) | |
| Hypertension | 74 (82.2) |
| Dyslipidemia | 57 (63.3) |
| Diabetes mellitus | 29 (32.2) |
| Chronic obstructive pulmonary disease | 20 (22.2) |
| Coronary artery disease | 25 (27.8) |
| Presenting symptom (n, %) | |
| Lower urinary tract symptoms | 34 (37.7) |
| Bone pain | 51 (56.7) |
| Weight loss | 1 (1.1) |
| Asymptomatic (PSA elevation on screening) | 4 (4.4) |
| PSA level at diagnosis (interquartile range) (ng/mL) | 151 (3–4850) |
| Gleason grade at diagnosis (n, %) | |
| Grade 7 | 7 (7.7) |
| Grade 8 | 28 (31.1) |
| Grade 9–10 | 55 (61.1) |
| Median follow-up (interquartile range) (months) | 22.3 (11.4–34.7) |
| Low Volume (n, %) | High Volume (n, %) | |
|---|---|---|
| Risk category (LATITUDE) | ||
| Low risk | 4 (80) | 2 (2.4) |
| High risk | 1 (20) | 83 (97.6) |
| First-line treatment in mCSPC | ||
| Docetaxel | – | 19 (22.4) |
| Abiraterone | 1 (20) | 25 (29.4) |
| Enzalutamide | 1 (20) | 12 (14.1) |
| ADT monotherapy | 2 (40) | 11 (12.9) |
| ADT + bicalutamide | 1 (20) | 18 (21.2) |
| Castration resistance following first-line therapy | ||
| Yes | – | 19 (22.4) |
| No | 5 (100) | 66 (77.6) |
| First-line treatment in mCRPC | ||
| Docetaxel | – | 5 (26.3) |
| Abiraterone | – | 8 (42.1) |
| Enzalutamide | – | 3 (15.8) |
| Best supportive care | – | 3 (15.8) |
| Progression after first-line treatment in mCRPC | ||
| Yes | – | 6 (31.6) |
| No | – | 13 (68.4) |
| Second-line treatment in mCRPC | ||
| Lutetium | – | 2 (33.3) |
| Best supportive care | – | 4 (66.7) |
| Variable | HR (95% CI) | p-Value | |
|---|---|---|---|
| Age at diagnosis | – | 1.05 (0.99–1.11) | 0.056 |
| Hypertension | Yes (ref) | 1.00 | – |
| No | 0.46 (0.23–0.92) | 0.028 | |
| Dyslipidemia | Yes (ref) | 1.00 | – |
| No | 0.91 (0.55–1.50) | 0.734 | |
| Diabetes | Yes (ref) | 1.00 | – |
| No | 0.86 (0.52–1.42) | 0.568 | |
| COPD | Yes (ref) | 1.00 | – |
| No | 1.12 (0.63–2.00) | 0.677 | |
| Coronary artery disease (CAD) | Yes (ref) | 1.00 | – |
| No | 1.23 (0.72–2.09) | 0.435 | |
| PSA at diagnosis (per 10 ng/mL increase) | – | 1.000 (0.997–1.003) | 0.656 |
| Gleason grade | Grade 7 (ref) | 1.00 | – |
| Grade 8 | 0.83 (0.28–2.50) | 0.752 | |
| Grade 9–10 | 1.12 (0.40–3.15) | 0.752 | |
| CHAARTED volume | Low-volume (ref) | 1.00 | – |
| High-volume | 1.43 (0.51–3.94) | 0.487 | |
| LATITUDE risk | Low-risk (ref) | 1.00 | – |
| High-risk | 1.39 (0.56–3.48) | 0.474 | |
| First-line treatment in mCSPC | Docetaxel (ref) | 1.00 | – |
| Abiraterone | 1.05 (0.53–2.06) | 0.793 | |
| Enzalutamide | 0.66 (0.29–1.49) | 0.793 | |
| LHRH agonist monotherapy | 0.99 (0.42–2.28) | 0.793 | |
| LHRH agonist + Bicalutamide | 1.06 (0.53–2.13) | 0.793 |
| Variable | HR (95% CI) | p-Value | |
|---|---|---|---|
| Age at diagnosis | 0.97 (0.85–1.10) | 0.649 | |
| Hypertension | Yes (ref) | 1.00 | – |
| No | 0.52 (0.16–1.67) | 0.275 | |
| Dyslipidemia | Yes (ref) | 1.00 | – |
| No | 1.36 (0.54–3.39) | 0.510 | |
| Diabetes | Yes (ref) | 1.00 | – |
| No | 1.04 (0.37–2.93) | 0.934 | |
| COPD | Yes (ref) | 1.00 | – |
| No | 0.61 (0.23–1.63) | 0.332 | |
| Coronary artery disease | Yes (ref) | 1.00 | – |
| No | 0.87 (0.33–2.33) | 0.794 | |
| PSA at diagnosis (per 10 ng/mL increase) | 1.000 (0.997–1.003) | 0.260 | |
| Gleason grade | Grade 7 (ref) | 1.00 | – |
| Grade 8 | 3.38 (0.43–26.50) | 0.088 | |
| Grade 9–10 | 1.25 (0.15–10.11) | 0.088 | |
| CHAARTED volume | Low-volume (ref) | 1.00 | – |
| High-volume | 1.49 (0.19–11.20) | 0.698 | |
| LATITUDE risk | Low-risk (ref) | 1.00 | – |
| High-risk | 1.90 (0.25–14.30) | 0.533 | |
| First-line treatment in mCSPC | Docetaxel (ref) | 1.00 | – |
| Abiraterone | 1.75 (0.53–5.76) | 0.776 | |
| Enzalutamide | 0.84 (0.19–3.62) | 0.776 | |
| LHRH agonist monotherapy | 1.72 (0.46–6.43) | 0.776 | |
| LHRH agonist + Bicalutamide | 1.98 (0.69–5.49) | 0.776 | |
| Castration resistance | No (ref) | 1.00 | – |
| Yes | 0.28 (0.06–1.22) | 0.092 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Published by MDPI on behalf of the Lithuanian University of Health Sciences. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ozberk, U.; Esen, S.A.; Uguz, A.; Algın, E.; Bal, O.; Akıncı, B.; Uncu, D. Elderly Men with De Novo Metastatic Castration-Sensitive Prostate Cancer: Therapy and Does Comorbidity Matter. Medicina 2025, 61, 2068. https://doi.org/10.3390/medicina61112068
Ozberk U, Esen SA, Uguz A, Algın E, Bal O, Akıncı B, Uncu D. Elderly Men with De Novo Metastatic Castration-Sensitive Prostate Cancer: Therapy and Does Comorbidity Matter. Medicina. 2025; 61(11):2068. https://doi.org/10.3390/medicina61112068
Chicago/Turabian StyleOzberk, Ugur, Selin Akturk Esen, Alican Uguz, Efnan Algın, Oznur Bal, Bulent Akıncı, and Dogan Uncu. 2025. "Elderly Men with De Novo Metastatic Castration-Sensitive Prostate Cancer: Therapy and Does Comorbidity Matter" Medicina 61, no. 11: 2068. https://doi.org/10.3390/medicina61112068
APA StyleOzberk, U., Esen, S. A., Uguz, A., Algın, E., Bal, O., Akıncı, B., & Uncu, D. (2025). Elderly Men with De Novo Metastatic Castration-Sensitive Prostate Cancer: Therapy and Does Comorbidity Matter. Medicina, 61(11), 2068. https://doi.org/10.3390/medicina61112068






