Femoral Malunion and Its Correction: A Review
Abstract
1. Introduction
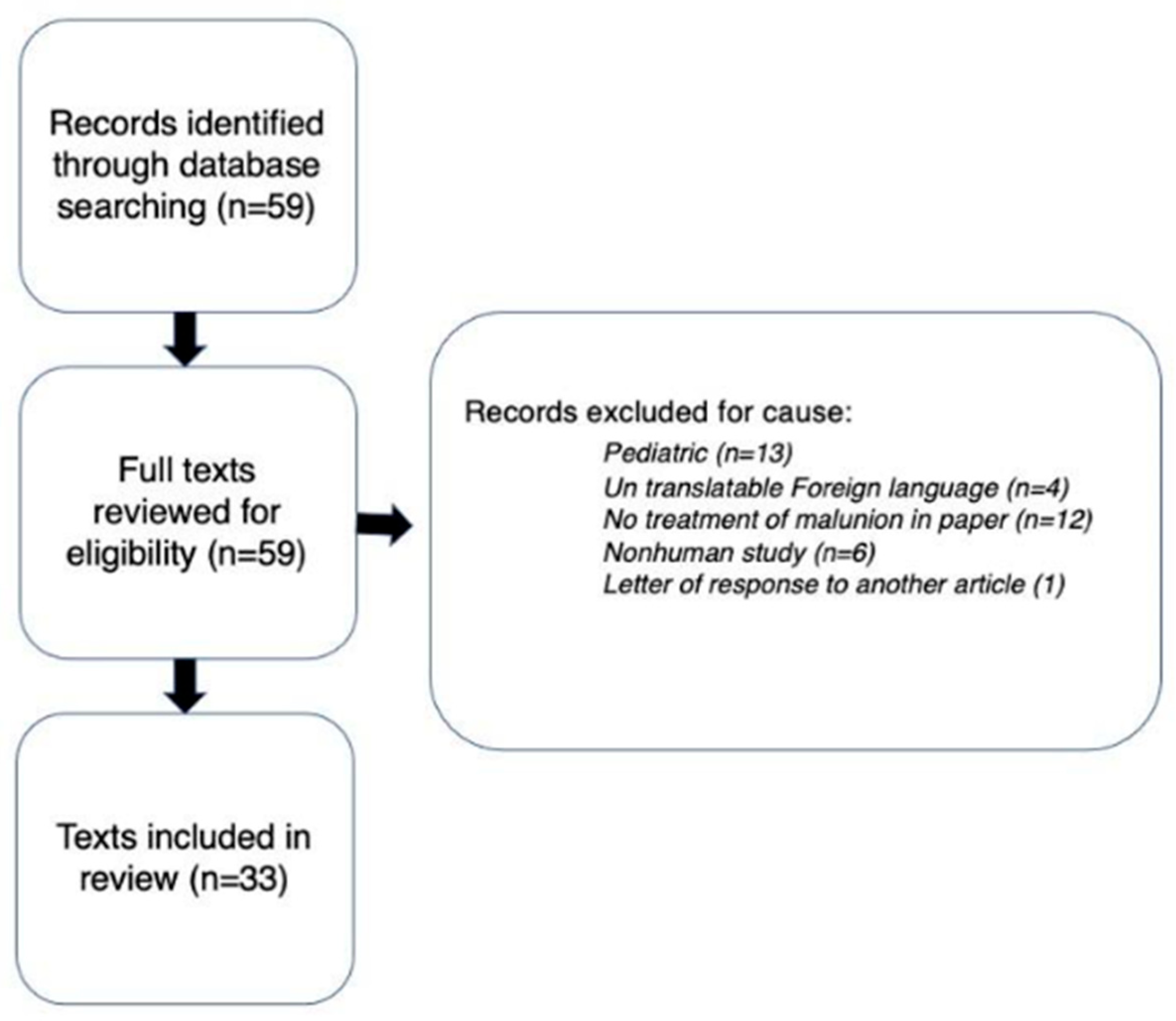
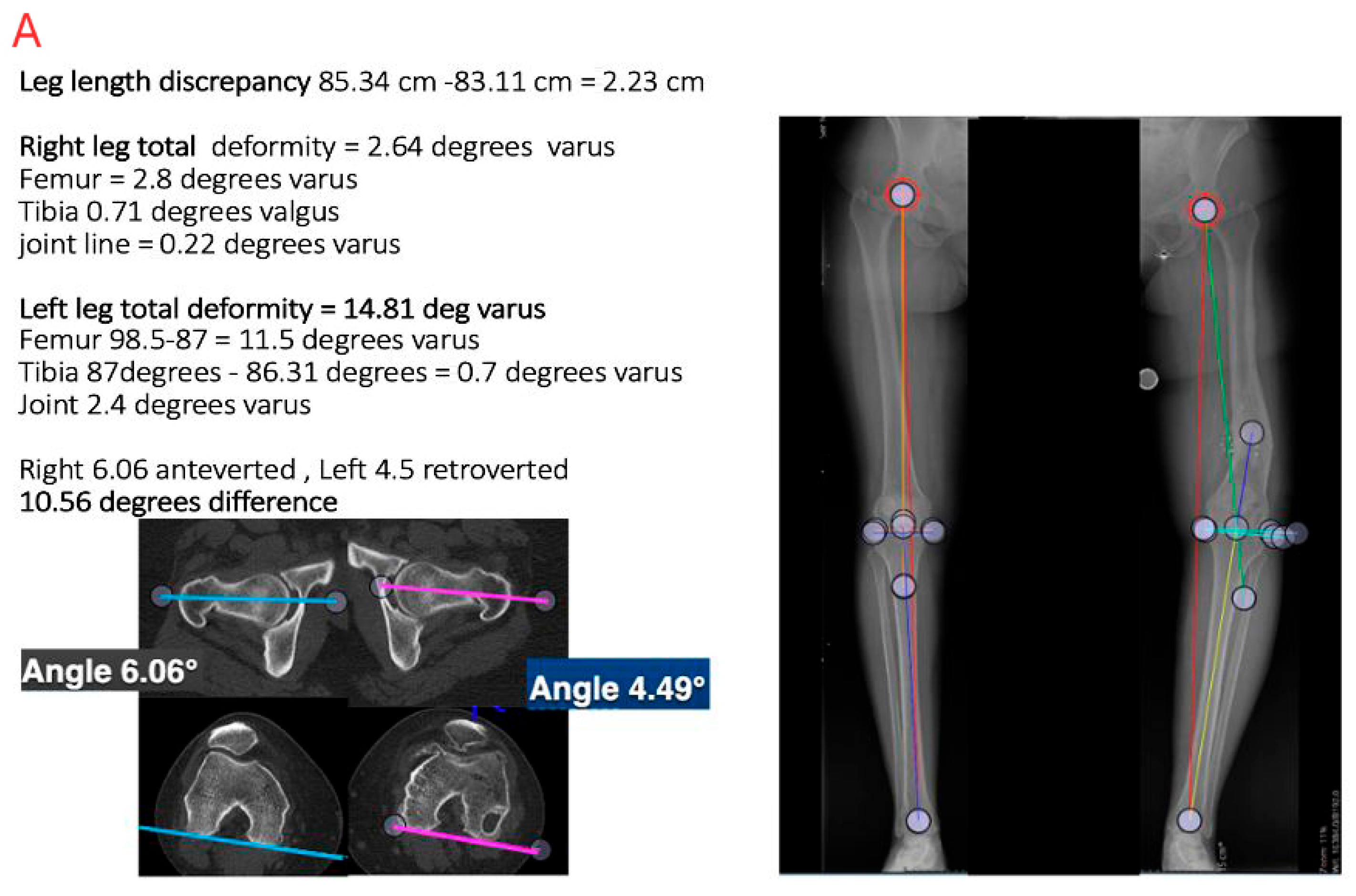
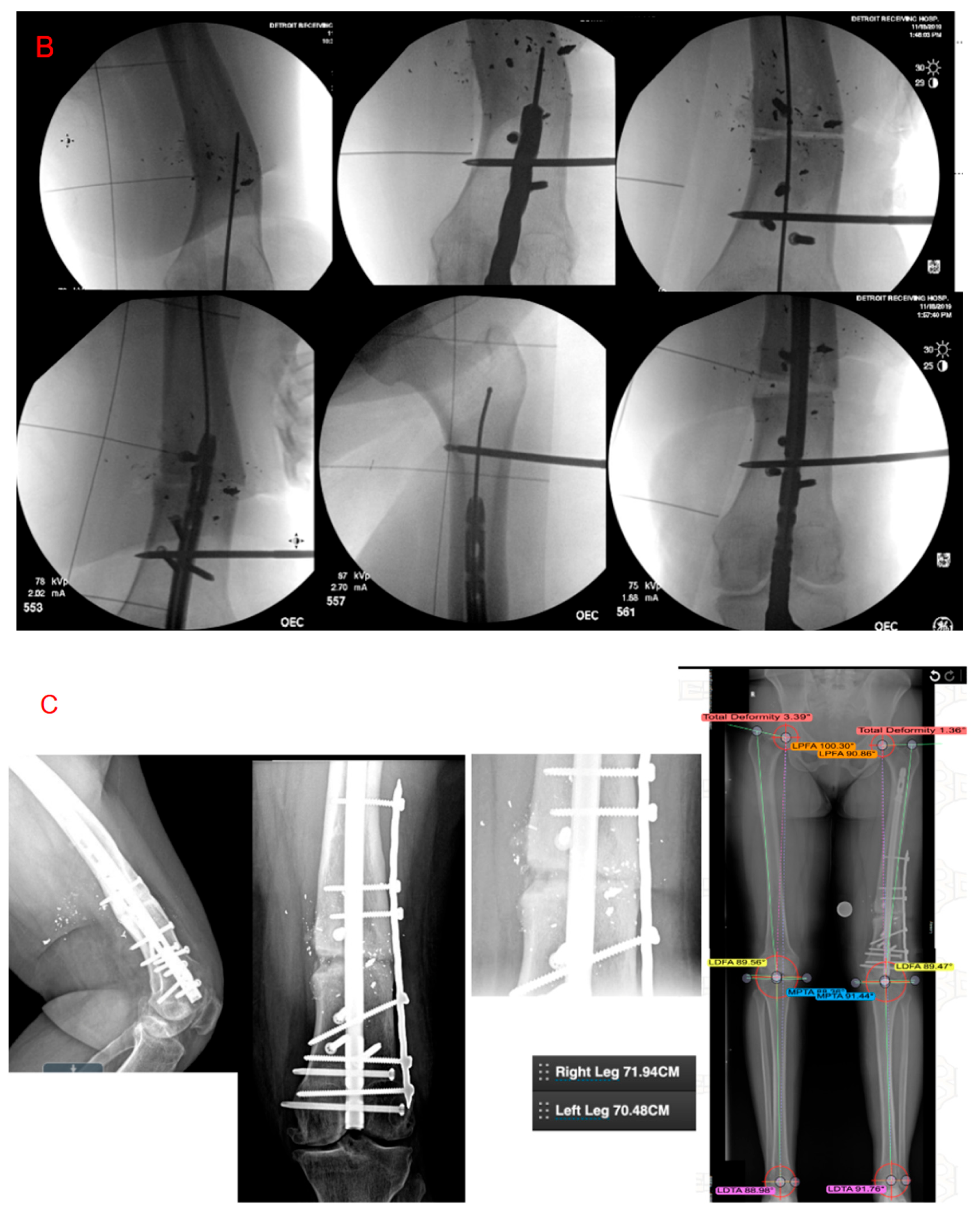
2. Materials and Methods
3. Definition of Femur Fracture Malunion
3.1. Cause of Femoral Malunion
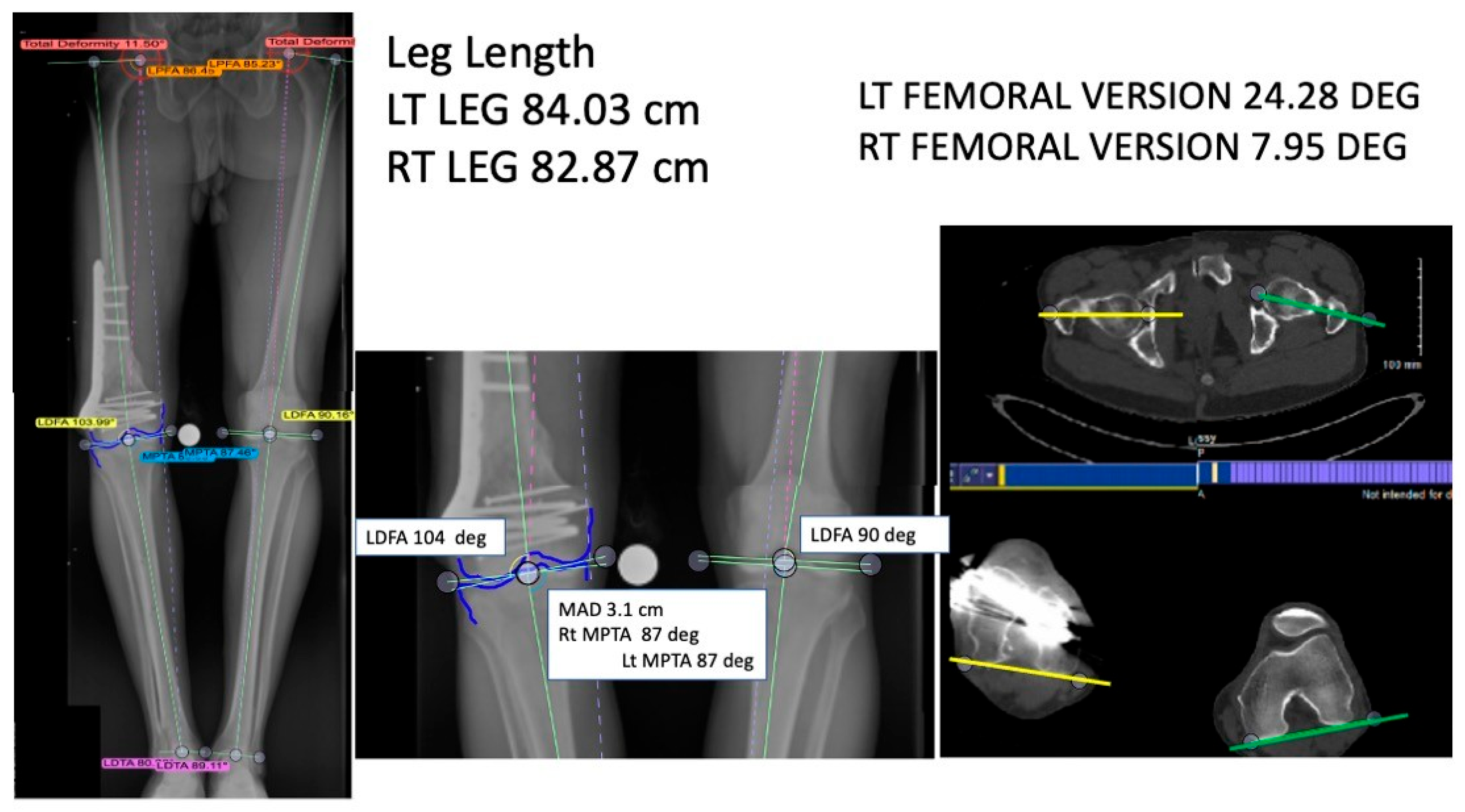
3.2. Evaluation
4. Malunion Manifestations
5. Surgical Indications, Procedures, and Outcomes
6. Femoral Head
7. Femoral Neck
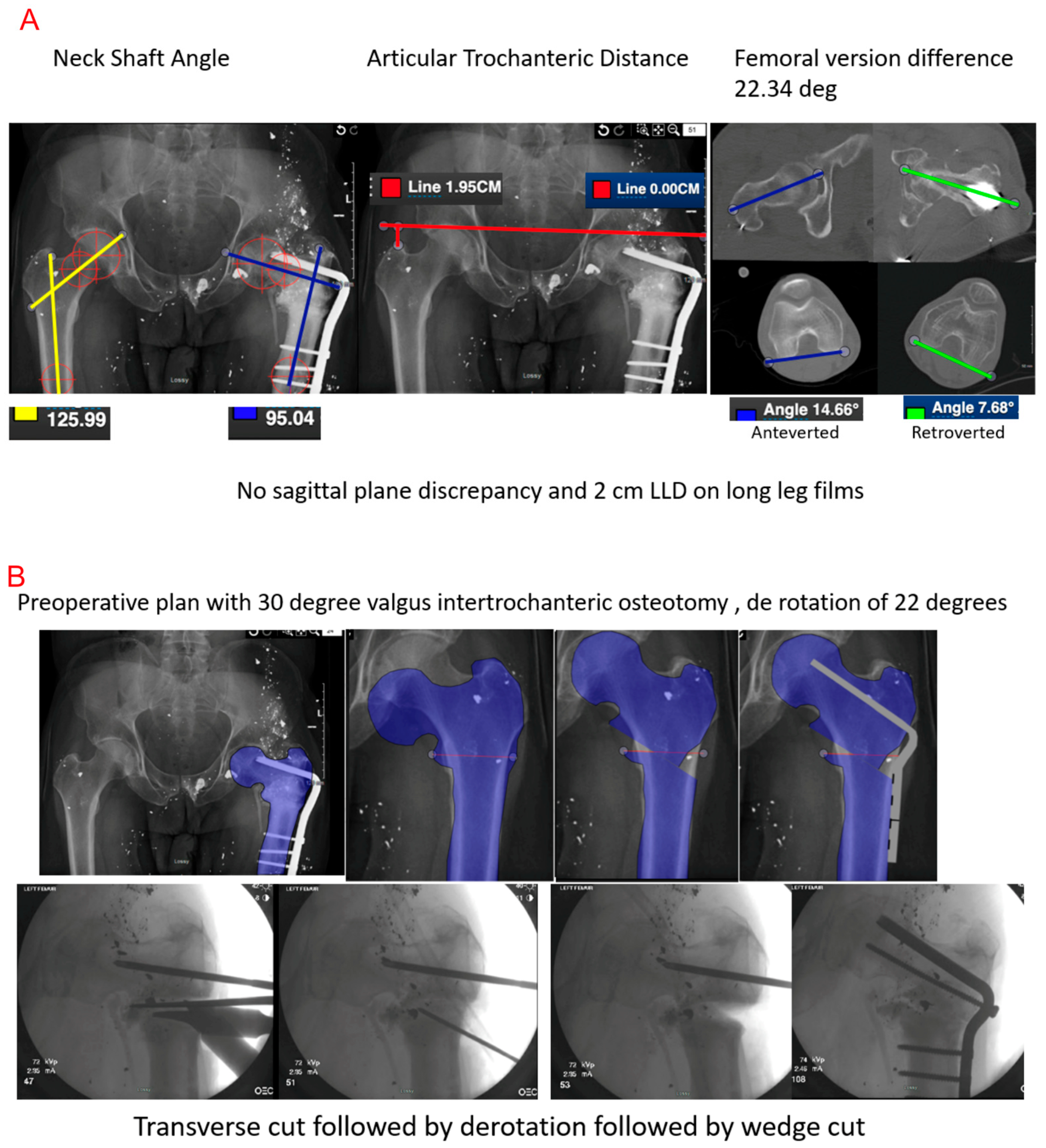
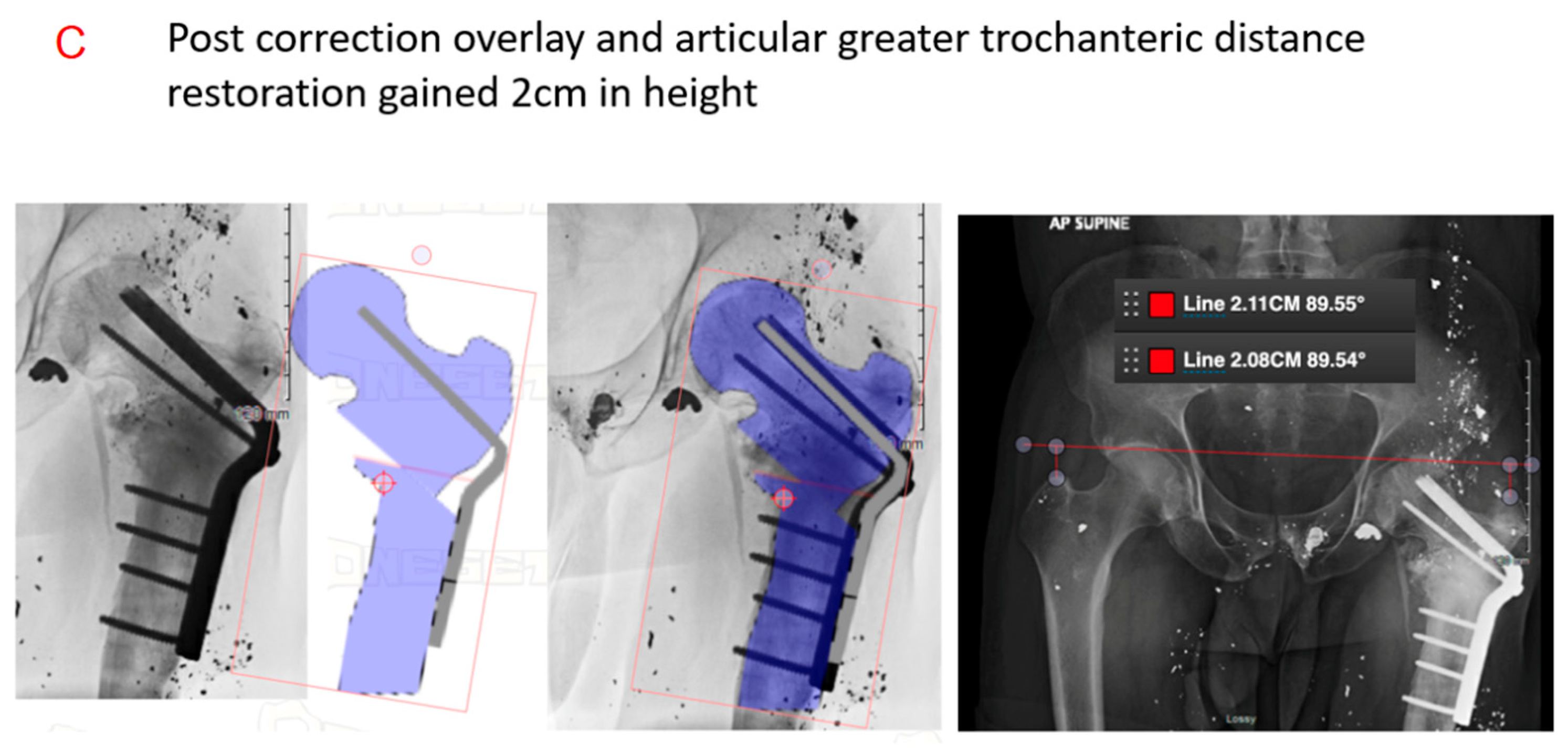
Peritrochanteric/Intertrochanteric
8. Femur Shaft Malunion
9. Distal Femur
Complications
10. Limitations
11. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| LLD | Leg Length Discrepancy |
| MAD | Mechanical axis deviation |
| CT | Computed Tomography |
| AP | Anteroposterior |
| LDFA | Lateral distal femoral angle |
| PDFA | Posterior distal femoral angle |
| MLDFA | Mechanical lateral distal femoral angle |
| APDFA | Anatomic posterior distal femoral angle |
| MPTA | Medial proximal tibial angle |
| VITO | Valgus intertrochanteric osteotomy |
| SHS | Sliding hip screw |
| CMN | Cephalo-medullary nailing |
| ABP | Angled blade plates |
| OHS | Oxford hip score |
| PMS | Parker mobility scale |
| ROM | Range of motion |
| TKA | Total knee arthroplasty |
| VAS | Visual assessment scale |
| MFTA | Mechanical femoral tibial angle |
| JLCA | Joint line convergence angle |
References
- Ekegren, C.L.; Edwards, E.R.; de Steiger, R.; Gabbe, B.J. Incidence, Costs and Predictors of Non-Union, Delayed Union and Mal-Union Following Long Bone Fracture. Int. J. Environ. Res. Public Health 2018, 15, 2845. [Google Scholar] [CrossRef]
- Zehntner, M.K.; Marchesi, D.G.; Burch, H.; Ganz, R. Alignment of supracondylar/intercondylar fractures of the femur after internal fixation by AO/ASIF technique. J. Orthop. Trauma 1992, 6, 318–326. [Google Scholar] [CrossRef] [PubMed]
- Link, B.C.; Babst, R. Current concepts in fractures of the distal femur. Acta Chir. Orthop. Traumatol. Cechoslov. 2012, 79, 11–20. [Google Scholar] [CrossRef] [PubMed]
- Acharya, K.N.; Rao, M.R. Retrograde nailing for distal third femoral shaft fractures: A prospective study. J. Orthop. Surg. 2006, 14, 253–258. [Google Scholar] [CrossRef] [PubMed]
- Phillips, J.R.; Trezies, A.J.; Davis, T.R. Long-term follow-up of femoral shaft fracture: Relevance of malunion and malalignment for the development of knee arthritis. Injury 2011, 42, 156–161. [Google Scholar] [CrossRef]
- Agarwal, A. Malunions: Introduction and Brief Overview; Springer: New York, NY, USA, 2021; pp. 1–12. [Google Scholar]
- Agrawal, A.; Kiyawat, V. Complex AO type C3 distal femur fractures: Results after fixation with a lateral locked plate using modified swashbuckler approach. Indian J. Orthop. 2017, 51, 18–27. [Google Scholar] [CrossRef]
- Gelalis, I.D.; Politis, A.N.; Arnaoutoglou, C.M.; Korompilias, A.V.; Pakos, E.E.; Vekris, M.D.; Karageorgos, A.; Xenakis, T.A. Diagnostic and treatment modalities in nonunions of the femoral shaft: A review. Injury 2012, 43, 980–988. [Google Scholar] [CrossRef]
- Bhandari, M.; Fong, K.; Sprague, S.; Williams, D.; Petrisor, B. Variability in the definition and perceived causes of delayed unions and nonunions: A cross-sectional, multinational survey of orthopaedic surgeons. J. Bone Jt. Surg. Am. 2012, 94, e1091–e1096. [Google Scholar] [CrossRef]
- Castillo, R.C.; Bosse, M.J.; MacKenzie, E.J.; Patterson, B.M.; Group, L.S. Impact of smoking on fracture healing and risk of complications in limb-threatening open tibia fractures. J. Orthop. Trauma 2005, 19, 151–157. [Google Scholar] [CrossRef]
- Gandhi, A.; Liporace, F.; Azad, V.; Mattie, J.; Lin, S.S. Diabetic fracture healing. Foot Ankle Clin. 2006, 11, 805–824. [Google Scholar] [CrossRef]
- McKee, M.D.; DiPasquale, D.J.; Wild, L.M.; Stephen, D.J.; Kreder, H.J.; Schemitsch, E.H. The effect of smoking on clinical outcome and complication rates following Ilizarov reconstruction. J. Orthop. Trauma 2003, 17, 663–667. [Google Scholar] [CrossRef]
- Murnaghan, M.; Li, G.; Marsh, D.R. Nonsteroidal anti-inflammatory drug-induced fracture nonunion: An inhibition of angiogenesis? J. Bone Jt. Surg. Am. 2006, 88, 140–147. [Google Scholar] [CrossRef]
- Riehl, J.T.; Widmaier, J.C. Techniques of obtaining and maintaining reduction during nailing of femur fractures. Orthopedics 2009, 32, 581. [Google Scholar] [CrossRef] [PubMed]
- Calori, G.M.; Colombo, M.; Mazza, E.L.; Mazzola, S.; Malagoli, E.; Marelli, N.; Corradi, A.l. Validation of the Non-Union Scoring System in 300 long bone non-unions. Injury 2014, 45, S93–S97. [Google Scholar] [CrossRef] [PubMed]
- Fakler, J.K.; Hepp, P.; Marquass, B.; von Dercks, N.; Josten, C. Is distal femoral replacement an adequate therapeutic option after complex fractures of the distal femur? Z. Orthop. Unfallchirurgie 2013, 151, 173–179. [Google Scholar]
- Patterson, R.H. Malunion of Fractures of the Femur. Ann. Surg. 1931, 93, 984–997. [Google Scholar] [CrossRef]
- Wu, C.C. An improved surgical technique to treat femoral shaft malunion: Revised reamed intramedullary nailing technique. Arch. Orthop. Trauma Surg. 2001, 121, 265–270. [Google Scholar] [CrossRef]
- Saleeb, H.; Tosounidis, T.; Papakostidis, C.; Giannoudis, P.V. Incidence of deep infection, union and malunion for open diaphyseal femoral shaft fractures treated with IM nailing: A systematic review. Surgeon 2019, 17, 257–269. [Google Scholar] [CrossRef]
- Bhowmick, K.; Matthai, T.; Boopalan, P.R.J.; Jepegnanam, T.S. Decision making in the management of malunion and nonunion of intertrochanteric fractures of the hip. Hip Int. 2020, 30, 793–798. [Google Scholar] [CrossRef]
- Ozan, F.; Okur, K.T.; Unlu, O.C.; Melez, M.; Yamak, K.; Kayali, C.; Altay, T. Corrective Osteotomy for Coronal Plane Malunion of the Medial Femoral Condyle. Cureus 2018, 10, e3222. [Google Scholar] [CrossRef]
- Paley, D. Principles of Deformity Correction; Springer: Berlin/Heidelberg, Germany, 2002; pp. 31–60. [Google Scholar]
- Rollo, G.; Pichierri, P.; Grubor, P.; Marsilio, A.; Bisaccia, M.; Grubor, M.; Bisaccia, M.; Grubor, M.; Pace, V.; Riccardo, M.L.; et al. The challenge of nonunion and malunion in distal femur surgical revision. Med. Glas. 2019, 16. [Google Scholar] [CrossRef]
- Middleton, S.; Walker, R.W.; Norton, M. Decortication and osteotomy for the correction of multiplanar deformity in the treatment of malunion in adult diaphyseal femoral deformity: A case series and technique description. Eur. J. Orthop. Surg. Traumatol. 2018, 28, 117–120. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.W.; Chen, W.S.; Lin, P.C.; Hsu, C.S.; Wang, C.J. Total knee replacement with intra-articular resection of bone after malunion of a femoral fracture: Can sagittal angulation be corrected? J. Bone Jt. Surg. Br. 2010, 92, 1392–1396. [Google Scholar] [CrossRef] [PubMed]
- van der Woude, J.A.; Spruijt, S.; van Ginneken, B.T.; van Heerwaarden, R.J. Distal femoral valgus osteotomy: Bone healing time in single plane and biplanar technique. Strateg. Trauma Limb Reconstr. 2016, 11, 177–186. [Google Scholar] [CrossRef] [PubMed]
- He, Q.F.; Wang, H.X.; Sun, H.; Zhan, Y.; Zhang, B.B.; Xie, X.T.; Luo, C.F. Medial Open-wedge Osteotomy with Double-plate Fixation for Varus Malunion of the Distal Femur. Orthop. Surg. 2019, 11, 82–90. [Google Scholar] [CrossRef]
- Yoon, T.R.; Chung, J.Y.; Jung, S.T.; Seo, H.Y. Malunion of femoral head fractures treated by partial ostectomy: Three case reports. J. Orthop. Trauma 2003, 17, 447–450. [Google Scholar] [CrossRef]
- Ross, J.R.; Clohisy, J.C. Correction of a Femoral Head Fracture Malunion with Surgical Dislocation of the Hip: A Case Report. JBJS Case Connect. 2012, 2, e71. [Google Scholar] [CrossRef]
- Matsuda, D.K. Arthroscopic osteosynthesis of femoral head malunion. Arthrosc. Tech. 2014, 3, e31–e34. [Google Scholar] [CrossRef]
- Jackson, M.; Learmonth, I.D. The treatment of nonunion after intracapsular fracture of the proximal femur. Clin. Orthop. Relat. Res. 2002, 399, 119–128. [Google Scholar] [CrossRef]
- Garden, R.S. Reduction and fixation of subcapital fractures of the femur. Orthop. Clin. N. Am. 1974, 5, 683–712. [Google Scholar] [CrossRef]
- Haidukewych, G.J.; Rothwell, W.S.; Jacofsky, D.J.; Torchia, M.E.; Berry, D.J. Operative treatment of femoral neck fractures in patients between the ages of fifteen and fifty years. J. Bone Jt. Surg. Am. 2004, 86, 1711–1716. [Google Scholar] [CrossRef]
- Satish, B.R.; Ranganadham, A.V.; Ramalingam, K.; Tripathy, S.K. Four quadrant parallel peripheral screw fixation for displaced femoral neck fractures in elderly patients. Indian J. Orthop. 2013, 47, 174–181. [Google Scholar] [CrossRef]
- Verma, N.; Singh, M.P.; Ul Haq, R.; Aggarwal, A.N.; Jain, A. Malunion in displaced intracapsular fracture of femoral neck: A rare case. Chin. J. Traumatol. 2015, 18, 307–310. [Google Scholar] [CrossRef] [PubMed]
- Haidukewych, G.J.; Berry, D.J. Salvage of failed treatment of hip fractures. J. Am. Acad. Orthop. Surg. 2005, 13, 101–109. [Google Scholar] [CrossRef] [PubMed]
- Bartonícek, J.; Skála-Rosenbaum, J.; Dousa, P. Valgus intertrochanteric osteotomy for malunion and nonunion of trochanteric fractures. J. Orthop. Trauma 2003, 17, 606–612. [Google Scholar] [CrossRef] [PubMed]
- Subash, Y. Valgus Osteotomy with DHS Fixation in the Management of Malunited Intertrochanteric Fractures in a Rural Population. Malays. Orthop. J. 2020, 14, 98–103. [Google Scholar] [CrossRef]
- Butala, R.; Mukherjee, S.; Samant, P.; Khedekar, R. Valgus subtrochanteric osteotomy for malunited intertrochanteric fractures: Our experience in 5 cases. Indian J. Basic Appl. Med. Res. 2016, 6, 176–182. [Google Scholar]
- Gosselin, R.; Lavaly, D. Perkins traction for adult femoral shaft fractures: A report on 53 patients in Sierra Leone. Int. Orthop. 2007, 31, 697–702. [Google Scholar] [CrossRef]
- Vaidya, R.; Dimovski, R.; Cizmic, Z.; Vaidya, A.; Gheraibeh, P.; Hudson, I. Use of Inherent Anteversion of an Intramedullary Nail to Avoid Malrotation in Comminuted Femur Fractures: A Prospective Case–Control Study. J. Orthop. Trauma 2018, 32, 623–628. [Google Scholar] [CrossRef]
- Gheraibeh, P.; Vaidya, R.; Hudson, I.; Meehan, R.; Tonnos, F.; Sethi, A. Minimizing Leg Length Discrepancy After Intramedullary Nailing of Comminuted Femoral Shaft Fractures: A Quality Improvement Initiative Using the Scout Computed Tomography Scanogram. J. Orthop. Trauma 2018, 32, 256–262. [Google Scholar] [CrossRef]
- Farquharson-Roberts, M.A. Corrective osteotomy for combined shortening and rotational malunion of the femur. J. Bone Jt. Surg. Br. 1995, 77, 979–980. [Google Scholar] [CrossRef]
- Marsh, D.R.; Shah, S.; Elliott, J.; Kurdy, N. The Ilizarov method in nonunion, malunion and infection of fractures. J. Bone Jt. Surg. Br. 1997, 79, 273–279. [Google Scholar] [CrossRef]
- Sangeorzan, B.J.; Sangeorzan, B.P.; Hansen, S.T., Jr.; Judd, R.P. Mathematically directed single-cut osteotomy for correction of tibial malunion. J. Orthop. Trauma 1989, 3, 267–275. [Google Scholar] [CrossRef] [PubMed]
- Johnson, E.E. Multiplane correctional osteotomy of the tibia for diaphyseal malunion. Clin. Orthop. Relat. Res. 1987, 215, 223–232. [Google Scholar] [CrossRef]
- Mayo, K.A.; Benirschke, S.K. Treatment of tibial malunions and nonunions with reamed intramedullary nails. Orthop. Clin. N. Am. 1990, 21, 715–724. [Google Scholar] [CrossRef]
- Lammens, J.; Van Laer, M.; Motmans, R. Ilizarov treatment for femoral mal-union or non-union associated with fatigue fracture of an intramedullary nail. Injury 2008, 39, 256–259. [Google Scholar] [CrossRef]
- Tall, M.; Ouedraogo, I.; Nd Kasse, A.; Tekpa, B.J.; Bonkoungou, G.; Belem, S.; Toe, M.F.; Da, S.C. Femur malunion treated with open osteotomy and intramedullary nailing in developing countries. Orthop. Traumatol. Surg. Res. 2012, 98, 784–787. [Google Scholar] [CrossRef]
- Ries, M.; O’Neill, D. A method to determine the true angulation of long bone deformity. Clin. Orthop. Relat. Res. 1987, 218, 191–194. [Google Scholar] [CrossRef]
- Russell, G.V.; Graves, M.L.; Archdeacon, M.T.; Barei, D.P.; Brien, G.A., Jr.; Porter, S.E. The clamshell osteotomy: A new technique to correct complex diaphyseal malunions. J. Bone Jt. Surg. Am. 2009, 91, 314–324. [Google Scholar] [CrossRef]
- Wilson, A.J.; Nandi, S.; Robbins, C.E.; Bono, J.V. TKA after clamshell osteotomy for femoral diaphyseal malunion. Orthopedics 2012, 35, e969–e972. [Google Scholar] [CrossRef]
- Knight, J.L.; Ratcliffe, S.S.; Weber, J.K.; Hansen, S.T., Jr. Corrective osteotomy of femoral shaft malunion causing complete occlusion of the superficial femoral artery. J. Bone Jt. Surg. Am. 1980, 62, 303–306. [Google Scholar] [CrossRef]
- Paley, D.; Chaudray, M.; Pirone, A.M.; Lentz, P.; Kautz, D. Treatment of malunions and mal-nonunions of the femur and tibia by detailed preoperative planning and the Ilizarov techniques. Orthop. Clin. N. Am. 1990, 21, 667–691. [Google Scholar] [CrossRef]
- Mast, J.W.; Teitge, R.A.; Gowda, M. Preoperative planning for the treatment of nonunions and the correction of malunions of the long bones. Orthop. Clin. N. Am. 1990, 21, 693–714. [Google Scholar] [CrossRef]
- Gangavalli, A.K.; Nwachuku, C.O. Management of Distal Femur Fractures in Adults: An Overview of Options. Orthop. Clin. N. Am. 2016, 47, 85–96. [Google Scholar] [CrossRef]
- Paley, D.; Herzenberg, J.E.; Tetsworth, K.; McKie, J.; Bhave, A. Deformity planning for frontal and sagittal plane corrective osteotomies. Orthop. Clin. N. Am. 1994, 25, 425–465. [Google Scholar] [CrossRef]
- Wu, C.C. A novel approach for evaluating acceptable intra-operative correction of lower limb alignment in femoral and tibial malunion using the deviation angle of the normal contralateral knee. Knee 2014, 21, 573–581. [Google Scholar] [CrossRef]
- Gugenheim, J.J., Jr.; Brinker, M.R. Bone realignment with use of temporary external fixation for distal femoral valgus and varus deformities. J. Bone Jt. Surg. Am. 2003, 85, 1229–1237. [Google Scholar] [CrossRef]
- Chou, W.Y.; Ko, J.Y.; Wang, C.J.; Wang, F.S.; Wu, R.W.; Wong, T. Navigation-assisted total knee arthroplasty for a knee with malunion of the distal femur. J. Arthroplast. 2008, 23, 1239.e13–1239.e17. [Google Scholar] [CrossRef]
- Sasidharan, B.; Shetty, S.; Philip, S.; Shetty, S. Reconstructive osteotomy for a malunited medial Hoffa fracture—A feasible salvage option. J. Orthop. 2016, 13, 132–135. [Google Scholar] [CrossRef]
- Winquist, R.A. Closed intramedullary osteotomies of the femur. Clin. Orthop. Relat. Res. 1986, 212, 155–164. [Google Scholar] [CrossRef]
- Kempfe, I.; Grosse, A.; Abalo, C. Locked Intramedullary Nailing: Its Application to Femoral and Tibial Axial, Rotational, Lengthening, and Shortening Osteotomies. Clin. Orthop. Relat. Res. 1986, 212, 165–173. [Google Scholar] [CrossRef]
- Keshet, D.; Eidelman, M. Clinical utility of the Taylor spatial frame for limb deformities. Orthop. Res. Rev. 2017, 9, 51–61. [Google Scholar] [CrossRef] [PubMed]
- Kirane, Y.M.; Fragomen, A.T.; Rozbruch, S.R. Precision of the PRECICE internal bone lengthening nail. Clin. Orthop. Relat. Res. 2014, 472, 3869–3878. [Google Scholar] [CrossRef] [PubMed]
- Chiodo, C.P.; Jupiter, J.B.; Alvarez, G.; Chandler, H.P. Oblique osteotomy for multiplanar correction of malunions of the femoral shaft. Clin. Orthop. Relat. Res. 2003, 406, 185–194. [Google Scholar] [CrossRef]
| Study | Patients (n) | Surgical Treatment | Outcomes |
|---|---|---|---|
| Yoon et al. 2003 [28] | 3 | Partial femoral head ostectomy | Union eventually achieved in all cases, with return to activity and painless near-normal range of motion |
| Ross et al. 2012 [29] | 1 | Open corrective osteotomy, femoral head | Improved functional outcome score, with full return to activities and no residual motion deficits |
| Matsuda et al. 2014 [30] | 1 | Arthroscopic osteotomy of femoral head with bone grafting, screw fixation, and cephaloplasty | Return of preoperative motion, gait, and activity level, and improved functional outcome score |
| Verma et al. 2015 [35] | 1 | Non-operative treatment, displaced femoral neck | Successful union through callus formation. Full restoration of hip motion, complete absence of pain, and no restrictions during activity |
| Butala et al. 2016 [39] | 5 | Lateral closed wedge valgus osteotomy | All patients achieved radiographic union; femoral neck–shaft angle was corrected to 130 degrees or greater for every patient; average Oxford Hip Score 39 |
| Subash 2011 [38] | 15 | Valgus osteotomy with DHS fixation | All patients healed without complications; improved mean Harris Hip Score from 72.33 (61–80) to 91 (80–97); and nearly anatomical abduction, adduction, flexion, internal rotation, and external rotation |
| Bhowmick et al. 2020 [20] | 12 | Valgus osteotomy | All patients healed without complications with either absent or mild pain; average Parker Mobility Scale score 8.25 (9–5) |
| Bartonícek et al. 2003 [37] | 11 | Valgus intertrochanteric osteotomy | All patients achieved radiographic union with one patient requiring revision surgery and two delayed union; average Harris Hip Score increased to 90.2 (76–98) from 75 (65–82) |
| Study | Patients (n) | Deformity | Surgical Treatment | Outcomes | Complications |
|---|---|---|---|---|---|
| Knight et al. 1980 [53] | 1 | 35 degrees anterior angulation; 25 degrees external rotation | Osteotomy with Kuntscher nail | Anatomic correction | Occlusion sup femoral artery |
| I. Kempf et al. 1986 [63] | 15 | 12 LLD plus axial 3 | Acute lengthening up to 4cm with 13 Z osteotomies, 1 oblique, 1 transverse/12 lengthening 3 length rotation | Healed some loss of length | 3 deep infections and 2 losses of correction |
| Winquist 1986 [62] | 12 | Angular not described | Angular deformities osteotomy plus bone graft if an open wedge occurs | 10 /12 anatomic | 2 incomplete corrections |
| Paley et al. 1990 [54] | 6 | Short >1.5 cm angulation >5 deg Rotation >15 deg translation >1 cm | Percutaneous Osteotomy and Illizarov apparatus | All corrected | Minor pin tract infections |
| Mast et al. 1990 [55] | 12 | 0–3.5 cm short, 15 val to 20 var 5 pro to 35 recurvatum, 0–30 deg ir | Osteotomy closing or open wedge with plate | All reduced within acceptable parameters | N/a |
| Farquharson-Roberts 1995 [43] | 1 | Rotational deformity >10°, LLD >1.5 cm, shortening >3.5 cm; external rotation deformity ~30° | Oblique rotational osteotomy/IM Nail | Complete correction of rotational and angular deformity within 1 cm | N/a |
| Wu et al. 2001 [18] | 21 | Angulation 24 + 6 deg 18 pts/malrotation 25–30 deg in 3 pts shortening of >2 cm 10 pts | Oblique rotational osteotomy/IM Nail | Restored knee ROM and deformity, healed to normal parameters (angulation < 10°; malrotation < 10°; shortening < 2cm) | N/a |
| Chiodo et al. 2003 [66] | 6 | Average varus 21.7° (range, 12°–32°); average antecurvatum 22.8° (range, 10°–30°); average leg length discrepancy was 1.8 cm (range, 0.5–3 cm | Osteotomy with ORIF Plate | Average varus deformity improved from 21.6 degrees to 4.2 degrees. The average deformity improved from 22.5 degrees to 7.0 degrees antecurvatum | N/a |
| Lammens et al. 2008 [48] | 1 | 2 cm shortening; unspecified amount of antecurvatum | Ilizarov percutaneous osteotomy/removal of prior nail | Anatomic correction | N/a |
| Russell et al. 2009 [51] | 4 | Unspecified/non-quantified deformity | Clamshell osteotomy with intramedullary nail | Complete correction of limb length inequalities to within 2 cm (0–5 cm) | N/a |
| Tall et al. 2012 [49] | 16 | Mean LLD of 3 cm (2–6 cm); mean knee flexion limitation of 90° | Oblique rotational osteotomy IM Nail | Healed to normal parameters (angulation < 10°; malrotation < 10°; shortening < 2cm) | N/a |
| Middleton et al. 2018 [24] | 7 | Average shortening of 2.7 cm. 5/7 had average rotational deformity of 33°. 2/7 with tri-planar deformity (vs. biplanar in 5/7 | Oblique rotational osteotomy plate graft | Healed to normal parameters (angulation < 10°; malrotation < 10°; shortening < 2 cm) | N/a |
| Study | Patients (n) | Deformity | Surgical Treatment | Outcomes |
|---|---|---|---|---|
| Gugenheim et al. 2003 [59] | 2 | Mechanical axis deviation of >15 mm; mLDFA <85° or >90° 90 mm lateral to 120 mm medial | Temporary external fixation and subsequent percutaneous dome osteotomy retrograde nail | Correction of mLDFA and mechanical axis Average mLDFA ~89° MAD <15 |
| Chou et al. 2008 [60] | 1 | 15° of coronal plane varus and 8.7° within the sagittal plane, mechanical and anatomical axes in 8° and 3° of varus | Navigation-assisted TKA | Resolution of pain and LLD; ROM improved Radiographically normal knee alignment |
| Wu et al. 2014 [58] | 24 | aLDFA bw 2 and 14 deg varus | Opening-wedge osteotomy Blade plate or nail multi-planar deformity | Ideal knee alignment and knee function 4.2 mo healing time, 4 nonunions 2 infected, repeat surgery healed them correction to within 3 deg of aLDFA 79–82 deg |
| van der Woude et al. 2016 [26] | 5 | Non-zero mFTA; MPTA and mLDFA <85° or >90°; knee JLCA >3° medially | Lateral closing wedge valgus osteotomy single plane deformity uni- or biplanar osteotomy | VAS scores improved with maintained range of motion biplanar healed faster average correction of preoperative mFTA from 10.0° (±2.6°) of varus to 3.1° (±2.6°) varus postoperatively, and of mLDFA from 95.9 (±2.7) to 89.3 (±2.9), with no significant changes in MPTA or JLCA |
| Sasidharan et al. 2016 [61] | 1 | Incongruous femoral knee joint surface | Open intraarticular corrective osteotomy | Improved ROM Complete anatomic alignment 20–80 deg to 5 to 110 deg |
| Ozan et al. [21] 2018 [21] | 1 | Incongruous femoral knee joint surface | Open intraarticular corrective osteotomy | Improvements in function and pain, with return to normal activities Complete anatomic alignment 25 deg flexion contracture improved ROM and function |
| He et al. 2019 [27] | 15 | Non-zero mFTA; mLDFA <87° or >90°, aPDFA of <79° or >87°; LLD >2–3 cm | Medial open-wedge osteotomy with double plate fixation | LLD improved to 0.8cm; VAS scores increased mFTA from 17.5° preoperatively to 2.3° postoperatively; mLDFA from 102.3° to 85.2°; aPDFA from 77.1° to 82.7°; and LLD from 3.38 cm to 0.8 cm |
| Rollo et al. 2019 [23] | 22 | mLDFA <85° or >90°in the coronal plane, PDFA <79° or >87° in the sagittal plane. Any rotational or intraarticular deformity. No specific radiographic parameters noted. | Lateral closed-wedge blade plate augmented with an auto- or allograft strut | Improved functional outcome scores had poor outcomes. Bony union with significant improvements in limb length discrepancy, quality of life, and knee functionality; no correctional parameters given |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Published by MDPI on behalf of the Lithuanian University of Health Sciences. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Vaidya, R.; Mazur, M.; Agomuoh, I.; Abdelnour, D.; Boutany, M.; Teitge, R. Femoral Malunion and Its Correction: A Review. Medicina 2025, 61, 2050. https://doi.org/10.3390/medicina61112050
Vaidya R, Mazur M, Agomuoh I, Abdelnour D, Boutany M, Teitge R. Femoral Malunion and Its Correction: A Review. Medicina. 2025; 61(11):2050. https://doi.org/10.3390/medicina61112050
Chicago/Turabian StyleVaidya, Rahul, Matthew Mazur, Ihunanya Agomuoh, David Abdelnour, Magd Boutany, and Robert Teitge. 2025. "Femoral Malunion and Its Correction: A Review" Medicina 61, no. 11: 2050. https://doi.org/10.3390/medicina61112050
APA StyleVaidya, R., Mazur, M., Agomuoh, I., Abdelnour, D., Boutany, M., & Teitge, R. (2025). Femoral Malunion and Its Correction: A Review. Medicina, 61(11), 2050. https://doi.org/10.3390/medicina61112050






